Abstract
Purpose
To determine the effect of coffee on the stainability of CAD/CAM ceramics after different surface treatment protocols.
Methods
Ninety specimens (2 mm × 10 mm) of CAD/CAM ceramic materials (Vitablocs Mark II, VITA Enamic, and VITA Suprinity) were prepared. The specimens were subdivided (n = 10) into three groups: G1: Glazed (control group), G2: Subjected to finishing and polishing, and G3: Re-glazed after finishing and polishing. The surface treatment was performed using a diamond polishing system for porcelain (Diapol) followed by applying a diamond polishing paste (Diapolisher). The specimens were immersed in distilled water for 24 h, and the baseline color measurement after finishing and polishing was recorded. Each group was then immersed in a staining solution (coffee) for one week, and the second color measurement was recorded.
Results
The color of the CAD/CAM ceramic materials in the finishing and polishing groups changed significantly after staining (P < 0.05). Statistically significant differences were noticed after staining in the polished groups of Vita Enamic and Vita Suprinity compared with the glazed group (control). However, the color change between the re-glazed and control groups was insignificant for all the materials (P > 0.05). Although the color change values of the three CAD/CAM materials increased, these changes were within the clinically acceptable value (ΔE < 3.3).
Conclusion
Staining of the tested CAD/CAM ceramic materials increased the color change values within the clinically acceptable range in all the groups, with the highest values found after finishing and polishing. Re-glazing is recommended after surface adjustment for all the tested materials to increase their resistance to staining.
Keywords: CAD/CAM, Ceramics, Color stability, Surface treatment, Stainability
1. Introduction
Dental ceramics are one of the most common restorations owing to their advantages such as good esthetics, the ability to produce smooth surfaces (which minimizes plaque adherence and subsequent periodontal inflammation), and biocompatibility (Rosenblum and Schulman, 1997, Leinfelder, 2000, Dalkiz et al., 2009). Several classifications of dental ceramics have been made. They can be categorized in terms of their microstructure (i.e., the amount and type of crystalline phase and glass composition). Although the microstructures of the materials differ, the basic compositional categories are glass-based systems (mainly silica), glass-based systems (mainly silica) with fillers, crystalline (leucite or lithium disilicate), crystalline-based systems with glass fillers (mainly alumina), and polycrystalline solids (alumina and zirconia). These materials can be processed using different techniques. A simpler way to classify the ceramics used in dentistry is in terms of their processing method (power-liquid, pressed, or machined) (Wright et al., 2004).
Dental restorations that mimic all the characteristics of natural teeth are esthetically pleasing; dentists can provide such restorations owing to the transmission property of light (Mclaren and Cao, 2009). Tooth-colored dental materials made using computer-aided design/computer-aided manufacturing (CAD/CAM) are currently very popular in esthetic dentistry. The CAD/CAM technology was mainly developed to resolve three challenges: to ensure a suitable material strength, attain restorations with natural appearance, and to prepare easier, faster, and more accurate restorations (van der Burgt et al., 1990, Pop-Ciutrila et al., 2016). CAD/CAM systems have been improved to be chemically stable, esthetic, and biocompatible (Miyazaki et al., 2009); they can overcome brittleness and reduced longevity due to decreased crystalline content or filler particles of regular ceramics (Kelly and Benetti, 2011, Denry and Kelly, 2014).
Prefabricated blocks of ceramics (feldspathic, leucite, lithium disilicate, and blocks containing zirconia or alumina materials) are milled to create tooth-colored restorations (van der Burgt et al., 1990). Many factors have been reported to influence the definitive color of dental ceramic restorations, such as surface spectral reflectance, thickness, translucency, and the underlying cement (Pecho et al., 2015, Touchstone et al., 2010, Van Zeghbroeck, 2012). After placing a restoration, inadequate color stability and/or staining may be reasons for a clinician to renew it. The shade of the finished restorations must remain satisfactory even after a long time (Touchstone et al., 2010). Finishing and polishing may influence the color of porcelain (Sarac et al., 2006, Yılmaz et al., 2008, Atay et al., 2009). Rough porcelain surfaces are more susceptible to staining than smoother porcelain surfaces (Yılmaz et al., 2008, Atay et al., 2009). Kim et al. (2003) stated that rough or irregularly textured surfaces influence the color of porcelain by reflecting an irregular and diffuse pattern of light, which changes the color of the restoration.
An optimum restoration is necessary to prevent any mechanical or bacterial damage to tooth or surrounding tissues. Silness (1980) reported that preserving healthy tissues around a crown may prevent inflammation and the consequences that might affect the longevity of the abutment teeth. Adjustment of the ceramic restoration is necessary for correcting contour and height and for esthetic improvements. The surface of a ceramic restoration will retain glaze unless dentists need to perform clinical adjustments to improve the appearance, correct occlusal interference, and finish the margins. Consequently, removing the super facial glazing layer increases the surface roughness, thus leading to an unsatisfactory restoration. To minimize color change and improve the translucency of restorations, various surface finishing protocols can be used (Jagger and Harrison, 1994).
