Abstract
Background:
Controversy exists regarding the optimal bony fixation technique for lateral meniscal allografts.
Purpose/Hypothesis:
The objective was to quantify knee joint contact mechanics across the lateral plateau for keyhole and bone plug meniscal allograft transplant fixation techniques throughout simulated gait. It was hypothesized that both methods of fixation would improve contact mechanics relative to the meniscectomized condition, while keyhole fixation would restore the distribution of contact stress closer to that of the intact knee.
Study Design:
Controlled laboratory study.
Methods:
Six human cadaveric knees were mounted on a multidirectional dynamic simulator and subjected to the following conditions: (1) native intact meniscus, (2) keyhole fixation of the native meniscus, (3) bone plug fixation of the native meniscus, and (4) meniscectomy. Contact area, peak contact stress, and the distribution of stress across the tibial plateau were computed at 14% and 45% of the gait cycle, at which axial forces are at their highest. Translation of the weighted center of contact stress throughout simulated gait was computed.
Results:
Both bony fixation techniques improved contact mechanics relative to the meniscectomized condition. The keyhole technique was not significantly different from the intact condition for the following metrics: contact area, peak contact stress, distribution of force between the meniscal footprint and cartilage-to-cartilage contact, and the position of the weighted center of contact. In contrast, bone plug fixation resulted in a significant decrease of 21% to 28% in contact area at 14% and 45% of the simulated gait cycle, a significant increase in peak contact stresses of 34% at 45% of the gait cycle, and a shift in the weighted center of contact, which increased forces in the cartilage-to-cartilage contact area at 45% of the gait cycle.
Conclusion:
While both keyhole and bone plug fixation methods improved lateral compartment contact mechanics relative to the meniscectomized knee, keyhole fixation restored contact mechanics closer to that of the intact knee.
Clinical Relevance:
Method of meniscal fixation is under the direct control of the surgeon. From a biomechanics perspective, keyhole fixation is advocated for its ability to mimic intact knee joint contact mechanics.
Keywords: knee, meniscus, allograft, contact mechanics, simulated gait
The medial and lateral menisci of the knee joint serve a range of functions that include force distribution, lubrication, and proprioception.4,22,34 Meniscal deficiency and injury can lead to the rapid development of osteoarthritis.8,21,25,30 In the instance of absolute meniscal deficiency, defined by the absence of an intact meniscal rim, meniscal allograft transplantation is considered a salvage procedure to improve joint function and redistribute joint loads across the tibial plateau.11–14,26–29,35,36 While many variables, such as graft size, concomitant injury, knee stability, joint alignment, and rehabilitation protocols, can affect the outcomes after graft transplantation, fixation technique is a key factor directly controllable by the surgeon.1,3,7,11,19,24,38
Two primary bony fixation techniques are used during lateral meniscal allograft transplantation: (1) keyhole fixation, in which the posterior and anterior horns of the graft remain connected via a bone bridge placed into a corresponding slot created in the tibia; (2) bone plug fixation, in which 2 separate bone segments attached to the anterior and posterior meniscal horns are harvested with the graft and fixed into their respective bone tunnels located at the tibial attachment sites of the native meniscus.7,18,19,29,31,32,38 Keyhole fixation is currently recommended for lateral meniscal allograft transplantation because of concerns related to the intersection of the anterior and posterior bone tunnels in the bone plug fixation technique. However, the bone plug fixation method offers the advantage that the surgeon has more control over the relative positions of the individual anterior and posterior attachment sites.
Previous biomechanical studies on the effect of lateral allograft transplantation on knee joint mechanics have shown that the keyhole and bone plug fixation techniques partially restore contact mechanics to those of the intact knee after lateral meniscal allograft transplantation.9,26,28 But these studies were performed with static and quasi-static loading conditions, which cannot capture the multidirectional forces applied across the knee joint during activities of daily living. It has been further suggested that meniscal allograft keyhole fixation, which maintains relative root positions, may allow the graft to better resist hoop stresses and result in less extrusion of the body of the meniscus16,17; however, these concepts have not been explored biomechanically. Our team previously developed a dynamic model capable of simulating activities of daily living5,13 and demonstrated that transosseous fixation of medial meniscal allografts provides superior load distribution as compared with suture-only fixation, particularly during the early stance phase of gait.35 However, such analyses have not been applied to the lateral compartment.
Our objective was to quantify knee joint contact mechanics across the lateral plateau for keyhole and bone plug meniscal allograft transplant fixation techniques throughout simulated gait. We hypothesized that both methods of fixation would improve contact mechanics relative to the meniscectomized condition, while keyhole fixation would restore the distribution of contact stress closer to that of the intact knee.
