Abstract
We present a case of adult-onset Kawasaki disease shock syndrome complicated by coronary aneurysms, in which profound hypotension and reduced left ventricular ejection fraction were treated successfully with intravenous immunoglobulin. The diagnosis of Kawasaki disease shock syndrome should be considered in cases of rapidly developing shock, particularly in young adults with an infectious prodrome, in whom it may be under-recognized. We advocate for early identification to minimize delays in treatment with intravenous immunoglobulin, which reverses left ventricular dysfunction and decreases risk of long-term sequelae such as coronary artery aneurysms.
Résumé
Nous présentons un cas de syndrome de choc dans la maladie de Kawasaki survenu à l'âge adulte et compliqué par des anévrismes des artères coronaires, chez lequel l'injection d'immunoglobulines par voie intraveineuse a permis de traiter avec succès une hypotension prononcée et une fraction d'éjection ventriculaire gauche réduite. Le diagnostic de syndrome de choc dans la maladie de Kawasaki devrait être envisagé dans les cas de choc évoluant rapidement, en particulier chez les jeunes adultes en phase prodromique d'une infection, chez lesquels cette affection peut passer inaperçue. Nous préconisons un diagnostic précoce afin de réduire au minimum les délais du traitement aux immunoglobulines par voie intraveineuse qui a pour effet d'inverser la dysfonction ventriculaire gauche et de diminuer le risque de séquelles à long terme, comme l'anévrisme des coronaires.
Novel Teaching Points.
-
1.
KDSS should be on the differential for cases of rapidly developing shock, particularly in young adults with an infectious prodrome.
-
2.
Cases of KDSS may go unrecognized and this can result in delayed treatment.
-
3.
The early use of IVIG is effective in reducing LV dysfunction and decreases the risk of coronary artery aneurysms.
Kawasaki disease (KD) is a generalized vasculitis affecting medium- and small-sized vessels, usually occurring in children aged less than 5 years.1 Kawasaki disease shock syndrome (KDSS), described by Kanegaye et al.,2 includes traditional features of KD (Table 1) and shock symptoms, defined as “systolic hypotension, a sustained decrease in systolic blood pressure from baseline of ≥ 20%, or clinical signs of poor perfusion.”2 Some 7% of KD cases in the pediatric population meet this criteria.2 KDSS is associated with cardiac sequelae, including reduced left ventricular ejection fraction (LVEF), mitral regurgitation, and coronary artery abnormalities.2 Although KD is rare in adults, cases with shock are even less frequently reported. We present a case of adult-onset KDSS with heart failure, complicated by coronary aneurysms.
Table 1.
| Criteria | Description |
|---|---|
| Kawasaki disease | |
| Fever | Duration of 5+ d, AND 4 of the following: |
| 1. Conjunctivitis | Bilateral bulbar conjunctival injection without exudate |
| 2. Mucocutaneous features | Erythema of oral and pharyngeal mucosa, erythema and cracking of lips, strawberry tongue |
| 3 .Rash | Maculopapular, diffuse, or can be erythema multiforme-like |
| 4. Lymphadenopathy | Cervical, usually unilateral, > 1.5 cm diameter |
| 5. Hands and feet | Acute phase: erythema, edema, or subacute phase: periungual desquamation |
| If coronary artery aneurysms are detected, the diagnosis of KD is considered confirmed in most cases, even if above criteria are not fully met. | |
| Kawasaki disease shock syndrome | |
| Shock syndrome | Must additionally include one of: |
| Hypotension and shock∗ | Requiring initiation of volume expanders OR |
| Infusion of vasoactive agents OR | |
| Transfer to intensive care units | |
KD, Kawasaki disease.
Defined as “systolic hypotension, a sustained decrease in systolic blood pressure from baseline of ≥ 20% or clinical signs of poor perfusion.”2
Case Report
A previously healthy 20-year-old man of East Asian descent presented with 5 days of 40°C fevers, migratory arthralgias, and an erythematous nonblanching rash of the trunk and limbs. Clinical assessment also revealed bilateral conjunctivitis, mild pharyngitis, headache, neck stiffness, and sporadic diarrhea. No exposures, travel, or ill contacts were identified. Laboratory results revealed leukocytosis of 16.3, C-reactive protein (CRP) of 315, mild transaminitis, and bland cerebrospinal fluid. Initial chest x-ray was unremarkable.