Previous studies evaluated the influence of common beverages on the color stability of CAD/ CAM materials. Sarikaya et al. (2018) found that among beverages, coffee causes the most staining on hybrid ceramic and resin nanoceramic surfaces. Saba et al. (2017) showed that coffee may adversely affect the color and microhardness of Vita Enamic and Vitablocs Mark II, thus compromising the esthetics. To the best of the authors’ knowledge, studies on the color stability of CAD/CAM restorations after adjustments are limited. The aim of this study was to determine the effect of coffee on the stainability of CAD/CAM ceramics after different surface treatment protocols. The null hypothesis was that finishing and polishing have no effect on the stainability of CAD/CAM ceramic materials.
2. Materials and methods
2.1. Specimen fabrication
In this study, frequently used and commercially available ceramic materials were tested. Table 1 lists the ceramic type, shade, material composition, and the names of manufacturers. A total of 90 disc-shaped specimens (2 mm × 10 mm) were fabricated from different CAD/CAM ceramic blocks [Vitablocs Mark II, VITA Enamic, and Vita Suprinity] (Vita Zahnfabrik, Bad Sȁckingen, Germany). The disk thickness was made approximately 2.0 mm for ease of manipulation and polishing (Sarikaya and Guler, 2010, Kursoglu et al., 2014, Steiner et al., 2015). The specimens were prepared using a dental milling machine (DentalCAM, vhf Inc., Hauppauge, NY). The specimens were randomly subdivided into three equal groups (n = 10) according to the surface treatment protocol:
Table 1.
CAD/CAM ceramic blocks used in this study.
| Material Type | Shade | Composition by weight |
Manufacturer | |
|---|---|---|---|---|
| Filler | Polymer | |||
| Vitablocs Mark II Feldspathic ceramic block | 2M2C | 30% Fine particle feldspar ceramic | Vita Zahnfabrik, Germany | |
| Vita Enamic Polymer infiltrated ceramic network | 2M2-T | 86% ceramic | 14% UDMA + TEGGDMA | Vita Zahnfabrik, Germany |
| Vita Suprinity Zirconia reinforced lithium silicate glass ceramic | 2M2-HT | 8–12% ZrO2 (zirconia), 56–64% SiO2 (silicon dioxide), 15–21% Li2O (lithium oxide), 0.1% La2O3 (lanthanum oxide), Pigments < 10%, Various > 10% |
Vita Zahnfabrik, Germany | |
G1: Glazed/not subjected to finishing or polishing (control group).
G2: Subjected to finishing and polishing.
G3: Re-glazed after finishing and polishing.
2.2. Finishing and polishing
The surface finishing and polishing were performed using a diamond polishing system for porcelain (Diapol, EVE Emst Vetter GmbH, Germany) in a sequence of decreasing abrasiveness with intermittent movements as suggested by the manufacturer. This started with a green polisher for grinding and shaping. A blue coarse polisher was then used for smoothening, followed by a pink medium for pre-polishing, followed by a white fine for high shine polishing. A diamond polishing paste was applied using a Buff disc (Super Snap Buff Discs; Shofu Inc., Quioto, Japan) for a final high luster polishing. This procedure was performed using a straight hand piece with a low speed of 10.000 rpm according to manufactural instructions and at a moderate pressure with a specific angle controlled by the customized holder. The grinding and finishing of the material were performed for 15 s for each step, and the polishing paste was applied for 20 s. The glazing and re-glazing of the ceramic surfaces were performed using Vita Akzent Plus Glaze (Vita Zahnfabrik) for Vitablocs Mark II and Vita Suprinity. Vita Enamic Glaze (Vita Zahnfabrik) was used for the Vita Enamic material. These were performed according to the manufacturer instructions for each material. The specimens were stored in distilled water for 24 h at 37 °C, and the baseline color measurement was recorded.
After finishing and polishing, all the specimens were immersed in coffee, which is a frequently consumed beverage. The immersion was performed in 15 gm of coffee (Coffee Nescafé Classic1, Nestlé, Spain) dissolved in 500 ml of water for 15 min at 37 °C followed by rinsing for 10 s and drying with a paper towel. Staining was performed daily for one week, and the color measurement was recorded.
