Abstract
Mesothelioma is an aggressive cancer that has a poor prognosis. Tumors develop in the mesothelial lining of the pleural and peritoneal cavities in response to asbestos exposure. Surgical debulking followed by chemotherapy is initially effective, but this treatment ultimately selects for resistant cells that form aggressive and therapy resistant recurrent tumors. Mesothelioma cancer stem cells (MCS cells) are a highly aggressive subpopulation present in these tumors that are responsible for tumor maintenance and drug resistance. In the present manuscript, we examine the impact of targeting YAP1/TAZ/TEAD signaling in MCS cells. YAP1, TAZ and TEADs are transcriptional mediators of the Hippo signaling cascade that activate gene expression to drive tumor formation. We show that two YAP1 signaling inhibitors, verteporfin and CA3, attenuate the MCS cell phenotype. Verteporfin or CA3 treatment reduces YAP1/TEAD level/activity to suppress MCS cell spheroid formation, matrigel invasion, migration and tumor formation. These agents also increase MCS cell apoptosis. Moreover, constitutively-active YAP1 expression antagonizes inhibitor action, suggesting that loss of YAP1/TAZ/TEAD signaling is required for response to verteporfin and CA3. These agents are active against mesothelioma cells derived from peritoneal (epithelioid) and patient-derived pleural (sarcomatoid) mesothelioma, suggesting that targeting YAP1/TEAD signaling may be a useful treatment strategy.
Implications:
These studies suggest that inhibition of YAP1 signaling may be a viable approach to treating mesothelioma.
Keywords: CA3, YAP, TAZ, TEAD, mesothelioma therapy, verteporfin, tumors, cancer stem cells
Introduction
Mesothelioma is an aggressive/poor-prognosis cancer arising from the mesothelial lining of the pleura, peritoneum and pericardium in response to asbestos exposure [1,2]. The first-line treatment is surgical resection coupled with chemotherapy [3]. This treatment initially works, but the cancer cells eventually become resistant [2] leading to tumor recurrence and poor post-therapy survival [4]. This poor clinical experience speaks to the need for improved therapeutic approaches. Cancer stem cells maintain tumors and mediate drug resistance [5–7]. We have characterized mesothelioma cancer stem cells (MCS cells) [8,9] which comprise 0.15% of tumor cell population [8]. MCS cells are highly aggressive compared to non-stem cancer cells and display vigorous spheroid formation, matrigel invasion and migration. They also form highly aggressive and rapidly growing tumors relative to non-stem cancer cells [8,9].
YAP1/TAZ/TEAD signaling is a centrally important pro-cancer signaling pathway [10] and is often highly activated cancer stem cells [11–13]. YAP1 and TAZ factors interact with nuclear TEAD transcription factors to drive cancer cell survival-related gene expression and tumor growth [14] and are considered important cancer therapy targets [15]. The central importance of this signaling cascade has engendered a search for inhibitors [16,17]. Verteporfin, a photosensitizer that is approved for the treatment of macular degeneration [18], was recently shown to inhibit YAP1/TEAD interaction to reduce YAP1 signaling [16]. In addition, CA3 was identified in a TEAD reporter transcription screen as suppressing YAP1/TEAD-dependent transcription and tumor formation in mice [17]. YAP1/TAZ and TEAD have a role in mesothelioma where they are overexpressed and drive the malignant phenotype [19–21].
In the present study, we examine the impact of suppressing YAP1/TAZ/TEAD signaling on the MCS cell phenotype using cell culture and tumor models. We show that YAP1 function is required to maintain the MCS cell phenotype, and that treatment with CA3 or verteporfin suppresses MCS cell spheroid formation, matrigel invasion and migration. Verteporfin and CA3 also suppress xenograft tumor formation without evidence of adverse side effects. In each case, these agents inhibit YAP1/TAZ signaling and activate apoptosis. Thus, these agents target YAP1 signaling via different mechanisms to reduce the survival of pleural- and parietal-derived mesothelioma cancer cells.
