Abstract
Background
Optimal design of clinical programs for patients with premature atherosclerotic cardiovascular disease (ASCVD) (men aged ≤ 50 years, women aged ≤ 55 years) requires an understanding of their priorities. We aimed to explore patient and family priorities for services in clinical programs.
Methods
We co-designed this study with a Patient Partner Committee using a sequential exploratory mixed-methods design. In Phase I, we conducted semistructured interviews with participants from the Study to Avoid Cardiovascular Events in British Columbia (SAVE BC) (n = 15). In Phase II, we designed a questionnaire based on Phase I data and distributed it to all current SAVE BC participants. We collected close-ended responses (n = 116) and stratified data using participant category (index, family member), age, sex, and number of clinic visits.
Results
We identified 4 major priorities for services in clinical programs: social support (weight: 62.6%), patient education (weight: 83.5%), mental health (weight: 50.7%), and lifestyle changes (85.1%). To address these priorities, participants wanted ASCVD clinical programs to enable recruitment of their family members, establish a comprehensive education component (with research updates in research programs), deliver mental health screening and support after myocardial infarction, and provide longitudinal sessions to support maintenance of lifestyle modifications. These services were identified in Phase I and verified in Phase II.
Conclusion
We identified 4 priorities for services in clinical programs designed for patients with premature ASCVD and their families. Further research should be done to elucidate their outcomes and most effective methods to provide these services.
Résumé
Introduction
La conception optimale des programmes cliniques des patients atteints d’une maladie cardiovasculaire athéroscléreuse (ASCVD pour atherosclerotic cardiovascular disease) prématurée (hommes âgés ≤ 50 ans, femmes âgées ≤ 55 ans) exige une compréhension de leurs priorités. Nous avions pour objectif d’examiner les priorités des patients et de leur famille en matière de services dans les programmes cliniques.
Méthodes
Nous avons conçu la présente étude en collaboration avec le Patient Partner Commitee à l’aide d’un devis séquentiel exploratoire en méthodes mixtes. À la Phase 1, nous avons réalisé des entrevues auprès de participants de la Study to Avoid Cardiovascular Events in British Columbia (SAVE BC) (n = 15). À la Phase II, nous avons conçu un questionnaire en nous basant sur les données de la Phase I et l’avons distribué à tous les participants actuels de la SAVE BC. Nous avons recueilli les réponses fermées (n = 116) et stratifié les données en utilisant la catégorie (indice, membre de la famille), l’âge, le sexe et le nombre de consultations des participants.
Résultats
Nous avons défini les 4 grandes priorités en matière de services dans les programmes cliniques : le soutien social (62,6 %), l’éducation des patients (83,5 %), la santé mentale (50,7 %) et les changements au mode de vie (85,1 %). Pour répondre à ces priorités, les participants voulaient des programmes cliniques sur la ASCVD pour favoriser le recrutement des membres de leur famille, établir un volet d’éducation complet (avec les dernières informations sur les travaux de recherche des programmes de recherche), offrir le dépistage de la santé mentale et le soutien après l’infarctus du myocarde, et offrir des séances longitudinales qui assureront le maintien des modifications au mode de vie. Ces services ont été définis à la Phase I et vérifiés à la Phase II.
Conclusion
Nous avons défini les 4 priorités en matière de services dans les programmes cliniques conçus pour les patients atteints d’une ASCVD prématurée et leur famille. D’autres recherches devraient être réalisées pour élucider leurs résultats et les méthodes les plus efficaces pour offrir ces services.
Premature atherosclerotic cardiovascular disease (ASCVD), defined as coronary artery disease in men aged ≤ 50 years and women aged ≤ 55 years, is an ongoing public health issue in Canada.1 More than 3800 men and 1000 women in these age groups are diagnosed with an acute myocardial infarction (MI) every year (Public Health Agency of Canada, Canadian Chronic Disease Surveillance System, 2012). Compared with older patients, younger patients have greater access to health information and have different social responsibilities, such as raising families, establishing careers, and attaining financial security. Many clinical and research programs recruit patients with premature ASCVD, but their priorities are not often considered in their design.
Traditional clinical research has viewed patients solely as research subjects, rather than as active partners. Therefore, the research focus is often derived from the interest of investigators, funding organizations, or clinicians, rather than that of patients and caregivers. Little has been done to identify the priorities of patients in clinical programs; however, patients can provide valuable insight into potential services that align with their priorities.2, 3 Such insights may include the importance of social support networks for patients with ASCVD, association of education in ASCVD to achievement of lifestyle goals, and depression as a major health problem in patients with ASCVD.4, 5, 6, 7 These priorities may be used to design healthcare programs more suited to the needs of its patients. Despite significant research in ASCVD, there is little known about priorities of patients with premature ASCVD and families regarding their preferred clinical services.