2.3. Color measurements
The color measurements were recorded after finishing and polishing of the specimens and after staining in coffee to assess the color change in the polished specimens. Three color measurements were taken for each specimen using a spectrophotometer (LabScan® XE, Hunter Associates Laboratory Inc., Reston, VA) with a black background to mimic the clinical environment, under a standard D65 illumination. The color change (ΔE) of each specimen was calculated using the following equation:
The CIE L* measures the lightness of a material, CIE a* measures the redness (positive value) or greenness (negative value), and CIE b* measures the yellowness (positive value) or blueness (negative value). It has been reported that a change in color can be unnoticeable by human eyes when ΔE < 1; when 1.0 < ΔE < 3.3, only a skilled individual can notice the change, and the values in this range are considered clinically acceptable, whereas when ΔE > 3.3, the color change can be easily detected and is considered clinically unacceptable (Hunter, 1975, Kuenhi and Marcus, 1979, Ardu et al., 2010).
2.4. Statistical analysis
Two-way repeated measure analysis of variance (ANOVA), one-way ANOVA, Tukey post hoc test, and paired t-test were used for statistics analysis. The statistical analysis were conducted at a significance level of P < 0.05. The statistical tests were completed using the SPSS 21.0 program (SPSS Inc., Chicago, IL, USA).
3. Results
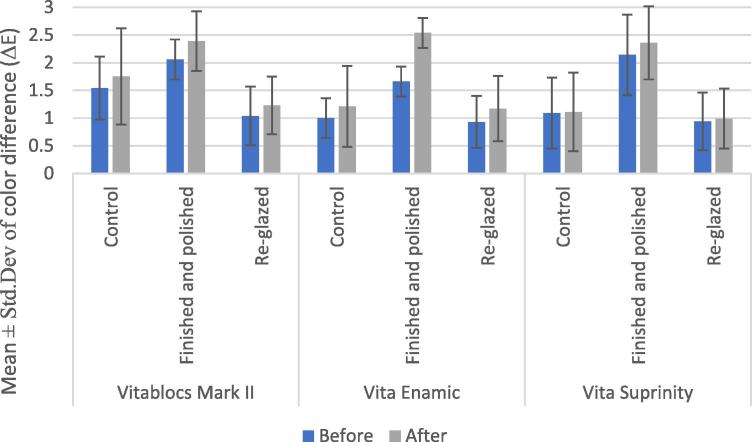
Table 2 lists the mean (ΔE) and standard deviation (SD) of the color change value before and after staining of the ceramic materials. The results show an increase in the color change value after staining, with the highest mean of ΔE observed within the groups subjected to finishing and polishing, ranging from 2.36 to 2.54 for all the three ceramic materials. Fig. 1 shows the mean of the color change values for the ceramic materials within each subgroup before and after staining.
Table 2.
Mean and standard deviation of color change for each CAD/CAM ceramic material before and after staining.
| Material | Tested groups | Mean ± Std.Dev of (ΔE) before staining | Mean ± Std.Dev of (ΔE) after staining |
|---|---|---|---|
| Vitablocs Mark II | Control | 1.54 ± 0.57 | 1.75 ± 0.87 |
| Finished and polished | 2.06 ± 0.36 | 2.39 ± 0.54 | |
| Re-glazed | 1.04 ± 0.53 | 1.23 ± 0.52 | |
| Vita Enamic | Control | 1.00 ± 0.36 | 1.21 ± 0.73 |
| Finished and polished | 1.66 ± 0.27 | 2.54 ± 0.27 | |
| Re-glazed | 0.93 ± 0.47 | 1.17 ± 0.59 | |
| Vita Suprinity | Control | 1.09 ± 0.64 | 1.11 ± 0.71 |
| Finished and polished | 2.14 ± 0.73 | 2.36 ± 0.66 | |
| Re-glazed | 0.94 ± 0.52 | 0.99 ± 0.54 | |
Fig. 1.
Mean and standard deviation (Std.Dev) of color differences of each material before and after staining.
The two-way repeated measure ANOVA (Table 3) showed significant differences in time, interaction between time and materials, and the interaction between time and surface treatment protocols (P < 0.05). However, no significant differences were found in the interaction between the three factors. The one-way ANOVA and Tukey post hoc test for multiple comparisons showed that there is a significantly greater color change in the polished group compared with the re-glazed groups for all the materials after staining (P < 0.05). On the other hand, there was no significant color change between the control and re-glazed groups (P > 0.05). A significant increase in the color change value was also noticed after staining in the polished groups of Vita Enamic and Vita Suprinity compared with the control. In Vitablocs Mark II, staining did not cause any significant change in the color of the polished and re-glazed groups compared with the control group (P > 0.05). The paired t-test showed that staining in all the ceramic materials significantly increases after finishing and polishing (P < 0.05).
Table 3.
