Abstract
Objectives:
Compliance to advanced cardiac life support algorithm is low and associated with worse outcomes from in-hospital cardiac arrests. This study aims to improve algorithm compliance by delegation of two separate code team members for timing rhythm check and epinephrine administration in accordance to the advanced cardiac life support algorithm.
Design:
Prospective intervention with historical controls.
Setting:
Single academic medical center.
Patients:
Patients who suffered in-hospital cardiac arrest during study period were considered for inclusion. Patients in which the advanced cardiac life support algorithm or new timekeeper roles were not used were excluded.
Interventions:
Two existing code team members were delegated to time epinephrine and rhythm checks.
Measurements and Main Results:
Primary endpoint was deviations from the 2-minute rhythm check or 3- to 5-minute epinephrine administration. Each deviation outside allotted time intervals was counted as one deviation. However, instances in which multiple intervals passed were counted as multiple deviations. Algorithm adherence was analyzed before and after intervention. Secondary endpoints included return of spontaneous circulation rate, time until first dose of epinephrine, and anonymous survey data. Thirteen pre intervention in-hospital cardiac arrests were compared with 13 in-hospital cardiac arrests post. Prior to intervention, the median deviation per in-hospital cardiac arrest was 5 (interquartile range, 3–7) versus 1 post (interquartile range 0–1; p = 0.0003). The median time until first dose of epinephrine was administered pre intervention was 5 minutes (interquartile range, 0–4) versus post intervention median of 0 (interquartile range, 0–0; p = 0.02). Pre-intervention return of spontaneous circulation rate was 46.1% versus 69.2% post. Surveys demonstrated advanced cardiac life support providers felt time keeping roles made it easier to track epinephrine administration and rhythm checks and improved team communication.
Conclusions:
Two separate timekeeper roles during in-hospital cardiac arrests improved algorithm compliance, code team function, and was favored by code team members. Timekeeper roles may be associated with improved rates of return of spontaneous circulation and less time until the first dose of epinephrine was administered. This study is limited by small sample size and single-center design.
Keywords: advanced cardiac life support, cardiac arrest, sudden, cardiopulmonary resuscitation, epinephrine, guideline, in-hospital cardiac arrest
The prevalence of in-hospital cardiac arrest (IHCA) is well documented with 1 to 5 events occurring per 1,000 hospital admissions (1). Unfortunately, patients who suffer from IHCAs have a low survival to discharge rate of 17% and only 44% of patients achieving return of spontaneous circulation (ROSC) (2). Furthermore, of those patients who survive to discharge only 86% have favorable neurologic outcomes (2).
Despite the widespread use of the American Heart Association’s—Advanced Cardiac Life Support (ACLS), compliance to ACLS algorithms remains low and despite frequent re-training, noncompliance to ACLS guidelines remains high (3, 4). During IHCAs, there are countless tasks and decisions that must be made by members of code teams. Regrettably, there are multiple reasons for noncompliance to the ACLS algorithm such as reduced communication due to chaotic nature of IHCAs, difficulty with tracking time, stress during high acuity situations, lack of knowledge, and more.
A handful of studies have investigated the frequency and effect of deviations from ACLS algorithm (3) and lower rates of protocol deviations may be associated with higher probability of ROSC (5). Interventions such as increased training (6–8) or including a pharmacist in resuscitations (9) have been studied as options to increase algorithm compliance with limited success. However, few studies have developed interventions which have demonstrated meaningful improvement in outcomes.
Our primary aim was to increase compliance to the 2015 update of the ACLS algorithm and improve code team function during IHCAs. We hypothesized that the use of timing devices and delegation of two separate code team members for timing rhythm checks and epinephrine (epinephrine) dosing will increase adherence to ACLS algorithm during IHCAs. To determine the effectiveness of our intervention, we compared the number of algorithm deviations after institution of our intervention with the number of deviations from historical controls.
