Abstract
Background
Hydrotubation with oil‐soluble contrast media for unexplained infertility and adhesiolysis for infertility due to peritubal adhesions are primary procedures that are of recognised benefit. It is less clear whether postoperative procedures such as hydrotubation or second‐look laparoscopy with adhesiolysis are beneficial following pelvic reproductive surgery.
Objectives
To assess the value of postoperative hydrotubation and second‐look laparoscopy with adhesiolysis following female pelvic reproductive surgery.
Search methods
We searched the Cochrane Menstrual Disorders and Subfertility Group Specialised Register (August 2008), Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2007, Issue 2), MEDLINE (1966 to August 2008), EMBASE (1980 to August 2008), PsycINFO (1967 to August 2008), Current Contents (1993 to August 2008), Biological Abstracts (1969 to August 2008), CINAHL (1982 to August 2008) and reference lists of identified articles.
Selection criteria
All randomised controlled trials in which a postoperative procedure was compared with a control group following pelvic reproductive surgery were considered for inclusion in the review.
Data collection and analysis
Five randomised controlled trials were identified and included in this updated review. An attempt was made to obtain further information from the authors of all five trials. All trials were assessed for quality. The studied outcomes were pregnancy, live birth, ectopic pregnancy and miscarriage rates, and the rates of tubal patency and procedure‐related complications. Review authors extracted the data independently and the odds ratios (OR) were estimated for these dichotomous outcomes.
Main results
Five randomised controlled trials were identified and included in this review. The odds of pregnancy (OR 1.12, 95% confidence interval (CI) 0.57 to 2.21) and live birth (OR 0.61, 95% CI 0.24 to 1.59) were not significantly different with postoperative hydrotubation versus no hydrotubation. The odds of pregnancy (OR 0.96, 95% CI 0.44 to 2.07) or live birth (OR 0.67, 95% CI 0.19 to 2.32) were also not significantly different with second‐look laparoscopy and adhesiolysis versus no second‐look laparoscopy. Whether hydrotubation was early or late and whether hydrotubation fluid contained steroid or not had no significant impact on the odds of pregnancy or live birth. Late antibiotic hydrotubation increased the odds of at least one patent fallopian tube when compared with early hydrotubation in women (OR 7.72, 95% CI 2.50 to 8.93). The odds of infective morbidity significantly increased with early hydrotubation when compared with late non‐antibiotic hydrotubation (OR 4.72, 95% CI 2.50 to 8.93). When comparing late hydrotubation following tubal stent removal with early hydrotubation in women who had no tubal stenting, there was no significant difference in pregnancy or live birth rates.
Authors' conclusions
There is insufficient evidence to support the routine practice of hydrotubation or second‐look laparoscopy following female pelvic reproductive surgery. The studies on which this conclusion is based were either of poor quality or underpowered. These interventions should be performed in the context of a good quality, adequately powered randomised controlled trial. Postoperative hydrotubation with fluid containing antibiotic may offer benefit over hydrotubation fluid without antibiotic following tubal surgery. A randomised controlled trial of postoperative hydrotubation with antibiotic‐containing fluid versus no hydrotubation for improving fertility following tubal surgery is justified.
Plain language summary
Postoperative procedures for improving fertility following pelvic reproductive surgery
There is insufficient evidence to show the benefit or harm of routine hydrotubation or second‐look laparoscopy following surgery on a woman's reproductive system. Surgery to correct tubal damage is undertaken to improve pregnancy and live birth rates. Laparoscopy (where the abdominal organs are examined through a small surgical cut in the abdomen) to treat postoperative adhesions and postoperative hydrotubation (flushing out of the fallopian tubes) have been used to improve the results of tubal surgery. The review of trials found there is insufficient evidence to support the routine practice of hydrotubation or this second‐look laparoscopy after pelvic reproductive surgery. More research is needed.
Background
Description of the condition
Pelvic reproductive surgery may be defined as surgery on the pelvis that is intended to improve fertility. It may include surgery on the uterus, ovaries, pelvic peritoneum (in the case of endometriosis), and most commonly the fallopian tubes. A variety of procedures are collectively known as tubal surgery. Salpingo‐ovariolysis is division of adhesions involving the fallopian tube and ovary; salpingostomy is the refashioning of a distal tubal ostium for distal tubal occlusion, and is designed to keep the fallopian tube open; tubal reanastomosis is the rejoining of fallopian tubes, typically performed for reversal of sterilisation; cornual anastomosis and utero‐tubal implantation are recognised surgical treatments for cornual occlusion. Whilst surgery on the fallopian tubes has been performed less frequently since the advent of in vitro fertilisation (Novy 1995) other types of pelvic reproductive surgery, including 'ovarian drilling' as a treatment for clomiphene‐resistant polycystic ovarian syndrome, are being performed more widely.
The pregnancy and live birth rates following female pelvic reproductive surgery can be disappointing in spite of apparent normal anatomical relationships at the time of surgery and the restoration of fallopian tube patency in tubal surgery. Pre‐existing damage to the sensitive fimbrial end of the fallopian tube and intrinsic inflammatory tubal damage limit the success of reproductive surgery (Strandell 1995; Winston 1991). Other causes of failure to conceive following pelvic surgery include postoperative adhesion formation or (re)occlusion of the fallopian tubes. Failure to capture or to pass the released egg down the fallopian tube may then result.
Description of the intervention
Hydrotubation is the flushing of the fallopian tubes via transcervical instillation of fluid into the uterine cavity. It is widely used in the technique of hysterosalpingography to provide diagnostic information about the fallopian tubes when investigating infertility. Hydrotubation with oil‐soluble contrast media is of proven primary benefit in infertile couples (Vandekerckhove 1998), which may be due to the flushing out of occluding 'tubal plugs'. Hydrotubation could theoretically flush out debris which may accumulate within the lumen of the fallopian tube after tubal surgery and thus reduce the likelihood of tubal reocclusion. Grant (Grant 1971) claimed increased pregnancy rates in women undergoing early postoperative hydrotubation following tubal surgery.
How the intervention might work
Laparoscopy is widely used for diagnostic purposes in the investigation of infertility, usually in association with hydrotubation to determine tubal patency. It has the advantage over hysterosalpingography in that division of pelvic adhesions may be performed at the same time. Adhesiolysis, whether performed at laparotomy (Tulandi 1990) or laparoscopically (Reich 1987), is of primary benefit in tubal infertility. It has been claimed that following pelvic reproductive surgery second‐look laparoscopy with adhesiolysis may increase the intrauterine pregnancy rate (Surrey 1982) and decrease the ectopic pregnancy rate (Trimbos‐Kemper 1985) although others have failed to demonstrate increased pregnancy rates (Luber 1986; Gomel 1986). Second‐look laparoscopy is widely undertaken in the USA (DiZerega 2003).
Objectives
To assess the effectiveness and safety of postoperative procedures following female pelvic reproductive surgery in improving pregnancy and live birth outcomes.
Methods
Criteria for considering studies for this review
Types of studies
All randomised controlled trials (RCTs) were eligible for inclusion where a postoperative procedure was compared with a control group following pelvic reproductive surgery. Quasi‐randomised trials were not included.
Types of participants
Women of reproductive years experiencing primary or secondary infertility who underwent pelvic reproductive surgery.
Types of interventions
The following interventions after pelvic reproductive surgery were analysed.
1. Hydrotubation versus no hydrotubation (with and without other intraoperative or postoperative interventions).
2. Different modalities of hydrotubation (e.g. fluid containing steroids or antibiotics).
3. Second‐look laparoscopy with adhesiolysis versus no second‐look laparoscopy (with and without other intraoperative or postoperative interventions).
4. Any other postoperative procedure.
Types of outcome measures
The following rates should be defined within a given time period.
Primary outcomes
1. Pregnancy rate (per woman) 2. Live birth rate (per woman)
Secondary outcomes
1. Ectopic pregnancy rate (per woman) 2. Miscarriage rate (per intrauterine pregnancy or per woman) 3. Infection rate 4. Other complications 5. Tubal patency rate, at least one fallopian tube remaining open
Search methods for identification of studies
The search strategy of the Menstrual Disorders and Subfertility Group was used to identify all publications that described or might have described randomised trials of postoperative procedures following pelvic reproductive surgery.
We searched the electronic databases: the Cochrane Menstrual Disorders and Subfertility Group Trials Register (August 2008), Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2008, Issue 2), MEDLINE (1966 to August 2008), EMBASE (1988 to August 2008), and Biological Abstracts (1969 to August 2008). Reference lists of identified articles were searched and researchers in the field were contacted.
1. The Menstrual Disorders and Subfertility Group Trials Register was searched for any trial with any of the keywords in the title, abstract or keywords section. This Register is based on regular searches of MEDLINE, EMBASE, CINAHL, PsycINFO, and handsearching of 20 relevant journals and conference proceedings.
2. The MEDLINE and Biological Abstract databases were searched using the subject headings and keywords detailed in the abstracts Appendix 1.
3. The EMBASE database was searched using the same subject headings and keywords as detailed in the MEDLINE search strategy Appendix 3.
5. CENTRAL was searched using the following keywords: pelvic surgery, tubal surgery, fertility surgery, reproductive surgery, postoperative, postoperative procedures, hydrotubation, hysterosalpingogram, HSG, postoperative laparoscopy, second‐look laparoscopy,and adhesiolysisAppendix 2.
6. The citation lists of relevant publications, review articles, and included studies were also searched.
For the included trials, either the first or corresponding author was contacted to clarify data extraction issues.
Data collection and analysis
Two review authors independently selected the trials to be included in accordance with the above‐mentioned criteria. Disagreements were resolved by discussion.