Two-way repeated measure ANOVA results for stainability of CAD/CAM ceramic materials after different surface treatment protocols.
| Source | Type III Sum of Squares | df | Mean Square | F | Sig. |
|---|---|---|---|---|---|
| Time | 3.08 | 1.000 | 3.08 | 22.63 | 0.00 |
| Time * Materials | 0.90 | 2.000 | 0.45 | 3.32 | 0.04 |
| Time * Subgroups | 1.04 | 2.000 | 0.52 | 3.82 | 0.03 |
| Time * Materials * Subgroups | 0.56 | 4.000 | 0.14 | 1.04 | 0.39 |
| Error | 11.03 | 81.00 | 0.14 |
4. Discussion
Esthetics is one of the main aspects to be considered when choosing the appropriate restorative material. The CAD/CAM ceramics evaluated in this study have been used clinically in the construction of anterior or posterior crowns, inlays, and onlays. CAD/CAM restorative materials have been successfully introduced in clinical dentistry. Recent reports have demonstrated their excellent hardness (Colombo et al., 2019) and optical characteristics (Della Bona et al., 2015). These materials allow a completely digital workflow, from impression to final framework, with clinical reliability (Alessandretti et al., 2017) and good patient feedback (Sfondrini et al., 2018). The optical properties of ceramic materials are affected by their microstructure, fabrication process, chemical composition, and properties of polycrystalline ceramics such as the crystalline content, particle size, homogeneity, refractive index, and porosity (Della Bona et al., 2014, Bahgat et al., 2015).
Discoloration can be assessed visually or by utilizing specified instruments, such as Spectrophotometer, which can reduce subjective errors in color assessment (Bolt et al., 1994). The LabScan XE spectrophotometer, which was used in this study, is advantageous as it can accurately measure optically brightened materials, offer ultraviolet calibration and control of the illumination source, automatically check and adjust to the internal reference standard, and provide excellent inter-instrument agreement. The color change value of the tested materials was obtained with a black background to be more comparable to the oral cavity.
Several studies have evaluated finishing and polishing and glazing techniques in correlation with surface roughness stainability. The surface treatment protocols used in this study have been recommended to produce smooth surfaces. Sasahara et al. (2006) studied the effect of different surface treatment protocols on leucite-based porcelains. They found that discs or rubber followed by applying a diamond paste is the best surface treatment for porcelains. Another recent study concluded that manually polished CAD/CAM ceramics are smoother than glazed feldspathic ceramics in terms of the surface roughness of CAD/CAM and conventional ceramic disks after polishing or glazing (Oliveira-Junior et al., 2013). On the other hand, another study reported good results with the Sof-lex system compared with other polishing techniques used with Vitablocs Mark II and IPS Empress. They found that among all the polishing methods, Sof-Lex discs produced the smoothest surfaces, considered to be even smoother than glazed ones (Flury et al., 2010). However, there is no consensus on the ideal polishing protocol (Kim et al., 2003).
Based on the results of this study, the null hypothesis that different surface treatment procedures had no effect on the stainability of CAD/CAM ceramic materials was rejected. The results showed that finishing and polishing increase the staining compared with the re-glazed groups in all the materials, with the largest stain noticed in Vita Enamic followed by Vitablocs Mark II and Vita Suprinity. This is may be associated with the differences in the composition of each material, which could have resulted in differences in their stain resistance. Vita Enamic is a hybrid ceramic material composed of a dual network structure where the dominant porous sintered feldspathic ceramic network (86 wt%) is strengthened by a methacrylate polymeric network (14 wt%). It combines the properties of both ceramic and resin materials and can be considered a composite material. Moreover, the polymer consists of hydrophobic urethane dimethacrylate (UDMA) and hydrophilic triethylene glycol dimethacrylate (TEGDMA). These may have resulted in greater water sorption and penetration of any hydrophilic colorant into the resin matrix, thus contributing to the higher discoloration values obtained by Vita Enamic (Acar et al., 2016). Previous studies showed that ceramic materials have better color stability than composites (Acar et al., 2016, Gawriolek et al., 2012).
Vitablocs Mark II contain feldspathic crystalline particles embedded in a glassy matrix. Vita Suprinity is a Zirconia-reinforced lithium silicate glass ceramic, which combines zirconia particles and silicon dioxide with lithium oxide ceramic particles. The difference in the composition may be the reason for the difference in their stain resistance. In this study, Vita Suprinity showed the highest stain resistance among the other materials. This is in agreement with Alp et al. (2018) who studied zirconia-reinforced lithium silicate glass-ceramic and lithium disilicate glass-ceramic with two surface treatments (finishing and glazing) followed by coffee thermocycling. They found a lower level of color change with polished zirconia-reinforced ceramic (Vita Suprinity), explained by their fine, rod-like small crystalline particles, and homogeneous structure, resulting in a higher color stability.
