Abstract
Background
A diseased lumbar intervertebral vacuum disc void of any structurally intact tissue may be vertically unstable. A primary standalone endoscopic decompression and interbody fusion surgery in the treatment of vertical instability in patients with a vacuum disc may be a more reliable treatment than decompression alone.
Methods
The authors solicited responses to an online survey sent to spine surgeons by email, and chat groups on social media networks, including Facebook, WeChat, WhatsApp, and Linkedin. Descriptive and correlative statistics were employed to count the responses and compare the surgeon’s responses recorded on a Likert scale from 1 (disagree) to 10 (agree) or in multiple-choice questions. Surgeons were asked about their familiarity with the concept of vacuum disc and vertical instability and how they would treat such patients. Kappa statistics and linear regression analysis of agreement of incoming responses were performed.
Results
A total of 1,165 surgeons accessed the survey. The completion rate was 22.78. The majority surgeons were very familiar with the concept of a “vacuum disc” as a sign of end-stage lumbar degenerative disc disease and a collapsing lumbar motion segment (182/273; 66.7%; Likert score 6.53). The majority of surgeons also thought that vertical instability precedes anterolateral lumbar instability (187/273; 68.5%; Likert score 6.64) and that a vacuum disc may cause vertical instability with symptomatic dynamic foraminal & lateral recess stenosis (222/273; 81%; Likert score 7.48), mechanical back pain (201/273; 73.1%; Likert score 7.48), and may cause sciatica-type low back and leg pain (179/273; 66.3%; Likert score 6.59). The majority of surgeons indicated that vacuum phenomenon on radiographic studies is associated with vertical instability and collapse resulting in dynamic foraminal and lateral recess stenosis and should be treated surgically (199/266; 73.7%; 7 missing responses; Likert score 6.86). Preferred treatments were decompression alone without fusion (P<0.014). There was consensus in support of fusion by TLIF or PLIF with a Likert score of 6.68 (184/266; 69.2%; 7 missing responses). There was no consensus on standalone fusion.
Conclusions
Vacuum phenomenon on radiographic studies is associated with a vertical instability and collapse, resulting in dynamic foraminal and lateral recess stenosis that should be treated surgically. Preferred surgical treatments were decompression alone, decompression with interbody fusion using just bone graft, and fusion employing TLIF or PLIF. Further research into the clinical significance of lumbar vacuum disc, vertical instability and its most appropriate surgical treatments if any is necessary.
Keywords: Vacuum disc, vertical instability, surgical treatment
Introduction
Minimally invasive spinal surgery techniques (MISST) and endoscopic spinal fusion techniques, in particular, have received some attention recently as a means to further simplify spinal surgery for patients and to facilitate their transition into outpatient ambulatory surgery center (ASC) setting (1-4). Various applications of endoscopic spinal surgery techniques in the delivery of interbody fusion cages in combination with percutaneous bilateral or unilateral pedicle screw constructs or as standalone endoscopic fusion have been demonstrated, proposed by different surgeons and stakeholders (4). The authors of this article were explicitly interested in better understanding the opinions of the surgeons surveyed. Some opinions reflect the use of fusion regarding indications and patient selection criteria for a standalone endoscopic decompression and interbody fusion surgery (5).
The well-accepted indications for open lumbar decompression and spinal fusion surgery include spondylolisthesis with motion on dynamic lateral extension-flexion views and decompression induced instability for severe spinal stenosis dictating aggressive resection of the posterior spinal elements. However, these traditional indications for open translaminar lumbar fusion surgery may not be ideal for the successful application of endoscopic spinal surgery techniques. While advances in endoscopic decompression technologies with motorized burrs and more effective larger-diameter endoscopic rongeurs equaling those used in open surgeries have certainly allowed expanding the indications of endoscopic surgery, treating patients with end-stage degenerative disc- and facet disease with associated severe central stenosis or greater than Grade I spondylolisthesis may be pushing the limits of endoscopic surgery. Instead, patients with less severe forms of spinal stenosis affecting predominately the lateral recess or the foramina are more likely to be chosen for the endoscopic decompression procedure. Many of these patients may be successfully treated in such a way with favorable long-term outcomes, even up to five years postoperatively (6). However, some patients—particularly those with end-stage lumbar disease and persistent or progressive postoperative vertical or anterolateral instability—may require additional surgeries for recurrent symptoms in spite of initial functional improvements. A vacuum phenomenon on preoperative imaging studies has been recognized as a radiographic sign of end-stage degenerative disc disease (7-23). It correlates with a dysfunctional delaminated, fissured, cavitated or entirely hollow lumbar intervertebral disc (17,19) often directly visualized during routine endoscopy (5).
The authors of this study stipulate that such a diseased lumbar intervertebral vacuum disc void of any structurally intact tissue is at the end of its biological life cycle and that treating it with a primary reconstructive interbody fusion procedure may deliver more reliable long-term functional outcome improvements in patients who suffer from it. A simplified standalone outpatient endoscopic lumbar interbody fusion procedure may be an elegant way to treat this group of patients in a more durable manner diminishing the overall utilization by avoiding costly aftercare and early repetitive revision surgeries. It is evident that such a clinical protocol calling for primary intervertebral height reconstruction by interbody fusion in cases of vacuum disc invites controversy and deserves further investigation before its implementation in routine practice. In this survey study, the authors attempted to vet the opinions of practicing spine surgeons about the significance of a vacuum disc and the concept of vertical instability. At the outset of this study, the authors intended to use this consensus-building opinion research in the value-based discussion of early and staged intervention of common painful lumbar degenerative conditions—a concept that is in direct competition with traditional spine care delivery models where escalating cost of treating the end-stage of lumbar spine disease may simply hamper its affordability unless rationed. Treatment for pain is complex and multifactorial. Pain is an end result of normal physiologic aging, and patients respond differently along with cultural differences.