This exploratory sequential mixed-methods study investigated patient priorities for services within the Study to Avoid Cardiovascular Events in British Columbia (SAVE BC). SAVE BC is a prospective, observational study designed to identify patients with premature ASCVD (men ≤ aged 50 years or women aged ≤ 55 years) and provide long-term cardiovascular screening and risk stratification for their family members by using imaging and laboratory modalities (ie, carotid ultrasound, coronary artery calcium scoring, lipoprotein(a)).1 The overall purpose of SAVE BC is to improve the outcomes of such patients and to evaluate the yield of such a screening program. We identified major patient priorities for services in clinical programs. To the best of our knowledge, this is the first study to explore patient priorities for services in cardiovascular clinical programs.
Methods
We co-designed this study with the SAVE BC Patient Partner Committee (PPC), consisting of 6 patients with premature ASCVD and family members. The PPC contributed to writing the initial proposal, making revisions to research documents and providing insights into Phase I and II results (Supplemental Table S1).
Phase I: Qualitative semistructured interviews
We used semistructured interviews in Phase I to explore experiences with ASCVD and priorities for clinical services.8 We randomly selected participants of SAVE BC who had provided consent to contact by assigning each a number and using a random number generator. The inclusion criteria are the same as those listed in SAVE BC.1 Forty-five participants were invited, and 15 agreed to participate.
In-depth semistructured interviews were conducted via telephone by 2 members of the SAVE BC study team (Supplemental Fig. S1). A flexible interview guide co-designed with the PPC was used to explore participants’ experience with ASCVD and their thoughts on cardiovascular prevention programs and treatment options. These topics were developed through literature review on patient satisfaction in cardiac clinical programs.9, 10 Fifteen audio-recorded interviews were conducted, each lasting 30 to 45 minutes (Table 1).
Table 1.
Demographic information of participants in Phase I and Phase II
| Phase I | Phase II | |
|---|---|---|
| Total participants (N) | 15 | 116 |
| Sex (N) | ||
| Male | 8 | 68 |
| Female | 7 | 46 |
| Not specified | 0 | 2 |
| Mean age, y | 49.3 ± 10.6 | 48.4 ± 8.4 |
| Participant category (N) | ||
| Index | 8 | 75 |
| FDR | 4 | 24 |
| Spouse | 3 | 15 |
| Not specified | 0 | 2 |
| Attended appointments with SAVE BC (N) | ||
| Yes | 15 | 82 |
| No | 0 | 34 |
FDR, first-degree relative; SAVE BC, Study to Avoid cardioVascular Events in British Columbia.
Recordings were transcribed through a professional transcription service (Scriptastic). Qualitative thematic analysis was conducted using NVivo 10 (Version 10, 2012; QSR International Pty Ltd, Melbourne, Australia). Analyses to identify common themes were conducted independently by 2 researchers using a thematic network.11 The thematic network was continuously refined and verified between the researchers; discrepancies were discussed with the research team (8 researchers) until agreement was reached.
Phase II: quantitative questionnaire
The 4 themes identified in Phase I were used to develop a questionnaire to verify and further examine potential services in a larger cohort (Supplemental Appendix S1). Each question was linked to a theme that emerged from the interviews. Responses were collected using Likert-style and multiple-choice questions. All individuals in SAVE BC who had consented to being contacted for studies were invited to complete the questionnaire. The online questionnaire was administered and analyzed using Qualtrics software (Qualtrics, Provo, UT). T tests and chi-square tests were used to compare responses among participant demographics (index cases, first-degree relative [FDR], spouse), sex, ages, geographic locations, and whether they have attended clinic yet.
Results
In Phase I, 4 priorities for services in clinical programs were identified, including social support, education, mental health, and lifestyle modifications. The questionnaire (Phase II) was then distributed to all 315 consented SAVE BC participants, and 116 respondents completed it (36.9% response rate) (Table 1).