The results showed that staining of Vitablocs Mark II did not cause any significant change in the color of the polished and re-glazed groups compared with the control group. This was in agreement with Sarikaya and Guler, 2010 who studied different feldspathic ceramics (VMK 95, Ceramco III, Matchmaker MC, Vitablocs Mark II) with different surface finishing tools and reported that feldspathic porcelain block Mark II shows a lower roughness value than the other porcelain materials, without significant differences between the different polishing techniques because of the extreme hardness of the material. However, Schürmann and Olms, 2018 compared the shade stability of a polymer-infiltrated ceramic (Vita Enamic) and a resin nano ceramic (Lava Ultimate) with a conventional feldspar ceramic (Vitablocs Mark II) and an acrylate polymer (CAD-Temp). They concluded that Vitablocs Mark II was stained by coffee more significantly than Vita Enamic.
There was no significant color change between the glazed and re-glazed groups of all the materials. This is consistent with that reported by Kilinc and Turgut (2018) who studied different CAD/CAM materials (Cerasmart, Lava Ultimate, Vita Enamic, Vita Suprinity, and Vitablocs Mark II) and different surface finishing techniques and found no statistically significant differences between the ΔE values of the control and re-glazed groups of the Vita Suprinity and Vitablocs Mark II specimens.
The results showed a significant increase in staining in all the finishing and polishing groups regardless of the material type. This could be attributed to the microscopic surface roughness as noticed by Al-Wahadni and Martin, 1998 in their review of studies that examined the visual and microscopic appearance and roughness of glazed, unglazed, and polished porcelain surfaces using scanning electron microscopy or surface profilometry; most studies agreed that glazed porcelain provides a smoother surface compared with polishing treatment. Moreover, staining can be attributed to coffee immersion, as coffee contains approximately 22 types of acids including citric acid, acetic acid, malic acid, and other high-molecular weight acids (Engelhardt and Maier, 1985). This acidity can cause chemical erosion, leading to ceramic material stainability (Kim et al., 2003). Moreover, the discoloration by coffee could be due to the adsorption and absorption properties of ceramics and infiltration of stains into the organic phase of the ceramic materials (Um and Ruyter, 1991, Fasbinder and Neiva, 2016).
An increase in the color change value was also noticed after staining in the polished groups of Vita Enamic and Vita Suprinity compared with the glazed group (control). This is in agreement with Kanat-Ertürk (2019) who studied zirconia-reinforced lithium silicate ceramic in three groups: glazed, mechanical polishing, and external staining and glaze, and subsequently subjected them to tea and coffee in storage periods of 1 week, 2 weeks, 1 month, and 2 months. The results showed that for the zirconia-reinforced ceramic, the glaze procedure had lower ΔE values than mechanical polishing. Our findings were in contrast to those reported by Özarslan et al. (2016) who found that finishing and polishing VITA Enamic restorations using a clinical and technical kit [silicon carbide pink rubber disc, grey] results in smoother material surfaces instead of glazing; this could be due to the differences in the polishing techniques used in this study.
Although the results showed that staining of the tested CAD/CAM ceramic materials increases after surface treatment, these changes can be observed only by a skilled person and are considered clinically acceptable (ΔE < 3.3). This was in contrast with another study that reported clinically unacceptable color change of Vitablocs Mark II and Vita Enamic (ΔE = 3.83 and 4.81 respectively) after immersion in coffee. These could be due to the different immersion period (28 days) evaluated in that study (Saba et al., 2017). Another study found that Vitablocs Mark II (ΔE = 1.26) and Vita Suprinity (ΔE = 2.19) had ΔE within the acceptable range for the re-glazed group when compared with the control and finishing groups. With regard to their findings of Vita Enamic, the color change was above the acceptable threshold (ΔE > 3.3) for all the groups but was the lowest when re-glazed (ΔE = 4.64), which could be recommended for better clinical color stability (Kilinc and Turgut, 2018). The differences between the current study and theirs can be mostly attributed to the use of UV aging instead of coffee staining.
One of the limitations of this study is that it was an in vitro study with a short immersion time, which could have limited the efficacy of the staining. Including more staining solutions in comparison with coffee could affect the clinical preference of CAD/CAM ceramics. Moreover, the material was stained on both surfaces; this is different to the clinical situation in which the material is bonded to the tooth structure. The effect of surface roughness on the color changes of the CAD/CAM ceramics should be explored and correlated with spectrophotometer results. Different results can be expected with different types of porcelain and polishing protocols.
5. Conclusion
Following are the conclusions drawn based on the findings of this in vitro study:
-
1.
The tested CAD/CAM materials exhibited increased color change value after staining in all surface treatment groups, with the highest values found after finishing and polishing.