Data were extracted and the trials were analysed for the following quality criteria, methodological details, and descriptive data of participants and outcomes. This information is presented in the table Characteristics of included studies.
Trial characteristics
Each included trial was assessed for the following criteria: concealed assignment, technique of randomisation, time of randomisation (pre or intraoperatively), number of randomised patients, number of patients not randomised with explanation, exclusion from randomisation, the presence of blinding, documentation of dropouts, follow up, standardisation of outcome assessment, and whether the intention‐to‐treat analysis or power calculation was employed. This information was included in the table Characteristics of included studies.
Two review authors performed the assessments of the quality of trials and data were extracted independently. All discrepancies were resolved by discussion. Additional information on trial methodology and trial data were sought from the authors of trials that appeared to meet the eligibility criteria but had aspects of methodology that were unclear, or data that were in a form that was unsuitable for meta‐analysis.
Statistical analysis was performed in accordance with the guidelines for statistical analysis in Section 8 of the Cochrane Handbook for Systematic Reviews of Interventions Higgins 2008 . Results for each study were expressed as odds ratios (OR) with 95% confidence intervals (CI) and were combined for meta‐analysis with RevMan software.
The Chi2 test was performed and the I2 statistic calculated to determine whether there was significant heterogeneity.
This review shall be updated every two years as per the Cochrane Collaboration recommendations.
Results
Description of studies
The selection of trials for inclusion in the review was performed by two review authors after employing the search strategy described previously. Differences of opinion were resolved by consensus. The search strategy yielded 607 studies. Of these 41 papers required closer scrutiny based on the title and abstract: 15 studies examined pregnancy outcome following the interventions and five of these were found to be RCTs eligible for inclusion. A single trial that met the eligibility criteria was excluded (Alborzi 2003) and has been discussed in the Discussion section of the review. The study could not be included as it randomised participants by alternation on admission.
Five RCTs with a total of 588 women met the criteria for inclusion in the review. All trials were published in full in peer‐reviewed journals. Three trials examined postoperative hydrotubation (Comninos 1977; Rock 1984; Soihet 1974) and two trials examined second‐look laparoscopy with adhesiolysis (Gurgan 1992; Tulandi 1989). Additional information has been sought for all five of these trials and was forthcoming, to date, only in two cases (Gurgan 1992; Tulandi 1989). The review authors are unaware of any ongoing trials relevant to this review. The year of publication of the included studies ranged from 1977 to 1992.
Trials examining postoperative hydrotubation
Comninos (Comninos 1977) randomised 30 women undergoing bilateral salpingostomy to early postoperative hydrotubation on the third, fifth, and seventh postoperative day versus peritubal irrigation on the third, fifth, and seventh postoperative day. Peritubal irrigation was via a prosthesis (the salpingostomy device of Cognat) that was attached to the serosa of the fallopian tube and uterine fundus and covered the distal portion of the tube. It was followed by three late hydrotubations three, five and seven days after removal of the prosthesis on the 12th postoperative day.
Rock (Rock 1984) randomised 206 women undergoing bilateral distal tubal surgery (unilateral if only one residual fallopian tube) to three groups comparing postoperative hydrotubation with lactated Ringer's solution versus postoperative hydrotubation with lactated Ringer's solution containing hydrocortisone versus no hydrotubation in women undergoing tubal surgery. The hydrotubations were performed on the first and third postoperative day and on the day of discharge from hospital.
Soihet undertook a three‐group parallel trial (Soihet 1974) and randomised 258 women undergoing a variety of tubal surgical procedures into three groups: early postoperative hydrotubation (twice weekly from the fifth postoperative day to six weeks); late postoperative hydrotubation (twice weekly from the 6th to 12th postoperative week) where the surgery had included anterior uterine suspension and Teflon tube stenting of the fallopian tubes (electively removed after six weeks); and late postoperative hydrotubation (twice weekly from the 6th to 12th postoperative week) with a solution containing gentamicin where the surgery included tubal suspension in addition to anterior uterine suspension and tubal stenting as described above.
Trials examining second‐look laparoscopy with adhesiolysis
Gurgan (Gurgan 1992) randomised 20 women undergoing laparoscopic Nd‐YAG laser photocoagulation of the ovaries for clomiphene‐resistant polycystic ovarian syndrome to second‐look laparoscopy with adhesiolysis within three to four weeks of surgery versus no second‐look laparoscopy.
Tulandi (Tulandi 1989) randomised 74 women failing to conceive one year after terminal salpingostomy or salpingo‐ovariolysis to second‐look laparoscopy with adhesiolysis versus no second‐look laparoscopy.
No power calculations were given in any paper although one author (Tulandi 1989) stated in correspondence that a power calculation had been performed prior to the trial to determine sample size. No source of funding was stated for any of the trials. One trial was multicentre, involving five centres: three in the USA, one in the Netherlands, and one in Colombia (Rock 1984); four were single‐centre trials (Comninos 1977; Gurgan 1992; Soihet 1974; Tulandi 1989). The timing and duration of the trial was given in the publication for one trial (Rock 1984) and in correspondence for two trials (Gurgan 1992; Tulandi 1989).
The important prognostic factors of women's ages and the duration of infertility were stated in all trials except Soihet (Soihet 1974). Only one trial (Gurgan 1992) specified the proportion of women with primary or secondary infertility. The investigative work up was described in all trials except Soihet (Soihet 1974); these included semen analysis, assessments of likelihood of ovulation and of tubal patency. The results of these investigations were all normal in the couples in Comninos (Comninos 1977) and not specified by Rock (Rock 1984). Tulandi (Tulandi 1989) mentioned that all other investigations were normal and these were specified in correspondence. In Gurgan (Gurgan 1992) five women had minimal endometriosis (three undergoing second‐look laparoscopy and two controls) and four male partners had mild oligoasthenospermia (one partner of a woman undergoing second‐look laparoscopy and three partners of women in the control group). The extent of the cause of infertility was defined in all trials: Comninos (Comninos 1977) studied women with bilateral distal tubal occlusion; Rock (Rock 1984) and Tulandi (Tulandi 1989) confirmed tubal disease in all women, Rock (Rock 1984) noted that mild tubal disease correlated with surgical success; Soihet (Soihet 1974) studied women with tubal occlusion or immobility; Gurgan (Gurgan 1992) studied women with polycystic ovarian syndrome resistant to high‐dose clomiphene citrate but failed to specify their body mass indices. Only two trials stated previous fertility treatments that had been undertaken: the women in Comninos (Comninos 1977) had all undergone 12 therapeutic hydrotubations in the three cycles prior to tubal surgery; Gurgan (Gurgan 1992) had treated all women with clomiphene, in doses up to 200 mg. Exclusion criteria prior to randomisation were stated in only two trials: Comninos (Comninos 1977) excluded women with fibroids, endometriosis, and ovarian cysts; Tulandi (Tulandi 1989) excluded women with endometriosis.
The number of pregnancies was given and the pregnancy rate per woman could be extracted from the data in all trials; this was done for all outcomes in order to maintain homogeneity of outcomes, as far as possible, for this review. Ectopic pregnancy rates per woman (the number of women experiencing at least one ectopic pregnancy over the time period defined by the trial) could also be extracted from the data in all trials. Comparison of these rates per woman within a defined time period was, therefore, possible in all studies except one (Soihet 1974). The preferable method of reporting success rates in any trial would be discrete time survival analysis, followed by continuous time survival analysis, then rates per woman within a given time period (used in this review). Only one trial expressed the outcomes in a continuous time survival analysis (Tulandi 1989). Live birth rates were stated in two trials (Soihet 1974; Rock 1984) and live birth rate plus ongoing pregnancy rate at the time of publication was stated in one (Gurgan 1992). Miscarriage rates were stated in three trials (Comninos 1977; Gurgan 1992; Rock 1984), tubal patency rates in three trials (Comninos 1977; Soihet 1974; Tulandi 1989 in correspondence), post‐treatment infection rates in four trials (Gurgan 1992 in correspondence; Rock 1984; Soihet 1974; Tulandi 1989) and post‐treatment complication rates in three trials (Gurgan 1992 in correspondence; Rock 1984; Tulandi 1989 in correspondence). The duration of follow up was stated in all trials except Soihet (1974) and in three trials the duration of follow up was 24 months or longer (Comninos 1977; Rock 1984; Tulandi 1989).
Risk of bias in included studies
The overall quality of the included trials was poor, particularly the oldest trials, by the standards of RCTs currently being undertaken see Figure 1 and Figure 2.
1.
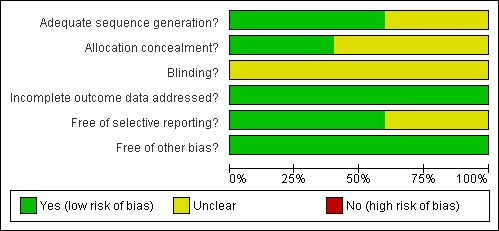
Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.
2.
