Supplemental Digital Content is available in the text.
Keywords: critical illness, experience-based co-design, intensive care, postintensive care syndrome, peer support, qualitative methods, recovery
Objectives:
To use experience-based co-design to identify the key design requirements of a peer support model for critical care survivors; understand the use of the experience-based co-design method from clinician, patients, and family perspectives.
Design:
Using experience-based co-design, qualitative data about participants’ preferences for a peer support model were generated via workshops. Participants’ perspectives of experience-based co-design were evaluated with focus groups.
Setting:
University-affiliated hospital in Melbourne, Australia.
Subjects:
Snowball sampling was used to recruit clinicians from across the care spectrum (ICU-community); critical care survivors and nominated family members were recruited using convenience sampling.
Measurements and Main Results:
Consensus on a peer support model was reached through the experience-based co-design process, with the following key themes: 1) socialization and group cohesion; 2) management of potential risks; and 3) individualized needs of patients and families. Evaluation of participants’ perspectives of the experience-based co-design method identified five key themes: 1) participation as a positive experience; 2) emotional engagement in the process; 3) learning from patients and family members; 4) feeling heard; and 5) practical challenges of experience-based co-design and readiness to participate.
Conclusions:
Experience-based co-design was a feasible approach to developing a peer support model for use with critical care survivors and was well received by participants. Future testing of the co-designed peer support model in a pilot randomized controlled trial will enhance understanding of peer support in critical care and the use of experience-based co-design as a design methodology.
Following critical care, patients and families often experience postintensive care syndrome (PICS) encompassing long-term disability with impairments in physical, cognitive, and mental health (1). Peer support may reduce the severity of PICS by providing crucial social support (2) and has been effective in stroke (3), traumatic brain injury (4), and cancer (5) populations. To date, there is a paucity of research investigating peer support in critical care (6).
Within the contemporary healthcare landscape, impetus to engage patients and families in service design continues to grow (7, 8). Experience-based co-design (EBCD) facilitates the design of healthcare services in partnership with patients and families rather than for them (9). It is a form of participatory action research (10) which seeks to understand how people experience a process or service (11). The benefits of EBCD include a systematic method to incorporate the unique insights of patients and families, with the ultimate aim of improving service quality and the patient experience (12), which may also positively impact clinician well-being (10, 13). EBCD’s effectiveness is evident in cancer services (14) and mental illness (15) yet has not been evaluated within a critical care cohort to date. Potential barriers to the application of EBCD in the critical care context include challenges in reaching this cohort posthospital discharge due to ongoing disease burden, numerous appointments, physical limitations, and difficulties traveling back to the hospital. We therefore sought to ascertain whether it was feasible to use EBCD to design a service for critical care survivors.
Given that ICU interventions have traditionally been developed solely from the clinicians’ perspective (2, 16) with little structured patient and family input, this study aimed to:
1) Use EBCD to identify the key design requirements of a peer support model including logistics, barriers, and facilitators to implementation and
2) Understand the perspectives of participating clinicians, patients, and their family members in the use of EBCD.
MATERIALS AND METHODS
This study is reported using Consolidated Criteria for Reporting Qualitative Research checklist (17).
Setting
The study was conducted between June 2017 and September 2017, at a university-affiliated hospital. The ICU comprises 27-beds across two sites (level III tertiary referral centers, admitting over 1,600 critically ill adult patients annually).
Study Design
Qualitative inquiry was used to: 1) interpret the data generated through the EBCD process and 2) evaluate use of EBCD, as it provides an interpretative approach to describe complex phenomena that do not fit a quantitative model of hypothesis testing (18, 19). A phenomenological approach (20) was used to identify themes from the data generated via two methodological processes:
1) EBCD method (aim 1): EBCD is a form of participatory action research (10), seeking to understand how people experience a process or service (11). Core aspects of this methodology include use of filmed patient and family narratives, workshops with patients, families, and clinicians to explore their narratives including identification of “touch points”—pivotal moments of truth that shape a person’s overall experience, and then in partnership working together to co-design an improved experience (10, 21). Participants’ perceptions of key design features of a potential peer support mode to improve the recovery experience were explored at these workshops, including logistics, barriers, and facilitators to implementation and
2) Evaluation of EBCD (aim 2): Focus groups were conducted to investigate participants’ perspectives of participating in the EBCD method (Supplemental Appendix 1, Supplemental Digital Content 1, http://links.lww.com/CCX/A6).