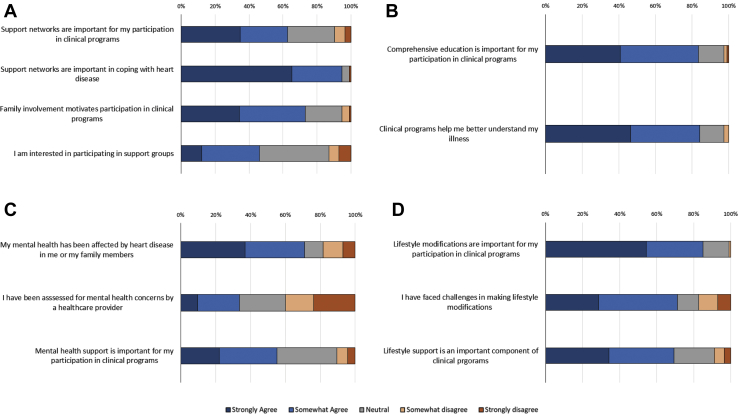
Social support
Questionnaire respondents believed that a support network was important in self-management of ASCVD (94.8%, n = 115) and in clinical program participation (62.6%, n = 115) (Fig. 1A). Index patients believed that having family members involved in clinical programs improved their own engagement (61.5%, n = 75) (Table 2). Of note, 79.3% (n = 82) of those who have attended a SAVE BC clinic wanted to see their family members enrolled, compared with 47.1% (n = 34) of those who had not (P = 0.0015).
Figure 1.
Participant responses to questionnaire categorized into questions pertaining to support network, education, mental health, and lifestyle changes. (A) Participants prioritize support networks for living with atherosclerotic cardiovascular disease (ASCVD) and research participation when enrolling in clinical research programs (n = 115). (B) Participants (83.5%) believe education encourages active participation in research, and many participate (84.2%) to better understand their illness (n = 114). (C) Mental health and services that address such concerns are priorities in managing ASCVD in clinical programs (n =114). (D) Participants believe that positive lifestyle changes and support programs promoting them improved their participation (n = 114).
Table 2.
Joint display of themes identified in Phase I qualitative phase, further examined in Phase II quantitative phase
| Organizing themes | Interview quotations | Questionnaire (“believe” indicates that patients “agree” or “strongly agree”) |
|---|---|---|
| Support network: Support networks are important for patients in coping with ASCVD. |
“Nobody can do it alone – you need a mother and a father, and it’s that positive reinforcement that I’m getting from my wife.” | 94.8% (N = 115) believe that a support network is important in recovery from heart disease. |
| Support network: Family plays a significant role in patients’ active participation in clinical research programs. |
“My participation in SAVE BC program is all for my daughter … because there is a family history of heart disease on my mom’s side.” | 62.6% (N = 115) believe that social support is an important area to address in clinical programs. 72.9% (N = 111) believe that family involvement encourages active participation. 61.5% (N = 75) of index patients want family members enrolled as co-participants, and 41.0% (N = 75) want them to undergo additional education. 79.3% (N = 85) of respondents who have attended a SAVE BC clinic want to see their family members enrolled compared with 47.1% (N = 35) who have not. |
| Support network: Participants prioritize a comprehensive support network. |
“Personally, I’m just one of those guys who shares stuff with my friends…mentally, emotionally, I’m pretty well taken care of.” “I think I’m going to have another heart attack and when I do, I can phone [SAVE BC] all over it. Usually within a day, he’s phoning me back.” “I talked with quite a few heart attack survivors, so we all talk about it.... It’s a therapy session for us as well.” |
Supports identified by interviewees (N = 116) 64.7% Informational support – advice, feedback 63.9% Emotional support – empathy, concern 39.7% Companionship support – sense of belonging 33.6% Tangible support –goods and services 46.1% (N = 115) currently or would like to participate in support groups for people with similar lived experiences. |
| Education: Patients desire education adapted to their own condition and interests. |
“I’m all about the why, why, why. And I will ask why 100 times if I have to…. That’s the attitude I take to SAVE BC.” | 83.5% (N = 114) expect patient-specific education in clinical programs. Top 5 topics for education in ASCVD (N = 116): 79.3% nutrition; 76.7% exercise; 67.2% etiology/pathophysiology; 66.4% psychological aspects; 66.4% medication Desired method of information delivery (N = 116): 59.4% Recommendation of reputable online resources 57.8% Private discussion w/ healthcare professional 56.0% Written information packages |
| Education: Patients want to be active members in the research process |
“Having an opportunity to participate in something that might help somebody else…. I like to do things that help people and if it’s helping my own, it’s more important. So [participation in SAVE BC] the best opportunity for me.” | 84.2% (N = 115) believe that education enables active participation in research programs. 91.4% (N = 116) want to receive updates on research findings. Top 3 reasons for participating in ASCVD research (N = 116): 84.5% Contribute to body of knowledge 75.0% Benefit personally from research 64.7% Help those close to them |
| Mental health: Acute cardiac events have a significant effect on patient and family mental health. |
“For the first 6 months after the event, I was having some depression issues. I’m seeing a psychiatrist to work through those…. It was basically fear of having another attack.” | 71.0% (N = 114) believe that heart disease has negatively affected their mental health. |