Methods
The authors used an approach of soliciting responses to an online survey they had employed in other survey-based opinion research. The questionnaire was sent to prospective respondent surgeons by email, chat groups in social networks including Facebook, WeChat, WhatsApp, and LinkedIn. The survey was available online (www.typeform.com) and distributed via a link distributed through these social network media to surgeons worldwide. The details of the survey methodology have been described in detail elsewhere. Surgeons could answer the survey question on their computer, laptop, and any hand-held devices such as an iPad, or a cellular smartphone. Surgeons were asked to answer a variety of clinical questions by choosing their level of agreement on a Likert scale from 1 to 10—with 1 being equivalent to complete disagreement and 10 being equal to complete agreement (24-28). Several additional multiple-choice questions were also included. Responding spine surgeons were also asked to provide some demographic information including their gender, age, country of residence, practice setting, type, and extent of postgraduate residency and fellowship training, as well as the types of MISST surgeries they perform (Table 1). The survey questions and the results of their respective Likert-scale data analysis are listed in Tables 2-5. To improve survey completion rate and to minimize the impact of geographic bias the survey questions written by the team of authors and were translated into Mandarin by the second author (X Zhang), into Spanish by the third author (JF Ramírez León), and into Portuguese by the fourth author (PST de Carvalho). In other words, four versions of the survey were published and distributed to surgeons residing in the respective world regions. Responses were synthesized into one database for statistical analysis. Backend translation of the survey responses was not necessary since all responses were given by choosing a number on a Likert scale from 1 to 10 or by selecting one of several multiple-choice answers.
Table 1. Demographic data of responding spine surgeons.
| Survey question | Frequency, N=273 | Percent | Valid percent | Cumulative percent |
|---|---|---|---|---|
| Postgraduate training | ||||
| Missing responses | 127 | 46.5 | 46.5 | 46.5 |
| Neurosurgeon | 57 | 20.9 | 20.9 | 67.4 |
| Orthopaedic surgeon | 89 | 32.6 | 32.6 | 100.0 |
| Fellowship training | ||||
| Missing responses | 130 | 47.6 | 47.6 | 47.6 |
| Spine fellowship trained (6–12 months) | 143 | 52.4 | 52.4 | 100.0 |
| Employment setting | ||||
| Missing responses | 35 | 12.8 | 12.8 | 12.8 |
| Hospital employed | 139 | 50.9 | 50.9 | 63.7 |
| Private practice setting | 66 | 24.2 | 24.2 | 87.9 |
| University setting | 33 | 12.1 | 12.1 | 100.0 |
| Practice setting | ||||
| Missing responses | 206 | 75.5 | 75.5 | 75.5 |
| I prefer not to answer | 5 | 1.8 | 1.8 | 77.3 |
| Multispecialty group | 29 | 10.7 | 10.7 | 88.0 |
| Single specialty group | 33 | 12.0 | 12.0 | 100.0 |
| Number of surgeons in my group | ||||
| 1 | 20 | 7.3 | 7.3 | 7.3 |
| 2 | 49 | 17.9 | 17.9 | 25.3 |
| 3 | 33 | 12.1 | 12.1 | 37.4 |
| 4 | 25 | 9.2 | 9.2 | 46.5 |
| 5 | 26 | 9.5 | 9.5 | 56.0 |
| 6 | 24 | 8.8 | 8.8 | 64.8 |
| 7 | 13 | 4.8 | 4.8 | 69.6 |
| 8 | 14 | 5.1 | 5.1 | 74.7 |
| 9 | 10 | 3.7 | 3.7 | 78.4 |
| 10 | 59 | 21.6 | 21.6 | 100.0 |
| Respondent surgeons’ age | ||||
| 18 to 24 | 2 | .7 | .7 | .7 |
| 25 to 34 | 32 | 11.7 | 11.7 | 12.5 |
| 35 to 44 | 112 | 41.0 | 41.0 | 53.5 |
| 45 to 54 | 84 | 30.8 | 30.8 | 84.2 |
| 55 to 64 | 31 | 11.4 | 11.4 | 95.6 |
| 65 or older | 12 | 4.4 | 4.4 | 100.0 |
| Region | ||||
| China | 117 | 42.9 | 42.9 | 42.9 |
| Mexico | 36 | 13.2 | 13.2 | 56.0 |
| Colombia | 27 | 9.9 | 9.9 | 65.9 |
| Brazil | 26 | 9.5 | 9.5 | 75.5 |
| India | 13 | 4.8 | 4.8 | 80.2 |
| South Korea | 10 | 3.7 | 3.7 | 83.9 |
| United States of America | 10 | 3.7 | 3.7 | 87.5 |
| Argentina | 5 | 1.8 | 1.8 | 89.4 |
| Iran | 2 | 0.7 | 0.7 | 90.1 |
| Taiwan | 2 | 0.7 | 0.7 | 90.8 |
| United Kingdom | 2 | 0.7 | 0.7 | 91.6 |
| Other | 23 | 8.4 | 8.4 | 100.0 |
Table 2. Spine surgeons’ Familiarity with vacuum disc phenomenon and frequency of intraoperative observation.
1. How familiar are you with the concept of a “vacuum disc” as a sign of end-stage lumbar degenerative disc disease on a Likert scale 1–10?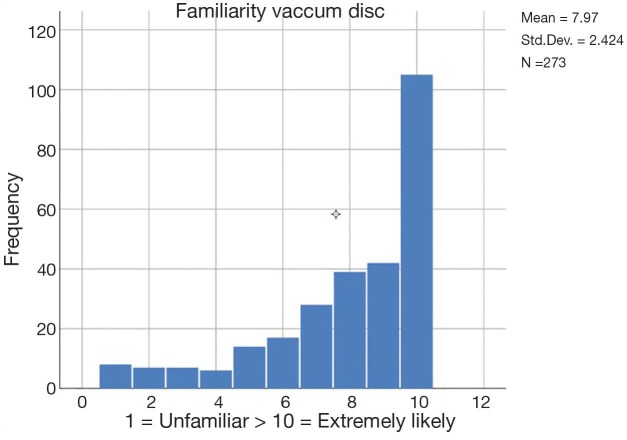
| |||
|---|---|---|---|
| 2. How often do you encounter a hollow disc during routine lumbar microdiscectomy? | |||
| 1. Never | |||
| 2. Occasionally (<25% of cases) | |||
| 3. Often (25%–75% of cases) | |||
| 4. Practically all the time (>75% of cases) | |||
| Response | Frequency | Percent | Cumulative percent |
| Never | 43 | 15.8 | 15.8 |
| < 25% | 187 | 68.5 | 84.2 |
| 25—75% | 42 | 15.4 | 99.6 |
| >75% | 1 | 0.4 | 100.0 |
| 273 | 100.0 | ||
3. How often do you find a vacuum disc shown below on intraoperative fluoroscopy during routine lumbar endoscopic transforaminal discectomy as a sign of endstage degenerative disc disease on a Likert scale 1–10?