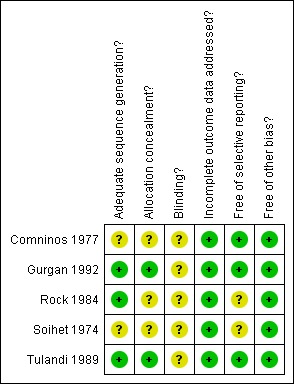
Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
Of the five RCTs, three stated a genuine method of randomisation: a random number table (Gurgan 1992), a pack of cards (Rock 1984), computer‐generated random numbers (Tulandi 1989). Two trials had unusual numbers in their groups: Rock (Rock 1984) had 86, 60, and 60 participants respectively; and Soihet (Soihet 1974) had 67, 100, and 91 participants respectively, which raised concerns over the randomisation process. The uneven numbers per group could represent deliberate unequal randomisation (unlikely), failure to use permuted blocks (very likely), abuse of the process (also likely), post‐randomisation exclusions (almost certain), or combinations of the above. The timing of randomisation was not stated in any of the three trials that examined postoperative hydrotubation; in the other two trials the randomisation took place: immediately after the initial surgery (Gurgan 1992), and one year after the initial surgery (Tulandi 1989). Allocation concealment was adequate in two trials (Gurgan 1992, Tulandi 1989), unclear in one trial (Rock 1984), and probably not used in the other two trials (Comninos 1977; Soihet 1974). None of the trials used blinding and indeed by the nature of the interventions, hydrotubation or second‐look laparoscopy, blinding would be difficult. However, Rock (Rock 1984) and Soihet (Soihet 1974) could have built double‐blinding into two arms of their studies. Scope for bias from not blinding includes the possibility of more thorough follow up by investigators to find outcomes in couples not attending follow‐up clinics.
Withdrawals after randomisation were mentioned by only Gurgan (Gurgan 1992): one participant declined second‐look laparoscopy and was excluded from the analysis. In this case an intention‐to‐treat analysis was not done by the authors but was possible and was performed in this review. Since no withdrawals or losses to follow up were mentioned in any of the other trials, it is likely that only women completing the study were used in the results analysis. This meant that an intention‐to‐treat analysis was probably not done and nor would be possible for those trials.
The effect of the intervention hydrotubation was seriously obscured by the presence of other interventions in the control groups, in two trials (Comninos 1977; Soihet 1974).
Effects of interventions
Trial results have been combined for only five outcomes and with not more than two studies in any analysis. There was no evidence of statistical heterogeneity in any of the comparisons.
Hydrotubation versus no hydrotubation (Rock 1984) Based on 86 women in a single study, the intervention hydrotubation did not significantly alter the odds of pregnancy (OR 1.12, 95% CI 0.57 to 2.21), live birth (OR 0.61, 95% CI 0.24 to 1.59), ectopic pregnancy (OR 1.62, 95% CI 0.52 to 5.03), or miscarriage (OR 2.71, 95% CI 0.62 to 11.84). Rock 1984 reported that there were no post‐treatment infections or complications in either the treatment or control groups.
Hydrotubation with steroid versus hydrotubation without steroid (Rock 1984) Based on 60 women in a single study, the addition of hydrocortisone to the hydrotubation fluid did not significantly alter the odds of pregnancy (OR 0.82, 95% CI 0.35 to 1.95), live birth (OR 0.49, 95% CI 0.13 to 1.89), ectopic pregnancy (OR 2.04, 95% CI 0.53 to 7.91), or miscarriage (OR 1.19, 95% CI 0.17 to 8.21). Rock 1984 reported that there were no post‐treatment infections or complications in either the treatment or control groups.
Hydrotubation with antibiotic versus hydrotubation without antibiotic (Soihet 1974) Based on 55 women in a single study, the addition of gentamicin to the hydrotubation significantly increased the odds of pregnancy (OR 2.23, 95% CI 1.12 to 4.44) and live birth (OR 2.37, 95% CI 1.11 to 5.05); decreased the odds of infection (OR 0.12, 95% CI 0.05 to 0.28); but failed to significantly alter the odds of ectopic pregnancy (OR 1.39, 95% CI 0.37 to 5.30) or tubal patency (OR 0.86, 95% CI 0.48 to 1.55). However, the women who received hydrotubation with gentamicin received the additional intervention of tubal suspension at initial surgery. Soihet (1974) specifically stated febrile morbidity (infection) as one of the outcomes of the trial and reported infections in as many as 60% of women in the early hydrotubation group.
Early hydrotubation versus late non‐antibiotic hydrotubation (Soihet 1974) Based on 67 women in a single study, early hydrotubation when compared to late non‐antibiotic hydrotubation was associated with significantly increased odds of infective morbidity (OR 4.72, 95% CI 2.50 to 8.93) and significantly reduced odds of patency of at least one fallopian tube at subsequent assessment (OR 0.29, 95% CI 0.16 to 0.55), which suggested a possible benefit with the use of late non‐antibiotic hydrotubation following its removal. Early hydrotubation when compared to late non‐antibiotic hydrotubation failed to significantly alter the odds of pregnancy (OR 1.11, 95% CI 0.48 to 2.61), live birth (OR 0.94, 95% CI 0.35 to 2.55), or ectopic pregnancy (OR 1.54, 95% CI 0.39 to 6.51).
Early hydrotubation versus tubal stenting (Comninos 1977) Based on 30 women in a single study, early hydrotubation when compared to tubal stenting failed to significantly alter the odds of pregnancy (OR 0.52, 95% CI 0.11 to 2.54), ectopic pregnancy (OR 1.00, 95% CI 0.06 to 16.79), miscarriage (OR 0.85, 95% CI 0.06 to 11.78), or miscarriage (OR 0.34, 95% Cl 0.08 to 1.44).
Second‐look laparoscopy versus no second‐look laparoscopy (Gurgan 1992; Tulandi 1989) Whether considered both independently and combined in a meta‐analysis, early second‐look laparoscopy with adhesiolysis (Gurgan 1992) and late second‐look laparoscopy with adhesiolysis (Tulandi 1989) did not significantly alter the odds of pregnancy (OR 0.96, 95% CI 0.44 to 2.07), live birth (OR 0.67, 95% CI 0.19 to 2.32), ectopic pregnancy (OR 1.49, 95% CI 0.46 to 4.79), or miscarriage (OR 1.27, 95% CI 0.15 to 10.88). Gurgan 1992 and Tulandi 1989 reported that there were no post‐treatment infections or complications in either treatment or control groups.
Discussion
This systematic review of RCTs has failed to show a significant benefit or detriment of hydrotubation or second‐look laparoscopy with adhesiolysis following pelvic reproductive surgery. Hydrotubation with antibiotic versus hydrotubation without antibiotic may increase the odds of pregnancy and live birth while reducing the odds of infection. The use of a tubal stent or prosthesis followed, after its removal, by late hydrotubation may reduce the odds of infection and increase the odds of at least one fallopian tube remaining patent but there is no evidence that it improves fertility.
Whilst this review did not demonstrate a significant increase in the odds of infection or complications following the postoperative procedures, the interventions studied are not without invasive characteristics. Hydrotubation is uncomfortable, embarrassing, and carries a cost. Laparoscopy causes discomfort, carries the hazards of general anaesthesia and the rare but recognised hazards of gastrointestinal, urinary tract or vascular injury and, even when performed on a day‐case basis, is costly for the health service and the patient. The interventions should not be performed without evidence of benefit.
Grant (Grant 1971) reported increased pregnancy rates in women undergoing postoperative hydrotubation with a solution containing hydrocortisone when compared to a control group but studied consecutive patients and used a historical control group. There are reports of a variety of types of hydrotubation fluid used postoperatively (Arronet 1969; Jessen 1971; Rock 1978) but no other studies have claimed benefit of postoperative hydrotubation over a control group. Whilst the number of women in the three trials examining postoperative hydrotubation was 474, there are quality concerns over all three trials (Comninos 1977; Rock 1984; Soihet 1974) and unfortunately none of the authors of these trials responded to requests for additional information. It is difficult to obtain reliable data from the 'oldest' trials, which tend to be the poorest quality trials and the least likely to be clarified in correspondence. The corresponding authors may no longer be contact able and if contact able they may be unlikely to make meaningful comments about research performed, in some cases, more than 20 years previously.
The apparent benefit of antibiotic in hydrotubation fluid was based on trial data from Soihet (Soihet 1974), a trial of poor quality. In particular, the group of women receiving hydrotubation fluid containing gentamicin had also undergone tubal suspension as part of additional surgery (an additional intervention not performed in the control group). The trial author emphasised the importance of avoiding infection for the success of tubal surgery (Soihet 1974). It may simply be that administration of antibiotic versus no antibiotic confers benefit following tubal stent removal six weeks after tubal surgery; with the route of antibiotic administration, in this case by hydrotubation, being coincidental. Increased odds of pregnancy and live birth in late hydrotubation after tubal stent removal, where hydrotubation fluid contains antibiotic versus no antibiotic, must therefore be interpreted cautiously. It is worthy of further evaluation.
A future RCT examining postoperative hydrotubation to improve fertility following tubal surgery would be justifiable if the hydrotubation fluid was to contain antibiotic, and if the trial was adequately powered. Live birth rates of 23% and 11% occurred with late postoperative hydrotubation with antibiotic and without antibiotic, respectively (Soihet 1974). In order to have 80% power to detect such an increase in the live birth rate at the 95% confidence level, a trial would need to randomise 338 women undergoing postoperative hydrotubation with antibiotic versus no hydrotubation. This would be the absolute minimum number to confer sufficient weight to the results and conclusions of such a trial.
The total number of women in the two RCTs examining second‐look laparoscopy (Gurgan 1992; Tulandi 1989) was only 56. With underpowered studies, conclusions about the ineffectiveness of these procedures must be made cautiously as this is absence of evidence of benefit rather than evidence of absence of benefit. Much consideration was given to the pooling of data from the trials of Gurgan (Gurgan 1992) and Tulandi (Tulandi 1989) in a meta‐analysis. The primary surgery was very different (tubal surgery compared with laser photocoagulation of polycystic ovaries), the participants differed in that the primary surgery had already failed to reverse infertility in those undergoing tubal surgery (not the case for the women undergoing ovarian photocoagulation), and in addition there was a difference in the timing of the second‐look laparoscopy. The decision to pool the data was based on the fact that both trials used the single intervention of second‐look laparoscopy with adhesiolysis; there was an absence of evidence with respect to early and late second‐look laparoscopic division of adhesions, that one offers benefit over the other; and the fact that results of the trials were very similar.