MATERIALS AND METHODS
Design, Setting, and Population
We performed a pre-post interventional study of IHCA patients at a single academic medical center in Cambridge, MA between the period of September 2018 to June 2019. Formal institutional review board (IRB) approval was obtained for medical record review and the enrollment of ACLS providers for completion of anonymous surveys (IRB number 023-2018). A waiver of informed consent from patients was obtained as this was primarily a quality improvement project and was very low risk. Long-term follow-up and outcome data were not collected due to IRB approval.
All adult patients (> 18 yr old) who suffered from an IHCA at our facility during September 2018 to June 2019 were considered for inclusion. Patients were excluded if the ACLS algorithm was intentionally not used (i.e., patients post cardiac surgery where Cardiac Advanced Life Support was used) or if the new roles and timing devices were not used. Convenience sampling was used to collect the 13 historical control as all IHCAs which occurred the year prior to intervention at our institution were examined.
Intervention
Our intervention consisted of development of two separate time keeping roles, one for timing rhythm checks and the other for timing epinephrine administration in accordance with the ACLS algorithm. We provided educational training to all ACLS providers in our facility prior to the initiation of the study regarding these new roles and devices. We placed two separate stopwatches on all code carts in the hospital for timekeepers to use. However, other timing devices, such as cell phones, could be used. Timekeepers were instructed to use timekeeping devices to time their assigned role and once the correct time interval had passed, he/she was supposed to announce to the code leader it was time to perform a rhythm check or time to administer epinephrine. In order to reduce the possibility of educational bias, there was no additional training provided on ACLS guidelines beyond the standard AHA requirements.
Measurements and Outcome
We analyzed algorithm adherence before and after implementation of timekeeper roles. Each deviation outside the 2-minute rhythm check or 3- to 5-minute epinephrine administration was counted as one deviation. However, deviations in which multiple intervals passed with missed actions were considered more than one deviation. Each patient’s cardiac arrest record was examined to determine if deviations occurred.
Our primary endpoint was the number of deviations from the ACLS algorithm per IHCA, recorded as a continuous variable, which has been highlighted as a potentially relevant maker for performance during resuscitation (3). Secondary outcomes included rates of ROSC, time until first dose of epinephrine, and survey data. We chose to include these outcomes as the time until the first dose of epinephrine is administered for nonshockable rhythms has been associated with increased rates of ROSC (10). Survey data was examined to assess the acceptability of the intervention among ACLS providers. Surveys were delivered to 100% of ACLS providers who had participated in IHCAs post intervention via Survey Monkey. The surveys consisted of yes or no questions including; “Do you feel the use of time keeping devices made it easier to track the epinephrine administration,” “Do you feel the use of time keeping devices made it easier to track pulse check intervals,” and “On a 1-5 Likert scale do you believe the use of the time keeping devices improved team communication (1 strongly disagree – 5 strongly agree).”
Statistical Analysis
Data were summarized using simple descriptive statistics including frequencies with percentages for discrete or count data as well as means with sds, or medians with interquartile ranges (IQRs), as appropriate. For the primary outcome of total deviations, we treated the outcome variable as a continuously distributed variable. We assessed distribution of each variable of interest with visual inspection of histograms. We compared differences in count of deviations in the pre-intervention group to the count in the post-intervention group using a Wilcoxon rank-sum test. Given the observational nature of these data, there was potential for confounding. In order to assess potential confounding, we generated univariable models for potentially relevant confounding variables including age, sex, and initial arrest rhythm. None of these variables were significantly (all p > 0.2) associated with the primary outcome and we therefore did not construct multivariable model for the primary aim.
For the secondary outcomes of time to epinephrine, rate of ROSC, and health provider perceptions of the intervention, we performed simple descriptive statistics to summarize the data. We compared differences in time to epinephrine data using Wilcoxon rank-sum test. All statistical tests of the data were performed using SAS Software (version 9.4; SAS Institute, Cary, NC) and were assumed to be two-sided with an alpha of 0.05.