Ethics Approval
The institutional ethics committee approved the study (HREC/17/MH/31). All participants provided written informed consent.
Sample and Recruitment
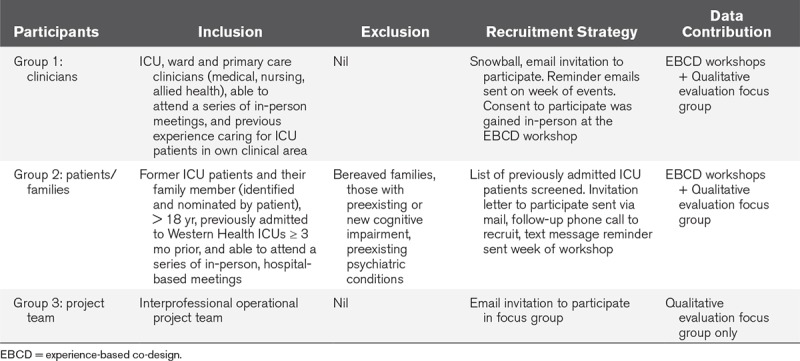
Eligible participant groups were screened, recruited, and contributed data (Table 1).
TABLE 1.
Participant Selection, Recruitment, and Data Contribution
EBCD Workshops.
Snowball sampling was used to recruit eligible clinicians (group 1) from the target population (nursing, medical, allied health) across the care arc from ICU, acute, sub-acute, and community settings. Convenience sampling was used to recruit former critical care patients and their nominated family member (group 2). An approximate group size of 10–15 clinicians (group 1) and 10–15 patients/families (group 2) was estimated to provide sufficient information power for descriptions of different experiences, contributing new knowledge (22).
Evaluation of EBCD Focus Groups.
Purposive sampling was used to invite groups 1 and 2, along with the eight members of the project team (group 3) to participate in the focus groups.
Data Collection and Procedure
Demographics were collected by individual electronic surveys (groups 1 and 3) and from hospital medical records for patients and telephone for families (group 2). The dual processes of this study are summarized (details in Supplemental Appendix 2, Supplemental Digital Content 1, http://links.lww.com/CCX/A6):
-
1) EBCD method (Supplemental Fig. 1, Supplemental Digital Content 2, http://links.lww.com/CCX/A7; legend: Outline of EBCD Method): Three separate, 2-hour workshops took place over 3 months:
a) Workshop 1 (participant group 1);
b) Workshop 2 (participant group 2); and
c) Workshop 3 (both groups, based on attendee availability).
In workshops 1 and 2, participants’ perspectives on positive and negative experiences of recovery from the ICU stay, hospitalization, and returning home were captured (e.g., clinician participants provided their perspectives on how well they thought care was delivered to support patients/families in their recovery as they transitioned across the care arc, whereas patient and family participants provided the lived experience). Ideas for how the service could be improved were captured in an experience map (Supplemental Appendix 2, Supplemental Digital Content 1, http://links.lww.com/CCX/A6). Potential barriers and facilitators to setting up a peer support model were discussed. In the third workshop, both groups collaborated to define and reach consensus on how the peer support model might operate.
2) Qualitative evaluation of EBCD: Subsequently, all groups were invited to participate in three separate, 1-hour, follow-up focus groups to understand their experiences of the EBCD method.
Data Analysis
EBCD workshop data were transcribed, stored, and managed in Excel for Mac 2011 (Version 14.1.0; Microsoft Corporation, Santa Rosa, CA). Focus group data were managed in Word for Mac 2011 (Version 14.7.7; Microsoft Corporation, Santa Rosa, CA); participants checked the relevant focus group transcript for accuracy. Three coders (K.J.H., C.H., K.C.) independently analyzed the data from multiple collection points, using accepted thematic analysis techniques (24), to reach consensus on the main themes.