The most appropriate time to perform postoperative pelvic adhesiolysis is uncertain and has varied from eight days to two years after the primary surgery (DeCherney 1984; Gomel 1986; Raj 1982; Surrey 1982; Trimbos‐Kemper 1985). It is very clear that, even with the most scrupulous of surgical techniques, adhesions do often form after pelvic reproductive surgery and that early second‐look laparoscopy with adhesiolysis at a later date reduces the extent of such adhesions (Jansen 1988; Raj 1982; Trimbos‐Kemper 1985). Jansen (1988) suggested the ideal time for early postoperative adhesiolysis would be between the time of serosal healing (eight days) and established adhesion fibrosis (21 days). Others have suggested these early fine fibrinous adhesions are a normal consequence of tissue repair and may eventually disappear with time, due to local release of breakdown mediators in the remodelling process (Gillett 1994). In the RCTs of this review, early second‐look laparoscopy with adhesiolysis was undertaken after three to four weeks (Gurgan 1992). Late second‐look laparoscopy has additional diagnostic value in the rational planning of future fertility treatment, for example accelerating referral for in vitro fertilisation with women deemed unlikely to conceive based on the laparoscopic appearance of the pelvis. Late second‐look laparoscopy was performed one year after the primary surgery in the RCT included in this review (Tulandi 1989). It is also interesting to speculate, but premature to conclude, that the lysis of adhesions due to surgery gives a different outcome from the lysis of non‐surgical adhesions, the latter considered beneficial based on non‐randomised studies by Tulandi (Tulandi 1990) and Reich (Reich 1987).
Unfortunately, to the best of our knowledge, no further truly randomised studies examining second‐look laparoscopy with adhesiolysis following pelvic reproductive surgery, which could have been included in the update of this review, have been published. A single study was published in 2003 which examined the place for second‐look laparoscopy following laparoscopic salpingo‐ovariolysis (Alborzi 2003). This study could not be included in this systematic review as patients were allocated on the basis of a quasi‐randomisation technique. Forty‐six women underwent second‐look laparoscopy while 44 women did not undergo second‐look laparoscopy following laparoscopic salpingo‐ovariolysis. The study reported no difference in live birth rates when comparing those who underwent second‐look laparoscopy (n = 11) and the women who did not (n = 15).
In future a RCT examining second‐look laparoscopy with adhesiolysis following pelvic reproductive surgery would be justifiable if it had adequate power and was able to randomise to early (eight to 21 days postoperatively), late, or no second‐look laparoscopy with adhesiolysis. The overall pregnancy rates (including with second‐look laparoscopy and no second‐look laparoscopy) were 45% following laparoscopic laser ovarian photocoagulation (with 40% live birth rate) (Gurgan 1992), 22% following salpingostomy (Tulandi 1989), and 61% following salpingo‐ovariolysis (Tulandi 1989). An increase in the total pregnancy rate of 25% (risk ratio 1.25) would be clinically important after any of these procedures, giving pregnancy rates of 56%, 28%, and 76% respectively. In order to have 80% power to detect such increases in the total pregnancy rates at the 95% confidence level, a trial would need to randomise 652 women following laparoscopic laser ovarian photocoagulation, 2002 following salpingostomy, and 414 women following salpingo‐ovariolysis to second‐look laparoscopy with adhesiolysis or no second‐look laparoscopy. RCTs with the three groups suggested above (early versus late second‐look laparoscopy with adhesiolysis versus no second‐look laparoscopy) could increase the power of the study.
Authors' conclusions
Implications for practice.
There is insufficient evidence to support the routine practice of postoperative hydrotubation or second‐look laparoscopy with adhesiolysis following female pelvic reproductive surgery.
Implications for research.
RCTs of higher quality and sufficient power should be undertaken to examine the interventions of early and late second‐look laparoscopy with adhesiolysis and postoperative hydrotubation. In the case of postoperative hydrotubation, there is justification for a RCT of postoperative hydrotubation with antibiotic‐containing fluid versus no hydrotubation for improving fertility following tubal surgery.
Evaluation of the outcomes in these trials should include pregnancy, live birth, ectopic pregnancy rates per woman, miscarriage rates per intrauterine pregnancy and also: ‐ patient satisfaction; ‐ cost; ‐ complications, although the serious laparoscopic complications are rare and would require large numbers to show significant results.
What's new
| Date | Event | Description |
|---|---|---|
| 11 February 2009 | New citation required but conclusions have not changed | Review updated August 2008 |
History
Protocol first published: Issue 3, 1999 Review first published: Issue 1, 2000
| Date | Event | Description |
|---|---|---|
| 12 August 2008 | New search has been performed | Search strategy re‐run. No new RCTs identified. Text of the review updated especially the review methodology, results, discussion and conclusions. |
| 26 May 2008 | New search has been performed | Converted to new review format. |
| 31 March 2008 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
We would like to thank the members of the Cochrane Menstrual Disorders and Subfertility Review Group based in Auckland, New Zealand who assisted with this review. We wish to thank Patrick Vandekerckhove and Richard Lilford for their input into the initial draft of the protocol.
Appendices
Appendix 1. MEDLINE search strategy
1 gynecologic surgical procedures/ or hysteroscopy/ or salpingostomy/ or sterilization, tubal/ (8462) 2 exp adnexal diseases/su or endometriosis/su or exp uterine diseases/su (28082) 3 Polycystic Ovary Syndrome/su (429) 4 Pelvic Inflammatory Disease/su or exp Pelvic Pain/su or Pelvis/su (1517) 5 Sterilization Reversal/ (918) 6 ((tubal or pelvic or ovar$ or uter$ or fertility or reproducti$) adj surgery).tw. (1802) 7 (tubal adj disease).tw. (297) 8 (block$ adj5 tub$).tw. (1817) 9 (salpingo‐ovariolysis or salpingostomy or tubal reanastomosis or cornual anastomosis or utero tubal implantation).tw. (380) 10 or/1‐9 (39707) 11 second‐look surgery/ (173) 12 Hysterosalpingography/ (3309) 13 Fallopian Tube Patency Tests/ (527) 14 (hydrotubation or hysterosalpingogr$ or salpingog$ or HSG).tw. (2403) 15 (postoperative laparoscop$ or postoperative procedure$ or second‐look laparoscop$).tw. (364) 16 adhesiolysis.tw. (485) 17 tub$ patency.tw. (616) 18 or/11‐17 (5749) 19 10 and 18 (1108) 20 randomised controlled trial.pt. (229481) 21 controlled clinical trial.pt. (74116) 22 Randomized Controlled Trials/ (46944) 23 Random allocation/ (56812) 24 Double‐blind method/ (89516) 25 Single‐blind method/ (10609) 26 or/20‐25 (389441) 27 clinical trial.pt. (431918) 28 exp clinical trials/ (186631) 29 (clin$ adj25 trial$).ti,ab,sh. (125917) 30 ((singl$ or doubl$ or tripl$ or trebl$) adj25 (blind$ or mask$)).ti,ab,sh. (88774) 31 Placebos/ (25762) 32 placebo$.ti,ab,sh. (112355) 33 random$.ti,ab,sh. (478353) 34 Research design/ (46062) 35 or/27‐34 (847992) 36 animal/ not (human/ and animal/) (3032479) 37 26 or 35 (854870) 38 37 not 36 (783796) 39 19 and 38 (160) 40 exp Carcinoma/ (352410) 41 (cancer$ or carcinoma).tw. (756335) 42 39 not (40 or 41) (135) 43 Male/ (4658956) 44 42 not 43 (132) 45 from 44 keep 1‐132 (132)
Appendix 2. CENTRAL
1 second‐look surgery/ (16) 2 Hysterosalpingography/ (77) 3 Fallopian Tube Patency Tests/ (22) 4 (hydrotubation or hysterosalpingogr$ or salpingog$ or HSG).tw. (116) 5 (postoperative laparoscop$ or postoperative procedure$ or second‐look laparoscop$).tw. (83) 6 adhesiolysis.tw. (34) 7 tub$ patency.tw. (49) 8 or/1‐7 (267) 9 exp gynecologic surgery/ or exp uterine tube surgery/ or exp uterus surgery/ or exp sterilization reversal/ (1988) 10 exp adnexa disease/ or exp ovary disease/ or exp ovary cyst/ or exp follicle cyst/ or exp ovary polycystic disease/ or exp stein leventhal syndrome/ or exp ovary insufficiency/ or exp ovary tumor/ or exp pelvic inflammatory disease/ (445) 11 ((tubal or pelvic or ovar$ or uter$ or fertility or reproducti$) adj surgery).tw. (92) 12 (tubal adj disease).tw. (18) 13 (block$ adj5 tub$).tw. (117) 14 (salpingo‐ovariolysis or salpingostomy or tubal reanastomosis or cornual anastomosis or utero tubal implantation).tw. (28) 15 or/9‐14 (2637) 16 8 and 15 (45) 17 limit 16 to yr="2002 ‐ 2007" (12) 18 from 17 keep 1‐12 (12)
Appendix 3. EMBASE
1 second‐look surgery/ (1449) 2 Hysterosalpingography/ (1529) 3 Fallopian Tube Patency Tests/ (1460) 4 (hydrotubation or hysterosalpingogr$ or salpingog$ or HSG).tw. (1645) 5 (postoperative laparoscop$ or postoperative procedure$ or second‐look laparoscop$).tw. (349) 6 adhesiolysis.tw. (509) 7 tub$ patency.tw. (535) 8 or/1‐7 (6000) 9 exp gynecologic surgery/ or exp uterine tube surgery/ or exp uterus surgery/ or exp sterilization reversal/ (55648) 10 exp adnexa disease/ or exp ovary disease/ or exp ovary cyst/ or exp follicle cyst/ or exp ovary polycystic disease/ or exp stein leventhal syndrome/ or exp ovary insufficiency/ or exp ovary tumor/ or exp pelvic inflammatory disease/ (65719) 11 ((tubal or pelvic or ovar$ or uter$ or fertility or reproducti$) adj surgery).tw. (1615) 12 (tubal adj disease).tw. (284) 13 (block$ adj5 tub$).tw. (1548) 14 (salpingo‐ovariolysis or salpingostomy or tubal reanastomosis or cornual anastomosis or utero tubal implantation).tw. (347) 15 or/9‐14 (116999) 16 8 and 15 (2302) 17 Controlled study/ or randomised controlled trial/ (2470434) 18 double blind procedure/ (64962) 19 single blind procedure/ (6784) 20 crossover procedure/ (18946) 21 drug comparison/ (81250) 22 placebo/ (101777) 23 random$.ti,ab,hw,tn,mf. (376909) 24 latin square.ti,ab,hw,tn,mf. (1071) 25 crossover.ti,ab,hw,tn,mf. (33101) 26 cross‐over.ti,ab,hw,tn,mf. (11407) 27 placebo$.ti,ab,hw,tn,mf. (150676) 28 ((doubl$ or singl$ or tripl$ or trebl$) adj5 (blind$ or mask$)).ti,ab,hw,tn,mf. (108040) 29 (comparative adj5 trial$).ti,ab,hw,tn,mf. (6105) 30 (clinical adj5 trial$).ti,ab,hw,tn,mf. (496797) 31 or/17‐30 (2960973) 32 nonhuman/ (2922616) 33 animal/ not (human/ and animal/) (12862) 34 or/32‐33 (2926220) 35 31 not 34 (1741888) 36 16 and 35 (655) 37 (2002$ or 2003$ or 2004$ or 2005$ or 2006$ or 2007$).em. (3072997) 38 36 and 37 (294) 39 from 38 keep 1‐294 (294)
Data and analyses
Comparison 1. Hydrotubation (all types) versus no hydrotubation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Total pregnancy rate | 1 | 206 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.12 [0.57, 2.21] |
| 2 Livebirth rate | 1 | 206 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.61 [0.24, 1.59] |
| 3 Ectopic pregnancy rate | 1 | 206 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.62 [0.52, 5.03] |
| 4 Miscarriage rate | 1 | 30 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 2.71 [0.62, 11.84] |
| 5 Infection rate | 1 | 206 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Complication rate | 1 | 206 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