| Mental health: Patients with ASCVD desire greater mental health support for their psychosocial health and engagement. |
“They give a bunch of information, but it’s so overwhelming. They focus so much on you getting better but barely even talked about depression, which as far as I’m concerned is a major issue that needs to be dealt with as a heart attack survivor.” | 37.8% (N = 74) of index patients believe their mental health issues have been addressed by healthcare providers. 50.7% (N = 75) of index patients believe that mental health support is important for engagement in clinical programs. Top 5 avenues for mental health support (for participants who believe their mental health has been affected by ASCVD) (N = 81) 59.3% Stress management education 28.4% Shared-experience support groups 28.4% Referral to mental health specialist 19.8% Referral to community counselling |
| Lifestyle changes: Participants are well educated on the importance of lifestyle modifications. |
“The 2 pointers I give people is, I mean I know it’s common sense and it sounds funny but get moving and get rid of sugar.” | 85.1% (N = 114) believe that making lifestyle changes improves participation in clinical programs. |
| Lifestyle changes: Participants find challenges in motivating lifestyle changes and require longitudinal support to maintain it. |
“I enjoy food. It is a good time…my problem now is I just eat too much.” “Off again on again…he has times with more difficulty staying motivated to go to the gym.” |
71.3% (N = 115) believe that they have faced challenges in making lifestyle changes. 93.8% (N = 113) believe that exercise/dietary programs can help them make lifestyle changes. 69.3% (N = 114) believe that exercise/dietary components are important in cardiac clinical programs (only 8.8% disagree). Frequency participants would like to follow up for lifestyle changes (N = 114): 14.0% weekly 13.2% biweekly 42.1% monthly 20.2% yearly 5.3% 1-time event 5.3% never |
ASCVD, atherosclerotic cardiovascular disease; SAVE BC, Study to Avoid Cardiovascular Events in British Columbia.
Likewise, interviewees reported that social support, particularly from family members, was important in self-management of ASCVD. Emotional support and the burden of providing for their young families motivated their own health maintenance, which improved their engagement in clinical programs. For example, FDR #1 stated the following:
“I want to make sure that I, my wife, and my 2 daughters monitor their health and keep on the right track… if you’re not there, who’s going to look after them apart from their mother?”
Index patients primarily obtained emotional and informational support (ie, patient education/counselling) from family members and healthcare providers, respectively. For example, INDEX #2 stated that “[he] can’t just hand over [his] well-being to somebody else and just go with it… Explain, explain it to [him] again.” Each member of the index’s support network, including family, friends, other patients with similar experiences, and healthcare providers, played an important role in fulfilling their comprehensive needs.
Regarding clinical research programs, interviewees often participated to support their loved ones. Interviewees stated that demonstrable benefits (eg, cardiovascular risk factor screening of FDRs1) increased their likelihood of participating in research; INDEX #2 reported that “[his] participation in SAVE BC is all for [his] daughter.” Participants were also less likely to participate if there were little or no services with potential health benefits for them.
Education
Many questionnaire respondents (84.2%, n = 114) reported participating in SAVE BC to attain further education in ASCVD. They (83.5%, n = 114) believe that an established education component encourages active participation in clinical programs (Fig. 1B). When asked about topics they were interested in, respondents (n = 116) most often chose nutrition (79.3%) and exercise (76.7%), followed by pathophysiology (67.2%), psychosocial effects (66.4%), and medications (66.4%), topics that were identified in Phase I. Respondents preferred to have multiple methods of education delivery (Table 2). For research programs, most respondents (84.5%, n = 116) participated to contribute to scientific knowledge and wanted to receive updates on research findings.
Many interviewees reported that they relied on education from clinical programs to better understand their condition. SPOUSE #2 noted that “additional assistance in the early stages, where there’s lots of uncertainty” was effective in managing her functional limitations. Many patients continued to look for additional information on ASCVD to guide their lifestyle and reported that clinical programs with strong educational components fostered greater engagement. INDEX #5 stated the following:
“I am a person who will ask 1000 questions before I will give in to what I need. I’m not one that says ‘okay, well if you say so’… That’s the attitude I take to these programs.”