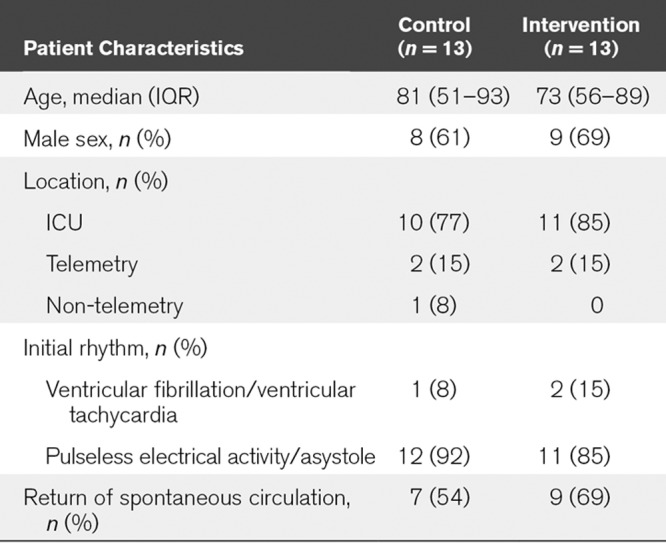
RESULTS
Between August 2018 to June 2019, there were of 13 IHCAs at our facility which were included. Prior to intervention (July 2017 to July 2018), 13 IHCAs were included. One IHCA post intervention was excluded as the patient had undergone cardiothoracic surgery and ACLS was intentionally not used. Additionally, two other IHCAs were excluded as the events were very short, both patients achieved ROSC in under 1 minute, and timekeeper roles were not used. The initial rhythm was pulseless electrical activity/asystole in 92% of the pre-intervention group versus 85% post intervention. The pre intervention group was composed of 61% male sex versus 69% male sex post intervention. In the pre intervention group, 77% of patients were in the ICU during the event versus 85% post intervention. Pre-intervention the average age was 81 ± 13.7 versus 73 ± 9.1 (Table 1).
TABLE 1.
Breakdown of Patient Characteristics of the Sample Pre and Post Intervention; Including Age, Sex, Initial Rhythm at Time of Arrest, and Rate of Return of Spontaneous Circulation
Prior to implementation, there were a total of 82 deviations (36 were epinephrine administration deviations and 46 rhythm check deviations). Post implementation, there were a total of 12 deviations (seven epinephrine administration deviations and five rhythm check deviations). There was a significantly lower rate of protocol deviations following intervention compared with before intervention (median deviation per code 5 IQR 3–7 vs 1 IQR 0–1; p = 0.0003; Fig. 1). With delegation of a code team members to timing epinephrine administration, the average time until the first dose of epinephrine was administered decreased to 0.5 compared with pre intervention average of 2.9 (median time until first dose was 5 min pre-intervention IQR 0–4 vs post intervention median of 0 IQR 0–0; p = 0.02; Fig. 2). Last, we identified an increase in ROSC rate with these changes, pre-implementation the ROSC rate was 46.1% versus 69.2% post intervention.
Figure 1.
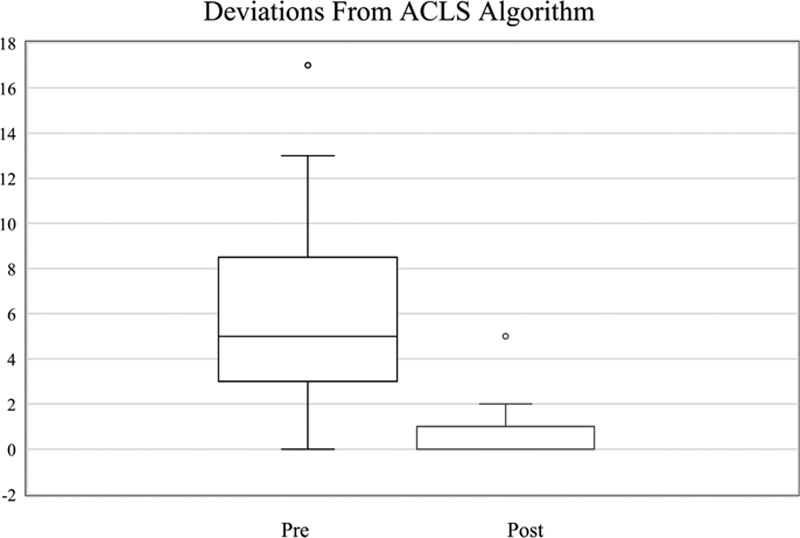
Box plot representing deviations from the advanced cardiac life support (ACLS) algorithm pre and post intervention. n = 13 for both groups, median deviation per code pre intervention was 5 (interquartile range [IQR] 3–7) versus 1 (IQR 0–1; p = 0.0003).