RESULTS
Participants
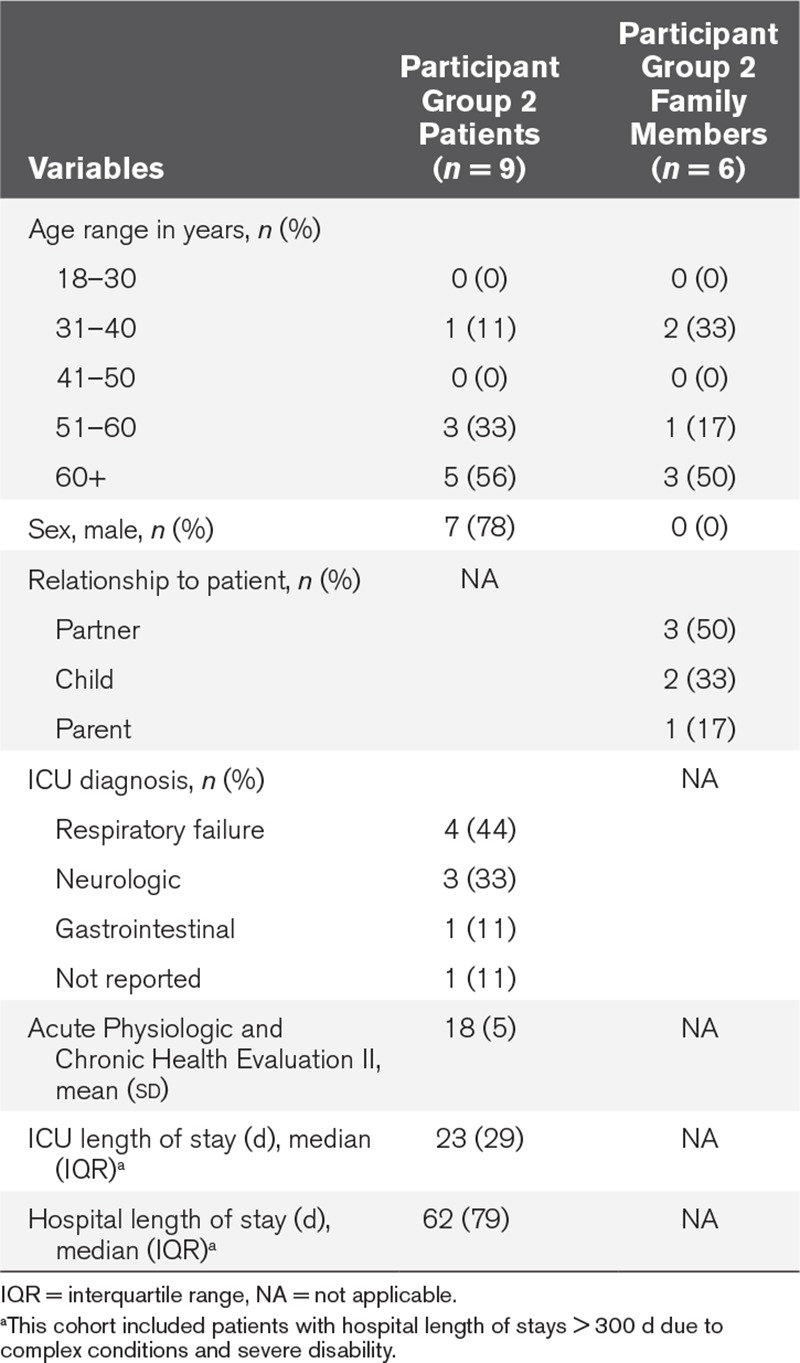
A cross-section of clinicians from varied professional groups and clinical areas participated (Table 2 and Fig. 1). Patients represented a middle-aged, male, long-stay ICU cohort (Table 3).
TABLE 2.