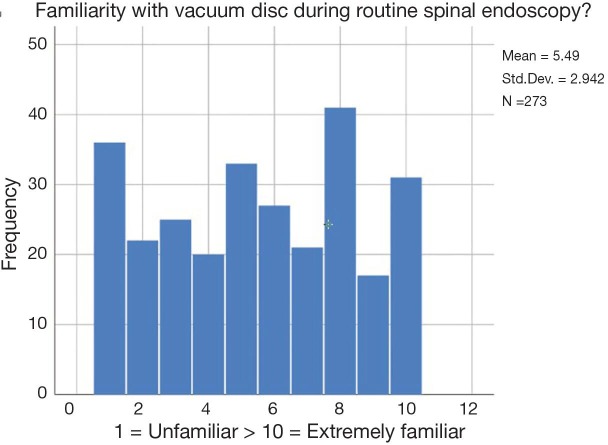
Table 3. Spine surgeons’ familiarity with vertical spinal instability concept.
1. How familiar are you with the concept of “vertical instability” being the result of degenerative disc disease and collapse of the lumbar motion segment causing sciatica-type back- and leg pain on a Likert scale from 1 to 10?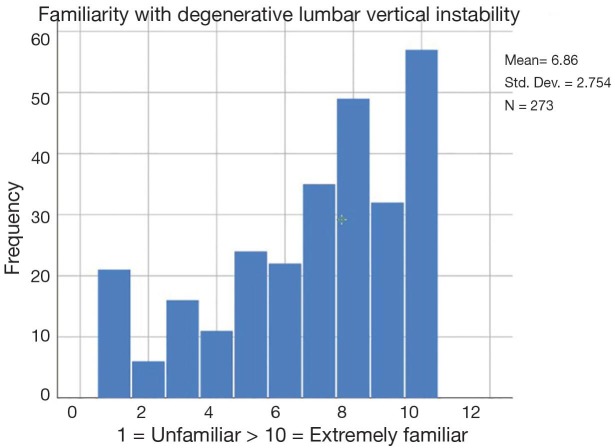
|
2. On a Likert scale from 1 to 10, how likely are you to agree with the statement that vertical instability is the result of a collapsing lumbar disc? 1–10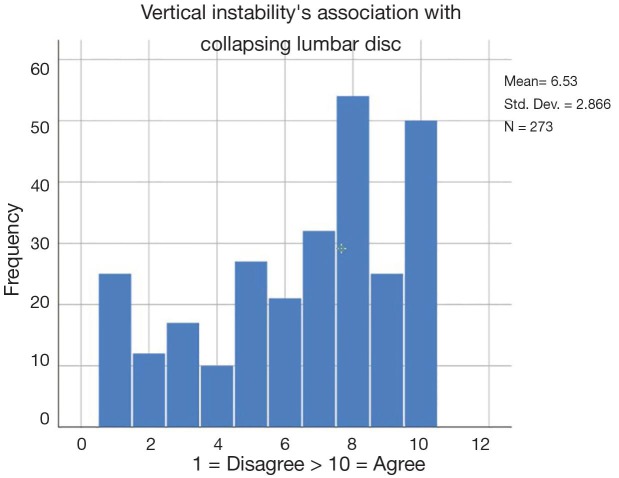
|
3. On a Likert scale from 1 to 10, how likely are you to agree vertical instability precedes anterolateral lumbar instability (degenerative spondylolisthesis)?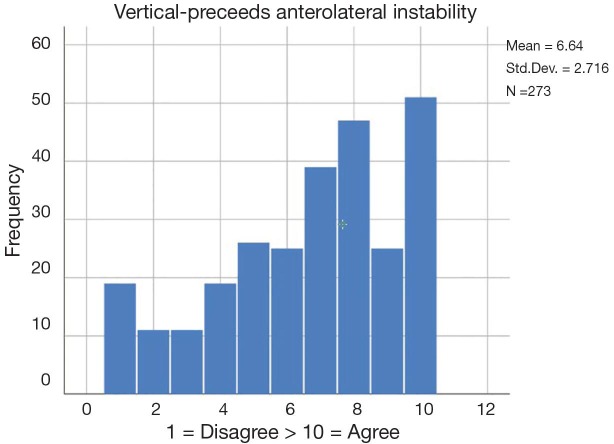
|
Table 4. Spine surgeons’ opinions on clinical relevance of lumbar vacuum disc.
1. On a Likert scale from 1 to 10, how likely are you to agree with that a vacuum disc may cause vertical instability with symptomatic dynamic foraminal & lateral recess stenosis?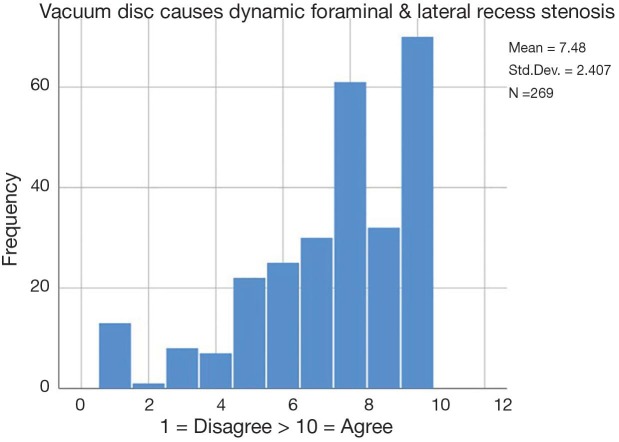
|
2. On a Likert scale from 1 to 10, how likely are you to agree with that a vacuum disc may cause mechanical back pain?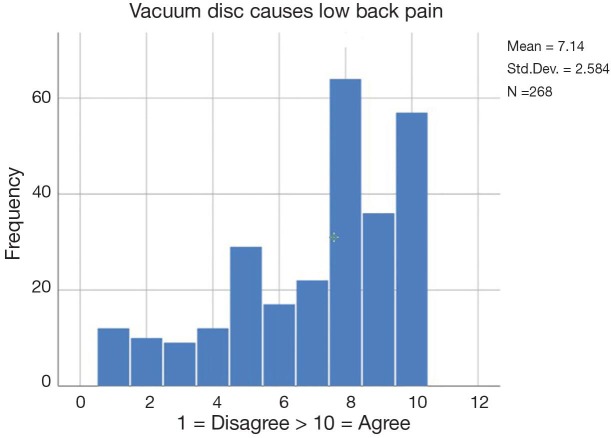
|
3. On a Likert scale from 1 to 10, how likely are you to agree with that a vacuum disc may cause sciatica-type low back and leg pain?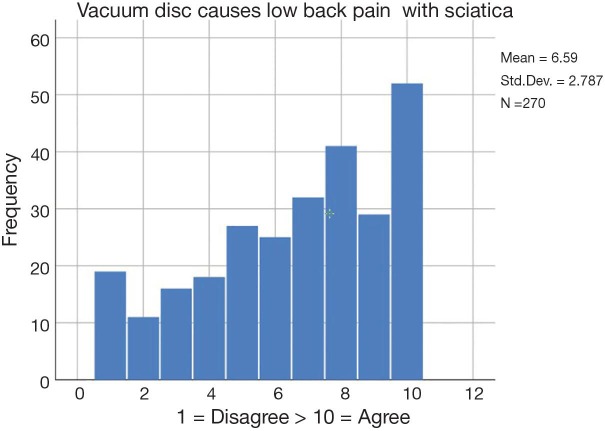
|
Table 5. Spine surgeons’ responses to diagnostic workup, and preferred treatment of lumbar vacuum disc on a Likert scale from 1 (least agreeable) to 10 (extremely agreeable) and annual surgical volume.