Figure 2.
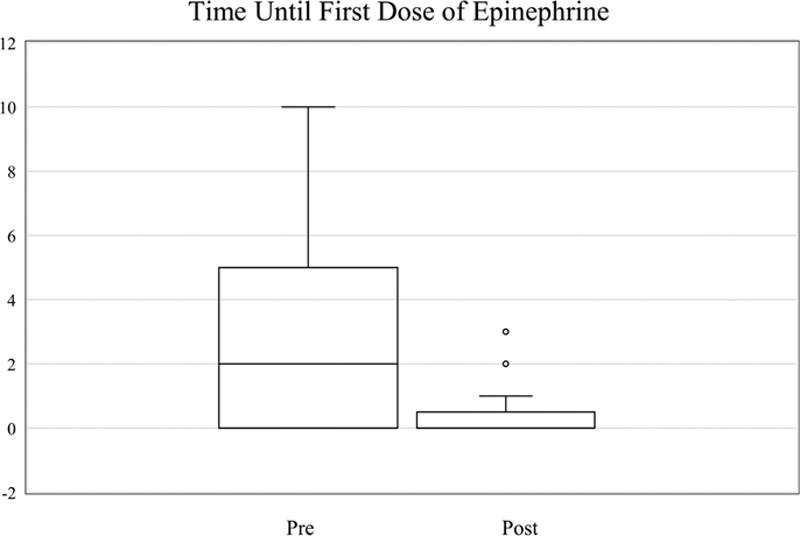
Box plot displaying the time until the first dose of epinephrine was administered pre versus post intervention. n = 13 for both groups, median time until first dose was administered was 5 min pre-intervention (interquartile range [IQR] 0–4) versus post intervention median of 0 (IQR 0–0; p = 0.02).
Surveys were delivered to 100% of the ACLS providers who had participated in the IHCAs post intervention for a total of 103 participants. A total of 81 surveys were completed for a response rate of 79%. Survey data demonstrated that 94% of ACLS providers felt that time keeping devices made it easier to track epinephrine administration and 95% of ACLS providers felt it was easier to track rhythm checks with these changes. Additionally, 63 out of 81 ACLS providers “strongly agree” on Likert scale that the use of timekeeping roles and devices improved code team communication.
DISCUSSION
In this study, to assess the effect of dedicated timekeeper roles on compliance to in-hospital ACLS guidelines, we observed a significant decrease in the rate of protocol deviations, earlier delivery of epinephrine and improved ROSC rates. Additionally, we found that code blue team staff favored the new roles and use of timing devices and believed that the use timekeeping roles and devices increased team communication.
We hypothesized that the delegation of two separate code team members for timing rhythm checks and epinephrine dosing would increase adherence to ACLS algorithm during IHCAs. Our hypothesis was based on previous research from Honarmand et al (3) and McEvoy et al (5) which demonstrated that deviations from the ACLS algorithm are common during IHCAs and that higher amounts of deviations are associated with worse outcomes.