Interviewees found that 1-on-1 appointments, online resources, and personalized information packages were effective educational methods (Table 2). SPOUSE #3 “enjoyed talking to [SAVE BC physician], to see him as the real person” but also preferred routine follow-ups/education through emails for accessibility, “because [she] doesn’t always have a chance to read them in the middle of the day.” Many participants shared this perspective that education was more effective when multiple methods of delivery were offered.
Interviewees were interested in contributing to cardiovascular research and outreach. SPOUSE #2 stated, “If there’s a way to prevent [premature death] just by screening alone, then I think it’s worth it and I want to be a part of that.” They also believed there should be greater outreach efforts to identify and educate individuals at risk of ASCVD, “something similar to a yearly prostate exam or cancer screening” (INDEX #5).
Mental health
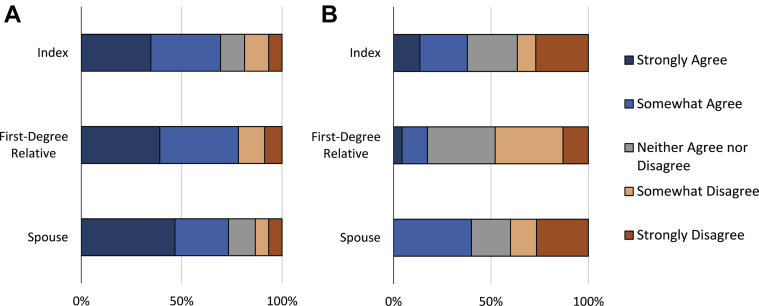
A majority of questionnaire respondents (71.0%, n = 114) believed their mental health was negatively affected by ASCVD (Fig. 1C). Regarding their mental health, index patients, FDRs, and spouses in our study were equally affected (Fig. 2). Despite this high burden, few patients (37.8%, n = 74) reported that their mental health was addressed by a healthcare worker. Many (50.7%, n = 75) believed that their participation would improve if mental health services were provided by clinical programs. Among those whose mental health was affected by ASCVD, 59.3% (n = 81) preferred primarily stress management education to other strategies identified in Phase I (Table 2).
Figure 2.
Responses to mental health questions, stratified by participant category. (A) “My mental health has been affected by heart disease affecting me or my family members” (P = 0.835). (B) “I have been assessed for mental health concerns by a healthcare provider” (P = 0.046).
Interviewees experienced significant stress and negative mood shifts after diagnosis of ASCVD. INDEX #7 was “angry and despondent every time [he] got a tweak in [his] chest.” INDEX #1 was “very shocked” and no longer felt “invincible.” Family members also reported their relatives’ cardiovascular event adversely affected their own mental health. Despite this, many experienced an overall lack of support from the healthcare system. INDEX #7 stated the following:
“[Healthcare workers] give a bunch of information but it’s so overwhelming. They focus so much on you getting better but barely even talked about depression, which as far as I’m concerned, is a major issue that needs to be dealt with as a heart attack survivor.”
Interviewees identified potential mental health services they would like offered through ASCVD clinical programs, including referral to mental health specialists, community counselling services, stress management education, and support groups (Table 2). INDEX #7 stated that “it helped that [he] was talking to other heart attack survivors,” when discussing the efficacy of support groups. Although there was no strong preference for any service, interviewees clearly wanted greater mental health support from healthcare workers.
Lifestyle changes
Questionnaire respondents (85.1%, n = 115) believed that lifestyle modifications improve participation in clinical programs (Fig. 1D). However, many (71.3%, n = 114) believed that they faced challenges in accomplishing lifestyle goals. They (93.8%, n = 114) believed structured supports for diet and exercise would help them maintain lifestyle modifications and a majority (69.3%, n = 114) desired monthly or more frequent supportive sessions (Table 2).
Participants were overall well educated on the benefits of lifestyle modifications, and many participated independently in exercise programs or cardiac rehabilitation as adjuncts to their personal efforts. Despite having few challenges in initiating lifestyle changes, participants often faced difficulties maintaining them, often due to anxiety and fatigue secondary to ASCVD. INDEX #7 stated the following:
“After my heart attack I was scared to do anything… I didn’t recognize that I was gaining weight, I was feeling listless and it took me almost a year after visiting [SAVE BC] to realize.”
Other interviewees were ambivalent to lifestyle modifications despite adequate education (Table 2). For example, INDEX #4 stated that “his problem is that [he] just eat too much” and has “difficulty staying motivated to exercise”; he “needs someone to come here each week, clear [his] cupboard.” For this issue, interviewees were more likely to maintain motivation when their lifestyle supports were consistent. They noted that long-term exercise programs and dietary resources/counselling (eg, books, dieticians) “reinforced the importance of exercise” and improved their daily nutrition, respectively.