| Survey question | N | Range | Minimum | Maximum | Mean | Std. Dev |
|---|---|---|---|---|---|---|
| Diagnostic workup of vacuum disc | ||||||
| Preoperative MRI or CT may fail to demonstrate vacuum disc? | 270 | 10 | 0 | 10 | 5.35 | 3.472 |
| Does MRI underestimate vacuum disc? | 269 | 10 | 0 | 10 | 6.93 | 2.835 |
| How would you treat vacuum disc? | ||||||
| Pain management | 261 | 9 | 1 | 10 | 6.55 | 2.504 |
| Epidural steroid Injections | 265 | 9 | 1 | 10 | 5.32 | 2.858 |
| Surgical management | 266 | 9 | 1 | 10 | 6.86 | 2.621 |
| Regenerative treatment | 261 | 9 | 1 | 10 | 3.08 | 2.472 |
| Intradiscal therapy | 265 | 10 | 0 | 10 | 4.78 | 3.125 |
| Soft interbody fusion with bone graft only | 258 | 9 | 1 | 10 | 3.55 | 2.820 |
| Decompression only | 270 | 10 | 0 | 10 | 5.34 | 3.602 |
| Standalone interbody fusion | 264 | 9 | 1 | 10 | 5.28 | 3.130 |
| Standalone ALIF | 263 | 10 | 0 | 10 | 4.20 | 3.346 |
| TLIF or PLIF with interbody cages and pedicle screws | 266 | 9 | 1 | 10 | 6.68 | 2.942 |
| Do you observe inferior outcomes with vacuum disc? | 262 | 10 | 0 | 10 | 5.29 | 3.054 |
| Respondents’ annual surgical volume | ||||||
| How many discectomies do you perform annually? | 249 | 800 | 0 | 800 | 112.44 | 136.378 |
| How many fusions do you perform annually? | 247 | 600 | 0 | 600 | 61.69 | 79.552 |
| Valid N (listwise) | 207 | |||||
ALIF, anterior lumbar interbody fusion; TLIF, transforaminal lumbar interbody fusion; PLIF, posterior lumbar interbody fusion.
The survey ran from November 25, 2018, to May 27, 2019. The authors were blinded as to the identity of the responding surgeon at all times. Individual personal identifiers were not recorded. The typeform.com survey created a time-stamp upon initiation of the study, and once the completed questionnaire was submitted. Also, a unique network identifier (ID without IP address) was recorded for each responding surgeon. Upon completion of the survey, the responses were downloaded in an Excel file format and imported into IBM SPSS (version 25) statistical software package for further data analysis. Descriptive statistic measures were used to count responses and calculate the mean, range, and standard deviation as well as percentages. Missing responses were included for accurate percentage calculation and are listed at the top of each data table. Wherever applicable, a P value of 0.05 or less was considered statistically significant, and a confidence interval of 95% was employed for all statistical tests. The Likert scale responses from spine surgeons were analyzed as numerical variables. The authors also used linear regression and kappa analysis of agreement in an attempt to measure the presumed consistency of the submitted responses in real-time as they came in because of unknown sample size required to have sufficient power for clinically meaningful statistical analysis.
Results
One thousand one hundred seventy-nine surgeons accessed the online survey during a total of 1,596 visits to the typeform.com web site. Of the 1,179 spine surgeons who were directed to the survey, 273 submitted a valid survey recording. Thus, the completion rate was 22.78%, and the average time to complete the survey was 16:21 minutes. The demographics of the responding surgeon is shown in Table 1. Of the 273 respondents, 20.9% indicated that they were neurosurgeons, 32.6% designated that they were orthopedic surgeons, and 52.4% had completed a spine fellowship. There were no statistically significant differences in the response rates between neuro- or orthopaedic spine surgeons regardless of fellowship training. Therefore, responses are reported for the group as a whole. Forty-one percent of responding surgeons were between the ages of 35 to 44, and another 30.8% between the ages of 45 to 54 years. When asked about their practice setting, 50.9% indicated that they were hospital employed. Another 24.2% were in a private practice setting, and 12.1% were working at a university. The respondent surgeons worked at nearly equal portions in a single- versus a multispecialty group with the majority of surgeons being in a larger group of 10 surgeons, or in a small group with another physician (17.9%), or two other surgeons (12.1%). The majority of responding spine surgeons were residing in China (42.9%). The remaining responding spine surgeon in descending order were from Mexico (13.2%), Colombia (9.9%), Brazil (9.5%), India (4.5%), South Korea (3.7%), USA (3.7%), Argentina (1.8%), Iran (0.7%), Taiwan (0.7%), United Kingdom (0.7%), and other areas (8.4%). Surgeons from China exclusively used their smartphone when answering the online survey. Surgeons from all other parts of the world used a computer or tablet at a much higher rate of nearly equal portions. The survey completion rate was more than twice higher when surgeons used a computer rather than their smartphone. There was no statistically discernable difference in impact of practice setting, or country of residence.