1.1. Analysis.
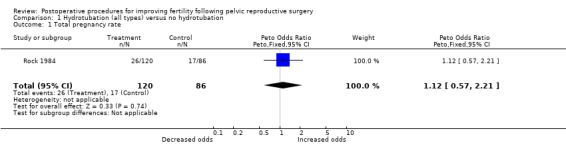
Comparison 1 Hydrotubation (all types) versus no hydrotubation, Outcome 1 Total pregnancy rate.
1.2. Analysis.
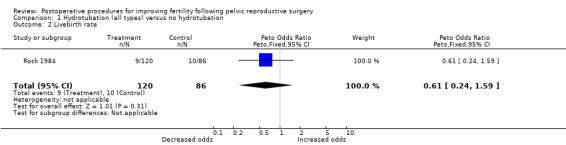
Comparison 1 Hydrotubation (all types) versus no hydrotubation, Outcome 2 Livebirth rate.
1.3. Analysis.
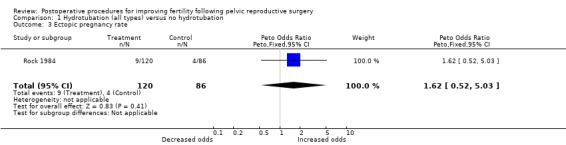
Comparison 1 Hydrotubation (all types) versus no hydrotubation, Outcome 3 Ectopic pregnancy rate.
1.4. Analysis.
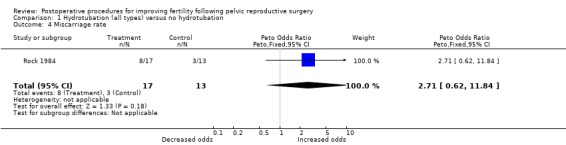
Comparison 1 Hydrotubation (all types) versus no hydrotubation, Outcome 4 Miscarriage rate.
1.5. Analysis.
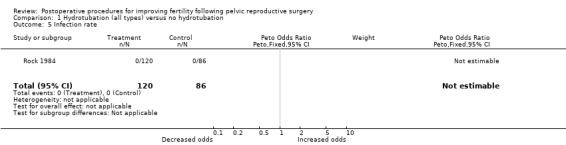
Comparison 1 Hydrotubation (all types) versus no hydrotubation, Outcome 5 Infection rate.
1.6. Analysis.
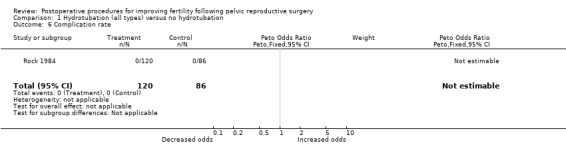
Comparison 1 Hydrotubation (all types) versus no hydrotubation, Outcome 6 Complication rate.
Comparison 2. Hydrotubation with steroid versus hydrotubation without steroid.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Total pregnancy rate | 1 | 120 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.82 [0.35, 1.95] |
| 2 Livebirth rate | 1 | 120 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.49 [0.13, 1.89] |
| 3 Ectopic pregnancy rate | 1 | 120 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 2.04 [0.53, 7.91] |
| 4 Miscarriage rate | 1 | 17 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.19 [0.17, 8.21] |
| 5 Infection rate | 1 | 120 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Complication rate | 1 | 240 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
2.1. Analysis.
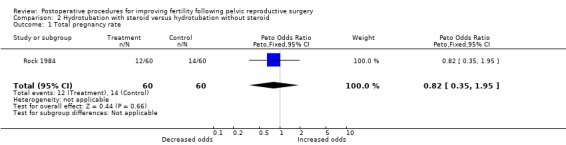
Comparison 2 Hydrotubation with steroid versus hydrotubation without steroid, Outcome 1 Total pregnancy rate.
2.2. Analysis.
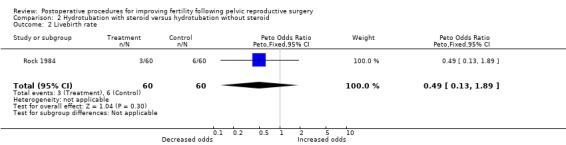
Comparison 2 Hydrotubation with steroid versus hydrotubation without steroid, Outcome 2 Livebirth rate.
2.3. Analysis.
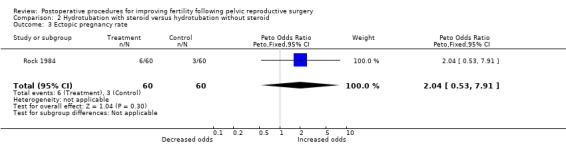
Comparison 2 Hydrotubation with steroid versus hydrotubation without steroid, Outcome 3 Ectopic pregnancy rate.
2.4. Analysis.
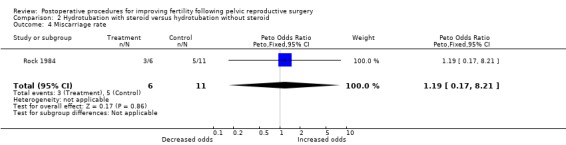
Comparison 2 Hydrotubation with steroid versus hydrotubation without steroid, Outcome 4 Miscarriage rate.
2.5. Analysis.
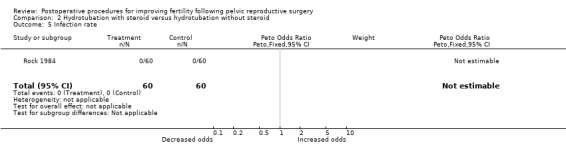
Comparison 2 Hydrotubation with steroid versus hydrotubation without steroid, Outcome 5 Infection rate.
2.6. Analysis.
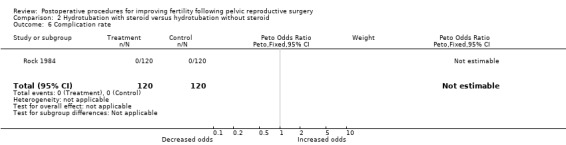
Comparison 2 Hydrotubation with steroid versus hydrotubation without steroid, Outcome 6 Complication rate.
Comparison 3. Hydrotubation with antibiotic versus hydrotubation without antibiotic.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Total pregnancy rate | 1 | 191 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 2.23 [1.12, 4.44] |
| 2 Livebirth rate | 1 | 191 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 2.37 [1.11, 5.05] |
| 3 Ectopic pregnancy rate | 1 | 191 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.39 [0.37, 5.30] |
| 4 Infection rate | 1 | 191 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.12 [0.05, 0.28] |
| 5 Tubal patency rate | 1 | 191 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.86 [0.48, 1.55] |
3.1. Analysis.
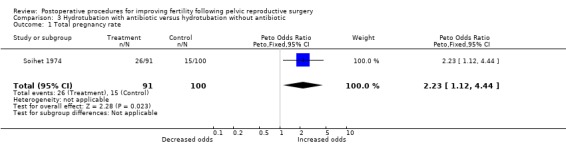
Comparison 3 Hydrotubation with antibiotic versus hydrotubation without antibiotic, Outcome 1 Total pregnancy rate.