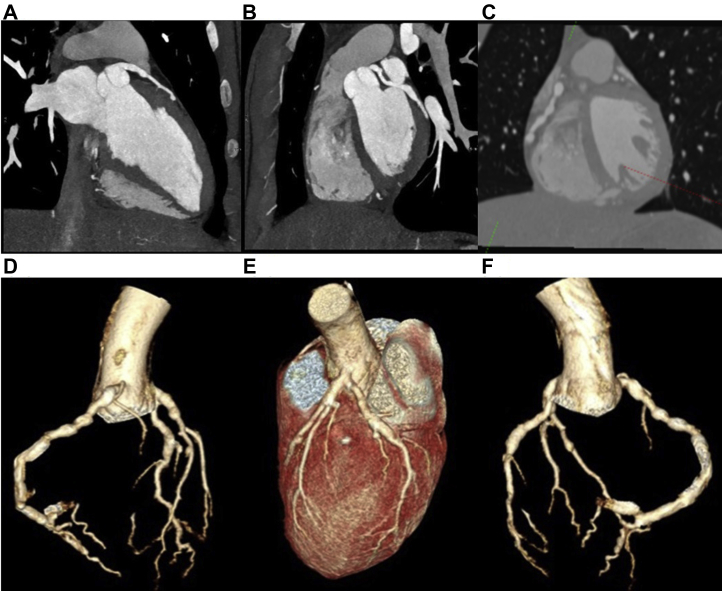
The patient remained febrile and tachycardic for several days. On day 5 postadmission, he developed acute heart failure, with hypotension and pulmonary edema requiring transfer to the coronary intensive care unit. Brain natriuretic peptide was 1767 and LVEF measured 35% via transthoracic echocardiogram (TTE). The study revealed moderately reduced global systolic function and a mildly dilated left ventricle (LV). Moderate functional mitral regurgitation and a small circumferential pericardial effusion were present. Cardiac magnetic resonance imaging displayed global hypokinesis with no evidence of late gadolinium enhancement, no myocarditis, and no infiltrative cardiomyopathy. Cardiac computed tomography angiography (CCTA) revealed diffuse coronary artery ectasia. All 3 coronaries showed multiple aneurysms up to 200% of baseline diameter, with a maximum diameter of 7.2 mm (Fig. 1).
Figure 1.
Cardiac-gated contrast-enhanced computed tomography demonstrating coronary aneurysms involving the (A) left anterior descending artery, (B) left circumflex artery, and (C) right coronary artery. (D-F) Three-dimensional reconstructions of coronary arteries.
The patient was diagnosed with adult-onset, incomplete KD. Initial treatment consisted of high-dose acetylsalicylic acid (ASA) and an infusion of intravenous immunoglobulin (IVIG). He defervesced and was discharged after 13 days with no signs of heart failure. He also received low-dose carvedilol 6.25 mg twice daily and ramipril 1.25 mg once daily for the reduced LVEF (doses were limited because of low blood pressure).
In follow-up 2 weeks after discharge, the patient was improved symptomatically, although he still had conjunctival irritation. CRP had decreased to 116 by discharge and completely normalized to 0.8 after 2 months. Brain natriuretic peptide 1 month later measured < 10. Repeat CCTA demonstrated stable coronary aneurysms. Two weeks later, repeat TTE revealed LVEF improvement to 55%. High-dose ASA was then decreased to a daily dose of 81 mg, and clopidogrel 75 mg daily was added as per the American Heart Association’s 2017 Scientific Statement on the Diagnosis, Treatment, and Long-Term Management of Kawasaki Disease.1 The goal of dual antiplatelet therapy in this context is to decrease the risk of coronary artery thrombosis, which is much higher in an individual with aneurysmal coronary anatomy.
Four months after discharge, the patient’s LVEF had further increased to 65% on TTE. At this time carvedilol was discontinued, and he remained on 1.25 mg of ramipril daily.
In further follow-up, CCTA at 1 year showed stable coronary aneurysms without improvement. Because of the persistent coronary aneurysms, he was maintained on clopidogrel and low-dose ASA. Because his LVEF remained normal and the patient was asymptomatic, his ramipril was discontinued, with planned ongoing follow-up of his ventricular function.
Discussion
There are few reported cases of heart failure complicating nonpediatric KD. One case report described a 16-year-old female patient with heart failure, prolonged febrile illness, bilateral conjunctivitis, transaminitis, and elevated CRP.3 Several aneurysms were found on coronary artery angiography and persisted 1 year later.3 Another case described a 31-year-old woman with transient heart failure, including reduced LVEF and pulmonary edema in the acute phase of KD.4
Distributive and cardiogenic shock are involved in KDSS.1 Circulating inflammatory mediators cause decreased peripheral vascular resistance.1 Myocarditis with inflammatory cell infiltration and myocardial interstitial edema cause LV stiffness and impaired contraction.1, 5 Hashimoto et al.5 compared LV function and contraction before and after IVIG administration in patients with typical acute KD. The average patient age was 3.2 years, and none were hypotensive.5 Before IVIG, LV end-diastolic volume was decreased, with associated reduction in LV stroke volume and LVEF.5 All of these parameters improved after IVIG.5
Although myocarditis may be an intrinsic component of KD’s pathophysiologic process, we suggest that the shock state may occur more commonly in children because they are unable to hemodynamically compensate. When the illness is severe enough to cause hemodynamic instability in a febrile adult, he/she may be misdiagnosed with septic shock. This is dangerous for patients who then receive high-volume fluid resuscitation in the context of LV dysfunction. In fact, there may be cases that go unidentified. Because of its rare incidence in the adult population, KDSS is typically not considered, and this could delay or prohibit the patient from accessing disease-modifying treatment with IVIG.
