ABSTRACT
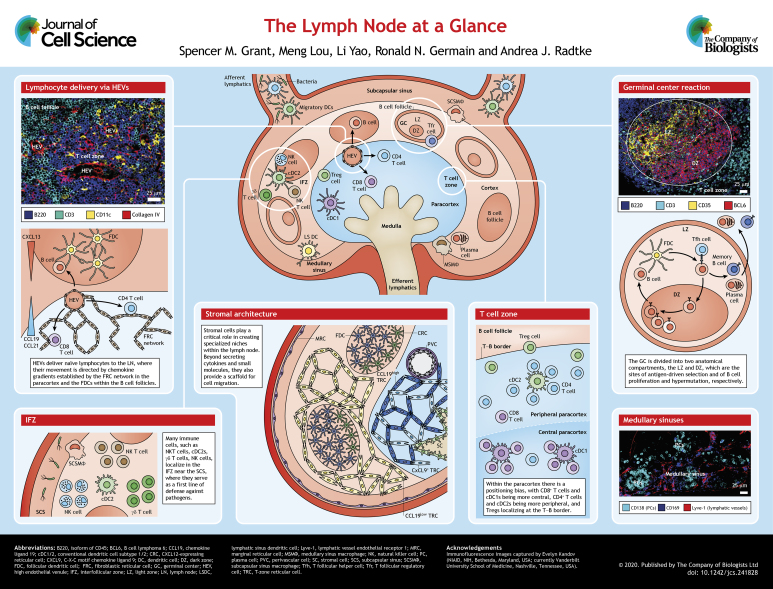
A hallmark of the mammalian immune system is its ability to respond efficiently to foreign antigens without eliciting an inappropriate response to self-antigens. Furthermore, a robust immune response requires the coordination of a diverse range of cells present at low frequencies within the host. This problem is solved, in part, by concentrating antigens, antigen-presenting cells and antigen-responsive cells in lymph nodes (LNs). Beyond housing these cell types in one location, LNs are highly organized structures consisting of pre-positioned cells within well-defined microanatomical niches. In this Cell Science at a Glance article and accompanying poster, we outline the key cellular populations and components of the LN microenvironment that are present at steady state and chronicle the dynamic changes in these elements following an immune response. This review highlights the LN as a staging ground for both innate and adaptive immune responses, while providing an elegant example of how structure informs function.
KEY WORDS: Adaptive immunity, Immunology, Innate immunity, Lymph node
Introduction
A defining characteristic of the immune system is its ability to respond robustly to a wide range of challenges (Wong and Germain, 2018). From bacteria breaching the skin, to pathogens traveling through the gastrointestinal tract, to self-reactive immune cells generated in primary and secondary lymphoid tissues, the immune response manages to consistently protect the host while minimizing collateral damage. Given the diversity of antigens and the low precursor frequency of antigen-specific lymphocytes that are at the heart of adaptive immunity, how does this system respond in a robust and efficient manner? The solution requires a dynamic system that is capable of responding and adapting to these unpredictable and evolving targets. As such, effective host defense relies on the strategic positioning of rare precursor cells that, upon detection of their cognate antigen on antigen-presenting cells, expand into a population of differentiated cells with diverse effector functions. To increase the probability that an immune response is mounted in a timely manner, these interactions are predominantly concentrated in one organ: the lymph node (LN).
In addition to distilling the peripheral tissue antigen landscape into discrete focal points, the LN performs several important functions, including pathogen containment, recruitment of naïve lymphocytes and antigen-presenting cells (APCs), generation of adaptive immune responses, suppression of autoreactive cells, and maintenance of memory through retention of antigens and central memory cells (Kastenmüller et al., 2012, 2013; Tew et al., 1984; von Andrian and Mempel, 2003; Gasteiger et al., 2016; Qi et al., 2014; Bajénoff et al., 2006; Girard et al., 2012). To manage these diverse activities, an additional layer of organization is required, which is achieved by localizing cells and their potential interacting partners into specialized niches within each individual LN. Owing to the diversity of pathogen entry points, humans have not one, but rather 500 to 600 LNs that are distributed throughout the body to provide region-specific immune responses (Moore and Bertram, 2019). Importantly, LNs that drain different regions of the intestine are both anatomically and functionally distinct (Carter and Collins, 1974; Mowat and Agace, 2014; Esterhazy et al., 2019). For instance, regulatory T cells (Tregs) express different surface receptors that direct their migration to specific tissues, a phenomenon that is largely defined by the draining LNs in which they reside (Fu et al., 2016). Similarly, the immunoglobulin isotypes of plasma cells, which partially determines the tissues they home to, is largely determined by the region of the body where they were initially exposed to antigen (Tufail et al., 2013). Here, we will discuss the key cellular players and structural elements of a representative LN at steady state, as well as during the early and late phases of an immune response.
Structure and organization of the LN
The lymphatic system is comprised of a network of vessels present throughout the body that are responsible for transporting lymph, which contains antigen and APCs. LNs are embedded throughout this extensive lymphatic vasculature and facilitate the induction of innate and adaptive immune responses by collecting soluble antigens from peripheral tissues (Girard et al., 2012). Lymphatic vessels that flow into the LN are called afferent lymphatic vessels, while those that flow out of the LN are efferent lymphatic vessels (see poster). Particles flow from the afferent to the efferent lymphatic vessels by means of LN sinuses, such as the subcapsular sinus (SCS) and medullary sinus. In addition to the lymphatic vessels, blood vessels known as high endothelial venules (HEVs) also branch throughout the LN (see Movie 1 for an animation of a voyage through the lymph node).
The LN is divided into three primary regions, namely, the cortex, paracortex and medulla (see poster). The cortex is the outermost region of the LN. Within the cortex are niches containing primarily B cells and follicular dendritic cells (FDCs), known as B cell follicles, as well as the interfollicular zone (IFZ), which separates the distinct B cell follicles. The interior region of the LN is the paracortex, also known as the T cell zone (TCZ). The paracortex contains fibroblastic reticular cells (FRCs), which are an integral component of the conduit system that branches throughout the paracortex. The medulla is located proximal to the efferent lymphatic vessels and contains the medullary sinuses (Qi et al., 2014) (see poster and Movie 1).