Materials and Methods
Reagents
RPMI 1640 with L-glutamine (10–040-CV) was purchased from Corning (Tewksbury, MA), and 0.25% trypsin-EDTA (T4049) was purchased from Sigma Aldrich (St. Louis, MO). Anti-PARP (556494) was obtained from BD Biosciences (San Jose, CA). Antibodies for Slug (ab27568) and Twist (ab49254) were obtained from Abcam (Cambridge, UK).β-actin (A5441) antibody, heat inactivated fetal calf serum (FCS, F4135) and DAPI (D9542) were purchased from Sigma (St Louis, MO). Antibodies for caspase-3 (9665), caspase-8 (9746), caspase-9 (9502), LATS1-P (9157), LATS1 (9153), YAP1-P (13008), YAP1 (4912), TAZ (4883), TEAD (13295) and Snail (3895) were purchased from Cell Signaling Technologies (Danvers, MA). Anti-TAZ-P (sc-17610) was obtained from Santa Cruz Technologies (Dallas, TX). Peroxidase-conjugated anti mouse IgG (NA931V) and anti-rabbit IgG (NA934V) were obtained from GE Healthcare (Buckinghamshire, UK), and anti-goat IgG (PA1–28664) was obtained from Invitrogen (Carlsbad, CA). These secondary antibodies were used as a 1:5000 dilution. Matrigel (354234) and BD BioCoat Millicell inserts (353097) were purchased from BD Bioscience (Franklin Lakes, NJ). The YAP1 signaling inhibitors, CA3 (CIL56) [17] and verteporfin [16] were purchased, respectively, from SelleckChem (Houston, TX), and Tocris (Bristol, UK). For use in cell culture, the compounds were dissolved in DMSO at a 1000-fold stock. YAP(S127A) (Addgene plasmid # 27370) is a plasmid encoding a constitutively active form of YAP1 donated by Kunliang Guan.
Cell culture and proliferation assay
Meso-1 and NCI-Meso-17 are immortal mesothelioma cell lines generated, respectively, from malignant epithelioid peritoneal and malignant sarcomatoid pleural mesothelioma, were maintained in RPMI 1640 medium supplemented with 10% heat-inactivated FCS [9,22]. Meso-1 cells have been in culture for several years. NCI-Meso-17 cells are short-term passage cells derived from a pleural mesothelioma tumor that has been used for patient-derived xenograft studies [22]. The NCI-Meso-17 cell line was kindly provided by Dr. Raffit Hassan (National Institutes of Health). Monolayer cells were plated at 200,000 cells per 9.6 cm2 plate (#353001, Corning, Tewksbury, MA) in RPMI 1640 medium supplemented with 10% heat-inactivated FCS. After attachment, plates were treated with 0 – 5 μM of verteporfin and cell number was counted in day two and expressed as mean ± SEM. The cells lines are periodically confirmed as authentic using short tandem repeat profiling. Cell lines were also tested for mycoplasma contamination at the time of initiation of the studies, and are generally retested yearly.
Spheroid formation, invasion and migration
For spheroid formation assay, Meso-1 or NCI-Meso-17 cell cultures (near-confluent) were dissociated with trypsin, collected by centrifugation, resuspended in RPMI1640 medium containing 10% FBS. Single cell suspension was plated for spheroid growth at 40,000 cells per 9.5 cm2 ultra-low attachment dishes (#4371, Corning, Tewksbury, MA) and allowed to form spheroids for 0 – 5 d. We count the total number of spheroids and/or average spheroid diameter. We define a spheroid as a clonal collection of cells achieving a diameter greater than or equal to 25 microns. Verteporfin and CA3 impact on spheroid growth/survival was monitored using growing and/or pre-formed spheroids. To monitor impact on nascent spheroid growth, cells were seeded on ultra-low attachment plates, the compound was added the next day and spheroid expansion was monitored thereafter. Alternately, spheroids were permitted to pre-form for 3 – 5 d prior to initiation of drug treatment.