Discussion
We explored the priorities of patients with premature ASCVD and their family members regarding services in clinical programs using an exploratory sequential mixed-methods design. We identified 4 major themes outlining those priorities: support network, education, mental health, and lifestyle changes. Because many participants sought out services addressing these priorities when deciding to enroll in clinical programs, those programs may want to consider implementing such services to support patient-identified health outcomes.
Limited social support is associated with increased risk of atherosclerosis, all-cause mortality, and lower quality of life.4, 5, 12 Our participants prioritized support networks, particularly from family members, in self-management of ASCVD and participation in clinical programs. This is supported by a study that assessed the feasibility of recruiting families into ASCVD clinical programs; family involvement was shown to improve lifestyle maintenance and overall engagement of index patients.13 Additionally, a significantly higher proportion of participants who have attended a SAVE BC clinic, compared with those who have not, wanted to see their family members enrolled. This suggests that clinical programs can optimize enrollment by engaging families after the index patient has been educated on the familial risk of ASCVD. Despite this, participant interest in support groups is markedly lower than the desire to engage family members. We hypothesize that interest in support groups is lower because emotional and informational needs are better met through loved ones and healthcare providers, a belief supported by our interviewees. Additionally, because ASCVD has low associated stigma (compared with human immunodeficiency virus, mental health, and so forth), participants are often more comfortable reaching out to loved ones for support. Therefore, programs should consider recruiting family members for improved cardiovascular risk reduction, engagement, and secondary prevention of ASCVD.
Comprehensive ASCVD education contributes to successful lifestyle modifications, but there is little agreement on the ideal method of its delivery.6 In this study, we identified clinically relevant topics and educational methods that were important to patients. Patients showed most interest in nutrition and exercise followed by pathophysiology, psychological effects, and medications for ASCVD. These suggest that patients are most interested in education related to lifestyle management of ASCVD.14 Participants preferred initial 1-on-1 clinic visits, take-home personalized information packages, and emails as their preferred methods of information delivery. Of note, many expressed a desire for a combination of these methods. A previous study supported the efficacy of this, showing that health education that uses multiple teaching strategies were more effective in changing behaviors.15 Meta-analyses of clinical cardiac programs also showed that the individual methods used to educate patients have limited effect on outcomes.16 Therefore, to improve information uptake and adherence, education should ideally be multifaceted and delivered according to patient preferences.
For research programs, many participants wanted to contribute actively and receive updates. Research programs ideally should have a plan for knowledge dissemination, including the preferred content and format of communication. As an example, our participants identified that they wanted to receive bimonthly newsletters outlining research in progress and innovations from other cardiovascular research groups. Patients often rely on information acquired through research participation to answer their personal questions.17 Therefore, fostering this discussion may promote further collaboration and identify patient-oriented research outcomes.
Depression is a significant health problem among people with ASCVD, with 20% of patients hospitalized for MI meeting the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition criteria for major depression.18 This may be caused by a bidirectional relationship between depression and ASCVD; adverse health behaviors associated with depression lead to worse cardiac outcomes, and their associated functional limitations may exacerbate depressive symptoms.19 Despite the high priority and prevalence (71.0%) of mental health concerns in all participants, few reported being assessed for them in the healthcare setting. Therefore, engagement in clinical programs may improve if providers are proactive in the discussion and care of mental health. It is important to note that participants preferred nonpharmacologic stress management education and peer support for post-MI mental health concerns. Because these tools have been shown to reduce the burden of mental health and improve cardiovascular outcomes, they warrant further consideration as potential tools in clinical programs.20, 21
Our patients found long-term lifestyle modifications challenging and required additional supports beyond simple education. They identified consistent and ongoing lifestyle support as effective tools in improving motivation. This is in agreement with previous studies that showed sustained support is more effective than a stand-alone counselling session in realizing lifestyle goals.22, 23 Psychosocial support for ASCVD, including cognitive behavioral therapy, was also shown to promote lifestyle changes.24 Regardless of methodology, our participants strongly believed that longitudinal strategies beyond short courses in cardiac rehabilitation were important to their long-term adherence to lifestyle goals. Therefore, a referral system to community-based programs that include exercise, smoking cessation, and dietary counselling may improve accessibility and reduce burden on clinical programs.22
Study limitations
This study has important limitations. By nature of the qualitative design, researcher bias and subjectivity are inevitable. We minimized this by having 2 researchers independently interpret interview transcripts, using analytical software, and achieving consensus with a team of 8 researchers. Additionally, the results may not be generalizable to all patients with ASCVD because SAVE BC participants are younger than most patients with ASCVD and are mainly residents of British Columbia or Yukon. Another significant limitation is the potential for sampling bias of the study participants. This study was conducted on patients already consented to participating in SAVE BC and potentially motivated by inclusion of family members. As a result, participants may be more engaged in health research than the general ASCVD population. This is particularly true in the patients participating in telephone interviews, who are more likely to be engaged in community endeavors.25 Therefore, the priorities identified in our study may be representative of participants who are more motivated and engaged than the general ASCVD population. Future studies should investigate these themes among a broader population who represent general patients with ASCVD.