The organization of the LN into functionally distinct niches is largely due to the distribution of various stromal cell populations throughout the LN (Rodda et al., 2018) (see poster). Recent studies utilizing single-cell RNA sequencing suggest that there are up to nine spatially distinct, transcriptionally unique stromal cell populations. Marginal reticular cells (MRCs) scattered beneath the subcapsular sinus shuttle antigens to B cells, facilitating their homing towards the follicle through employment of CXCL13, and contribute to barrier defense by attenuating pathogen spread (Cyster et al., 2000; Katakai et al., 2008; Rodda et al., 2018). Within the paracortex are various populations of T-zone reticular cells (TRCs), which are characterized by their expression of CCL21 and CCL19. CCL19high (i.e. with high expression of CCL19) TRCs are critical for maintaining the conduit system and supporting DC motility (Mueller and Germain, 2009), while CCL19low TRCs reside near the border of the TCZ and B cell follicles (denoted the T–B border) and the IFZ and send survival signals to B cells (Rodda et al., 2018). Additionally, TRCs that express CXCL9 are located throughout the TCZ and IFZ, and play an important role in positioning dendritic cells (DCs) and T cells within the IFZ. Within the medulla are INMT+ stromal cells, which aide with cell–cell communication, and NR4A1+ stromal cells, which are also present at lower densities elsewhere in the LN. There are also stromal cells within the LN that largely support vasculature, such as perivascular cells (PvCs), which surround vessels in the medulla and cortex, and CD34+ adventitial cells (ACs), which support the capsule and large vessels in the medullary cords (Rodda et al., 2018).
The LN at steady state
Lymph formed in local tissues enters LNs through the afferent lymphatic vessels, travels through the subcapsular and medullary sinuses, and exits through efferent lymphatic vessels that eventually return the lymph to the blood circulation (see poster and Movie 1). This journey through the sinuses allows antigen and APCs, as well as naïve lymphocytes from upstream LNs (Braun et al., 2011), to be delivered to the paracortex (Sixt et al., 2005). Naïve lymphocytes also enter LNs through HEVs, which deliver them from the blood circulatory system to the paracortex (Marchesi and Gowans, 1964; Thomas et al., 2016).
From the paracortex, immune cells utilize stromal cells and chemical cues to migrate within the LN, resulting in the formation of localized compartments (Gretz et al., 1996). Intranodal movement is largely dictated by FRCs and FDCs (Bajénoff et al., 2006; Eisenbarth, 2019). FRCs serve as the primary mechanism of paracortical lymphocyte migration. T cells, along with many DCs, are predominantly localized in the LN paracortex (Bajénoff et al., 2006). Alternatively, B cells eventually migrate to the periphery towards FDCs to enter B cell follicles in the cortex (Ansel et al., 2000). Stromal cells direct movement of cells within the LN by secreting chemoattractant proteins known as chemokines (Griffith et al., 2014). CC-chemokine ligand 21 (CCL21), for instance, is expressed on the interior walls of HEVs and engages CC-chemokine receptor 7 (CCR7), which is expressed by both B and T cells (Carlsen et al., 2005; Braun et al., 2011). This permits naïve lymphocytes to adhere to the HEV wall and pass into the paracortex (Stein et al., 2000). Within the paracortex, they continue to migrate in response to CCL21, which is associated with the FRC network (Link et al., 2007; Denton et al., 2014). Eventually, T cells and B cells separate and migrate to the TCZ and B cell follicles, respectively (see poster and Movie 1). This is mediated, in part, by the expression of CXCR5 on B cells and their recruitment to the peripheral regions of the LN by CXCL13-expressing FDCs (Ansel et al., 2000).
In addition to the B cell follicles and the T cell zone, the medulla and IFZ represent two distinct regions of the LN (see poster). The medulla contains a dense meshwork of blood vessels enriched with antibody-secreting plasma cells (PCs) and macrophages (Gray and Cyster, 2012). Within the IFZ and cortical ridge, a reticular structure at the boundary of the T and B cell zones (Katakai et al., 2004), lies a diverse network of lymphoid cells (natural killer cells, γδ T cells, natural killer T cells, and innate-like CD8+ T cells) located adjacent to lymphatic sinus-lining sentinel macrophages (Kastenmüller et al., 2012). These cells are joined in the IFZ by cDC2, a specific subset of DCs that ultimately present antigen to CD4+ T cells (Gerner et al., 2017). Thus, the strategic prepositioning of innate and adaptive immune cells within the LN allows it to serve as a gateway between innate and adaptive immunity. However, efficient regulation of these responses is also required to prevent the generation of autoimmunity. Quantitative imaging and histo-cytometry have demonstrated that Tregs cluster at the T–B border where they were shown to interact with autoreactive effector T cells (Liu et al., 2015a,b). Therefore, the highly organized structure of the LN enables the induction and, importantly, regulation of innate and adaptive immune responses in an efficient and robust manner.
The early LN response – the integration of innate and adaptive immunity
LN-resident macrophages (LN-Mɸs) clear the lymph of transiting pathogens and play a seminal role in coordinating both the innate and adaptive arms of the immune response (Gray and Cyster, 2012). As a result of their intimate association with lymphatic sinuses, LN-Mɸs are strategically positioned to be directly exposed to lymph. Specifically, a population of CD169+ macrophages in the subcapsular sinus (SCSMɸs) capture large particles and microorganisms that enter the LN through the afferent lymphatic vessels (Girard et al., 2012) (see poster). In addition to aiding in pathogen surveillance, the close proximity of CD169+ SCSMɸs to lymphatic endothelial cells (LECs) and stromal cells has been also shown to be critical for the maintenance of these macrophages via production of the RANKL (also known as TNFSF11) cytokine and LEC-derived survival factor CSF-1 (Camara et al., 2019; Mondor et al., 2019). Additionally, inflammasome activation and subsequent production of the interleukins IL-1β and IL-18 by SCSMɸs recruit neutrophils to the LN and activate other components of the early innate response (Kastenmüller, 2012; Sagoo et al., 2016; Chtanova et al., 2008; Iannacone et al., 2010; Frederico et al., 2015). SCSMɸs are also important for the induction of adaptive immune responses in the LN. For example, SCSMɸs facilitate B cell priming by transferring antigens to B cell follicles, as well as immune complexes to FDCs (Carrasco and Batista, 2007; Junt et al., 2007; Phan et al., 2007, 2009; Aichele et al., 2003; Veninga et al., 2015). Importantly, disruption of this macrophage network has been shown to impair B cell responses (Gaya et al., 2015). Similar to SCSMɸs, LN-resident CD11b+ DCs (LS-DCs) are strategically positioned within the LN lymphatic sinus endothelium, where they capture particulate antigens and lymph-borne pathogens for efficient presentation to naïve T cells (Gerner et al., 2015). LS-DCs exhibit the capacity to initiate robust T cell responses much earlier than DCs migrating from the site of infection. However, migratory DCs further augment the immune response by delivering antigens from peripheral tissues that may not otherwise drain to the LN, as well as by presenting higher densities of processed antigen than LN-resident DCs.