To measure invasion, BioCoat Millicell inserts (d = 1 cm, 8 μM pore size, #353097) were coated with 120 μl of 250 μg/ml Matrigel. Cells (20,000) were seeded atop the matrigel in 500 μl of RPMI1640 containing 1% fetal calf serum. The lower chamber contained the identical medium containing 10% fetal calf serum. When appropriate, pharmacologic agents were added to the bottom chamber. After 18 h the membrane was washed, fixed with 4% paraformaldehyde, and cells on the membraned inner surface were visualized by staining with 4’, 6-diamidino-2-phenylindole (DAPI) for fluorescence detection of nuclei. For migration assay, confluent monolayer cultures were wounded by scraping with a 10 μl pipette tip and the released cells were removed. Migration of cells to close the wound was monitored at 0 – 24 h.
Immunoblot
Cell or tumor samples were lysed in Laemmli buffer (0.063 M Tris-HCl, pH 7.5, 10% glycerol, 5% SDS, 5% β-mercaptoethanol) and equivalent amounts of protein were electrophoresed on denaturing and reducing 10% polyacrylamide gels and transferred to nitrocellulose. The membrane was blocked by 5% non-fat dry milk and then incubated with the appropriate primary (1:1000) and secondary antibodies (1:5000). Secondary antibody binding was visualized using chemiluminescence detection technology.
Electroporation of nucleic acids
Cells (1 million) were collected and electroporated with nucleofection reagent VPD-1002 (Walkersville, MD) [11]. The mixture, containing 3 μg siRNA or plasmid as indicated, was mixed and electroporated using the T-018 setting on the AMAXA Electroporator. Pre-warmed spheroid media was added and the suspension was transferred monolayer culture. At 24 h, the cells were used for spheroid formation, migration and invasion assays. For siRNA experiments, the cells were harvested and electroporated a second time, following the same protocol at 48 h after the initial electroporation [11].
Luciferase assay
Cells were transfected using Fugene 6 with 1 μg of pGL3B-Luc (empty vector) or pGL3B-8xGTIIC-Luc vector and permitted to recover for 24 h before treatment for 24 h with 2 μM verteporfin, an inhibitor of YAP1/TEAD interaction [16] or 1 μM CA3, which inhibits YAP1 signaling [17]. After 24 h the cells were harvested to assay for luciferase activity [23].
Tumor xenograft assay
Three million MCS cells (derived from Meso-1 spheroids) were suspended in 100 μl phosphate buffered saline containing 30% matrigel followed by subcutaneous injection into each front flank of five female NOD scid IL2 receptor gamma chain knockout mice (NSG mice) per treatment group using a 26.5 gauge needle. Verteporfin was prepared in DMSO and the diluted in phosphate buffered saline to prepare an injection solution containing 10% DMSO. CA3 was prepared in DMSO and diluted in phosphate buffered saline to prepare an injection solution containing 0.6% DMSO. Inhibitor treatment was initiated at 8 wks, the time of first tumor detection, by IP injection of 100 μl delivering final concentrations of 0, 50 and 100 mg/kg verteporfin or 1.5 mg/kg CA3 delivered three times per week (M/W/F). Tumor growth was monitored by measuring tumor diameter and calculating tumor volume = 4/3π × (diameter/2)3 [8]. Tumors were harvested at eleven weeks to acquire images and prepare extracts for immunoblot analysis. These studies were approved by the institutional board and followed accepted international practices for the treatment and welfare of animals. Statistics are assessed using the student’s t-test.