Clinicians and Project Team Demographics
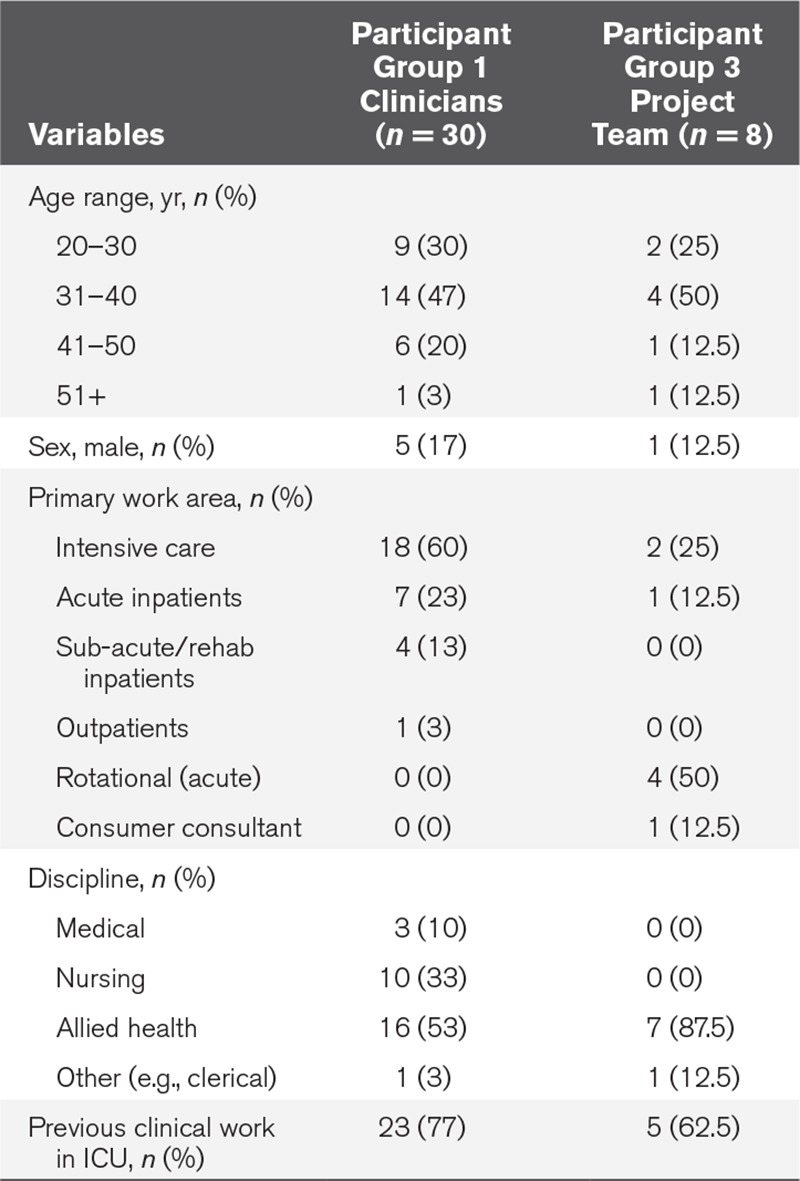
Figure 1.
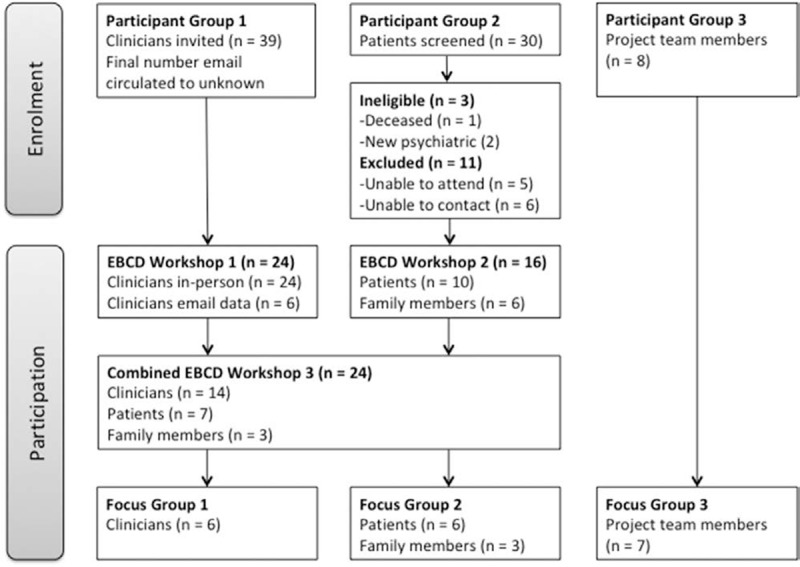
Participant flow diagram. EBCD = experience-based co-design.
TABLE 3.
Patient and Family Member Demographics
Major Themes—EBCD Method to Develop a Peer Support Model
Peer support was viewed as a mechanism to “discuss the lived experience—there is limited opportunity for patients to talk with others with a similar experience” (participant 21, clinician). Patients and family members emphasized the importance of sharing experiences and having “an opportunity to deal with the emotional and psychologic” (participant 8, patient).