A recent nationwide cohort study in Japan compared early (≤4 days), conventional (5-7 days), and late (8-10 days) IVIG administration in KD.6 The number of lesions, including coronary artery aneurysm and dilation at 30 days postsymptom onset, was reduced with early and conventional treatment compared with late therapy.6 IVIG treatment is generally safe and usually well tolerated. The most common adverse effects include fever (19%), nausea (14%), headache (28%), and urticaria (10%).7 One should also be aware of potential cardiac effects of the drug, which can be difficult to predict. An estimated 5% of recipients experience hypotension, and 7% become hypertensive.7
There is evidence supporting the potential use of infliximab in treatment-resistant cases.1, 8 Individuals treated with infliximab after failing conventional therapy were more likely to defervesce and show biochemical evidence of decreased inflammation.8 The use of infliximab in KD is likely safe and potentially effective. However, there are notable limitations to its use. Appropriate dosing for KD and KDSS, especially in adults, has not been determined. Furthermore, prospective trials are needed to understand infliximab’s impact on cardiac outcomes.
Conclusion
We believe KDSS should be on the differential for cases of rapidly developing shock, particularly in young adults with an infectious prodrome, in whom it may be under-recognized. We advocate for early identification to minimize delays in treatment with IVIG, which reverses LV dysfunction and decreases risk of long-term sequelae such as coronary artery aneurysms.
Acknowledgements
Vancouver General Hospital Radiology department for providing images.
Disclosures
The authors have no conflicts of interest to disclose.
Footnotes
Ethics Statement: The research reported has adhered to the relevant ethical guidelines.
See page 208 for disclosure information.
References
- 1.McCrindle B.W., Rowley A.H., Newburger J.W. Diagnosis, treatment, and long-term management of Kawasaki disease: a scientific statement for health professionals from the American Heart Association. Circulation. 2017;135:e927–e999. doi: 10.1161/CIR.0000000000000484. [DOI] [PubMed] [Google Scholar]
- 2.Kanegaye J.T., Wilder M.S., Molkara D. Recognition of a Kawasaki disease shock syndrome. Pediatrics. 2009;123:e783–e789. doi: 10.1542/peds.2008-1871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yamauchi A., Nakagawa N., Kawamura Y., Hasebe N. Incomplete Kawasaki disease manifesting as transient heart failure in a previously healthy adolescent. Intern Med. 2012;51:2169–2173. doi: 10.2169/internalmedicine.51.7413. [DOI] [PubMed] [Google Scholar]
- 4.Leclerc G., Bégin P., Laramée P., Genest P. Transient heart failure in an adult with Kawasaki disease. Clin Cardiol. 1986;9:128–130. doi: 10.1002/clc.4960090310. [DOI] [PubMed] [Google Scholar]
- 5.Hashimoto I., Saitou Y., Sakata N., Shibata K. Evaluation of longitudinal and radial left ventricular functions on 2-D and 3-D echocardiography before and after intravenous immunoglobulin in acute Kawasaki disease. Pediatr Int. 2017;59:1229–1235. doi: 10.1111/ped.13423. [DOI] [PubMed] [Google Scholar]
- 6.Kuwabara M., Yashiro M., Ae R., Yanagawa H., Nakamura Y. The effects of early intravenous immunoglobulin therapy for Kawasaki disease: The 22nd nationwide survey in Japan. Int J Cardiol. 2018;269:334–338. doi: 10.1016/j.ijcard.2018.07.092. [DOI] [PubMed] [Google Scholar]
- 7.Bonilla F.A. Intravenous immunoglobulin: adverse reactions and management. J Allergy Clin Immunol. 2008;122:1238–1239. doi: 10.1016/j.jaci.2008.08.033. [DOI] [PubMed] [Google Scholar]
- 8.Masuda H., Kobayashi T., Hachiya A. Infliximab for the treatment of refractory Kawasaki disease: a nationwide survey in Japan. J Pediatr. 2018;195 doi: 10.1016/j.jpeds.2017.10.013. 115-20.e3. [DOI] [PubMed] [Google Scholar]