METHODS
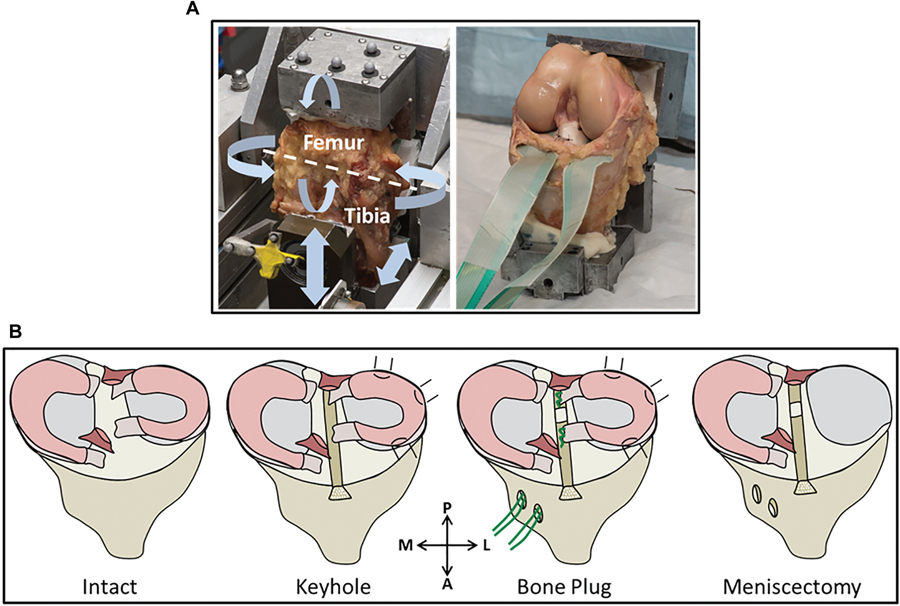
Under institutional review board approval, 6 human cadaveric knees (Anatomy Gifts Registry and Science Care) (Appendix Table A1, available in the online version of this article) were stripped of all soft tissue down to the joint capsule; care was taken to avoid interfering with the cruciate and collateral ligaments. Knee quality was assessed by a practicing sports medicine surgeon (M.M.) for the presence of osteoarthritis or meniscal damage. As previously described,5,6,36,37 a 2 mm–diameter Kirschner wire (K-wire) was drilled through the epicondylar axis of each knee to define the anatomic flexion axis. Positioning of the K-wire was visually assessed by a surgical fellow using fluoroscopic imaging in the coronal and sagittal planes. If the K-wire axis alignment was not accurate, it was manually repositioned and reimaged. Subsequently, the patella was removed, and knees were potted in custom-made fixtures with poly-methyl methacrylate. The K-wire was used to align the epicondylar axis of the knees to the flexion axis of a modified 4 degrees of freedom Stanmore knee simulator10 (Figure 1). Four conditions were tested (Figure 1B): (1) native intact meniscus, (2) keyhole fixation of the native meniscus, (3) bone plug fixation of the native meniscus, and (4) meniscectomy. Pilot testing demonstrated that it was not possible to create a stable keyhole graft after formation of the bone plugs, and as such, the order of testing was not randomized. Rather, the testing sequence was as follows: intact, keyhole, bone plug, meniscectomy.
Figure 1.
(A) Cadaveric specimen on the Stanmore knee simulator. The controlled forces and torques are displayed by the arrows, with the white dotted line representing the epicondylar axis of the knee. The waterproofed Tekscan sensor is placed underneath the menisci and across the tibial plateau and then sutured to the anterior cruciate ligament and posterior capsule. (B) Schematic diagram: the intact tibial plateau; keyhole fixation depicting the bone bridge placed in the corresponding slot and the suture attaching the lateral meniscus to the capsule; bone plug fixation depicting the 2 bone segments sutured through the bone tunnels and the suture attaching the lateral meniscus to the capsule; and the meniscectomized condition. A, anterior; L, lateral; M, medial; P, posterior.
To replicate the keyhole method, an oscillating surgical saw (Stryker Orthopaedics) was used to remove a bone block from the lateral tibial plateau, creating a slot in the tibia. This bone block maintained its connection to the anterior and posterior horns of the lateral meniscus. The meniscus was then resected from the capsule and removed from the joint. Next the ‘‘graft’’ was reinserted, and a shim (fashioned from cadaveric bone) was placed laterally to create an interference fit for the graft in the slot, replicating the secure fixation of the keyhole technique. The outer rim of the lateral meniscus was then resutured to the joint capsule. For the bone plug method, the central portion of the bone block was separated to create 2 bone plugs, which were attached to the anterior and posterior meniscal horns. The bone plugs were then repositioned into the slot in the tibia, and each plug was secured with sutures through the anterior or posterior horn bone segments and into tunnels drilled through the subchondral bone. The sutures were tied together across a bone bridge. The remaining central portion of the bone block was then placed into the remaining space between the bone plugs and secured with the cadaveric bone shim. Again, the outer rim of the lateral meniscus was resutured to the joint capsule. For the meniscectomy condition, the lateral meniscus was removed from the joint after detachment of the meniscal horns from the bone plugs and resection of the meniscus from its attachment at the joint capsule.