Results
Verteporfin suppresses the MCS cell phenotype
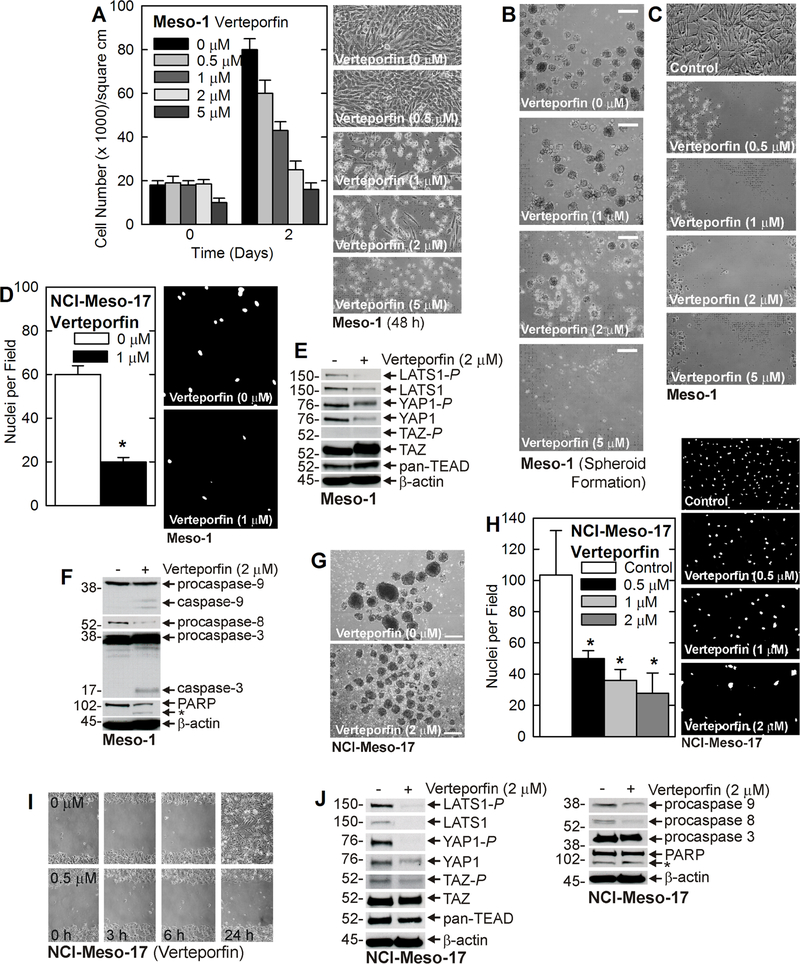
We first monitored the effect of verteporfin on the Meso-1 peritoneal-derived mesothelioma cancer cells [9]. As shown in Fig. 1A, verteporfin causes a dose-dependent reduction in Meso-1 monolayer cell growth that is associated with abnormal cell morphology suggestive of cell death. Mesothelioma cancer stem cells (MCS cells), which comprise 0.15% of the cells in monolayer cultures [8], are enriched in spheroid culture and display vigorous spheroid formation, matrigel invasion and migration (abilty to close a scratch wound) [8]. To assess the impact on the MCS cell phenotype, we examined the impact of verteporfin on spheroid formation, invasion and migration [8]. We grew 5 d pre-formed spheroids on low-attachment plates and then treated with vereporfin for 48 h. Verteporfin treatment promotes spheroid destruction and reduces spheroid number (Fig. 1B). Verteporfin treatment also suppresses MCS cell migration (Fig. 1C) and matrigel invasion (Fig. 1D). Verteporfin has been shown to inhibit YAP1/TEAD signaling [16], and so we assessed the impact of verteporfin treatment on YAP1, TAZ and TEAD signaling in MCS cell spheroids. Fig. 1E shows that verteporfin treatment reduces LATS1, LATS1-P, and YAP1 levels. In contrast, TAZ and pan-TEAD levels are slightly increased. Moreover, verteporfin treatment is associated with enhanced apoptosis as measured loss of procaspase 8, increased levels of active (cleaved) caspase 3 and 9, and PARP (Fig. 1F).
Fig. 1.