Although the themes and potential services outlined in this study highlight the priorities of young patients with ASCVD and family members, further research is required to determine whether they improve health outcomes and objectively increase patient engagement. Future studies should explore patient outcomes, cost-effectiveness, and feasibility of such services. These studies can prioritize services that address both patient priorities and overall health outcomes, and thus encourage implementation in cardiovascular clinical programs.
Conclusions
We investigated the priorities of patients with premature ASCVD and their family members regarding services in clinical programs. Participants prioritized services that addressed support networks, patient education, mental health, and lifestyle changes. Accordingly, cardiovascular clinical programs could best address patient-oriented outcomes by (1) implementing a design that allows for enrollment of family members; (2) providing education that includes combinations of initial 1-on-1 consults and flexible information packages (and regular updates on research); (3) screening patients for mental health concerns and offering stress management education and other as-needed services; and (4) delivering consistent supportive sessions for lifestyle modifications. To the best of our knowledge, this is the first study that explores patient priorities for services in cardiovascular clinical programs. Future studies should implement these studies into clinical programs to determine the most effective methods to deliver on these priorities and their effect on cardiovascular outcomes.
Acknowledgements
The authors thank the members of the P.P.C. (K.B., K.W., T.W., D.G., J.A., and C.H.) who have generously given their expertise to improve the quality and design of this study, and all the SAVE BC participants for their continued support for our research and cardiovascular prevention research in general.
Funding Sources
This study was supported by a Strategy for Patient Oriented Research grant from the Canadian Institutes of Health Research (F16-06006) to L.R.B. L.R.B. is supported by a Canadian Institutes of Health Research New Investigator Award and is a Michael Smith Foundation for Health Research Scholar.
Disclosures
The authors have no conflicts of interest to disclose.
Footnotes
Ethics Statement: The research reported in this article has adhered to the relevant ethical guidelines.
See page 114 for disclosure information.
To access the supplementary material accompanying this article, visit CJC Open at https://www.cjcopen.ca and at https://doi.org/10.1016/j.cjco.2019.02.003.
Supplementary Material
References
- 1.Brunham L.R., Lynch K., English A. The design and rationale of SAVE BC: the Study to Avoid CardioVascular Events in British Columbia. Clin Cardiol. 2018;41:888–895. doi: 10.1002/clc.22959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Patient-Centered Comparative Effectiveness Research Center. Patient Engagement Best Practices Resource Document. 2015. Available at: http://bwhresearch.org/wp-content/uploads/2015/10/PCERC-Patient-Engagement-Best-Practices-Resource-Document.pdf. Accessed April 10, 2018.
- 3.Canadian Institutes of Health Research. Strategy for patient-oriented research: Patient engagement framework. 2014:1-11. Available at: http://www.cihr-irsc.gc.ca/e/48413.html. Accessed April 26, 2015.