The knees were subjected to physiological loads to simulate gait at 0.5 Hz for 20 cycles (see online Video Supplement). Flexion-extension, anterior-posterior force, axial force, and internal-external torque were controlled, while medial-lateral force and varus-valgus torque were left floating.5,6,13,15,36,37 Contact stress across the tibial plateau was recorded with a thin electrical resistive sensor (model 4011; Tekscan Inc) that was equilibrated and calibrated with a standard protocol as previously described.13,36 The sensor was augmented with tabs for fixation and coated with waterproof film (Tegaderm; 3M Inc) to preserve sensor performance. The sensor was placed underneath the menisci and across the tibial plateau, and the fixation tabs were sutured to the posterior capsule and distal ACL to hold the sensor in place throughout testing. Care was taken to avoid damaging the meniscal root during the Tekscan insertion procedure. Data were collected at a rate of 100 Hz.
Outputs and Data Analysis
Contact area and peak contact stress on the lateral plateau were calculated at 14% and 45% of the gait cycle: the 2 points in the simulated gait cycle of maximum axial load.5,6,13,15,36,37 A custom-written Matlab code (Math-Works Inc) was used to identify regions of interest (ROIs) where the femoral cartilage contacted the tibial cartilage (cartilage-cartilage [C-C]) and where the tibial cartilage was in contact with the meniscus (cartilage-meniscus [C-M]) as seen by the outline of the meniscal footprint on the sensor. Throughout the gait cycle, the ROIs that were drawn for the intact condition were applied to keyhole, bone plug, and meniscectomy conditions by 2 independent observers (C.B., O.A.). The contact area and peak contact stress in the C-C and C-M contact regions were calculated for each surgical condition. Interobserver reliability was evaluated by calculating Cronbach alpha for each outcome measure at 14% and 45% of the gait cycle for the lateral plateau and the C-C and C-M ROIs. Reliability was acceptable (α > .80) for all outcome measures except peak contact stress in the C-M ROI at 14% of the gait cycle (α = .55); this could likely be attributed to the dependency of peak contact stress on single sensel variations—particularly if the peak sensel was located on the C-M border. As previously reported,13 the weighted center of contact stress (WCoCS) was calculated throughout the gait cycle by weighting sensels based on the magnitude of their contact stress. The following equation was used to calculate WCoCS: Σ(si x pi)/Σsi, where si represents the contact stress at sensel – i and pi represents the location of sensel – i in the sensor coordinate system.13,35 Principal component analysis was performed in Matlab to determine differences in the WCoCS among conditions throughout gait. All outcome measures were calculated by the same 2 authors using a customized Matlab code.13,35 A paired 1-way repeated measures analysis of variance with Dunnett post hoc test was used for statistical analysis to compare all interventions with the intact condition, with P < .05 representing significance. The study was powered on the basis of a similar study of meniscal fixation on the medial plateau.35 To determine if we had sufficient power to detect a change in peak contact stress at 45% of the gait cycle, a post hoc power analysis was performed with the difference in average peak contact stress between bone plug and intact conditions (2.2 MPa) and the SD of the bone plug condition (0.8 MPa), with an α of .05 and a sample size of 6 following a 1-way analysis of variance study design. The analysis revealed that the power of our study was 96%.