Verteporfin suppresses the MCS cell phenotype. A Meso-1 cells were seeded and permitted to attach before addition of drug on day zero and cell number was counted and images collected at 2 d. The values are mean ± SEM and the asterisks indicate a significant change compared to control, n = 3, p < 0.005. B Treatment of 5 d pre-formed spheroids with 0 – 5 μM verteporfin for 48 h causes spheroid destruction (Bars = 100 μm). C/D Verteporfin treatment suppresses matrigel invasion and migration. The values are mean ± SEM and the asterisks indicate a significant change compared to control, n = 3, p < 0.005. E/F Treatment of 5 d spheroids with 0 or 2 μM verteporfin for 72 h suppresses YAP1/TAZ signaling and enhances apoptosis (similar results were observed in two separate experiments). The asterisk indicates cleaved PARP. G NCI-Meso-17 cells were seeded as a single cell suspension on ultral-low attachment plates and after 24 h treated wtih 0 or 2 μM verteporfin (Bars = 100 μm). H/I NCI-Meso-17 cells were permitted to form spheroids and then seeded for matrigel invasion and migration assay with the indicated concentations of verteporfin. Invasion was monitored at 18 h after seeding. J Cells were seed on ultra-low attached plates and after 24 h treated with 0 or 2 μM verteporfin for 72 h before extracts were prepared for immunoblot. The same extract was blotte for both panels and so so the β-actin blot is identifical in each. The asterisk indicates cleaved PARP.
To assure that this effect is generalizable, we monitored the verteporfin impact on NCI-Meso-17 cell spheroid formation, invasion and migration. NCI-Meso-17 cells are low passage patient-derived pleural mesothelioma cells [22]. Cells were seeded on ultra-low attachment plates to assay spheroid formation in the presnce of verteporfin. Verteporfin reduces spheroid size and promotes accumulation of cell debris in the cultures (Fig. 1G). Verteporfin also reduces cell invasion and migration (Fig. 1H/I), and this is associated with reduced LATS1, LATS1-P, YAP1, YAP1-P, and procaspase-8 and −9 (Fig. 1J). Cleaved PARP is present in treated and untreated cells. No cleaved caspase is detected, but loss of pro-caspases without appearance of the cleaved products is not uncommon in apoptosing cells [24]. Thus, verteporfin decreases NCI-Meso-17 MCS cell YAP1 signaling and increases apoptosis.
CA3 suppresses the MCS cell phenotype
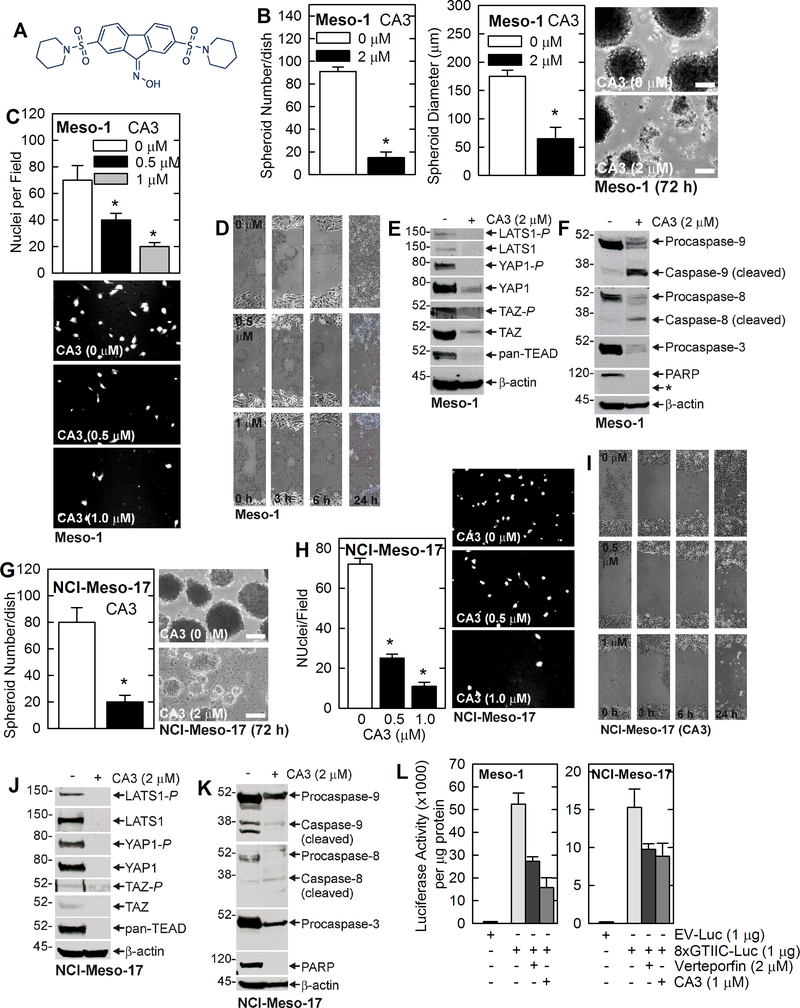