- 4.Barth J., Schneider S., Von Känel R. Lack of social support in the etiology and the prognosis of coronary heart disease: a systematic review and meta-analysis. Psychosom Med. 2010;72:229–238. doi: 10.1097/PSY.0b013e3181d01611. [DOI] [PubMed] [Google Scholar]
- 5.Holt-Lunstad J., Smith T.B., Layton J.B. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7:e1000316. doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alm-Roijer C., Stagmo M., Udén G. Better knowledge improves adherence to lifestyle changes and medication in patients with coronary heart disease. Eur J Cardiovasc Nurs. 2004;3:321–330. doi: 10.1016/j.ejcnurse.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 7.Üstün T.B., Ayuso-Mateos J.L., Chatterji S. Global burden of depressive disorders in the year 2000. Br J Psychiatry. 2004;184:386–392. doi: 10.1192/bjp.184.5.386. [DOI] [PubMed] [Google Scholar]
- 8.Fetters M.D., Curry L.A., Creswell J.W. Achieving integration in mixed methods designs - principles and practices. Health Serv Res. 2013;48:2134–2156. doi: 10.1111/1475-6773.12117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rouleau C.R., King-Shier K.M., Tomfohr-Madsen L.M. A qualitative study exploring factors that influence enrollment in outpatient cardiac rehabilitation. Disabil Rehabil. 2018;40:469–478. doi: 10.1080/09638288.2016.1261417. [DOI] [PubMed] [Google Scholar]
- 10.Gill L., White L. A critical review of patient satisfaction. Leadersh Heal Serv. 2009;22:8–19. [Google Scholar]
- 11.Attride-Stirling J. Thematic networks: an analytic tool for qualitative research. Qual Res. 2001;1:385–405. [Google Scholar]
- 12.Bucholz E.M., Strait K.M., Dreyer R.P. The effect of low perceived social support on health outcomes in young patients with acute myocardial infarction: results from the VIRGO study. J Am Heart Assoc. 2014;3:1252. doi: 10.1161/JAHA.114.001252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schumacher T.L., Burrows T.L., Thompson D.I. Feasibility of recruiting families into a heart disease prevention program based on dietary patterns. Nutrients. 2015;7:7042–7057. doi: 10.3390/nu7085323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dobler C.C., Harb N., Maguire C.A. Treatment burden should be included in clinical practice guidelines. BMJ. 2018;4065:k4065. doi: 10.1136/bmj.k4065. [DOI] [PubMed] [Google Scholar]
- 15.Smith Anderson-Bill E., Winett R.A., Wojcik J.R. Social cognitive determinants of nutrition and physical activity among web-health users enrolling in an online intervention: the influence of social support, self-efficacy, outcome expectations, and self-regulation. J Med Internet Res. 2011;13:e28. doi: 10.2196/jmir.1551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mullen P.D., Mains D.A., Velez R. A meta-analysis of controlled trials of cardiac patient education. Patient Educ Couns. 1992;19:143–162. doi: 10.1016/0738-3991(92)90194-n. [DOI] [PubMed] [Google Scholar]
- 17.Sheikh Z.A., Hoeyer K. “Stop talking to people; talk with them”: a qualitative study of information needs and experiences among genetic research participants in Pakistan and Denmark. J Empir Res Hum Res Ethics. 2019;14:3–14. doi: 10.1177/1556264618780810. [DOI] [PubMed] [Google Scholar]
- 18.Lichtman J.H., Froelicher E.S., Blumenthal J.A. Depression as a risk factor for poor prognosis among patients with acute coronary syndrome. Circulation. 2014;129:1350–1369. doi: 10.1161/CIR.0000000000000019. [DOI] [PubMed] [Google Scholar]
- 19.Stein M.B., Cox B.J., Afifi T.O. Does co-morbid depressive illness magnify the impact of chronic physical illness? A population-based perspective. Psychol Med. 2006;36:587–596. doi: 10.1017/S0033291706007239. [DOI] [PubMed] [Google Scholar]
- 20.Lundgren O., Garvin P., Kristenson M. A journey through chaos and calmness: experiences of mindfulness training in patients with depressive symptoms after a recent coronary event - a qualitative diary content analysis. BMC Psychol. 2018;6:1–10. doi: 10.1186/s40359-018-0252-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Blumenthal J.A., Sherwood A., Babyak M.A. Effects of exercise and stress management training on markers of cardiovascular risk in patients with ischemic heart disease. JAMA. 2005;293:1626. doi: 10.1001/jama.293.13.1626. [DOI] [PubMed] [Google Scholar]
- 22.Gregory S., Bostock Y., Backett-Milburn K. Recovering from a heart attack: a qualitative study into lay experiences and the struggle to make lifestyle changes. Fam Pract. 2006;23:220–225. doi: 10.1093/fampra/cmi089. [DOI] [PubMed] [Google Scholar]
- 23.Tod A.M., Read C., Lacey A., Abbott J. Barriers to uptake of services for coronary heart disease: qualitative study. BMJ. 2001;323:214. doi: 10.1136/bmj.323.7306.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Astin F., Yusuf R., Closs S. Managing lifestyle change and medicines after coronary angioplasty: partners’ perspectives. Eur J Cardiovasc Nurs. 2010;9:S31. [Google Scholar]
- 25.Pew Research Center. Keeter S, Hatley N, Kennedy C, et al. What low response rates mean for telephone surveys. 2017. Available at: https://www.pewresearch.org/methods/2017/05/15/what-low-response-rates-mean-for-telephone-surveys. Accessed December 29, 2018.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.