RESULTS
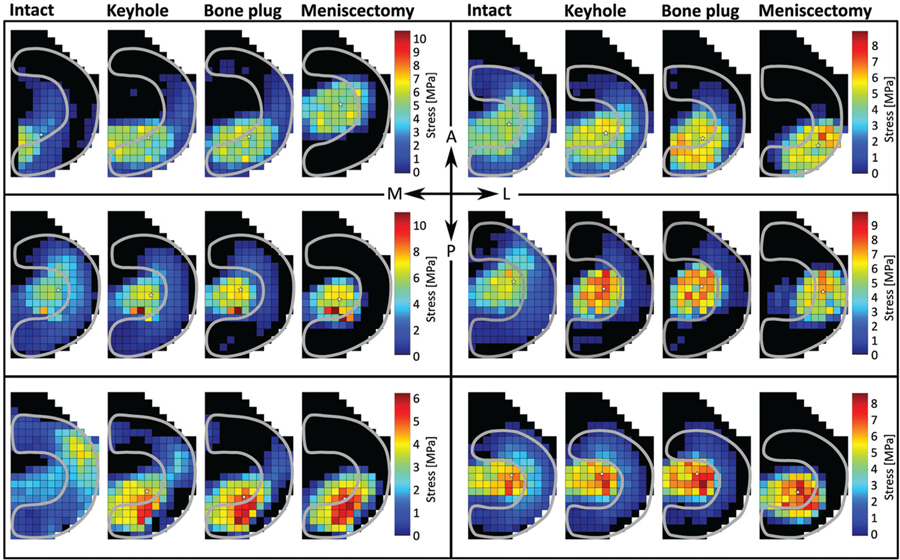
Contact mechanics data were successfully recorded for all 6 cadaveric knees for all conditions. Contact stresses and contact areas were highly variable across knees and conditions (Figure 2).
Figure 2.
Contact stress maps for each knee and each test condition at 45% of the gait cycle. Despite variability among knee contact patterns, a significant decrease in contact area and increase in peak contact stress in the cartilage-meniscal region of interest are shown for the meniscectomized condition. The decrease in contact area and increase in peak contact stress are also shown for the cartilage-cartilage region of interest for the meniscectomized condition as is the increase in peak contact stress for the bone plug condition. A, anterior; L, lateral; M, medial; P, posterior.
Total Contact Area and Contact Stress
At 14% and 45% of the gait cycle, meniscectomy significantly reduced the contact area on the lateral plateau by 51% and 55%, respectively, when compared with the intact condition (Figure 3A). At 14% and 45% of the gait cycle, meniscectomy significantly increased peak contact stress by 39% and 46%, respectively, when compared with the intact condition (Figure 3B). Bone plug fixation resulted in 21% and 28% reduction in the contact area relative to the intact condition at 14% and 45% of the gait cycle, respectively, and a significant increase (34%) in peak contact stress at 45% of the gait cycle. No significant difference was found between keyhole fixation and the intact condition for contact area or peak contact stress at either 14% or 45% of gait.
Figure 3.
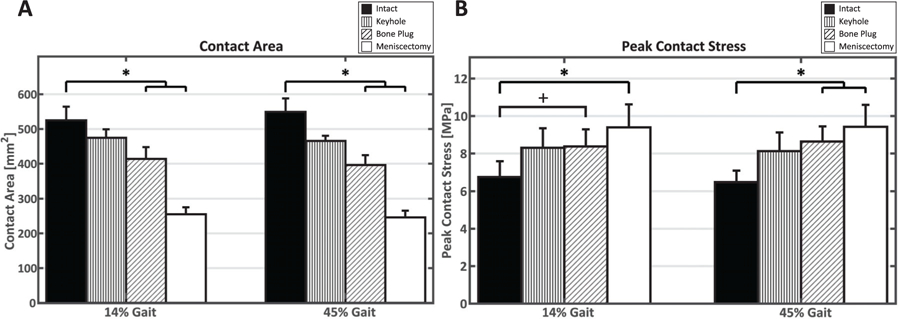
(A) Decrease in contact area and (B) increase in peak contact stress at 14% and 45% gait. Data are presented as mean ± SE. *P < .05 vs intact condition. +P = .051 vs intact condition.
ROI Contact Area and Contact Stress
Meniscectomy led to a significant reduction in contact area at 14% and 45% of the gait cycle in the C-C and C-M ROIs and a significant increase in peak contact stress in the C-C ROI at 45% of the gait cycle and the C-M ROI at 14% and 45% of the gait cycle (Table 1). Bone plug fixation significantly decreased the contact area in the C-M ROI and led to a small but significant increase in peak contact stress in the C-C ROI at 45% of the gait cycle when compared with the intact condition, suggesting a subtle shift in force distribution to the area of C-C contact (Table 2). No significant difference between meniscal allograft transplantation with keyhole fixation and the intact condition was found in peak contact stresses and contact areas in the C-C and C-M zones.
TABLE 1.
Contact Area for the C-C and C-M ROIs at 14% and 45% of Gaita
| Contact Area: C-C ROI, mm2 |
Contact Area: C-M ROI, mm2 |
|||
|---|---|---|---|---|
| 14% | 45% | 14% | 45% | |
| Intact | 175.4 ± 15.1 | 177.2 ± 14.9 | 349.6 ± 29.6 | 371.4 ± 27.2 |
| Keyhole | 168.1 ± 10.4 | 169.4 ± 11.1 | 306.7 ± 24.7 | 296.4 ± 19.4 |
| Bone plug | 156.1 ± 7.3 | 157.3 ± 8.1 | 257.7 ± 39.8b | 238.9 ± 34.4c |
| Meniscectomy | 119.8 ± 20.3c | 117.3 ± 19.3c | 135.5 ± 23.0c | 128.8 ± 20.5c |
Data are presented as mean ± SE. C-C, cartilage-cartilage; C-M, cartilage-meniscus; ROI, region of interest.