Ultimately, these antigen-bearing DCs must engage antigen-specific CD4+ and/or CD8+ T cells in the paracortex. A recent study demonstrated that naïve CD4+ T cells and CD8+ T cells are not uniformly distributed throughout the paracortex of the LN (Baptista et al., 2019). By performing advanced quantitative imaging of mouse LNs, the authors showed that CD4+ T cells are enriched in the periphery of the LN paracortex in an Ebi2-dependent manner, with CD8+ T cells being more centrally located (Baptista et al., 2019). Importantly, XCR1+ cDC1s, canonically responsible for CD8+ T cell cross-priming, and CD11b+ cDC2s, associated with CD4+ T cell priming, exhibit a similarly biased distribution (Ingulli et al., 2002; Gerner et al., 2012; Eickhoff et al., 2015). In addition to creating distinct niches within the LN, the presence of these specialized DC subsets in areas enriched for CD4+ or CD8+ T cells increases the likelihood that APCs productively engage their cognate lymphocytes. Beyond spatial segregation, recent literature suggests temporal staggering between CD4+ and CD8+ T cell activation in peripheral infections where pathogens do not drain to the LN (Hor et al., 2015). Originally thought to occur in parallel, the spatiotemporal dynamics of CD4+ and CD8+ T cells suggest asynchronous kinetics of lymphocyte activation by a distinct subset of DCs. Following these peripheral infections, migratory DCs readily activate CD4+ T cells in the draining lymph node, but alone are inefficient in directly priming the CD8+ T cells that require lymph node-resident XCR1+ cDC1s for activation (Hor et al., 2015; Kitano et al., 2016; Eickhoff et al., 2015).
The enrichment of DCs and CD4+ T cells at the T–B border also plays a crucial role in promoting humoral immunity. Specifically, T follicular helper (Tfh) cells, CD4+ T cells uniquely specialized in providing growth, differentiation and survival signals to B cells (Crotty, 2019), are generated in spatially distinct peripheral regions of the LN. Within the IFZ and T–B border, DCs and B cells cooperate in the production of Tfh cells in two canonical phases. First, pre-Tfh cells interact with DCs (Kerfoot et al., 2011; Kitano et al., 2011; Watanabe et al., 2017), resulting in the upregulation of BCL6, the central regulator of Tfh development, and CXCR5, the chemokine receptor that directs migration to the B cell follicle (Chen et al., 2015; Choi et al., 2011; DiToro et al., 2018). Secondly, upon entering the B cell follicle, they interact with B cells to complete their differentiation to mature Tfh cells (Qi et al., 2008; Kerfoot et al., 2011; Kitano et al., 2011; Liu et al., 2015a,b; Watanabe et al., 2017). These studies demonstrate that rapid cellular and humoral responses are facilitated by the strategic positioning of APCs and antigen-responsive lymphocytes within distinct LN niches.
The late LN response – the generation of memory
Following their interactions at the T–B border (Allen et al., 2007b; Qi et al., 2008; Kerfoot et al., 2011; Kitano et al., 2011), B and Tfh cells migrate towards the center of the B cell follicle near the FDCs and form a distinct substructure called the germinal center (GC) (Mesin et al., 2016; Victora and Nussenzweig, 2012; Cyster and Allen, 2019) (see poster). The GC microenvironment coordinates interactions between a diverse array of cells – Tfh cells, activated B cells, FDCs and tingible body macrophages – and fosters the development of highly antigen-specific B cells and PCs (Crotty, 2019). Much of our understanding of these dynamic structures has been informed by state-of-the-art imaging techniques and transgenic animal models (Allen et al., 2007b; Qi et al., 2008; Victora et al., 2010; Liu et al., 2015a,b; Tas et al., 2016). These studies and others have demonstrated that B cells begin to proliferate within the first 2–3 days after the GC initially forms. Meanwhile, the GC organizes itself into two distinct zones, the dark zone (DZ) and the light zone (LZ) (see poster), that promote optimal B cell responses through mutation, expansion and selection (Allen et al., 2004, 2007a,b; Bannard and Cyster, 2017; Victora et al., 2010; De Silva et al., 2015). One mechanism by which B cells change the structure of their immunoglobulin is class switch recombination (CSR), which occurs before entry into the GC and entails distinct rearrangements of the DNA segments encoding the various constant regions of the B cell receptor (BCR) or its secreted counterpart (Toellner et al., 1996; Roco et al., 2019). Another mechanism is somatic hypermutation (SHM), which introduces point mutations in the DNA encoding the antigen-binding region of BCRs of DZ B cells while they are multiplying (Berek et al., 1991). Owing to the largely random nature of SHM, these mutations yield a wide variety of BCR-recognition structures. Within the DZ, B cell interactions and migration patterns are largely directed by CXCL12-expressing reticular cells (CRCs) (Rodda et al., 2015). After that, selection for high-affinity B cells takes place in the LZ, where B cells must endure a thorough screening process that ultimately determines their fate. B cells with high-affinity BCRs are able to efficiently capture antigen from FDCs and present it to Tfh cells within the LZ, whereas the remaining B cells, which fail to present antigen in a manner that is sufficient to productively engage the Tfh, undergo apoptosis or return to the DZ (Suzuki et al., 2009; Allen et al., 2007a; Bannard and Cyster, 2017; Victora et al., 2010; Ise et al., 2018). While such a high volume of random mutations during the late response optimizes the affinity of differentiated B cells, it also introduces the potential to generate autoreactive B cells. One particular Treg subset known as follicular regulatory T (Tfr) cells help to prevent such responses (Chung et al., 2011; Linterman et al., 2011; Wollenberg et al., 2011; Zhu et al., 2015; Sage and Sharpe, 2016). Tfr cells have long been thought to exert their regulatory functions within the GC, but it has recently been shown that these cells are enriched at the T–B border of human LNs, suggesting that they execute their functions largely outside of the GC (Sayin et al., 2018).