The vast majority of responding spine surgeons were very familiar with the concept of a “vacuum disc” as a sign of end-stage lumbar degenerative disc disease (question 1; Table 2) with an average Likert score of 7.97. Also, the majority of surgeons indicated that they have encountered a hollow structurally incompetent disc during routine lumbar microdiscectomy with 68.5% of respondents declaring having encountered it in up to 25% of their cases, and another 15.4% admitting to having found it in 25% to 75% of cases (question 2, Table 2). Over half (137/273; 50.2%) of the responding surgeons had found a hollow vacuum disc during routine endoscopic discectomy surgery and validated its existence by direct endoscopic visualization (question 3; Table 2). The reported Likert score of 5.49 reflects the 49.2% of responding surgeon who did not perform endoscopic spine surgery (question 3; Table 3). The concept of “vertical instability” as a result of progressive degenerative disc disease and collapse of the lumbar motion segment causing sciatica-type back- and leg pain was very familiar to the majority of surgeons (139/273; 71.4%; Likert score 6.86; question 1; Table 3). A similar majority of surgeons thought that vertical instability is a result of a collapsing lumbar motion segment (182/273; 66.7%; Likert score 6.53; question 2; Table 3). The majority of surgeons also thought that vertical instability precedes anterolateral lumbar instability (187/273; 68.5%; Likert score 6.64; question 3; Table 3) and that a vacuum disc may cause vertical instability with symptomatic dynamic foraminal & lateral recess stenosis (222/273; 81%; Likert score 7.48; question 1; Table 4), mechanical back pain (201/273; 73.1%; Likert score 7.48; question 2; Table 4), and may cause sciatica-type low back and leg pain (179/273; 66.3%; Likert score 6.59; question 3; Table 4).
Spine surgeons’ responses regarding the diagnostic workup, and preferred treatment of lumbar vacuum disc on a Likert scale from 1 (least agreeable) to 10 (Extremely agreeable) and in relation their annual surgical volume are listed in Table 5. While surgeons where undecided one way or the other whether a preoperative MRI or CT scan may fail to demonstrate a vacuum disc, they agreed overwhelmingly with the statement that such advanced imaging studies underestimate the presence of a vacuum disc pain (199/273; 74%; Likert score 6.93; Table 5). This was statistically significant for surgeons who also believed that a vacuum disc is associated with dynamic foraminal and lateral recess stenosis, and for surgeons who thought that vertical instability precedes anterolateral instability (two-tailed independent t-test; P=0.003 for both tests assuming unequal variances). These surgeons were also convinced that presence of a vacuum disc is associated with inferior clinical outcomes regardless of treatment (P<0.022; two-tailed independent t-test assuming unequal variances). When asked how to treat patients with symptomatic vacuum disc, surgeons were in favor of pain management (177/261; 65.9%; 12 missing responses; Likert score 6.55; Table 5; not statistically significant) and surgical treatment (199/266; 73.7%; 7 missing responses; Likert score 6.86; Table 5) if surgeons were of the opinions that a vacuum disc is associated with vertical instability (P=0.15; two-tailed independent t-test assuming unequal variances) or causes dynamic foraminal or lateral recess stenosis instability (P=0.003; two-tailed independent t-test assuming unequal variances). Preferred surgical treatments reported by responding surgeons who were familiar with the vacuum disc phenomenon or had encountered hollow disc during endoscopic surgery were decompression alone without fusion (P<0.014; two-tailed independent t-test assuming unequal variances). Soft interbody with bone graft only without the use of an interbody fusion cage was preferred by surgeons who opined that vertical instability precedes anterolateral instability (P<0.007; two-tailed independent t-test assuming unequal variances). Transforaminal lumbar interbody (TLIF) or and posterior lumbar interbody fusion (PLIF) with a Likert score of 6.68 (184/266; 69.2%; 7 missing responses; Likert score 6.86; Table 5) was recommended by surgeons who believed that vertical instability causes collapse of the lumbar intervertebral disc. However, this did not achieve statistical significance level (P=0.08; two-tailed independent t-test assuming unequal variances). Surgeons reported their surgical average annual volume as 122.34±136.38 discectomies and 61.69±79.55.
Discussion
Endoscopic fusion procedures are on the horizon (5,29-34), and the debate on its appropriate clinical indications and patient selection criteria will likely intensify as more instrumentation sets and implants are hitting the market. The authors of this study solicited responses to an online survey from spine surgeons as to the clinical relevance of radiographic evidence of a vacuum phenomenon and endoscopically visualized hollow disc devoid of any structural tissue able to resist vertical collapse which presumably results in vertical instability with dynamic foraminal and lateral recess stenosis. These were the concepts tested in this opinion-based research study in an attempt to build consensus on the basis of the extensive clinical experience of the respondents many of whom indicated that they are at the pinnacles of their careers between the ages of 35 and 55 working in busy private practice (24.2%) or hospital setting (50.9%). Only a minority of surgeons worked in a university setting (12.1%). Many surgeons indicated that they had busy clinical practice with the majority of them performing several hundred discectomies and fusion surgeries per year with the most active surgeons reporting that they performed a staggering annual number of 800 discectomies or 600 fusions.
What became clear from this survey is that most surgeons believed that a vacuum phenomenon on radiographic studies is associated with a vertical instability and collapse resulting in dynamic foraminal and lateral recess stenosis that should be treated surgically (35). Responses supporting these conclusions had statistically significantly higher Likert scores for decompression surgery (P<0.014), and fusion—regardless of whether TLIF or PLIF—surgery (P=0.08). The majority of surgeons did concur that leaving a vertically unstable disc untreated or performing a decompression alone is associated with inferior clinical outcomes. Responding surgeons considered performing an un-instrumented interbody fusion for vertical instability with just bone graft as a reasonable surgical option (P<0.007). It had a higher Likert score than performing an instrumented standalone interbody fusion using a cage for which surgeons were undecided. The authors of this survey study concluded that the concept of a standalone interbody fusion without posterior supplemental pedicle screw instrumentation might currently still be too far out of the mainstream to be considered a reasonable treatment even though standalone expandable lumbar interbody fusion cages have received approval by the Food and Drug Administration.