Few studies have investigated interventions aimed at increasing compliance to the ACLS algorithm. The few studies that have been performed investigated interventions such as increased education/training or including a pharmacist during the resuscitation. However, only one study was able to provide an intervention that was able to increase compliance to the ACLS algorithm (9). Research by Donnino et al (10) established that for nonshockable rhythms earlier administration of epinephrine was associated with increased rates of ROSC.
The strengths of our study are clear. We are suggesting a low risk, low cost, simple intervention to improve ACLS algorithm compliance by the addition of two timekeeper roles and timing devices.
This study is limited by its small sample size and single-center design. Future research and validation regarding the use of timekeeping roles is warranted. Investigation into the impact on survival to discharge, ROSC rate, and algorithm deviations in a large multicenter trial would be beneficial.
CONCLUSIONS
The use of two separate timekeeper roles and time keeping devices during IHCAs successfully improved algorithm compliance, code team function and communication, and decreased time until the first dose of epinephrine. Timekeeper roles may be associated with improved rates of ROSC.
ACKNOWLEDGMENTS
The authors wish to extend their gratitude to all the individuals who helped develop and complete this study. They would not have been able to complete this study without the assistance of Dr. Peter Clardy, Becky Logiudice, and Dr. Jess McCannon. Last, the assistance provided by Dr. Justin Salciccioli with the development of this article was imperative to its completion. A sincere thanks to all of you.
Footnotes
The authors have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.Sandroni C, Nolan J, Cavallaro F, et al. In-hospital cardiac arrest: Incidence, prognosis and possible measures to improve survival. Intensive Care Med. 2007; 33:237–245 [DOI] [PubMed] [Google Scholar]
- 2.Peberdy MA, Kaye W, Ornato JP, et al. Cardiopulmonary resuscitation of adults in the hospital: A report of 14720 cardiac arrests from the national registry of cardiopulmonary resuscitation. Resuscitation. 2003; 58:297–308 [DOI] [PubMed] [Google Scholar]
- 3.Honarmand K, Mepham C, Ainsworth C, et al. Adherence to advanced cardiovascular life support (ACLS) guidelines during in-hospital cardiac arrest is associated with improved outcomes. Resuscitation. 2018; 129:76–81 [DOI] [PubMed] [Google Scholar]
- 4.Cline DM, Welch KJ, Cline LS, et al. Physician compliance with advanced cardiac life support guidelines. Ann Emerg Med. 1995; 25:52–57 [DOI] [PubMed] [Google Scholar]
- 5.McEvoy MD, Field LC, Moore HE, et al. The effect of adherence to ACLS protocols on survival of event in the setting of in-hospital cardiac arrest. Resuscitation. 2014; 85:82–87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cheng A, Lockey A, Bhanji F, et al. The use of high-fidelity manikins for advanced life support training–a systematic review and meta-analysis. Resuscitation. 2015; 93:142–149 [DOI] [PubMed] [Google Scholar]
- 7.Moretti MA, Cesar LA, Nusbacher A, et al. Advanced cardiac life support training improves long-term survival from in-hospital cardiac arrest. Resuscitation. 2007; 72:458–465 [DOI] [PubMed] [Google Scholar]
- 8.Sanders AB, Berg RA, Burress M, et al. The efficacy of an ACLS training program for resuscitation from cardiac arrest in a rural community. Ann Emerg Med. 1994; 23:56–59 [DOI] [PubMed] [Google Scholar]
- 9.Draper HM, Eppert JA. Association of pharmacist presence on compliance with advanced cardiac life support guidelines during in-hospital cardiac arrest. Ann Pharmacother. 2008; 42:469–474 [DOI] [PubMed] [Google Scholar]
- 10.Donnino MW, Salciccioli JD, Howell MD, et al. ; American Heart Association’s Get With The Guidelines-Resuscitation Investigators. Time to administration of epinephrine and outcome after in-hospital cardiac arrest with non-shockable rhythms: Retrospective analysis of large in-hospital data registry. BMJ. 2014; 348:g3028. [DOI] [PMC free article] [PubMed] [Google Scholar]