Consensus on a peer support model was readily reached through the EBCD process. In addition, the following themes were identified across the EBCD workshops (Supplemental Table 1, Supplemental Digital Content 1, http://links.lww.com/CCX/A6):
1) Socialization and group cohesion;
2) Management of potential risks (e.g., responding to trauma); and
3) Individualized needs of patients and families.
Key Components of the Co-Designed Peer Support Model
Participants identified nine important components: 1) format; 2) frequency/duration; 3) session length; 4) location; 5) who; 6) content; 7) advertising; 8) supporting infrastructure; and 9) sustainability.
Participants spontaneously generated ideas to operationalize these core components (Supplemental Table 2, Supplemental Digital Content 1, http://links.lww.com/CCX/A6). In the third workshop, consensus was reached on the final peer support model (Supplemental Table 3, Supplemental Digital Content 1, http://links.lww.com/CCX/A6). The final model was defined as an in-person group; co-facilitated by a social worker/psychologist and a senior ICU clinician. The group will be delivered fortnightly for six sessions, held in a nonclinical room separate to the ICU, and include a formal educational component (delivered by expert clinicians on various topics relevant to postintensive care recovery) and an informal peer to peer component to facilitate social cohesion.
Clinicians identified logistical and attendance barriers to implementing the model, including conflicting patient appointments, timing, parking costs, funding, and staffing resources. In marked contrast, patients and family members focused on the positive aspects of attending peer support and offered practical solutions to allow flexibility for attendance and participation:
I’d travel to help others. My life was saved—I’ll do anything to help. (Participant 2, patient)
Socialization and Group Cohesion.
Both groups thought intentional effort was needed to facilitate social connections within the group to build trust rapidly, led by a skilled facilitator. Ideas to build social cohesion included: inviting participants to exchange personal telephone numbers if they wished; having a minimal structure with an opportunity to socialize; and organize activities for social interaction such as an outdoors barbeque. Participants considered technological platforms (e.g., Facebook, Skype) useful facilitators of social interaction, with the caveat these different modalities needed to suit patient/family preferences.
Managing Potential Risks.
Clinician participants identified sources of risk more readily than patients and family participants. Particularly, clinicians were concerned with the need to engage professional expertise to support the psychologic safety of the group:
Psychologist + social worker as expert facilitator to prevent transference of trauma. Training other staff to be able to respond appropriately to trauma to not make worse. (Participant 14, clinician)
The patients and family members were also very clear that clinicians with the requisite expertise (e.g., social worker, psychologist) should be present and assist group facilitation.
Individualized Needs of Patients and Family Members.
Participants spoke about unique needs of patients and family members. Clinicians discussed patients and families need support at different times and a potential barrier to participating in peer support:
Patients already feel a burden to their families (often due to increased care needs/medical appointments) and may not want to attend additional meetings (if they do not see value in it). (Participant 5, clinician)
Patients and family participants clearly identified that family members should be supported too.
Important to have a group for carers—they need support and someone to call. (Participant 1, family member)
Both groups proposed to ensure family members are catered for in a peer support group with the potential to split the group into patients and family members so that the content might be specifically tailored to their specific needs.
Major Themes—Evaluation of EBCD Process Itself
Five key themes were identified: 1) participation in EBCD as a positive experience; 2) emotional engagement in the process; 3) learning from patients and family members; 4) feeling heard; and 5) practical challenges of EBCD and readiness to participate.
Participation in EBCD As a Positive Experience.
Participation was described as an overwhelmingly positive, exciting, and rewarding experience for both clinicians and patient/family participants:
It was very dynamic and there was a lot of enthusiasm from both sides. (Participant 5, clinician)
it’s a very enriching and rewarding process to actually in real time have patients and families designing care… (Participant 2, project team).
…Turning a negative in to a positive (Participant 13, patient).
Clinicians commented that using an EBCD approach was a fair and open way to obtain perspectives and information; they appreciated the anonymity of using “sticky notes” (Supplemental Appendix 2, Supplemental Digital Content 1, http://links.lww.com/CCX/A6):
… a really good process for capturing a lot of people’s thoughts … very transparent. (Participant 2, clinician)
The patient and family members agreed the best aspect about being involved in the EBCD process was “being asked (to participate).”