While it is evident that opinion surveys cannot replace actual clinical trials to prove up new clinical protocols, they have been considered a powerful tool to size-up support amongst surgeons for new procedures and implants and to identify areas of improvements likely to translate into a clinical benefit to patients. One such technology is endoscopic spinal surgery which has gained significant traction recently because of its minimally invasive nature, but also in part because it has been recognized as a platform for innovative surgical pain management and reconstructive procedures—standalone endoscopic decompression and fusion being one such example (1,2,5,33,36). The proof of concept has been demonstrated in recent clinical studies with the Lordotic Endoscopic Wedge Lumbar Interbody Fusion (5) (LEW-LIF™)—some of which have been published in this special focus issue on staged management of common lumbar pain generators. The LEW-LIF™ procedure is not only attractive because of its simplicity, but also for its consideration of patient-specific factors during the interbody height restoration surgery thereby reliably eliminating vertical instability and dynamic stenosis related recurrent symptom (5). This team of authors expects that an outpatient standalone endoscopic fusion substantially improves the durability of the endoscopic decompression procedure by providing long-lasting pain relief without the need for costly and repetitive cycles of medical and other supportive care measures, pain management, or revision surgeries. In spite of its limitations discussed below, this survey study amongst spine surgeons confronting these issues in their day-to-day practice certainly highlight the need for further research into the clinical significance of vertical instability and its most appropriate surgical treatments but also put the magnifying glass on the areas of controversies that will need to substantiated with high-grade clinical evidence to win the evolving medical necessity debate with payers, and governmental review boards alike. When it comes right down to it, this team of authors is looking to replace some of the traditional open translaminar surgeries, with more cost-effective and more reliable procedures. Of course, this burden of proof lies with those pioneers who decide to venture into this unchartered territory.
The survey was distributed via email and social media and had apparent limitations. Average response rates have been reported for an in-person survey at 57%, mail survey at 50%, email survey at 30%, online survey at 29%, telephone survey at 18%, an in-app study of 13%, with an overall average survey response rate of 33% (37-43). Clinical examples include a postal questionnaire sent to 2,048 prospective respondents with a response rate of 46% (44). Another web-based 59-items survey with 260 respondents had a response rate of 60% (45), and a written paper survey reported a response rate of 49.5% (302/610) (46). An online patient satisfaction survey in 9,975 Medicare beneficiaries with 434 unduplicated survey submissions had a response rate of 4.3% (47). These examples illustrate that there can be a wide range of survey response rates. The response rate of 22.78% obtained in this study seems low at first glance. However, this survey study still was able to discern statistically significant differences in response rates by respondents considering the high number of participating surgeons. After all, 1,179 spine surgeons were attempting to complete the survey. Ultimately, 273 of them were able to finish it and submit a complete recording. Whether or not the high usage of smartphones over computers or laptops harmed the overall response rate was beyond the authors’ abilities to analyze the data. In fact, responses were blinded, and the team of authors had no information as to the identity of the responding spine surgeons, hence, minimizing the impact of intuition and hindsight bias amongst the investigators. The effect of non-response bias due to the low response rate may improve survey accuracy and therefore was less problematic to this team of authors. Non-response bias has been recognized as an indicator of survey quality. Although lower response rates in the 20% range have been related to more accurate measurements than surveys with 60% to 70% response rates which are still considered preferable since the missing data is not random (48). Additional limitations may have arisen from geographic bias where the digital communication used in this survey study could have obliterated existing geographic diversity and various cultural perspectives of responding spine surgeons. The lack of statistical differences in response rates concerning the country of origin suggests a negligible impact of geographic bias factors. However, the authors had no way to exclude this scenario. Therefore, the authors were cautious not to generalize the findings of this survey in the context of their preconceived notions of vacuum disc phenomenon and vertical instability to counter the homogenizing effect of the digital data acquisition across multiple cultural boundaries while recognizing its limitations in the quest for genuinely alternative insights by other surgeons. To minimize the potentially distorting effects of such geographic biases, this international team of authors worked closely together on writing the survey in Mandarin, Spanish, Portuguese, as well as in English. The survey data analysis and interpretation took the cultural diversities among respondents into account.
This survey study amongst busy practicing spine surgeons on the clinical significance of vacuum disc and vertical instability was blinded, which minimized the impact of intuition and hindsight bias amongst the investigators. After all, the study investigators did not know the distribution of responses and which underlying trends would emerge when the survey launched. Hence, it was unclear at the outset of the online data acquisition when sufficient statistical sample size would have been achieved to close the survey. Linear regression monitoring of the change in response rates to the questions over time and kappa analysis of agreement in the 273 survey submissions showed a relatively stable distribution of asymmetric variances suggesting that similar percentage response rates could have been reasonably expected with a higher response rate. Therefore, the authors of this simply imply that results presented herein are in fact, representative of current opinions of spine surgeons and spine practitioners with various backgrounds regarding vacuum disc, vertical instability, and preferred treatments.
Conclusions
This online survey reached 273 spine surgeons. The majority of them believed that a vacuum phenomenon on radiographic studies is associated with a vertical instability and collapse resulting in dynamic foraminal and lateral recess stenosis that should be treated surgically. Statistical analysis using a p-value of 0.05 as a cut-off number show that preferred surgical treatments were decompression alone, decompression with interbody fusion using just bone graft, and fusion employing TLIF or PLIF. This survey reflects on the opinions of surgeons with various backgrounds with skewed views on opinions of stakeholders focused on decompression and fusion techniques as a solution for a normal aging condition that is dependent on individual patient needs. Treatment for pain covers a broad spectrum of indications, including just treating the pain generators in a staged manner.
Acknowledgments
None.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Disclaimer: The views expressed in this editorial represent those of the authors and no other entity or organization.
Footnotes
Conflicts of Interest: Jorge Felipe Ramírez León is shareholder & President of Board of Directors Ortomac, Colombia, consultant Elliquence, USA. The senior author designed and trademarked his inside-out YESS™ technique and receives royalties from the sale of his inventions. Indirect conflicts of interest (honoraria, consultancies to sponsoring organizations are donated to IITS.org, a 501c 3 organization). Other authors have no conflicts of interest to declare.