3.2. Analysis.
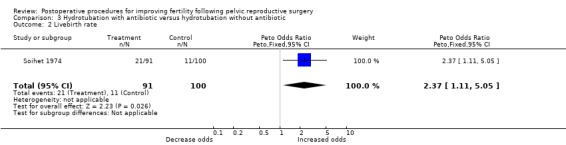
Comparison 3 Hydrotubation with antibiotic versus hydrotubation without antibiotic, Outcome 2 Livebirth rate.
3.3. Analysis.
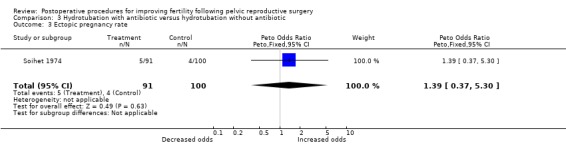
Comparison 3 Hydrotubation with antibiotic versus hydrotubation without antibiotic, Outcome 3 Ectopic pregnancy rate.
3.4. Analysis.
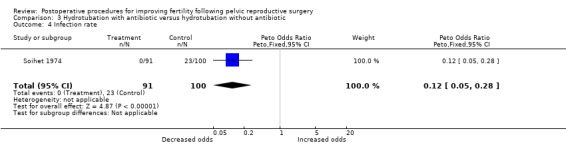
Comparison 3 Hydrotubation with antibiotic versus hydrotubation without antibiotic, Outcome 4 Infection rate.
3.5. Analysis.
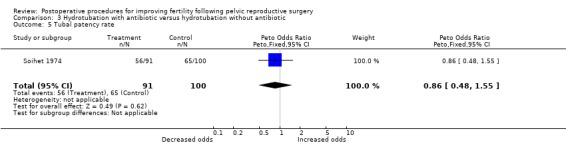
Comparison 3 Hydrotubation with antibiotic versus hydrotubation without antibiotic, Outcome 5 Tubal patency rate.
Comparison 4. Early hydrotubation versus late hydrotubation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Total pregnancy rate | 1 | 167 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.11 [0.48, 2.61] |
| 2 Livebirth rate | 1 | 167 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.94 [0.35, 2.55] |
| 3 Ectopic pregnancy rate | 1 | 167 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.54 [0.36, 6.51] |
| 4 Infection rate | 1 | 167 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 4.72 [2.50, 8.93] |
| 5 Tubal patency rate | 1 | 167 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.29 [0.16, 0.55] |
4.1. Analysis.
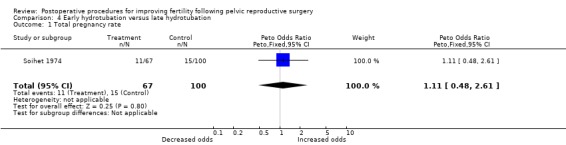
Comparison 4 Early hydrotubation versus late hydrotubation, Outcome 1 Total pregnancy rate.
4.2. Analysis.
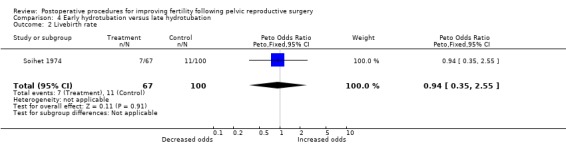
Comparison 4 Early hydrotubation versus late hydrotubation, Outcome 2 Livebirth rate.
4.3. Analysis.
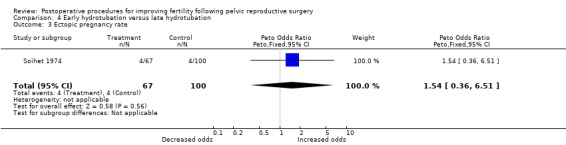
Comparison 4 Early hydrotubation versus late hydrotubation, Outcome 3 Ectopic pregnancy rate.
4.4. Analysis.
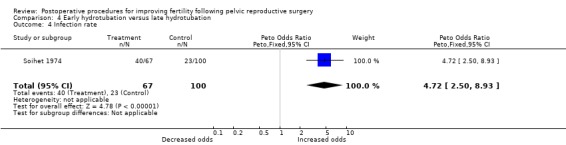
Comparison 4 Early hydrotubation versus late hydrotubation, Outcome 4 Infection rate.
4.5. Analysis.
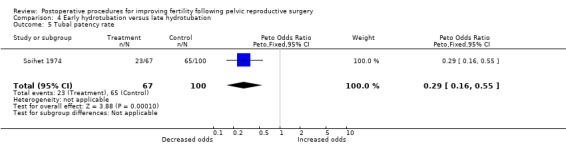
Comparison 4 Early hydrotubation versus late hydrotubation, Outcome 5 Tubal patency rate.
Comparison 5. Early hydrotubation versus tubal stent.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Total pregnancy rate | 1 | 30 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.52 [0.11, 2.54] |
| 2 Ectopic pregnancy rate | 1 | 30 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.0 [0.06, 16.79] |
| 3 Miscarriage rate | 1 | 11 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.85 [0.06, 11.78] |
| 4 Tubal patency rate | 1 | 30 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.34 [0.08, 1.44] |
5.1. Analysis.
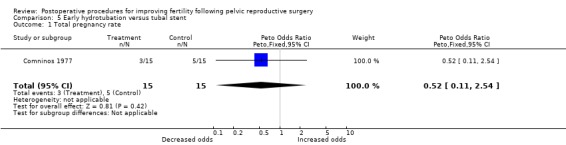
Comparison 5 Early hydrotubation versus tubal stent, Outcome 1 Total pregnancy rate.
5.2. Analysis.
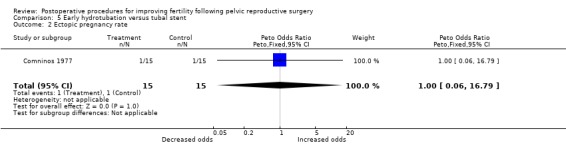
Comparison 5 Early hydrotubation versus tubal stent, Outcome 2 Ectopic pregnancy rate.
5.3. Analysis.
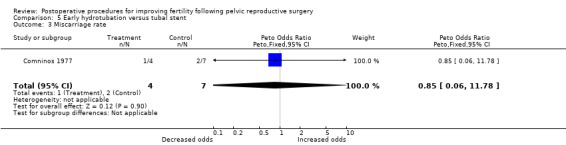
Comparison 5 Early hydrotubation versus tubal stent, Outcome 3 Miscarriage rate.
5.4. Analysis.
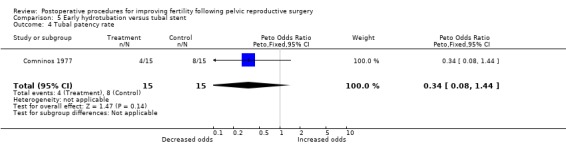
Comparison 5 Early hydrotubation versus tubal stent, Outcome 4 Tubal patency rate.
Comparison 6. Second‐look laparoscopy versus no second‐look laparoscopy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Total pregnancy rate | 2 | 114 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.99 [0.47, 2.06] |
| 1.1 Salpingostomy or Salpingo‐ovariolysis | 1 | 74 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.22 [0.49, 3.06] |
| 1.2 Laparoscopic ovarian drilling | 1 | 40 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.68 [0.20, 2.30] |
| 2 Livebirth rate | 1 | 40 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.67 [0.19, 2.32] |
| 2.1 Laparoscopic ovarian drilling | 1 | 40 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.67 [0.19, 2.32] |
| 3 Ectopic pregnancy rate | 2 | 114 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.51 [0.48, 4.81] |
| 3.1 Salpingostomy or Salpingo‐ovariolysis | 1 | 74 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.51 [0.48, 4.81] |
| 3.2 Laparoscopic ovarian drilling | 1 | 40 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Miscarriage rate | 1 | 20 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.27 [0.15, 10.88] |
| 4.1 Laparoscopic ovarian drilling | 1 | 20 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.27 [0.15, 10.88] |
| 5 Infection rate | 2 | 76 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.1 Salpingostomy or Salpingo‐ovariolysis | 1 | 36 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 Laparoscopic ovarian drilling | 1 | 40 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Complication rate | 2 | 76 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.1 Salpingostomy or Salpingo‐ovariolysis | 1 | 36 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 Laparoscopic ovarian drilling | 1 | 40 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Tubal patency rate | 1 | 36 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.1 Salpingostomy or Salpingo‐ovariolysis | 1 | 36 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
6.1. Analysis.
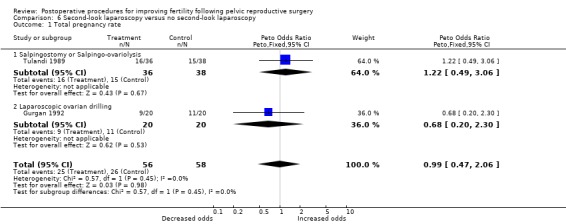
Comparison 6 Second‐look laparoscopy versus no second‐look laparoscopy, Outcome 1 Total pregnancy rate.
6.2. Analysis.
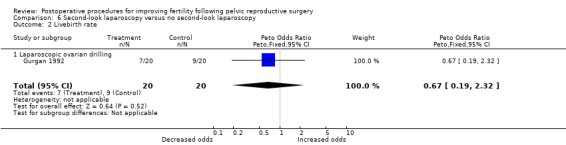
Comparison 6 Second‐look laparoscopy versus no second‐look laparoscopy, Outcome 2 Livebirth rate.