Emotional Engagement in the Process.
Talking about recovery after critical illness was very emotional for patients and families. Recognition of this shared experience amongst patients and families provided an opportunity for human connection as illustrated following:
… it surprised you as well when that sort of emotion came up and this idea of connectedness of people of the same experience … there was something really powerful in that. (Participant 6, project team)
Patient and family participants demonstrated empathy when recalling and sharing their experiences with each other, especially when others exhibited visible distress. Reflecting on participating in EBCD, one patient commented: “There’s stuff I’ve said here that I’ve not said to my wife” (participant 5, patient) another stated “I’ve always refused to talk to anybody about it but I am now” (participant 9, patient). Managing and interacting within an emotionally charged environment was also demanding for the clinicians:
…some staff … actually struggled with the concept of having to come back face-to-face with some of these patients and families. (Participant 6, project team)
Clinicians Learning From Patients and Family Members.
Clinicians clearly identified the EBCD process gave them a greater understanding of the impact of an ICU stay on patients and families, influencing their practice to have greater empathy. One clinician identified their EBCD experience changed their approach to communication:
I try to communicate directly with … patients more, especially … longer staying ... explaining what has happened and encouraging other staff members to do the same. (Participant 6, clinician)
Clinicians discussed how the sessions with patients and family members provided “heightened awareness of what they actually go through” (participant 4, clinician) and that it was “quite confronting to realize the long-lasting effects of some ICU therapies for the patients” (participant 3, clinician).
Patients and Families Feeling Heard.
Patient and family members discussed the inclusive nature of the EBCD process to feel valued and heard:
You’re not being talked at you’re being talked to. There’s a big difference. (Participant 7, patient)
Clinician participants highlighted that EBCD provided an opportunity for patients and families to have a voice:
… it’s great hearing what they want … because we can all come up with grand ideas—to actually hear it from the survivors themselves. (Participant 3, clinician)
Practical Challenges of EBCD and Readiness to Participate.
Clear themes were identified from the focus group around the practicality and feasibility of the EBCD process. The session timing, duration, and location were identified as challenges with the process:
Just a negative for me is the timeframe because I work. (Participant 2, family member)
The clinicians and project team observed patient and family members had difficulty separating their own experiences from the task-driven aspects of the workshops, where they were being asked to help design improvements in care, often returning to their own story:
Some participants were only able to reflect on their experience and were not able to think more broadly. (Field observer)
DISCUSSION
This study demonstrated the feasibility of EBCD in the development of a peer support model within a critical care cohort. EBCD represents an advanced form of patient and family engagement in the design and delivery of health services, recognized as a key method by which to promote patient-centered care (25). To our knowledge, this is the first time EBCD has been used in the development of a peer support model in any patient cohort. In partnership, clinicians, patients, and family members were able to collaboratively build a peer support model, define key features, and address potential logistical issues and barriers to implementation. There are few studies demonstrating patient and family engagement to benefit the care of others (2, 8, 16). Our study is particularly novel as it not only demonstrates this form of engagement cannot only be done but how to involve patients and families in development of support services after critical care. By eliciting the perspectives of both patients, families and clinicians, a broader in-depth understanding of potential issues could be gained and solutions devised collaboratively, potentially strengthening the peer support model.
Our previous systematic review demonstrated mixed results of peer support in critical care, although it appeared to reduce psychologic morbidity and no models were designed using EBCD (26). We have successfully sought funding for and have commenced a pilot feasibility study of our co-designed peer support model (trial registration number: ACTRN12618000615280).
Participation in EBCD was a positive experience for all participants. Patients and families especially valued “being asked” and feeling heard, and often have few opportunities to provide insights to help improve the future care of others. Clinicians gained meaningful information through their interactions with patients and families during the EBCD process, generating greater empathy. There is growing evidence supporting the link between clinician well-being and patient experience (10, 13). EBCD offers a humanistic approach to service improvement that may contribute to better clinician engagement, addressing contemporary critical care workforce issues such as compassion fatigue and burnout (27), although this requires testing.