B cells that survive the rigorous rounds of selection in the GC differentiate into either PCs or memory B cells, each playing distinct roles in humoral immunity (Cyster and Allen, 2019). PCs are terminally differentiated and secrete large amounts of high-affinity antibodies that can rapidly neutralize their target antigens (Nutt et al., 2015). Although recruitment and retention in the bone marrow is thought to be critical for long-term PC survival (Radbruch et al., 2006), a population of PCs remain in the LN medulla where they may provide an added layer of defense against lymph-borne pathogens (Fooksman et al., 2010). In contrast to PCs, memory B cells are not terminally differentiated and therefore can adapt to antigens related to the original priming antigen by re-entering the GC and undergoing further SHM of their B cell receptor (Kurosaki et al., 2015). To facilitate this process, memory B cells may continue circulating in the bloodstream and lymphatic system (Roy et al., 2002), or strategically localize in tissues that are near pathogen entry points (Liu et al., 1995; Fazilleau et al., 2007; Inoue et al., 2018). While beyond the scope of this article, it is important to note that the LN is an active site of T cell memory development and a population of memory CD8+ T cells has been found to be retained near pathogen entry sites (Mueller et al., 2013; Kastenmüller et al., 2013). In summary, the production and retention of these cells, along with memory B cells, highlights the critical role of the LN in the generation and maintenance of cellular and humoral immune responses.
Conclusions and perspectives
Within the past 20 years, our understanding of the LN has expanded beyond basic anatomy and function to yield an appreciation of a highly organized structure comprised of pre-positioned cells in well-defined niches. Advanced imaging techniques, developed by our laboratory and others (Allen et al., 2007b; Qi et al., 2008; Victora et al., 2010; Germain et al., 2012; Gerner et al., 2012; Jarjour et al., 2014; Liu et al., 2015a,b; Tas et al., 2016; Li et al., 2017, 2019), have been critical in defining the spatial relationships and dynamic behavior of lymphocytes and other cell types within this organ. In addition to describing critical associations between cells and their interacting partners, these studies have also revealed important spatial separations, such as the low frequency of DCs in the B cell follicle. While the exact function of this dissociation is unknown, it is tempting to speculate that DCs are prevented from entering the follicle to prevent their competition with B cells, an APC required for Tfh development. In addition to this question, many others remain to be explored. What is the significance of this discrete compartmentalization of the LN? How does it vary between LNs, individuals and with age? To this end, our ability to answer these questions, as well as many others, will undoubtedly benefit from the Human Cell Atlas and their efforts to apply cutting edge techniques – single-cell RNA sequencing, high dimensional imaging, and artificial intelligence – to the mapping of individual cells within human LNs (Regev et al., 2018, preprint). Thus, we fully anticipate that the principles outlined here will be continuously refined with additional advances in technology.
Supplementary Material
Footnotes
Competing interests
The authors declare no competing or financial interests.
Funding
Our work in this area is supported by the Intramural Research program of the Division of Intramural Research, National Institute of Allergy and Infectious Diseases (NIAID), NIH. Deposited in PMC for release after 12 months.
Supplementary information
Supplementary information available online at http://jcs.biologists.org/lookup/doi/10.1242/jcs.241828.supplemental
Cell science at a glance
A high-resolution version of the poster and individual poster panels are available for downloading at http://jcs.biologists.org/lookup/doi/10.1242/jcs.241828.supplemental
References
- Aichele P., Zinke J., Grode L., Schwendener R. A., Kaufmann S. H. E. and Seiler P. (2003). Macrophages of the splenic marginal zone are essential for trapping of blood-borne particulate antigen but dispensable for induction of specific T-cell responses. J. Immunol. 171, 1148-1155. 10.4049/jimmunol.171.3.1148 [DOI] [PubMed] [Google Scholar]
- Allen C. D. C., Ansel K. M., Low C., Lesley R., Tamamura H., Fuji N. and Cyster J. G. (2004). Germinal center dark and light zone organization is mediated by CXCR4 and CXCR5. Nat. Immunol. 5, 943-952. 10.1038/ni1100 [DOI] [PubMed] [Google Scholar]
- Allen C. D. C., Okada T. and Cyster J. G. (2007a). Germinal-center organization and cellular dynamics. Immunity 27, 190-202. 10.1016/j.immuni.2007.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen C. D. C., Okada T., Tang H. L. and Cyster J. G. (2007b). Imaging of germinal center selection events during affinity maturation. Science 315, 528-531. 10.1126/science.1136736 [DOI] [PubMed] [Google Scholar]
- Ansel K. M., Ngo V. N., Hyman P. L., Luther S. A., Förster R., Sedgwick J. D., Browning J. L., Lipp M. and Cyster J. G. (2000). A chemokine driven positive feedback loop organizes lymphoid follicles. Nature 406, 309-314. 10.1038/35018581 [DOI] [PubMed] [Google Scholar]
- Bajénoff M., Egen J. G., Koo L. Y., Laugier J. P., Brau F., Glaichenhaus N. and Germain R. N. (2006). Stromal cell networks regulate lymphocyte entry, migration, and territoriality in lymph nodes. Immunity 25, 989-1001. 10.1016/j.immuni.2006.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bannard O. and Cyster J. C. (2017). Germinal centers: programmed for affinity maturation and antibody diversification. Curr. Opin. Immunol. 45, 21-30. 10.1016/j.coi.2016.12.004 [DOI] [PubMed] [Google Scholar]
- Baptista A. P., Gola A., Huang Y., Milanez-Almeida P., Torabi-Parizi P., Urban J. F. Jr, Shapiro V. S., Gerner M. Y. and Germain R. N. (2019). The chemoattractant receptor Ebi2 drives intranodal naive CD4+ T cell peripheralization to promote effective adaptive immunity. Immunity 50, 1188-1201. 10.1016/j.immuni.2019.04.001 [DOI] [PubMed] [Google Scholar]