6.3. Analysis.
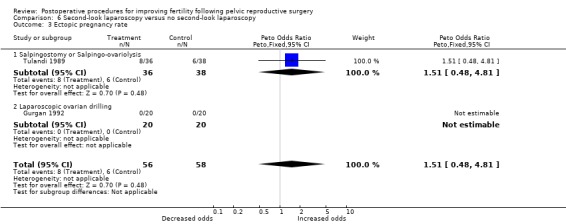
Comparison 6 Second‐look laparoscopy versus no second‐look laparoscopy, Outcome 3 Ectopic pregnancy rate.
6.4. Analysis.
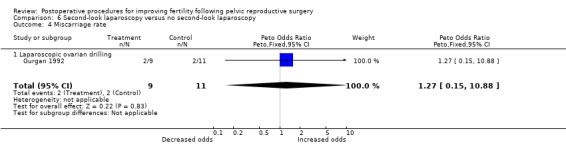
Comparison 6 Second‐look laparoscopy versus no second‐look laparoscopy, Outcome 4 Miscarriage rate.
6.5. Analysis.
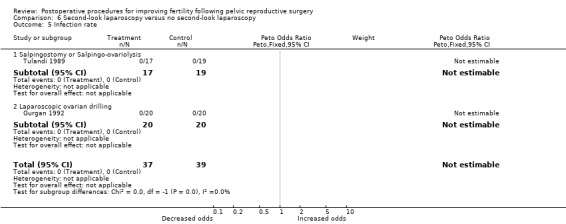
Comparison 6 Second‐look laparoscopy versus no second‐look laparoscopy, Outcome 5 Infection rate.
6.6. Analysis.
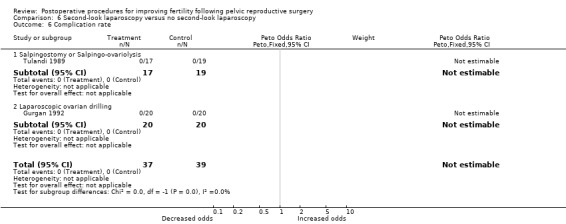
Comparison 6 Second‐look laparoscopy versus no second‐look laparoscopy, Outcome 6 Complication rate.
6.7. Analysis.
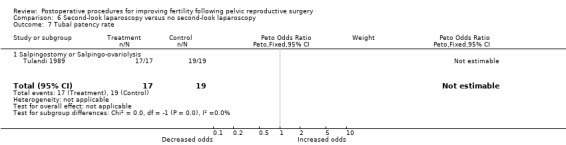
Comparison 6 Second‐look laparoscopy versus no second‐look laparoscopy, Outcome 7 Tubal patency rate.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Comninos 1977.
| Methods | Randomised trial (method not stated) Time of randomisation: not stated 30 women analysed No withdrawals after randomisation ‐ stated At least 24‐month follow up | |
| Participants | Women with primary or secondary infertility and bilateral distal tubal occlusion undergoing macro surgical salpingostomy covered by antibiotics (not specified). Age range 21‐30 years (mean not stated), duration of infertility 2‐4 years (mean not stated). Infertility work‐up revealed no other cause of infertility and included semen analysis, PCT, basal body temperature charting, cervical mucus examination, endometrial biopsy, HSG +/‐ laparoscopy. All women had had prior attempts at therapeutic hydrotubation with normal saline containing 50mg of hydrocortisone and 500mg of ampicillin four times over each of three cycles. Women with fibroids, endometriosis or ovarian cysts were excluded prior to randomisation. The trial was carried out at Marika Eliadi Maternity Hospital, Athens, Greece. Timing and duration not stated. | |
| Interventions | Early postoperative hydrotubation on days 3, 5 and 7 (using normal saline with 50mg hydrocortisone but no antibiotics) versus intraoperative insertion of prosthesis (Cognat's device) followed by postoperative transabdominal peritubal irrigation via the device on days 3, 5 and 7 (using normal saline with 50mg hydrocortisone and antibiotics ‐ not specified) followed by late postoperative hydrotubation (using normal saline with 50mg hydrocortisone but no antibiotics) following removal of the prosthesis on day 12 | |
| Outcomes | Outcomes of relevance to this review:
Total pregnancy rate (per woman)
Ectopic pregnancy rate (per woman)
Miscarriage rate (per intrauterine pregnancy)
Method of diagnosis of pregnancy ‐ not stated
Tubal patency rate (of at least 1 fallopian tube, per woman; assessed by HSG, or laparoscopy in some patients, during the first cycle after surgery) Other outcomes: Total number of pregnancies and total number of live births in each group ‐ some women had more than one pregnancy |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Study stated as randomised. |
| Allocation concealment? | Unclear risk | Not stated within text. |
| Blinding? All outcomes | Unclear risk | Not stated within text. |
| Incomplete outcome data addressed? All outcomes | Low risk | |
| Free of selective reporting? | Low risk | |
| Free of other bias? | Low risk | |
Gurgan 1992.
| Methods | Truly randomised (table of random numbers) Time of randomisation: after initial laparoscopic ovarian drilling 40 women randomised 1 woman declined treatment after the randomisation ‐ excluded from the analysis in the original study 6‐month follow up | |
| Participants | Women with polycystic ovarian syndrome resistant to clomiphene who underwent laparoscopic ovarian laser drilling. Mean age 25.2 years (range 21‐31 years), mean duration of infertility 4.4 years. 33 women had primary and 7 had secondary infertility. Infertility work up consisted of semen analysis (normal in 36 men and mildly oligo‐asthenospermic in 4 men) and normal HSG. No exclusion criteria prior to randomisation stated. The trial was carried out in 1991 at the University of Hecettepi, Ankara, Turkey, recruitment taking 6 months. | |
| Interventions | Postoperative second‐look laparoscopy and adhesiolysis 3‐4 weeks following surgery versus no second‐look laparoscopy | |
| Outcomes | Outcomes of relevance to this review:
Total pregnancy rate (per woman)
Live birth plus ongoing pregnancy rate (per woman)
Ectopic pregnancy rate (per woman)
Method of diagnosis of pregnancy: serum beta hCG levels and real time ultrasound
Miscarriage rate (per intrauterine pregnancy) Other outcomes: Ovulation rate (per woman) Multiple pregnancy rate (per pregnancy) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Random number tables. |
| Allocation concealment? | Low risk | Opaque envelopes. |
| Blinding? All outcomes | Unclear risk | Not stated within text. |
| Incomplete outcome data addressed? All outcomes | Low risk | |
| Free of selective reporting? | Low risk | |
| Free of other bias? | Low risk | |
Rock 1984.
| Methods | Truly randomised (pack of cards) Time of randomisation not stated 206 women analysed No withdrawals after randomisation stated 24‐months follow up | |
| Participants | Women with primary or secondary infertility and distal tubal disease. All women underwent bilateral salpingoneostomy of fimbrioplasty (unilateral if only 1 residual tube). Mean age 28 years (all women were under 36 years old), mean duration of infertility 12 years (range 1‐19 years). The infertility work up consisted of semen analysis, PCT, documentation of ovulation (method not stated), HSG and laparoscopy (90% of women). No exclusion criteria prior to randomisation stated. The trial was multicentre (5 centres) carried out from Jan 1978 to Dec 1981 in the USA (Baltimore, Brooklyn, Durham), Netherlands (Amsterdam) and Colombia (Bogota). | |
| Interventions | Postoperative hydrotubation on 1st, 2nd and 3rd postoperative days and on the day of discharge home with 50mls Ringer's lactate versus 50ml Ringers lactate with 150mg hydrocortisone versus no hydrotubation | |
| Outcomes | Outcomes of relevance to this review: Total pregnancy rate (per woman) Live birth rate (per woman) Miscarriage rate (per woman; rate per intrauterine pregnancy extrapolated) Ectopic pregnancy rate (per woman) Method of diagnosis of pregnancy ‐ not stated Infection and complication rates (per woman) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | A pack of cards. |
| Allocation concealment? | Unclear risk | Not stated within text. |
| Blinding? All outcomes | Unclear risk | Not stated within text. |
| Incomplete outcome data addressed? All outcomes | Low risk | |
| Free of selective reporting? | Unclear risk | Unequal numbers randomised into each group could represent deliberate unequal randomisation. |
| Free of other bias? | Low risk | |
Soihet 1974.
| Methods | Randomised trial (method not stated) Time of randomisation ‐ not stated 258 women analysed No withdrawals after randomisation stated Duration of follow up ‐ not stated | |
| Participants | Women with primary or secondary infertility with tubal immobility or occlusion. All women underwent tubal surgery involving cuff salpingostomy, tubal reanastomosis, tubal reimplantation, adhesiolysis or any combination of the above, in addition to ventrosuspension, by laparotomy. The procedure was covered by intraperitoneal instillation of chloramphenicol or penicillin and the same antibiotics systemically for 5 days. Mean age and mean duration of infertility not specified. Infertility work up not stated. No exclusion criteria prior to randomisation stated. The trial was carried out at San Marcos University, Lima, Peru. Timing and duration of trial not stated. | |
| Interventions | Early postoperative hydrotubation (solution not specified) twice weekly from day 5 to 6 weeks versus late postoperative hydrotubation twice weekly from weeks 6‐12 where the surgery had included Teflon stenting of the fallopian tubes (removed electively after 6 weeks) versus late postoperative hydrotubation twice weekly from week 6‐12 with a solution containing gentamicin where the surgery included tubal suspension in addition to Teflon tube stenting of the fallopian tubes (removed electively after 6 weeks) | |
| Outcomes | Outcomes of relevance to this review:
Pregnancy or live birth rate (per woman)
Ectopic pregnancy rate (per woman)
Method of diagnosis of pregnancy: term delivery
Tubal patency rate (of at least 1 fallopian tube, per woman)
Infective morbidity rate (per woman) Other outcomes: Bilateral tubal obstruction rate (per woman) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Study stated as randomised. |
| Allocation concealment? | Unclear risk | Not stated within text. |
| Blinding? All outcomes | Unclear risk | Not stated within text. |
| Incomplete outcome data addressed? All outcomes | Low risk | |
| Free of selective reporting? | Unclear risk | Unequal numbers randomised into each group could represent deliberate unequal randomisation. |
| Free of other bias? | Low risk | |
Tulandi 1989.