Since verteporfin may produce photosensitivity in patients, we tested another recently identified YAP1 signlaing inhibitor, CA3 (Fig. 2A) [17]. Fig. 2B/C/D show that CA3 treatment reduces the size and number of pre-formed Meso-1 cell spheroids, and suppresses matrigel invasion and migration. Moreover, CA3 reduces LATS1, LATS1-P, YAP1, YAP1-P, TAZ and pan-TEAD signaling (Fig. 2E). In addition, CA3 reduces procaspase-3, −8 and −9, and PARP level, and increases the level of cleaved (active) caspase-8 and −9 and PARP (Fig. 2F). Fig. 2G/H/I show that CA3 treatment of NCI-Meso-17 cells causes destruction of pre-formed spheroids, and suppresses matrigel invasion and migration. Moreover, these changes are associated with reduced YAP1/TAZ signaling and increased apoptosis (Fig. 2J/K). We also examined the impact of inhibitor treatment on YAP1-dependent transcription. Cells were transfected with empty vector luciferase (EV-Luc) or 8xTGIIC-Luc, which encodes repeats of the TEAD response element [25,26]. Fig. 2L shows that CA3 and verteporfin treatment reduce YAP1/TEAD response element dependent transcription in Meso-1 and NCI-Meso-17 cells. The reduction in transcription activity following inhibitor teatment is consistent with the treatment-dependent reduction in YAP1 level (Fig. 1E and Fig. 2E/J).
Fig. 2.
CA3 suppresses the MCS cell phenotype. A Structure of CA3 [17]. B/C/D Meso-1 cells were permitted to form spheroids for 3 d and then treated for 72 h with 0 or 2 μM CA3 before determining count and collecting images (Bars = 100 μm). Mean ± SEM and the asterisks indicate a significant change compared to control, n = 3, p < 0.005. CA3 treatment also suppresses matrigel invasion (18 h) and migration. E/F Pre-formed spheroids were treated for 72 h with CA3 and extracts were prepared to detect the indicated epitopes. The asterisk points to the barely visible cleaved PARP band present in the CA3 treated sample. G/H/I Meso-1 cells were permitted to form spheroids for 3 d and then treated for 72 h with 0 or 2 μM CA3 before determining count and collecting images (Bars = 100 μm). CA3 also suppresses martrigel invasion (18 h) and migration. J/K Pre-formed spheroids were treated for 72 h with CA3 and extracts were prepared to detect the indicated epitopes. Blots were repeated in two independent experiments. L Cells were transfected with the indicated luciferase reporter plasmids and then treated for 24 h with inhibitor before extracts were prepared for luciferase activity assay. Values are mean ± SD.