- Berek C., Berger A. and Apel M. (1991). Maturation of the immune response in germinal centers. Cell 67, 1121-1129. 10.1016/0092-8674(91)90289-B [DOI] [PubMed] [Google Scholar]
- Braun A., Worbs T., Moschovakis G. L., Halle S., Hoffmann K., Bölter J., Münk A. and Förster R. (2011). Afferent lymph-derived T cells and DCs use different chemokine receptor CCR7-dependent routes for entry into the lymph node and intranodal migration. Nat. Immunol. 12, 879-887. 10.1038/ni.2085 [DOI] [PubMed] [Google Scholar]
- Camara A., Cordeiro O. G., Alloush F., Sponsel J., Chypre M., Onder L., Asano K., Tanaka M., Yagita H., Ludewig B. et al. (2019). Lymph node mesenchymal and endothelial stromal cells cooperate via the RANK-RANKL cytokine axis to shape the sinusoidal macrophage niche. Immunity 50, 1467-1481. 10.1016/j.immuni.2019.05.008 [DOI] [PubMed] [Google Scholar]
- Carlsen H. S., Haraldsen G., Brandtzaeg P. and Baekkevold E. S. (2005). Disparate lymphoid chemokine expression in mice and men: no evidence of CCL21 synthesis by human high endothelial venules. Blood 106, 444-446. 10.1182/blood-2004-11-4353 [DOI] [PubMed] [Google Scholar]
- Carrasco Y. R. and Batista F. D. (2007). B cells acquire particulate antigen in a macrophage-rich area at the boundary between the follicle and the subcapsular sinus of the lymph node. Immunity 27, 160-171. 10.1016/j.immuni.2007.06.007 [DOI] [PubMed] [Google Scholar]
- Carter P. B. and Collins F. M. (1974). The route of enteric infection in normal mice. J. Exp. Med. 139, 1189-1203. 10.1084/jem.139.5.1189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen X., Ma W., Zhang T., Wu L. and Qi H. (2015). Phenotypic Tfh development promoted by CXCR5-controlled re-localization and IL-6 from radiation-resistant cells. Protein Cell 6, 825-832. 10.1007/s13238-015-0210-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi Y. S., Kageyama R., Eto D., Escobar T. C., Johnston R. J., Monticelli L., Lao C. and Crotty S. (2011). ICOS receptor instructs T follicular helper cell versus effector cell differentiation via induction of the transcriptional repressor Bcl6. Immunity 34, 932-946. 10.1016/j.immuni.2011.03.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chtanova T., Schaeffer M., Han S.-J., van Dooren G. G., Nollmann M., Herzmark P., Chan S. W., Satija H., Camfield K., Aaron H. et al. (2008). Dynamics of neutrophil migration in lymph nodes during infection. Immunity 29, 487-496. 10.1016/j.immuni.2008.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung Y., Tanaka S., Chu F., Nurieva R., Martinez G. J., Rawal S., Wang Y.-H., Lim H. Y., Reynolds J. M., Zhou X.-M. et al. (2011). Follicular regulatory T (Tfr) cells with dual Foxp3 and Bcl6 expression suppress germinal center reactions. Nat. Med. 17, 983-988. 10.1038/nm.2426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crotty S. (2019). T follicular helper cell biology: a decade of discovery and diseases. Immunity 50, 1132-1148. 10.1016/j.immuni.2019.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyster J. G. and Allen C. D. C. (2019). B cell responses: cell interaction dynamics and decisions. Cell 177, 524-540. 10.1016/j.cell.2019.03.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyster J. G., Ansel K. M., Reif K., Ekland E. H., Hyman P. L., Tang H. L., Luther S. A. and Ngo V. N. (2000). Follicular stromal cells and lymphocyte homing to follicles. Immunol. Rev. 176, 181-193. 10.1034/j.1600-065X.2000.00618.x [DOI] [PubMed] [Google Scholar]
- De Silva N. S. and Klein U. (2015). Dynamics of B cells in germinal centres. Nat. Rev. Immunol. 15, 137-148. 10.1038/nri3804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denton A. E., Roberts E. W., Linterman M. A. and Fearon D. T. (2014). Fibroblastic reticular cells of the lymph node are required for retention of resting but not activated CD8+ T cells. Proc. Natl. Acad. Sci. USA 111, 12139-12144. 10.1073/pnas.1412910111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiToro D., Winstead C. J., Pham D., Witte S., Andargachew R., Singer J. R., Wilson C. G., Zindl C. L., Luther R. J., Silberger D. J. et al. (2018). Differential IL-2 expression defines developmental fates of follicular versus non follicular helper T cells. Science 14, 361 10.1126/science.aao2933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eickhoff S., Brewitz A., Gerner M. Y., Klauschen F., Komander K., Hemmi H., Garbi N., Kaisho T., Germain R. N. and Kastenmüller W. (2015). Robust anti-viral immunity requires multiple distinct T cell-dendritic cell interactions. Cell 162, 1322-1337. 10.1016/j.cell.2015.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenbarth S. C. (2019). Dendritic cell subsets in T cell programming: location dictates function. Nat. Rev. Immunol. 19, 89-103. 10.1038/s41577-018-0088-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esterhazy D., Canesso M. C. C., Mesin L., Muller P. A., de Castro T. B. R., Lockhart A., ElJalby M., Faria A. M. C. and Mucida D. (2019). Compartmentalized gut lymph node drainage dictates adaptive immune responses. Nature 569, 126-130. 10.1038/s41586-019-1125-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fazilleau N., Eisenbraun M. D., Malherbe L., Ebright J. N., Pogue-Caley R. R., McHeyzer-Williams L. J. and McHeyzer-Williams M. G. (2007). Lymphoid reservoirs of antigen-specific memory T helper cells. Nat. Immunol. 8, 753-761. 10.1038/ni1472 [DOI] [PubMed] [Google Scholar]
- Fooksman D. R., Schwickert T. A., Victora G. D., Dustin M. L., Nussenzweig M. C. and Skokos D. (2010). Development and migration of plasma cells in the mouse lymph node. Immunity 33, 118-127. 10.1016/j.immuni.2010.06.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frederico B., Chao B., Lawler C., May J. S. and Stevenson P. G. (2015). Subcapsular sinus macrophages limit acute gammaherpesvirus dissemination. J. Gen. Virol. 96, 2314-2327. 10.1099/vir.0.000140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu H., Ward E. J. and Marielli-Berg F. M. (2016). Mechanisms of T cell organotropism. Cell. Mol. Life Sci. 73, 3009-3033. 10.1007/s00018-016-2211-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasteiger G., Ataide M. and Kastenmüller W. (2016). Lymph node - an organ for T-cell activation and pathogen defense. Immunol. Rev. 271, 200-220. 10.1111/imr.12399 [DOI] [PubMed] [Google Scholar]