References
- 1.Liu C, Zhou Y. Comparison Between Percutaneous Endoscopic Lumbar Discectomy and Minimally Invasive Transforaminal Lumbar Interbody Fusion for Lumbar Disc Herniation with Biradicular Symptoms. World Neurosurg 2018;120:e72-9. 10.1016/j.wneu.2018.07.146 [DOI] [PubMed] [Google Scholar]
- 2.Kim JE, Choi DJ. Biportal Endoscopic Transforaminal Lumbar Interbody Fusion with Arthroscopy. Clin Orthop Surg 2018;10:248-52. 10.4055/cios.2018.10.2.248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu C, Zhou Y. Percutaneous Endoscopic Lumbar Diskectomy and Minimally Invasive Transforaminal Lumbar Interbody Fusion for Recurrent Lumbar Disk Herniation. World Neurosurg 2017;98:14-20. 10.1016/j.wneu.2016.10.056 [DOI] [PubMed] [Google Scholar]
- 4.Lee SH, Erken HY, Bae J. Percutaneous Transforaminal Endoscopic Lumbar Interbody Fusion: Clinical and Radiological Results of Mean 46-Month Follow-Up. Biomed Res Int 2017;2017:3731983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lewandrowski KU, Ransom NA, Ramirez Leon JF, et al. The Concept for A Standalone Lordotic Endoscopic Wedge Lumbar Interbody Fusion: The LEW-LIF. Neurospine 2019;16:82-95. 10.14245/ns.1938046.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yeung A, Roberts A, Zhu L, et al. Treatment of Soft Tissue and Bony Spinal Stenosis by a Visualized Endoscopic Transforaminal Technique Under Local Anesthesia. Neurospine 2019;16:52-62. 10.14245/ns.1938038.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Murata K, Akeda K, Takegami N, et al. Morphology of intervertebral disc ruptures evaluated by vacuum phenomenon using multi-detector computed tomography: association with lumbar disc degeneration and canal stenosis. BMC Musculoskelet Disord 2018;19:164. 10.1186/s12891-018-2086-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Viswanathan VK, Subramanian S. Letter: Comparison of Posterior Lumbar Interbody Fusion and Posterolateral Lumbar Fusion in Monosegmental Vacuum Phenomenon within an Intervertebral Disc. Asian Spine J 2016;10:982-3. 10.4184/asj.2016.10.5.982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.An KC, Kong GM, Park DH, et al. Response to: Comparison of Posterior Lumbar Interbody Fusion and Posterolateral Lumbar Fusion in Monosegmental Vacuum Phenomenon within an Intervertebral Disc. Asian Spine J 2016;10:984. 10.4184/asj.2016.10.5.984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.An KC, Kong GM, Park DH, et al. Comparison of Posterior Lumbar Interbody Fusion and Posterolateral Lumbar Fusion in Monosegmental Vacuum Phenomenon within an Intervertebral Disc. Asian Spine J 2016;10:93-8. 10.4184/asj.2016.10.1.93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Murata Y, Kanaya K, Wada H, et al. L5 Radiculopathy due to Foraminal Stenosis Accompanied With Vacuum Phenomena of the L5/S Disc on Radiography Images in Extension Position. Spine (Phila Pa 1976) 2015;40:1831-5. 10.1097/BRS.0000000000001067 [DOI] [PubMed] [Google Scholar]
- 12.Söffler C, Karpenstein H, Kramer M. The intervertebral vacuum phenomenon as a computed-tomographic finding in the dog and its significance as an indicator for surgical treatment of vertebral disc herniations. Tierarztl Prax Ausg K Kleintiere Heimtiere 2014;42:88-93. [PubMed] [Google Scholar]
- 13.Lin TY, Liao JC, Tsai TT, et al. The effects of anterior vacuum disc on surgical outcomes of degenerative versus spondylolytic spondylolisthesis: at a minimum two-year follow-up. BMC Musculoskelet Disord 2014;15:329. 10.1186/1471-2474-15-329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liao JC, Lu ML, Niu CC, et al. Surgical outcomes of degenerative lumbar spondylolisthesis with anterior vacuum disc: can the intervertebral cage overcome intradiscal vacuum phenomenon and enhance posterolateral fusion? J Orthop Sci 2014;19:851-9. 10.1007/s00776-014-0618-z [DOI] [PubMed] [Google Scholar]
- 15.Lee CH, Cho JH, Hyun SJ, et al. Symptomatic gas-containing herniated disc with the vacuum phenomenon: mechanism and treatment. Case report. Neurol Med Chir (Tokyo) 2012;52:106-8. 10.2176/nmc.52.106 [DOI] [PubMed] [Google Scholar]
- 16.Pak KI, Hoffman DC, Herzog RJ, et al. Percutaneous intradiscal aspiration of a lumbar vacuum disc herniation: a case report. HSS J 2011;7:89-93. 10.1007/s11420-010-9168-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schweitzer ME, el-Noueam KI. Vacuum disc: frequency of high signal intensity on T2-weighted MR images. Skeletal Radiol 1998;27:83-6. 10.1007/s002560050342 [DOI] [PubMed] [Google Scholar]
- 18.Latif AB. Vacuum phenomenon in the intervertebral disc. Magy Traumatol Orthop Helyreallito Seb 1991;34:297-300. [PubMed] [Google Scholar]
- 19.Anda S, Stovring J, Ro M. CT of extraforaminal disc herniation with associated vacuum phenomenon. Neuroradiology 1988;30:76-7. 10.1007/BF00341949 [DOI] [PubMed] [Google Scholar]
- 20.Anda S, Dale LG, Vassal J. Intradural disc herniation with vacuum phenomenon: CT diagnosis. Neuroradiology 1987;29:407. 10.1007/BF00348927 [DOI] [PubMed] [Google Scholar]
- 21.Chevrot A, Pillon B, Revel M, et al. The radiological phenomenon of lumbar vacuum-disc (author's transl). J Radiol Electrol Med Nucl 1978;59:267-70. [PubMed] [Google Scholar]
- 22.Ford LT, Gilula LA, Murphy WA, et al. Analysis of gas in vacuum lumbar disc. AJR Am J Roentgenol 1977;128:1056-7. 10.2214/ajr.128.6.1056 [DOI] [PubMed] [Google Scholar]
- 23.Raines JR. Intervertebral disc fissures (vacuum intervertebral disc). Am J Roentgenol Radium Ther Nucl Med 1953;70:964-6. [PubMed] [Google Scholar]