P = .054 vs intact condition.
P < .05 vs intact condition.
TABLE 2.
Peak Contact Stress for the C-C and C-M ROIs at 14% and 45% Gaita
| Stress: C-C ROI, MPa |
Stress: C-M ROI, MPa |
|||
|---|---|---|---|---|
| 14% | 45% | 14% | 45% | |
| Intact | 6.74 ± 0.84 | 6.14 ± 0.89 | 4.55 ± 0.70 | 4.23 ± 0.35 |
| Keyhole | 8.21 ± 1.08 | 8.10 ± 1.01 | 5.46 ± 0.84 | 4.37 ± 0.73 |
| Bone plug | 8.31 ± 0.94 | 8.60 ± 0.83b | 5.11 ± 0.87 | 4.94 ± 1.00 |
| Meniscectomy | 8.04 ± 1.43 | 8.32 ± 1.30b | 8.23 ± 0.85b | 8.73 ± 0.86b |
Data are presented as mean ± SE. C-C, cartilage-cartilage; C-M, cartilage-meniscus; ROI, region of interest.
P < .05 vs intact condition.
Weighted Center of Contact Stress
Principal component analysis of the WCoCS demonstrated that meniscectomy resulted in a significant lateral shift from the intact condition throughout the gait cycle (Figure 4). Bone plug fixation resulted in a significant medial shift in WCoCS relative to the intact condition. We did not detect any significant differences in WCoCS between the intact condition and keyhole fixation. A small posterior shift (P = .05) of the WCoCS occurred with meniscectomy relative to the intact condition. No other significant difference in anterior-posterior WCoCS occurred.
Figure 4.
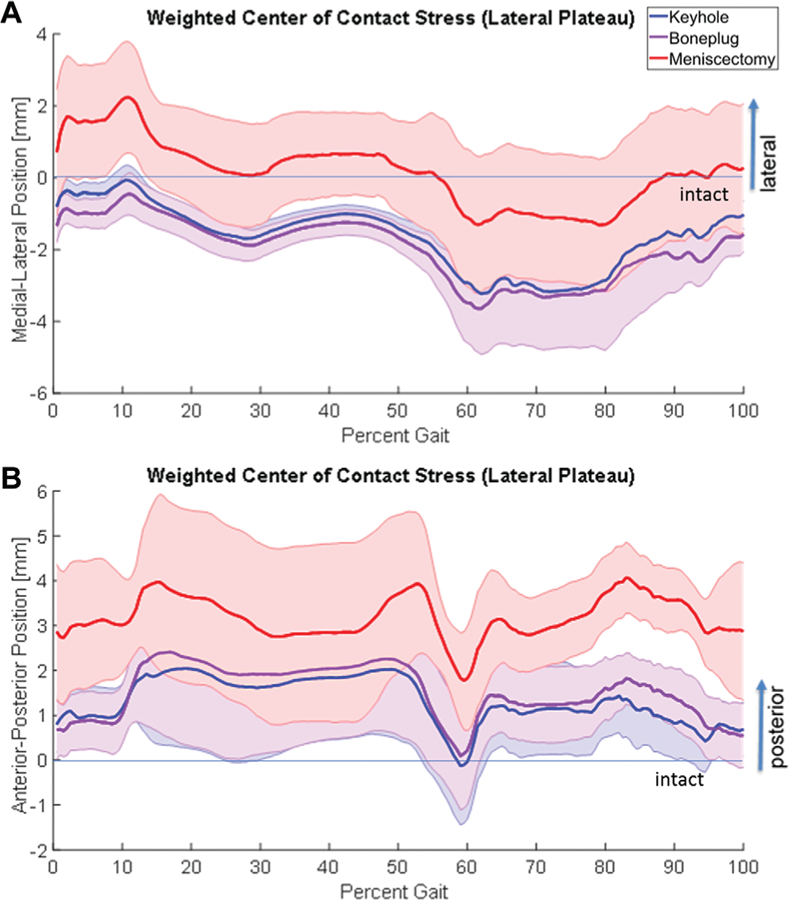
(A) Plot of medial-lateral shift in WCoCS on the lateral plateau for each condition, normalized to the intact condition throughout the gait cycle, shows a significant lateral shift after meniscectomy and a significant medial shift with bone plug fixation. (B) Plot of anterior-posterior shift in WCoCS on the lateral plateau for each condition, normalized to the intact condition throughout the gait cycle, shows a posterior shift of the WCoCS after meniscectomy (P = .05). Mean is presented as a solid line with the shaded bars representing the SE. WCoCS, weighted center of contact stress.