- Gaya M., Castello A., Montaner B., Rogers N., Reis e Sousa C., Bruckbauer A. and Batista F. D. (2015). Inflammation-induced disruption of SCS macrophages impairs B cell responses to secondary infection. Science 347, 667-672. 10.1126/science.aaa1300 [DOI] [PubMed] [Google Scholar]
- Germain R. N., Robey E. A. and Cahalan M. D. (2012). A decade of imaging cellular motility and interaction dynamics in the immune system. Science 336, 1676-1681. 10.1126/science.1221063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerner M. Y., Kastenmüller W., Ifrim I., Kabat J. and Germain R. N. (2012). Histo- cytometry: a method for highly multiplex quantitative tissue imaging analysis applied to dendritic cell subset microanatomy in lymph nodes. Immunity 37, 364-376. 10.1016/j.immuni.2012.07.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerner M. Y., Torabi-Parizi P. and Germain R. N. (2015). Strategically localized dendritic cells promote rapid T cell responses to lymph-borne particulate antigens. Immunity 42, 172-185. 10.1016/j.immuni.2014.12.024 [DOI] [PubMed] [Google Scholar]
- Gerner M. Y., Casey K. A., Kastenmüller W. and Germain R. N. (2017). Dendritic cell and antigen dispersal landscapes regulate T cell immunity. J. Exp. Med. 214, 3105-3122. 10.1084/jem.20170335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Girard J.-P., Moussion C. and Förster R. (2012). HEVs, lymphatics and homeostatic immune cell trafficking in lymph nodes. Nat. Rev. Immunol. 12, 762-773. 10.1038/nri3298 [DOI] [PubMed] [Google Scholar]
- Gray E. E. and Cyster J. G. (2012). Lymph node macrophages. J. Innate Immun. 4, 424-436. 10.1159/000337007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gretz J. E., Kaldjian E. P., Anderson A. O. and Shaw S. (1996). Sophisticated strategies for information encounter in the lymph node: the reticular network as a conduit of soluble information and a highway for cell traffic. J. Immunol. 157, 495-499. [PubMed] [Google Scholar]
- Griffith J. W., Sokol C. L. and Luster A. D. (2014). Chemokines and chemokine receptors: positioning cells for host defense and immunity. Anu. Rev. Immunol. 32, 659-702. 10.1146/annurev-immunol-032713-120145 [DOI] [PubMed] [Google Scholar]
- Hor J. L., Whitney P. G., Zaid A., Brooks A. G., Heath W. R. and Mueller S. N. (2015). Spatiotemporally distinct interactions with dendritic cell subsets facilitates CD4+ and CD8+ T cell activation to localized viral infection. Immunity 43, 554-565. 10.1016/j.immuni.2015.07.020 [DOI] [PubMed] [Google Scholar]
- Iannacone M., Moseman E. A., Tonti E., Bosurgi L., Junt T., Henrickson S. E., Whelan S. P., Guidotti L. G. and von Andrian U. H. (2010). Subcapsular sinus macrophages prevent CNS invasion on peripheral infection with a neurotropic virus. Nature 465, 1079-1083. 10.1038/nature09118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingulli E., Ulman D. R., Lucido M. M. and Jenkins M. K. (2002). In situ analysis reveals physical interactions between CD11b+dendritic cells and antigen-specific CD4 T cells after subcutaneous injection of antigen. J. Immunol. 169, 2247-2252. 10.4049/jimmunol.169.5.2247 [DOI] [PubMed] [Google Scholar]
- Inoue T., Moran I., Shinnakasu R., Phan T. G. and Kurosaki T. (2018). Generation of memory B cells and their reactivation. Immunol. Rev. 283, 138-149. 10.1111/imr.12640 [DOI] [PubMed] [Google Scholar]
- Ise W., Fujii K., Shiroguchi K., Ito A., Kometani K., Takeda K., Kawakami E., Yamashita K., Suzuki K., Okada T. et al. (2018). T follicular helper cell-germinal center B cell interaction strength regulates entry into plasma cell or recycling germinal center cell Fate. Immunity 48, 702-715. 10.1016/j.immuni.2018.03.027 [DOI] [PubMed] [Google Scholar]
- Jarjour M., Jorquera A., Mondor I., Wienert S., Narang P., Coles M. C., Klauschen F. and Bajénoff M. (2014). Fate mapping reveals origin and dynamics of lymph node follicular dendritic cells. J. Exp. Med. 211, 1109-1122. 10.1084/jem.20132409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Junt T., Moseman E. A., Iannacone M., Massberg S., Lang P. A., Boes M., Fink K., Henrickson S. E., Shayakhmetov D. M., Paolo N. C. D. et al. (2007). Subcapsular sinus macrophages in lymph nodes clear lymph-borne viruses and present them to antiviral B cells. Nature 450, 110-114. 10.1038/nature06287 [DOI] [PubMed] [Google Scholar]
- Kastenmüller W., Torabi-Parizi T., Subramanian N., Lämmermann T. and Germain R. N. (2012). A spatially-organized multicellular innate immune response in lymph nodes limits systemic pathogen spread. Cell 150, 1235-1248. 10.1016/j.cell.2012.07.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kastenmüller W., Brandes M., Wang Z., Herz J., Egen J. G. and Germain R. N. (2013). Peripheral prepositioning and local CXCL9 chemokine-mediated guidance orchestrate rapid memory CD8+ T cell responses in the lymph node. Immunity 13, 502-513. 10.1016/j.immuni.2012.11.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katakai T., Hara T., Lee J. H., Gonda H., Sugai M. and Shimizu A. (2004). A novel reticular stromal structure in lymph node cortex: an immuno-platform for interactions among dendritic cells, T cells and B cells. Int. Immunol. 16, 1133-1142. 10.1093/intimm/dxh113 [DOI] [PubMed] [Google Scholar]
- Katakai T., Suto H., Sugai M., Gonda H., Togawa A., Suematsu S., Ebisuno Y., Katagiri K., Kinashi T. and Shimizu A. (2008). Organizer-like reticular stromal cell layer common to adult secondary lymphoid organs. J. Immunol. 181, 6189-6200. 10.4049/jimmunol.181.9.6189 [DOI] [PubMed] [Google Scholar]