- 24.Koksel Y, Gencturk M, Spano A, et al. Utility of Likert scale (Deauville criteria) in assessment of Chemoradiotherapy response of primary oropharyngeal squamous cell Cancer site. Clin Imaging 2019;55:89-94. 10.1016/j.clinimag.2019.01.007 [DOI] [PubMed] [Google Scholar]
- 25.Krzych ŁJ, Lach M, Joniec M, et al. The Likert scale is a powerful tool for quality of life assessment among patients after minimally invasive coronary surgery. Kardiochir Torakochirurgia Pol 2018;15:130-4. 10.5114/kitp.2018.76480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Costa DN, Passoni NM, Leyendecker JR, et al. Diagnostic Utility of a Likert Scale Versus Qualitative Descriptors and Length of Capsular Contact for Determining Extraprostatic Tumor Extension at Multiparametric Prostate MRI. AJR Am J Roentgenol 2018;210:1066-72. 10.2214/AJR.17.18849 [DOI] [PubMed] [Google Scholar]
- 27.Reed CC, Wolf WA, Cotton CC, et al. A visual analogue scale and a Likert scale are simple and responsive tools for assessing dysphagia in eosinophilic oesophagitis. Aliment Pharmacol Ther 2017;45:1443-8. 10.1111/apt.14061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wadgave U, Khairnar MR. Parametric tests for Likert scale: For and against. Asian J Psychiatr 2016;24:67-8. 10.1016/j.ajp.2016.08.016 [DOI] [PubMed] [Google Scholar]
- 29.Yang JC. Current problems and challenges for percutaneous endoscopic transforaminal lumbar interbody fusion. Zhonghua Yi Xue Za Zhi 2019;99:2566-8. [DOI] [PubMed] [Google Scholar]
- 30.Qiao G, Feng M, Wang X, et al. Revision for endoscopic discectomy: Is lateral lumbar interbody fusion an option? World Neurosurg 2019. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 31.Park MK, Park SA, Son SK, et al. Correction to: Clinical and radiological outcomes of unilateral biportal endoscopic lumbar interbody fusion (ULIF) compared with conventional posterior lumbar interbody fusion (PLIF): 1-year follow-up. Neurosurg Rev 2019;42:763. 10.1007/s10143-019-01131-2 [DOI] [PubMed] [Google Scholar]
- 32.Park MK, Park SA, Son SK, et al. Clinical and radiological outcomes of unilateral biportal endoscopic lumbar interbody fusion (ULIF) compared with conventional posterior lumbar interbody fusion (PLIF): 1-year follow-up. Neurosurg Rev 2019;42:753-61. 10.1007/s10143-019-01114-3 [DOI] [PubMed] [Google Scholar]
- 33.Ahn Y, Youn MS, Heo DH. Endoscopic transforaminal lumbar interbody fusion: a comprehensive review. Expert Rev Med Devices 2019;16:373-80. 10.1080/17434440.2019.1610388 [DOI] [PubMed] [Google Scholar]
- 34.Yang J, Liu C, Hai Y, et al. Percutaneous Endoscopic Transforaminal Lumbar Interbody Fusion for the Treatment of Lumbar Spinal Stenosis: Preliminary Report of Seven Cases with 12-Month Follow-Up. Biomed Res Int 2019;2019:3091459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Luk KD, Chow DH, Holmes A. Vertical instability in spondylolisthesis: a traction radiographic assessment technique and the principle of management. Spine (Phila Pa 1976) 2003;28:819-27. 10.1097/01.BRS.0000058941.55208.14 [DOI] [PubMed] [Google Scholar]
- 36.Ling Q, He E, Zhang H, et al. A novel narrow surface cage for full endoscopic oblique lateral lumbar interbody fusion: A finite element study. J Orthop Sci 2019;24:991-8. 10.1016/j.jos.2019.08.013 [DOI] [PubMed] [Google Scholar]
- 37.Millar MM. Improving Response to Web and Mixed-Mode Surveys. Available online: https://www.academic.oup.com/poq/article/75/2/249/1860211.
- 38.Mind-blowing Employee Survey Statistic. Available online: http://www.officevibe.com/blog/employee-surveys-infographic.
- 39.Mobile Survey Response Rates: Averages and Benchmarks by App Category [Available from: http://www.apptentive.com/blog/2016/10/04/mobile-survey-response-rates/.
- 40.What is an acceptable survey response rate? Available online: http://socialnorms.org/what-is-an-acceptable-survey-response-rate/.
- 41.The Complete Guide to Acceptable Survey Response Rates. Available online: https://www.genroe.com/blog/acceptable-survey-response-rate-2/11504.
- 42.What Low Response Rates Mean for Telephone Surveys. Available online: http://www.pewresearch.org/2017/05/15/what-low-response-rates-mean-for-telephone-surveys/.
- 43.What Does It Really Take To Build A 7-Figure Business?˜ Available online: https://www.fieldboom.com/blog/survey-response-rate/.
- 44.Todd AL, Porter M, Williamson JL, et al. Pre-notification letter type and response rate to a postal survey among women who have recently given birth. BMC Med Res Methodol 2015;15:104. 10.1186/s12874-015-0097-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Odgaard L, Kothari M. Survey of oral nursing care attitudes, knowledge and practices in a neurorehabilitation setting. J Oral Rehabil 2019;46:730-7. [DOI] [PubMed] [Google Scholar]
- 46.Dombrecht L, Deliens L, Chambaere K, et al. NICU consortium Neonatologists and neonatal nurses have positive attitudes towards perinatal end-of-life decisions, a nationwide survey. Acta Paediatr 2019. doi: . 10.1111/apa.14797 [DOI] [PubMed] [Google Scholar]
- 47.Brandt NJ, Cooke CE, Sharma K, et al. Findings from a National Survey of Medicare Beneficiary Perspectives on the Medicare Part D Medication Therapy Management Standardized Format. J Manag Care Spec Pharm 2019;25:366-91. 10.18553/jmcp.2019.25.3.366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang J, Alotaibi NM, Ibrahim GM, et al. The Spectrum of Altmetrics in Neurosurgery: The Top 100 "Trending" Articles in Neurosurgical Journals. World Neurosurg 2017;103:883-95.e1. 10.1016/j.wneu.2017.04.157 [DOI] [PubMed] [Google Scholar]