-
2.
Vita Enamic exhibited the highest staining potential values, followed by Vitablocs Mark II and Vita Suprinity. However, all the materials showed clinically satisfactory color change values.
-
3.
Re-glazing is recommended after a surface adjustment for all the tested materials to increase the resistance to staining.
Ethical statement
The author has no ethical issue to declare.
Acknowledgments
Acknowledgment
The authors are grateful to the College of Dentistry Research Center and would like to extend their appreciation to Deanship of Scientific Research at King Saud University for funding this work (URSP-4-19-95) through the Undergraduate Student’s Research Support Program.
Declaration of Competing of Interest
The authors have no conflict of interest to declare.
Footnotes
Peer review under responsibility of King Saud University.
References
- Acar O., Yilmaz B., Altintas S.H., Chandrasekaran I., Johnston W.M. Color stainability of CAD/CAM and nanocomposite resin materials. J. Prosthet. Dent. 2016;115(1):71–75. doi: 10.1016/j.prosdent.2015.06.014. [DOI] [PubMed] [Google Scholar]
- Alessandretti R., Borba M., Benetti P., Corazza P.H., Ribeiro R., Della Bona A. Reliability and mode of failure of bonded monolithic and multilayer ceramics. Dent. Mater. 2017;33(2):191–197. doi: 10.1016/j.dental.2016.11.014. [DOI] [PubMed] [Google Scholar]
- Alp G., Subasi G., Johnston W.M. Effect of surface treatments and coffee thermocycling on the color and translucency of CAD-CAM monolithic glass-ceramic. J. Prosthet. Dent. 2018;120(2):263–268. doi: 10.1016/j.prosdent.2017.10.024. [DOI] [PubMed] [Google Scholar]
- Al-Wahadni A., Martin D.M. Glazing and finishing dental porcelain: a literature review. J. Can. Dent. Assoc. 1998;64(8):580–583. [PubMed] [Google Scholar]
- Ardu S., Braut V., Gutemberg D., Krejci I., Dietschi D., Feilzer A.J. A long-term laboratory test on staining susceptibility of esthetic composite resin materials. Quintessence Inter. 2010;41(8):695–702. [PubMed] [Google Scholar]
- Atay A., Karayazgan B., Ozkan Y., Akyil M.S. Effect of colored beverages on the color stability of feldspathic porcelain subjected to various surface treatments. Quintessence Int. 2009;40(7):e41–e48. [PubMed] [Google Scholar]
- Bahgat S.F.A., Basheer R.R., El Sayed S.M. Effect of zirconia addition to lithium disilicate ceramic on translucency and bond strength using different adhesive strategies. Egypt Dent. J. 2015;61(4):4519–4533. [Google Scholar]
- Bolt R.A., Bosch J.J., Coops J.C. Influence of window size in small-window colour measurement, particularly of teeth. Phys. Med. Biol. 1994;39(7):1133–1142. doi: 10.1088/0031-9155/39/7/006. [DOI] [PubMed] [Google Scholar]
- Colombo M., Poggio C., Lasagna A., Chiesa M., Scribante A. Vickers micro-hardness of new restorative CAD/CAM dental materials: evaluation and comparison after exposure to acidic drink. Mater. 2019;12(8):1246. doi: 10.3390/ma12081246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalkiz M., Sipahi C., Beydemir B. Effects of six surface treatment methods on the surface roughness of a low-fusing and an ultra low-fusing feldspathic ceramic materials. J. Prosthodont. 2009;18(3):217–222. doi: 10.1111/j.1532-849X.2008.00410.x. [DOI] [PubMed] [Google Scholar]
- Della Bona A., Nogueira A.D., Pecho O.E. Optical properties of CAD CAM ceramic systems. J. Dent. 2014;42(9):1202–1209. doi: 10.1016/j.jdent.2014.07.005. [DOI] [PubMed] [Google Scholar]
- Della Bona A., Pecho O.E., Ghinea R., Cardona J.C., Pérez M.M. Colour parameters and shade correspondence of CAD-CAM ceramic systems. J. Dent. 2015;43(6):726–734. doi: 10.1016/j.jdent.2015.02.015. [DOI] [PubMed] [Google Scholar]
- Denry I., Kelly J.R. Emerging ceramic-based materials for dentistry. J. Dent. Res. 2014;93(12):1235–1242. doi: 10.1177/0022034514553627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engelhardt U.H., Maier H.G. Acids in coffee. XI. The proportion of individual acids in the total titratable acid. Z Lebensm Unters Forsch. 1985;181(1):20–23. doi: 10.1007/BF01124801. [DOI] [PubMed] [Google Scholar]