DISCUSSION
By way of a cadaveric model designed to simulate gait, knee joint contact mechanics across the lateral plateau were quantified for the intact, meniscectomized, allograft keyhole fixation, and allograft bone plug fixation conditions. Using the output metrics of contact area, peak contact stress, distribution of stress across the tibial plateau, and translation of the WCoCS, we accepted the hypothesis that keyhole fixation restored the distribution of contact stress closer to that of the intact knee.
Our finding that total meniscectomy of the lateral meniscus significantly increased peak contact stress and decreased contact area during the gait cycle was not surprising.11,26,28 The magnitude of change in the contact area with meniscectomy (51%−55%) is within that reported by Paletta et al28 (51%−55%) and Chen et al9 (~48%). However, the increase in peak contact stresses after meniscectomy (39%−46%) is lower than that reported by Chen et al (61%) and McDermott et al26 (31%−150%) and substantially lower than that reported by Paletta et al (235%−335%). These differences are most likely caused by differences in the test setup, differences in the magnitude of applied input forces, and differences in the force and moment profiles to which the soft tissues are subjected during testing. Furthermore, the dynamic nature of the test used in this study would differentially influence the viscoelastic responses of the meniscus and articular cartilage and the ligaments, which in turn would influence the magnitude and distribution of joint contact.2,33
The exact relationship between specific levels of contact area and contact stresses and the biological responses of articular cartilage has yet to be elucidated.23 To help interpret the data generated, contact mechanics of both graft fixation methods were compared with those of the meniscectomized condition, which predisposes the knee joint to osteoarthritis, and the ‘‘normal’’ intact condition. For the meniscal allograft conditions, both fixation techniques improved contact mechanics relative to the meniscectomized condition, but differences between fixation techniques were identified. The keyhole fixation technique was not significantly different from intact for the following metrics: contact area, peak contact stress, distribution of force between the meniscal footprint and C-C footprint, and the position of the weighted center of contact. In contrast, bone plug fixation resulted in a significant decrease of 21% to 28% in contact area at both 14% and 45% of the simulated gait cycle, a significant increase in peak contact stresses of 34% at 45% of the gait cycle, and a shift in the weighted center of contact, with forces increased in the C-C contact area at 45% of the gait cycle. The change in the distribution of force between the cartilage that is covered by the meniscus and that in the area of C-C contact may lead to a change in cartilage strain in those zones and subsequent cartilage degeneration.20 Of note, the most pronounced changes in contact mechanics in the lateral compartment occurred in the second half of the gait cycle. This finding contrasts to a similar study,37 in which medial meniscal contact mechanics were most strongly influenced by fixation in the first half of the gait cycle, and emphasizes the differences in the biomechanical behavior of each compartment.
There are several limitations to this study. A key limitation is that the order of testing was not randomized, because a pilot study exhibited that it was impossible to do so, given the need to create stable fixation for both the keyhole and bone plug fixation conditions on the same sample. The test apparatus used herein maintains knee hydration and has previously been used to test up to 5 conditions on a single specimen,5,6 with no demonstrable deterioration in the knee. Nonetheless, it is possible that our sequence of testing may have led to bias toward the first method of fixation. An additional limitation is that the ‘‘native’’ meniscus was used as a graft, which would optimize graft matching. However, the effects of fixation can be studied without consideration of the effect of variability in graft geometry, which is an inherent challenge with graft use. Additionally, the data represent the immediate postoperative conditions, without due consideration of healing/fixation ingrowth. Finally, the effect of meniscal fixation on joint kinematics was outside the scope of the study.
In summary, using a human cadaveric model in which the activity of gait was simulated, we accepted the hypothesis that both keyhole and bone plug fixation methods improved contact mechanics relative to the meniscectomized knee at time zero. We also concluded that keyhole fixation restored contact mechanics closer to those of the intact knee. The changes in contact mechanics that were quantified could have long-term consequences for the response of the joint tissue.
Supplementary Material
ACKNOWLEDGMENT
The authors acknowledge Amanda Wach, MS, for her help creating the figures.
One or more of the authors has declared the following potential conflict of interest or source of funding: Research reported in this publication was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health under awards R01 AR066635 and R01 AR066635-03S1. This research was also supported by the Russell Warren Chair in Tissue Engineering. R.W., S.M., and T.C. are equity holders in AGelity Biomechanics. M.M. has received compensation for services other than consulting, education, and hospitality payments from Arthrex. R.W. has received royalties from Arthrex and Zimmer Biomet and hospitality payments from Arthrex. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Footnotes
A Video Supplement for this article is available online.