Strengths and Limitations
We engaged a cross-section of clinicians including ICU physicians, senior/junior nurses, physiotherapists, occupational therapists, psychologists, social workers, and speech-language therapists. There was less diversity in the patient/family participants who were primarily middle-aged males with accompanying female partners, which might reflect the recruitment strategy and local patient demographics. It is likely that EBCD primarily captures “very engaged” participants. Therefore, our designed model may not be generalizable, or acceptable to other ICU survivors.
Implications for Clinicians, Educators, and Administrators
This study is important for two key reasons: 1) There are few published examples of the systematic engagement of patients and families in the design of critical care services and research (17). This study demonstrates how to engage patients and families, using a methodology that is generalizable to other forms of service improvement (e.g., implementing the ICU Liberation bundle of care, end of life care, open visitation, inclusion of families on ward rounds) and 2) There is growing interest in peer support despite sparse data in critical care (26) and substantial variation in the specific services lumped together under the label “Peer Support” (28). This research describes an innovative approach to developing a peer support program, providing useful signposting for others, highlighting the details that ought to be considered when implementing this complex intervention. Key distinctions of the EBCD-developed model from existing models include design collaboratively led by patients, families, and clinicians rather than design led solely by clinicians, while otherwise reflecting similarities to the so-called “community-based model” (28).
Areas for Future Research
The co-designed model of peer support requires quantitative evaluation of feasibility and impact on patient and family-reported outcomes in adequately powered randomized controlled trials to inform clinical practice. Additional research into peer support model development from different hospitals and geographic locations is needed to make progress in peer support following critical illness (27).
CONCLUSIONS
EBCD produced a peer support model developed in partnership between clinicians, patients, and family members. EBCD was feasible in a critical care cohort and was viewed as a positive experience by those who participated in the study.
ACKNOWLEDGMENTS
We thank Ramona Hopkins for her article review and Bodil Rasmussen for her contribution to this research.
Supplementary Material
Footnotes
All authors contributed to study design and article preparation.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccejournal).
Drs. Haines’s, Holdsworth’s, Cranwell’s, Skinner’s, Holton’s, Bates’s, Booth’s, Carmody’s, Searle’s, and Shackell’s institutions received funding from Society of Critical Care Medicine (SCCM) (THRIVE grant) and Western Health. Dr. Skinner’s institution also received funding from Canadian Institutes of Health Research, National Health and Medical Research Council (Australia), HCF Research Foundation (Australia), and Deakin University (Australia), and she received funding from Western Health and Melbourne Health. Dr. Iwashyna disclosed that he is a government employee (U.S. Department of Veterans Affairs). Dr. French’s institution received funding from SCCM. Dr. Maher’s institution received funding from Western Health. The remaining authors have disclosed that they do not have any potential conflicts of interest.
The authors do not necessarily represent the views of the U.S. government or Department of Veterans Affairs.
REFERENCES
- 1.Needham DM, Davidson J, Cohen H, et al. Improving long-term outcomes after discharge from intensive care unit: Report from a stakeholders’ conference. Crit Care Med. 2012; 40:502–509 [DOI] [PubMed] [Google Scholar]
- 2.Mikkelsen ME, Jackson JC, Hopkins RO, et al. Peer support as a novel strategy to mitigate post-intensive care syndrome. AACN Adv Crit Care. 2016; 27:221–229 [DOI] [PubMed] [Google Scholar]
- 3.Ch’ng AM, French D, McLean N. Coping with the challenges of recovery from stroke: Long term perspectives of stroke support group members. J Health Psychol. 2008; 13:1136–1146 [DOI] [PubMed] [Google Scholar]
- 4.Struchen MA, Davis LC, Bogaards JA, et al. Making connections after brain injury: Development and evaluation of a social peer-mentoring program for persons with traumatic brain injury. J Head Trauma Rehabil. 2011; 26:4–19 [DOI] [PubMed] [Google Scholar]