- Kerfoot S. M., Yaari G., Patel J. R., Johnson K. L., Gonzalez D. G., Kleinstein S. H. and Haberman A. M. (2011). Germinal center B cell and T follicular helper cell development initiates in the interfollicular zone. Immunity 34, 947-960. 10.1016/j.immuni.2011.03.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitano M., Saya M., Yoshikazu A., Hikida M., Mori Y., Kurosaki T. and Okada T. (2011). Bcl6 protein expression shapes pre-germinal center B cell dynamics and follicular helper T cell heterogeneity. Immunity 34, 961-972. 10.1016/j.immuni.2011.03.025 [DOI] [PubMed] [Google Scholar]
- Kitano M., Yamazaki C., Takumi A., Ikeno T., Hemmi H., Takahashi N., Shimizu K., Fraser S. E., Hoshino K., Kaisho T. et al. (2016). Imaging of the cross-presenting dendritic cell subsets in the skin-draining lymph node. Proc. Natl Acad. Sci. USA 113, 1044-1049. 10.1073/pnas.1513607113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurosaki T., Kometani K. and Ise W. (2015). Memory B cells. Nat. Rev. Immunol. 15, 149-159. 10.1038/nri3802 [DOI] [PubMed] [Google Scholar]
- Li W., Germain R. N. and Gerner M. Y. (2017). Multiplex, quantitative cellular analysis in large tissue volumes with clearing-enhanced 3D microscopy (Ce3D). Proc. Natl. Acad. Sci. USA 114, E7321-E7330. 10.1073/pnas.1708981114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li W., Germain R. N. and Gerner M. Y. (2019). High-dimensional cell-level analysis of tissues with Ce3D multiplex volume imaging. Nat. Protoc. 14, 1708-1733. 10.1038/s41596-019-0156-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link A., Vogt T. K., Favre S., Britschgi M. R., Acha-Orbea H., Hinz B., Cyster J. G. and Luther S. A. (2007). Fibroblastic reticular cells in lymph nodes regulate the homeostasis of naive T cells. Nat. Immunol. 8, 1255-1265. 10.1038/ni1513 [DOI] [PubMed] [Google Scholar]
- Linterman M. A., Pierson W., Lee S. K., Kallies A., Kawamoto S., Rayner T. F., Srivastava M., Divekar D. P., Beaton L., Hogan J. J. et al. (2011). Foxp3+ follicular regulatory T cells control the germinal center response. Nat. Med. 17, 975-982. 10.1038/nm.2425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y.-J., Barthélémy C., de Bouteiller O., Arpin C., Durand I. and Banchereau J. (1995). Memory B cells from human tonsils colonize mucosal epithelium and directly present antigen to T cells by rapid up-regulation of B7-1 and B7-2. Immunity 2, 239-248. 10.1016/1074-7613(95)90048-9 [DOI] [PubMed] [Google Scholar]
- Liu D., Xu H., Shih C., Wan Z., Ma X., Ma W., Luo D. and Qi H. (2015a). T–B-cell entanglement and ICOSL-driven feed-forward regulation of germinal centre reaction. Nature 517, 214-218. 10.1038/nature13803 [DOI] [PubMed] [Google Scholar]
- Liu Z., Gerner M. Y., Van Panhuys N., Levine A. G., Rudensky A. Y. and Germain R. N. (2015b). Immune homeostasis enforced by co-localized effector and regulatory T cells. Nature 528, 225-230. 10.1038/nature16169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marchesi V. T. and Gowans J. L. (1964). The migration of lymphocytes through the endothelium of venules in lymph nodes: an electron microscopic study. Proc. R. Soc. Lond. B. Biol. Sci. 159, 283-290. 10.1098/rspb.1964.0002 [DOI] [PubMed] [Google Scholar]
- Mesin L., Ersching J. and Victora G. D. (2016). Germinal center B cell dynamics. Immunity 45, 471-482. 10.1016/j.immuni.2016.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mondor I., Baratin M., Lagueyrie M., Saro L., Henri S., Gentek R., Suerinck D., Kastenmuller W., Jiang J. X. and Bajénoff M. (2019). Lymphatic endothelial cells are essential components of the subcapsular sinus macrophage niche. Immunity. 50, 1453-1466. 10.1016/j.immuni.2019.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore J. E. and Bertram C. D. (2019). Lymphatic system flows. Annu. Rev. Fluid Mech. 50, 459-482. 10.1146/annurev-fluid-122316-045259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mowat A. M. and Agace W. W. (2014). Regional specialization within the intestinal immune system. Nat. Rev. Immunol. 14, 667-685. 10.1038/nri3738 [DOI] [PubMed] [Google Scholar]
- Mueller S. N. and Germain R. N. (2009). Stromal cell contributions to the homeostasis and functionality of the immune system. Nat. Rev. Immunol. 9, 618-629. 10.1038/nri2588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller S. N., Gebhardt T., Carbone F. R. and Heath W. R. (2013). Memory T cell subsets, migration patterns, and tissue residence. Annu. Rev. Immunol. 31, 137-161. 10.1146/annurev-immunol-032712-095954 [DOI] [PubMed] [Google Scholar]
- Nutt S. L., Hodgkin P. D., Tarlinton D. M. and Corcoran L. M. (2015). The generation of antibody-secreting plasma cells. Nat. Rev. Immunol. 15, 160-171. 10.1038/nri3795 [DOI] [PubMed] [Google Scholar]
- Phan T. G., Grigorova I., Okada T. and Cyster J. G. (2007). Subcapsular encounter and complement-dependent transport of immune complexes by lymph node B cells. Nat. Immunol. 8, 992-1000. 10.1038/ni1494 [DOI] [PubMed] [Google Scholar]
- Phan T. G., Green J. A., Gray E. E., Xu Y. and Cyster J. G. (2009). Immune complex relay by subcapsular sinus macrophages and noncognate B cells drives antibody affinity maturation. Nat. Immunol. 10, 786-793. 10.1038/ni.1745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi H., Cannons J. L., Klauschen F., Schwartzberg P. L. and Germain R. N. (2008). SAP-controlled T-B cell interactions underlie germinal centre formation. Nature 455, 764-769. 10.1038/nature07345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi H., Kastenmüller W. and Germain R. N. (2014). Spatiotemporal basis of innate and adaptive immunity in secondary lymphoid tissue. Anu. Rev. Cell Dev. Biol. 30, 141-167. 10.1146/annurev-cellbio-100913-013254 [DOI] [PubMed] [Google Scholar]
- Radbruch A., Muehlinghaus G., Luger E. O., Inamine A., Smith K. G. C., Dörner T. and Hiepe F. (2006). Competence and competition: the challenge of becoming a long-lived plasma cell. Nat. Rev. Immunol. 6, 741-750. 10.1038/nri1886 [DOI] [PubMed] [Google Scholar]
- Regev A., Teichmann S., Rozenblatt-Rosen O., Stubbington M., Ardlie K., Amit I., Arlotta P., Bader G., Benoist C., Biton M. et al. (2018). The human cell atlas white paper. arXiv:1810.05192v1 [q-bio.TO] 1-109. [Google Scholar]