REFERENCES
- 1.Abat F, Gelber PE, Erquicia JI, Pelfort X, Gonzalez-Lucena G, Monllau JC. Suture-only fixation technique leads to a higher degree of extrusion than bony fixation in meniscal allograft transplantation. Am J Sports Med 2012;40:1591–1596. [DOI] [PubMed] [Google Scholar]
- 2.Abusara Z, Von Kossel M, Herzog W. In vivo dynamic deformation of articular cartilage in intact joints loaded by controlled muscular contractions. PLoS One 2016;11(1):e0147547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alhalki MM, Howell SM, Hull ML. How three methods for fixing a medial meniscal autograft affect tibial contact mechanics. Am J Sports Med 1999;27(3):320–328. [DOI] [PubMed] [Google Scholar]
- 4.Allen A, Caldwell GL, Fu F. Anatomy and biomechanics of the meniscus. Oper Tech Orthop 1995;5(1):2–9. [Google Scholar]
- 5.Bedi A, Kelly N, Baad M, et al. Dynamic contact mechanics of the medial meniscus as a function of radial tear, repair, and partial meniscectomy. J Bone Joint Surg Am 2010;92(6):1398–1408. [DOI] [PubMed] [Google Scholar]
- 6.Bedi A, Kelly N, Baad M, et al. Dynamic contact mechanics of radial tears of the lateral meniscus: implications for treatment. Arthroscopy 2012;28(3):372–381. [DOI] [PubMed] [Google Scholar]
- 7.Brophy RH, Matava MJ. Surgical options for meniscal replacement. J Am Acad Orthop Surg 2012;20(5):265–272. [DOI] [PubMed] [Google Scholar]
- 8.Carbone A, Rodeo S. Review of current understanding of post-traumatic osteoarthritis resulting from sports injuries. J Orthop Res 2017;35(3):397–405. [DOI] [PubMed] [Google Scholar]
- 9.Chen MI, Branch TP, Hutton WC. Is it important to secure the horns during lateral meniscal transplantation? A cadaveric study. Arthroscopy 1996;12(2):174–181. [DOI] [PubMed] [Google Scholar]
- 10.DesJardins JD, Walker PS, Haider H, Perry J. The use of a force-controlled dynamic knee simulator to quantify the mechanical performance of total knee replacement designs during functional activity. J Biomech 2000;33(10):1231–1242. [DOI] [PubMed] [Google Scholar]
- 11.Dienst M, Greis PE, Ellis BJ, Bachus KN, Burks RT. Effect of lateral meniscal allograft sizing on contact mechanics of the lateral tibial plateau: an experimental study in human cadaveric knee joints. Am J Sports Med 2007;35(1):34–42. [DOI] [PubMed] [Google Scholar]
- 12.Elattar M, Dhollander A, Verdonk R, Almqvist KF, Verdonk P. Twenty-six years of meniscal allograft transplantation: is it still experimental? A meta-analysis of 44 trials. Knee Surg Sports Traumatol Arthrosc 2011;19(2):147–157. [DOI] [PubMed] [Google Scholar]
- 13.Gilbert S, Chen T, Hutchinson ID, et al. Dynamic contact mechanics on the tibial plateau of the human knee during activities of daily living. J Biomech 2014;47(9):2006–2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Greis PE, Bardana DD, Holmstrom MC, Burks RT. Meniscal injury: I. Basic science and evaluation. J Am Acad Orthop Surg 2002; 10(3):168–176. [DOI] [PubMed] [Google Scholar]
- 15.International Standards Organization. Implants for Surgery: Wear of Total Knee-Joint Prostheses. Part 1: Loading and Displacement Parameters for Wear-Testing Machines With Load Control and Corresponding Environmental Conditions for Test Geneva, Switzerland: International Standards Organization; 2009. ISO 142343-1:2009. [Google Scholar]
- 16.Kim JH, Bin SI, Lee BS, et al. Nonanatomic horn position increases risk of early graft failures after lateral meniscal allograft transplantation. Am J Sports Med 2018;46(14):3407–3414. [DOI] [PubMed] [Google Scholar]
- 17.Kim NK, Bin SI, Kim JM, Lee CR. Does lateral meniscal allograft transplantation using the keyhole technique restore the anatomic location of the native lateral meniscus? Am J Sports Med 2016;44(7):1744–1752. [DOI] [PubMed] [Google Scholar]
- 18.Lee AS, Kang RW, Kroin E, Verma NV, Cole BJ. Allograft meniscus transplantation. Sports Med Arthrosc Rev 2012;20:106–114. [DOI] [PubMed] [Google Scholar]