- 5.Hoey LM, Ieropoli SC, White VM, et al. Systematic review of peer-support programs for people with cancer. Patient Educ Couns. 2008; 70:315–337 [DOI] [PubMed] [Google Scholar]
- 6.Haines KJ, Beesley SJ, Hopkins RO, et al. Peer support in critical illness: A systematic review. Crit Care Med. 2018; 46:1522–1531 [DOI] [PubMed] [Google Scholar]
- 7.Carman KL, Dardess P, Maurer M, et al. Patient and family engagement: A framework for understanding the elements and developing interventions and policies. Health Aff (Millwood). 2013; 32:223–231 [DOI] [PubMed] [Google Scholar]
- 8.Burns KEA, Misak C, Herridge M, et al. Patient and Family Partnership Committee of the Canadian Critical Care Trials Group Patient and family engagement in the ICU. Untapped opportunities and underrecognized challenges. Am J Respir Crit Care Med. 2018; 198:310–319 [DOI] [PubMed] [Google Scholar]
- 9.Bate P, Robert G. Experience-based design: From redesigning the system around the patient to co-designing services with the patient. Qual Saf Health Care. 2006; 15:307–310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Robert G, Cornwell J, Locock L, et al. Patients and staff as codesigners of healthcare services. BMJ. 2015; 350:g7714. [DOI] [PubMed] [Google Scholar]
- 11.Dewar B, Mackay R, Smith S, et al. Use of emotional touchpoints as a method of tapping into the experience of receiving compassionate care in a hospital setting. J Res Nurs. 2010; 15:29–41 [Google Scholar]
- 12.Fucile B, Bridge E, Duliban C, et al. Experience-based co-design: A method for patient and family engagement in system-level improvement. Patient Exp J. 2017; 4:53–60 [Google Scholar]
- 13.Maben J, Adams M, Peccei R, et al. ‘Poppets and parcels’: The links between staff experience of work and acutely ill older peoples’ experience of hospital care. Int J Older People Nurs. 2012; 7:83–94 [DOI] [PubMed] [Google Scholar]
- 14.Tsianakas V, Maben J, Wiseman T, et al. Using patients’ experiences to identify priorities for quality improvement in breast cancer care: Patient narratives, surveys or both? BMC Health Serv Res. 2012; 12:271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Palmer VJ, Chondros P, Piper D, et al. The CORE study protocol: A stepped wedge cluster randomised controlled trial to test a co-design technique to optimise psychosocial recovery outcomes for people affected by mental illness in the community mental health setting. BMJ Open. 2015; 5:e006688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Haines KJ, Kelly P, Fitzgerald P, et al. The untapped potential of patient and family engagement in the organization of critical care. Crit Care Med. 2017; 45:899–906 [DOI] [PubMed] [Google Scholar]
- 17.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007; 19:349–357 [DOI] [PubMed] [Google Scholar]
- 18.Polkinghorne D. Language and meaning: Data collection in qualitative research. J Couns Psychol. 2005; 52:137–145 [Google Scholar]
- 19.Hammarberg K, Kirkman M, de Lacey S. Qualitative research methods: When to use them and how to judge them. Hum Reprod. 2016; 31:498–501 [DOI] [PubMed] [Google Scholar]
- 20.Starks H, Trinidad SB. Choose your method: A comparison of phenomenology, discourse analysis, and grounded theory. Qual Health Res. 2007; 17:1372–1380 [DOI] [PubMed] [Google Scholar]
- 21.Maher LBH. Working in partnership with service users. British Journal of Healthcare Management. 2009; 15:172–175 [Google Scholar]
- 22.Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: Guided by information power. Qual Health Res. 2016; 26:1753–1760 [DOI] [PubMed] [Google Scholar]
- 23.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006; 3:77–101 [Google Scholar]
- 24.Hoffmann TC, Glasziou PP, Boutron I, et al. Better reporting of interventions: Template for intervention description and replication (tidier) checklist and guide. BMJ. 2014; 348:g1687. [DOI] [PubMed] [Google Scholar]
- 25.Richards T, Coulter A, Wicks P. Time to deliver patient centred care. BMJ. 2015; 350:h530. [DOI] [PubMed] [Google Scholar]
- 26.Haines KJ, Beesley SJ, Hopkins RO, et al. Peer support in critical care: A systematic review. Crit Care Med. 2018; 46:1522–1531 [DOI] [PubMed] [Google Scholar]
- 27.van Mol MM, Kompanje EJ, Benoit DD, et al. The prevalence of compassion fatigue and burnout among healthcare professionals in intensive care units: A systematic review. Plos One. 2015; 10:e0136955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McPeake J, Hirshberg EL, Christie LM, et al. Models of peer support to remediate post-intensive care syndrome: A report developed by the SCCM International Peer Support Collaborative (THRIVE). Crit Care Med. 2019; 47:e21–e27 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