- Roco J. A., Mesin L., Binder S. C., Nefzger C., Gonzalez-Figueroa P., Canete P. F., Ellyard J., Shen Q., Robert P. A., Cappello J. et al. (2019). Class-switch recombination occurs infrequently in germinal centers. Immunity 51, 337-350. 10.1016/j.immuni.2019.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodda L. B., Bannard O., Ludewig O., Nagasawa T. and Cyster J. G. (2015). Phenotypic and morphological properties of germinal center dark zone Cxcl12-expressing reticular cells. J. Immunol. 195, 4781-4791. 10.4049/jimmunol.1501191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodda L. B., Bennet M. L., Sokol C. L., Wang X., Luther S. A., Barres B. A., Luster A. D., Ye C. J. and Cyster J. G. (2018). Single-Cell RNA Sequencing of lymph node stromal cells reveals niche-associated heterogeneity. Immunity 48, 1014-1028. 10.1016/j.immuni.2018.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy M. P., Kim C. H. and Butcher E. C. (2002). Cytokine control of memory B cell homing machinery. J. Immunol. 169, 1676-1682. 10.4049/jimmunol.169.4.1676 [DOI] [PubMed] [Google Scholar]
- Sage P. T. and Sharpe A. H. (2016). T follicular regulatory cells. Immunol. Rev. 271, 246-259. 10.1111/imr.12411 [DOI] [PubMed] [Google Scholar]
- Sagoo P., Garcia Z., Breart B., Lemaitre F., Michonneau D., Albert M. L., Levy Y. and Bousso P. (2016). In vivo imaging of inflammasome activation reveals a subcapsular macrophage burst response that mobilizes innate and adaptive immunity. Nat. Medicine. 22, 64-71. 10.1038/nm.4016 [DOI] [PubMed] [Google Scholar]
- Sayin I., Radtke A. J., Vella L. A., Jin W., Wherry E. J., Buggert M., Betts M. R., Herati R. S., Germain R. N. and Canaday D. H. (2018). Spatial distribution and function of T follicular regulatory cells in human lymph nodes. J. Exp. Med. 215, 1531-1542. 10.1084/jem.20171940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sixt M., Kanazawa N., Selg M., Samson T., Roos G., Reinhardt D. P., Pabst R., Lutz M. B. and Sorokin L. (2005). The conduit system transports soluble antigens from the afferent lymph to resident dendritic cells in the T cell area of the lymph node. Immunity 22, 19-29. 10.1016/j.immuni.2004.11.013 [DOI] [PubMed] [Google Scholar]
- Stein J. V., Rot A., Luo Y., Narasimhaswamy M., Nakano H., Gunn M. D., Matsuzawa A., Quackenbush E. J., Dorf M. E. and von Andrian U. H. (2000). The CC chemokine thymus- derived chemotactic agent 4 (TCA-4, secondary lymphoid tissue chemokine, 6ckine, exodus-2) triggers lymphocyte function-associated antigen 1-mediated arrest of rolling T lymphocytes in peripheral lymph node high endothelial venules. J. Exp. Med. 191, 61-76. 10.1084/jem.191.1.61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suzuki K., Grigorova I., Phan T. G., Kelly L. M. and Cyster J. G. (2009). Visualizing B cell capture of cognate antigen from follicular dendritic cells. J. Exp. Med. 206, 1485-1493. 10.1084/jem.20090209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tas J. M., Mesin L., Pasqual G., Targ S., Jacobsen J. T., Mano Y. M., Chen C. S., Weill J.-C., Reynaud C.-A., Browne E. P. et al. (2016). Visualizing antibody affinity maturation in germinal centers. Science 351, 1048-1054. 10.1126/science.aad3439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tew J. G., Mandel T. E., Phipps R. P. and Szakal A. K. (1984). Tissue localization and retention of antigen in relation to the immune response. Am. J. Anat. 170, 407-420. 10.1002/aja.1001700314 [DOI] [PubMed] [Google Scholar]
- Thomas S. N., Rohner N. A. and Edwards E. E. (2016). Implications of lymphatic transport to lymph nodes in immunity and immunotherapy. Annu. Rev. Biomed Eng. 18, 207-233. 10.1146/annurev-bioeng-101515-014413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toellner K. M., Gulbranson-Judge A., Taylor D. R., Sze D. M. and Maclennan I. C. (1996). Immunoglobulin switch transcript production in vivo related to the site and time of antigen-specific B cell activation. J. Exp. Med. 183, 2303-2312. 10.1084/jem.183.5.2303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tufail S., Badrealam K. F., Sherwani A., Gupta U. D. and Owais M. (2013). Tissue specific heterogeneity in effector immune cell response. Front. Immunol. 4, 1-10. 10.3389/fimmu.2013.00254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veninga H., Borg E. G. F., Vreeman K., Taylor P. R., Kalay H., van Kooyk Y., Kraal G., Martinez-Pomares L. and den Haan J. M. M. (2015). Antigen targeting reveals splenic CD169+ macrophages as promoters of germinal center B-cell responses. Eur. J. Immunol. 45, 747-757. 10.1002/eji.201444983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Victora G. D. and Nussenzweig M. C. (2012). Germinal centers. Annu. Rev. Immunol. 30, 429-457. 10.1146/annurev-immunol-020711-075032 [DOI] [PubMed] [Google Scholar]
- Victora G. D., Schwickert T. A., Fooksman D. R., Kamphorst A. O., Meyer-Hermann M., Dustin M. L. and Nussenzweig M. C. (2010). Germinal center dynamics revealed by multiphoton microscopy with a photoactivatable fluorescent reporter. Cell 143, 592-605. 10.1016/j.cell.2010.10.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Von Andrian U. H. and Mempel T. R. (2003). Homing and cellular traffic in lymph nodes. Nat. Rev. Immunol. 3, 867-878. 10.1038/nri1222 [DOI] [PubMed] [Google Scholar]
- Watanabe M., Fujihara F., Radtke A. J., Chiang Y. J., Bhatia S., Germain R. N. and Hodes R. J. (2017). Co-stimulatory function in primary germinal center responses: CD40 and B7 are required on distinct antigen-presenting cells. J. Exp. Med. 214, 2795-2810. 10.1084/jem.20161955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wollenberg I., Agua-Doce A., Hérnandez A., Almeida C., Oliveira V. G., Faro J. and Graca L. (2011). Regulation of the germinal center reaction by Foxp3+ follicular regulatory T cells. J. Immunol. 187, 4552-4560. 10.4049/jimmunol.1101328 [DOI] [PubMed] [Google Scholar]
- Wong H.S. and Germain R.N. (2018). Robust control of the adaptive immune system. Semin Immunol. 36, 17-27. 10.1016/j.smim.2017.12. [DOI] [PubMed] [Google Scholar]
- Zhu Y., Zou L. and Liu Y.-C. (2015). T follicular regulatory cells and autoimmunity. Int. Immunol. 28, 173-179. 10.1093/intimm/dxv079 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.