- Fasbinder D.J., Neiva G.F. Surface evaluation of polishing techniques for new resilient CAD-CAM restorative materials. J. Esthet Restor Dent. 2016;28(1):56–66. doi: 10.1111/jerd.12174. [DOI] [PubMed] [Google Scholar]
- Flury S., Lussi A., Zimmerli B. Performance of different polishing techniques for direct CAD/CAM ceramic restorations. Oper Dent. 2010;35(4):470–481. doi: 10.2341/09-373-L. [DOI] [PubMed] [Google Scholar]
- Hunter R.S. New York: Wiley; 1975. The measurement of appearance; pp. 77151–80152. 225, 334. [Google Scholar]
- Gawriolek M., Sikorska E., Ferreira L.F.V., Costa A.I., Khmelinskii I., Krawczyk A., Sikorski M., Koczorowski R. Color and luminescence stability of selected dental materials in vitro. J. Prosthodont. 2012;21(2):112–122. doi: 10.1111/j.1532-849X.2011.00808.x. [DOI] [PubMed] [Google Scholar]
- Jagger D.C., Harrison A. An in vitro investigation into the wear effects of unglazed, glazed, and polished porcelain on human enamel. J. Prosthet. Dent. 1994;72(3):320–323. doi: 10.1016/0022-3913(94)90347-6. [DOI] [PubMed] [Google Scholar]
- Kanat-Ertürk B. Color stability of CAD/CAM ceramics prepared with different surface finishing procedures. J. Prosthodont. 2019:1–7. doi: 10.1111/jopr.13019. [DOI] [PubMed] [Google Scholar]
- Kelly J.R., Benetti P. Ceramic materials in dentistry: historical evolution and current practice. Aust. Dent. J. 2011;56(Suppl 1):85–96. doi: 10.1111/j.1834-7819.2010.01299.x. [DOI] [PubMed] [Google Scholar]
- Kilinc H., Turgut S. Optical behaviors of esthetic CAD-CAM restorations after different surface finishing and polishing procedures and UV aging: An in vitro study. J. Prosthet. Dent. 2018;120(1):107–113. doi: 10.1016/j.prosdent.2017.09.019. [DOI] [PubMed] [Google Scholar]
- Kim I.J., Lee Y.K., Lim B.S., Kim C.W. Effect of the surface topography on the color of dental porcelain. J. Mater. Sci. Mater. Med. 2003;14(5):405–409. doi: 10.1023/a:1023206716774. [DOI] [PubMed] [Google Scholar]
- Kursoglu P., Karagoz Motro P.F., Kazazoglu E. Correlation of surface texture with the stainability of ceramics. J. Prosthet. Dent. 2014;112(2):306–313. doi: 10.1016/j.prosdent.2013.09.028. [DOI] [PubMed] [Google Scholar]
- Kuenhi R.C., Marcus R.T. An experiment in visual scaling of small color differences. Color Res. App. 1979;4(2):83–91. [Google Scholar]
- Leinfelder K.F. Porcelain esthetics for the 21st century. J. Am. Dent. Assoc. 2000;131(Suppl):47S–51S. doi: 10.14219/jada.archive.2000.0402. [DOI] [PubMed] [Google Scholar]
- Mclaren E.A., Cao P.T. Ceramics in dentistry-part I: classes of materials. Inside Dent. 2009;5(9):422–433. [Google Scholar]
- Miyazaki T., Hotta Y., Kunii J., Kuriyama S., Tamaki Y. A review of dental CAD-CAM: current status and future perspectives from 20 years of experience. Dent. Mater. J. 2009;28(1):44–56. doi: 10.4012/dmj.28.44. [DOI] [PubMed] [Google Scholar]
- Oliveira-Junior O.B., Buso L., Fujiy F.H., Lombardo G.H., Campos F., Sarmento H.R., Souza R.O. Influence of polishing procedures on surface roughness of dental ceramics made by different techniques. Gen. Dent. 2013;61(1):e4–e8. [PubMed] [Google Scholar]
- Özarslan M.M., Büyükkaplan U.Ş., Barutcigil Ç., Arslan M., Türker N., Barutcigil K. Effects of different surface finishing procedures on the change in surface roughness and color of a polymer infiltrated ceramic network material. J. Adv. Prosthodont. 2016;8(1):16–20. doi: 10.4047/jap.2016.8.1.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pecho O.E., Ghinea R., Ionescu A.M., Cardona J.C., Della Bona A., del Mar Pérez M. Optical behavior of dental zirconia and dentin analyzed by Kubelka-Munk theory. Dent Mater. 2015;31(1):60–67. doi: 10.1016/j.dental.2014.11.012. [DOI] [PubMed] [Google Scholar]