- 19.Lee YH, Caborn DN. A new technique for arthroscopic meniscus transplant using soft tissue fixation and anatomical meniscal root reinsertion. Knee Surg Sports Traumatol Arthrosc 2012;20(5):904–908. [DOI] [PubMed] [Google Scholar]
- 20.Liu B, Lad NK, Collins AT, et al. In vivo tibial cartilage strains in regions of cartilage-to-cartilage contact and cartilage-to-meniscus contact in response to walking. Am J Sports Med 2017;45(12):2817–2823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lohmander LS, Englund PM, Dahl LL, Roos EM. The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med 2007;35(10):1756–1769. [DOI] [PubMed] [Google Scholar]
- 22.MacConaill MA. The function of intra-articular fibrocartilages with special reference to the knee and inferior radio-ulnar joints. J Anat 1932;6:210–227. [PMC free article] [PubMed] [Google Scholar]
- 23.Maher SA, Wang H, Koff MF, Belkin N, Potter HG, Rodeo SA. Clinical platform for understanding the relationship between joint contact mechanics and articular cartilage changes after meniscal surgery. J Orthop Res 2017;35(3):600–611. [DOI] [PubMed] [Google Scholar]
- 24.Matava MJ. Meniscal allograft transplantation: a systematic review. Clin Orthop Relat Res 2007;455:142–157. [DOI] [PubMed] [Google Scholar]
- 25.McCann L, Ingham E, Jin Z, Fisher J. Influence of the meniscus on friction and degradation of cartilage in the natural knee joint. Osteoarthritis Cartilage 2009;17(8):995–1000. [DOI] [PubMed] [Google Scholar]
- 26.McDermott ID, Lie DT, Edwards A, Bull AM, Amis AA. The effects of lateral meniscal allograft transplantation techniques on tibio-femoral contact pressures. Knee Surg Sports Traumatol Arthrosc 2008; 16(6):553–560. [DOI] [PubMed] [Google Scholar]
- 27.McGuire DA, Carter TR, Shelton WR. Complex knee reconstruction: osteotomies, ligament reconstruction, transplants, and cartilage treatment options. Arthroscopy 2002;18(9)(suppl 2):90–103. [DOI] [PubMed] [Google Scholar]
- 28.Paletta GA Jr, Manning T, Snell E, Parker R, Bergfeld J. The effect of allograft meniscal replacement on intraarticular contact area and pressures in the human knee: a biomechanical study. Am J Sports Med 1997;25(5):692–698. [DOI] [PubMed] [Google Scholar]
- 29.Peters G, Wirth CJ. The current state of meniscal allograft transplantation and replacement. Knee 2003;10(1):19–31. [DOI] [PubMed] [Google Scholar]
- 30.Rangger C, Klestil T, Gloetzer W, Kemmler G, Benedetto KP. Osteoarthritis after arthroscopic partial meniscectomy. Am J Sports Med 1995;23(2):240–244. [DOI] [PubMed] [Google Scholar]
- 31.Rodeo SA. Meniscal allografts—where do we stand? Am J Sports Med 2001;29(2):246–261. [DOI] [PubMed] [Google Scholar]
- 32.Shelton WR, Dukes AD. Meniscus replacement with bone anchors: a surgical technique. Arthroscopy 1994;10(3):324–327. [DOI] [PubMed] [Google Scholar]
- 33.Varady NH, Grodzinsky AJ. Osteoarthritis year in review 2015: mechanics. Osteoarthritis Cartilage 2016;24(1):27–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Walker PS, Erkman MJ. The role of the menisci in force transmission across the knee. Clin Orthop Relat Res 1975;109:184–192. [DOI] [PubMed] [Google Scholar]
- 35.Wang H, Chen T, Gee AO, et al. Altered regional loading patterns on articular cartilage following meniscectomy are not fully restored by autograft meniscal transplantation. Osteoarthritis Cartilage 2015; 23(3):462–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang H, Chen T, Koff MF, et al. Image based weighted center of proximity versus directly measured knee contact location during simulated gait. J Biomech 2014;47(10):2483–2489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang H, Gee AO, Hutchinson ID, et al. Bone plug versus suture-only fixation of meniscal grafts: effect on joint contact mechanics during simulated gait. Am J Sports Med 2014;42(7):1682–1689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Woodmass JM, Johnson NR, Levy BA, Stuart MJ, Krych AJ. Lateral meniscus allograft transplantation: the bone plug technique. Arthrosc Tech 2017; 6(4):e1215–e1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.