| Methods | Truly randomised (computer‐generated random numbers) Time of randomisation: 1 year after initial surgery 74 women randomised Some women lost to follow up after randomisation ‐ taken into account in life‐table analysis Duration of follow up: 36 months | |
| Participants | Women who had failed to conceive within 12 months of undergoing tubal microsurgery with instillation of 32% dextran (38 had salpingo‐ovariolysis and 36 bilateral terminal salpingostomy). Mean age 30 years, duration of infertility at least 1 year prior to initial surgery. Other than tubal factor, further infertility work‐up (semen analysis, endometrial biopsy, luteal phase progesterone) was normal. HSG performed preoperatively in all women. Women with endometriosis were excluded from entry into the study. The trial was carried out over 2 years from 1986‐1988 at the Fertility Centre, McGill University, Montreal, Canada. | |
| Interventions | Laparoscopic tubal patency testing +/‐ laparoscopic adhesiolysis where indicated versus no laparoscopy 12 months after initial tubal microsurgery | |
| Outcomes | Outcomes of relevance to this review: Cumulative probability of pregnancy, live birth and ectopic pregnancy at 12, 24 and 36 months ‐ rates per woman could be calculated Method of diagnosis of pregnancy: urine pregnancy test and ultrasound Ectopic pregnancy rate Tubal patency rate (of at least 1 fallopian tube, per woman) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Computer generated random number tables. |
| Allocation concealment? | Low risk | Opaque envelopes. |
| Blinding? All outcomes | Unclear risk | Not stated within text. |
| Incomplete outcome data addressed? All outcomes | Low risk | |
| Free of selective reporting? | Low risk | |
| Free of other bias? | Low risk | |
HSG hysterosalpingogram
PCT postcoital test
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Alborzi 2003 | The study was quasi‐randomised. |
Differences between protocol and review
The search string was redesigned.
Contributions of authors
James Duffy 2008 update: Drafting of the update, performed and assessed the search strategy, updated the review as required.
Neil Johnson Original review: Primary author, involved in every step of the review. 2008 update: Supervised the drafting of the update, provided advice as required, proof reading of the final draft.
Gaity Ahmad 2008 update: Drafting of the update, performed and assessed the search strategy, updated the review as required.
Andrew Watson Original review: Involved with initial draft of the protocol, selection of trials for inclusion in the review, quality assessment of included trials, data extraction and proof reading the final draft. 2008 update: Supervised the drafting of the update, provided advice as required, proof reading of the final draft.
Declarations of interest
None known
Edited (no change to conclusions)
References
References to studies included in this review
Comninos 1977 {published data only}
- Comninos AC. Salpingostomy: results of two different methods of treatment. Fertility and Sterility 1977;28:1211‐4. [PubMed] [Google Scholar]
Gurgan 1992 {published data only}
- Gurgan T, Urman B, Aksu T, Yarali H, Develioglu O, Kisnisci H. The effect of short‐interval laparoscopic lysis of adhesions on pregnancy rates following Nd‐YAG laser photocoagulation of polycystic ovaries. Obstetrics and Gynecology 1992;80:45‐7. [PubMed] [Google Scholar]
Rock 1984 {published data only}
- Rock JA, Siegler AM, Meisel MB, Haney AF, Rosenwaks Z, Pardo‐Vargas F, et al. The efficacy of postoperative hydrotubation: a randomized prospective multicenter clinical trial. Fertility and Sterility 1984;42:373‐6. [DOI] [PubMed] [Google Scholar]
Soihet 1974 {published data only}
- Soihet S. Three comparative techniques on tubo‐plasty. International Journal of Fertility 1974;19:111‐5. [PubMed] [Google Scholar]
Tulandi 1989 {published data only}
- Tulandi T, Falcone T, Kafka I. Second‐look laparoscopy one year following reproductive surgery. Fertility and Sterility 1989;52:421‐4. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Alborzi 2003 {published data only}
- Alborzi S, Motazedian S, Parsanezhad ME. Chance of adhesion formation after laparoscopic salpingo‐ovariolysis: Is there a place for second‐look laparoscopy?. Journal of the American Association of Laparoscopists 2003;10(2):172‐6. [DOI] [PubMed] [Google Scholar]
Additional references
Arronet 1969
- Arronet GH, Eduljee SY, O'Brien JR. A nine‐year survey of fallopian tube dysfunction in human infertility: diagnosis and therapy. Fertility and Sterility 1969;20:903‐18. [DOI] [PubMed] [Google Scholar]
DeCherney 1984
- DeCherney AH, Mezer HC. The nature of posttuboplasty pelvic adhesions as determined by early and late laparoscopy. Fertility and Sterility 1984;41:643‐6. [DOI] [PubMed] [Google Scholar]
DiZerega 2003
- DiZerega GS, Roth R, Johns DB. Quantitation of peritoneal adhesions and correlation with clinical outcomes. Infertility and Reproductive Medicine Clinics of North America 2003;14(3):431‐56. [Google Scholar]
Gillett 1994
- Gillett WR, James C, Jetha N, McComb PF. Removal of the ovarian surface epithelium from the rabbit ovary ‐ a cause of adhesions following a standard injury. Human Reproduction 1994;9:497‐500. [DOI] [PubMed] [Google Scholar]
Gomel 1986
- Gomel V, Taylor PJ. Surgical endoscopy. In: Gomel V, Taylor PJ, Yuzpe AA, Rioux JE editor(s). Laparoscopy and hysteroscopy in gynecologic practice. Chicago: Yearbook Medical Publishers, 1986:p158. [Google Scholar]
Grant 1971
- Grant A. Infertility surgery of the oviduct. Fertility and Sterility 1971;22:496‐503. [PubMed] [Google Scholar]
Higgins 2008
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.0 [updated February 2008]. The Cochrane Collaboration, 2008. Available from www.cochrane‐handbook.org..
Jansen 1988
- Jansen RP. Early laparoscopy after pelvic operations to prevent adhesions: safety and efficacy. Fertility and Sterility 1988;49:26‐31. [PubMed] [Google Scholar]
Jessen 1971
- Jessen H. Forty‐five operations for sterility. Acta Obstetricia et Gynecologica Scandinavica 1971;50:105‐15. [DOI] [PubMed] [Google Scholar]
Luber 1986
- Luber K, Beeson CC, Kennedy JF, Villanueva B, Young PE. Results of microsurgical treatment of tubal infertility and early second‐look laparoscopy in the post‐pelvic inflammatory disease patient: implications for in vitro fertilisation. American Journal of Obstetrics and Gynecology 1986;154:1264‐70. [DOI] [PubMed] [Google Scholar]
Novy 1995
- Novy MJ. Tubal surgery or IVF ‐ making the best choice in the 1990s. International Journal of Menopausal Studies 1995;40:292‐7. [PubMed] [Google Scholar]
Raj 1982
- Raj SG, Hulka JF. Second‐look laparoscopy in infertility surgery: therapeutic and prognostic value. Fertility and Sterility 1982;38:325‐9. [PubMed] [Google Scholar]
Reich 1987
- Reich H. Laparoscopic treatment of extensive pelvic adhesions, including hydrosalpinges. Journal of Reproductive Medicine 1987;32:472‐5. [PubMed] [Google Scholar]
Rock 1978
- Rock JA, Katayama KP, Martin EJ, Woodruff JD, Jones HW Jr. Factors influencing the success of salpingostomy techniques for distal fimbrial obstruction. Obstetrics and Gynecology 1978;52:591‐6. [PubMed] [Google Scholar]
Strandell 1995
- Strandell A, Bryman I, Janson PO, Thorburn J. Background scoring systems in relation to pregnancy outcome after fertility surgery. Acta Obstetricia et Gynecologica Scandinavica 1995;74:281‐7. [DOI] [PubMed] [Google Scholar]
Surrey 1982
- Surrey MW, Friedman S. Second‐look laparoscopy after reconstructive pelvic surgery for infertility. Journal of Reproductive Medicine 1982;27:658‐60. [PubMed] [Google Scholar]
Trimbos‐Kemper 1985
- Trimbos‐Kemper TCM, Trimbos JB, Hall EV. Adhesion formation after tubal surgery: results of the eighth‐day laparoscopy in 188 patients. Fertility and Sterility 1985;43:395‐400. [DOI] [PubMed] [Google Scholar]
Tulandi 1990
- Tulandi T, Collins JA, Burrows E, Jarrell JF, McInnes RA, Wrixton W, Simpson CW. Treatment‐dependent and treatment‐independent pregnancy among women with periadnexal adhesions. American Journal of Obstetrics and Gynecology 1990;162:354‐7. [DOI] [PubMed] [Google Scholar]
Vandekerckhove 1998
- Vandekerckhove P, Watson A, Lilford R, Harada T, Hughes E. Oil‐soluble versus water‐soluble media for assessing tubal patency with hysterosalpingography or laparoscopy in subfertile women. Cochrane Database of Systematic Reviews 1998, Issue 3. [DOI: 10.1002/14651858.CD000092.] [DOI] [PubMed] [Google Scholar]
Winston 1991
- Winston RM, Margara RA. Microsurgical salpingostomy is not an obsolete procedure. British Journal of Obstetrics and Gynaecology 1991;98:637‐42. [DOI] [PubMed] [Google Scholar]