- Pop-Ciutrila I.S., Dudea D., Eugenia Badea M., Moldovan M., Cîmpean S.I., Ghinea R. Shade correspondence, color, and translucency differences between human dentine and a CAD/CAM hybrid ceramic system. J. Esthet. Restor. Dent. 2016;28(Suppl 1):S46–S55. doi: 10.1111/jerd.12195. [DOI] [PubMed] [Google Scholar]
- Rosenblum M.A., Schulman A. A review of all ceramic restorations. J Am Dent Assoc. 1997;128(3):297–307. doi: 10.14219/jada.archive.1997.0193. [DOI] [PubMed] [Google Scholar]
- Saba D.A., Salama R.A., Haridy R. Effect of different beverages on the color stability and microhardness of CAD/CAM hybrid versus feldspathic ceramic blocks: an in-vitro study. Futur. Dent. J. 2017;3:61–66. [Google Scholar]
- Sarac D., Sarac Y.S., Yuzbasioglu E., Bal S. The effects of porcelain polishing systems on the color and surface texture of feldspathic porcelain. J. Prosthet. Dent. 2006;96(2):122–128. doi: 10.1016/j.prosdent.2006.05.009. [DOI] [PubMed] [Google Scholar]
- Sarikaya I., Guler A.U. Effects of different polishing techniques on the surface roughness of dental porcelains. J. Appl. Oral Sci. 2010;18(1):10–16. doi: 10.1590/S1678-77572010000100004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarikaya I., Yerliyurt K., Hayran Y. Effect of surface finishing on the color stability and translucency of dental ceramics. BMC Oral Health. 2018;18(1):40. doi: 10.1186/s12903-018-0508-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sasahara R.M.C., Ribeiro F.C., Cesar P.F., Yoshimura H.N. Influence of the finishing technique on surface roughness of dental porcelains with different microstructures. Oper. Dent. 2006;31(5):577–583. doi: 10.2341/05-104. [DOI] [PubMed] [Google Scholar]
- Schürmann M.G., Olms C. Shade stability of polymer-infiltrated and resin nano ceramics. Open Dent. J. 2018;12:791–800. doi: 10.2174/1745017901814010791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sfondrini M.F., Gandini P., Malfatto M., Di Corato F., Trovati F., Scribante A. Computerized casts for orthodontic purpose using powder-free intraoral scanners: accuracy, execution time, and patient feedback. Biomed. Res. Int. 2018;23:4103232. doi: 10.1155/2018/4103232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silness J. Fixed prosthodontics and periodontal health. Dent. Clin. North Am. 1980;24(2):317–329. [PubMed] [Google Scholar]
- Steiner R., Beier U.S., Heiss-Kisielewsky I., Engelmeier R., Dumfahrt H., Dhima M. Adjusting dental ceramics: An in vitro evaluation of the ability of various ceramic polishing kits to mimic glazed dental ceramic surface. J. Prosthet. Dent. 2015;113(6):616–622. doi: 10.1016/j.prosdent.2014.12.007. [DOI] [PubMed] [Google Scholar]
- Touchstone A., Nieting T., Ulmer N. Digital transmission: the collaboration between dentists and laboratory technicians on CAD/CAM restorations. J. Am. Dent. Assoc. 2010;141(Suppl 2):15S–19S. doi: 10.14219/jada.archive.2010.0353. [DOI] [PubMed] [Google Scholar]
- Um C.M., Ruyter I.E. Staining of resin-based veneering materials with coffee and tea. Quintessence Inter. 1991;22(5):377–386. [PubMed] [Google Scholar]
- van der Burgt T.P., ten Bosch J.J., Borsboom P.C.F., Kortsmit W.J.P.M. A comparison of new and conventional methods for quantification of tooth color. J. Prosthet. Dent. 1990;63(2):155–162. doi: 10.1016/0022-3913(90)90099-x. [DOI] [PubMed] [Google Scholar]
- Van Zeghbroeck L. CAD/CAM treatment for the elderly-a case report. Gerodontology. 2012;29(2):e1176–e1179. doi: 10.1111/j.1741-2358.2011.00521.x. [DOI] [PubMed] [Google Scholar]
- Wright M.D., Masri R., Driscoll C.F., Romberg E., Thompson G.A., Runyan D.A. Comparison of three systems for the polishing of an ultra-low fusing dental porcelain. J. Prosthet. Dent. 2004;92(5):486–490. doi: 10.1016/j.prosdent.2004.07.021. [DOI] [PubMed] [Google Scholar]
- Yılmaz C., Korkmaz T., Demirköprülü H., Ergün G., Ozkan Y. Color stability of glazed and polished dental porcelains. J. Prosthet. Dent. 2008;17(1):20–24. doi: 10.1111/j.1532-849X.2007.00237.x. [DOI] [PubMed] [Google Scholar]