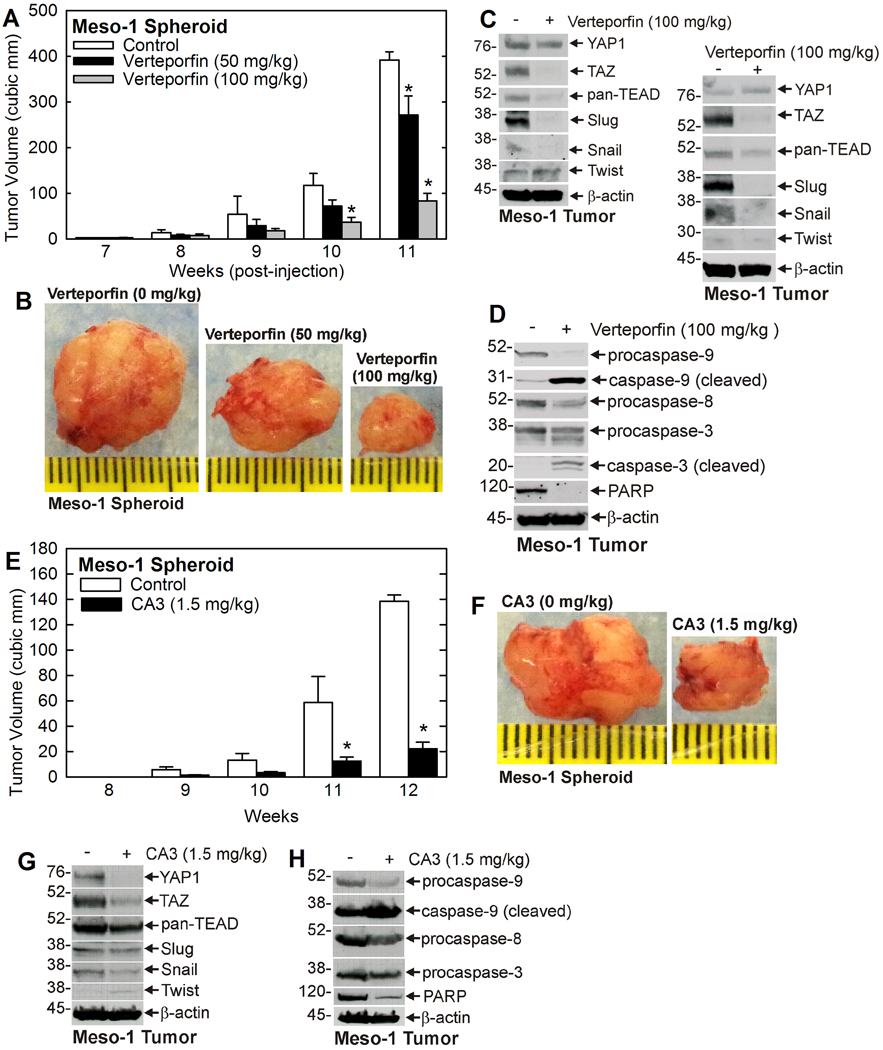
Verteporfin and CA3 inhibit tumor formation
To confirm that the regulation we observe in cells is observed in tumors, we examined the impact of verteporfin and CA3 treatment on MCS cell tumor formation, and YAP1/TAZ signaling. Meso-1 spheroid-derived MCS cells were injected into NSG mice and tumor formation was monitored. When tumors were first palpated at 7 – 9 wks, inhibitor treatment was initated. Fig. 3A/B shows that verteporfin produces a dose-dependent reduction in tumor formation. Fig. 3C shows immunoblot proflies from two separate tumors which indicate that YAP1/TAZ signaling is suppressed in verteporfin-treated tumors. These findings show that verteporfin suppresses TAZ and pan-TEAD level, but not YAP1 level. We also observe a reduction in Slug and Snail, which are regulators that drive epithelial to mesenchymal transition (EMT), suggesting that verteporfin treatment suppresses EMT. Another EMT factor, Twist, was not regulated. Fig. 3D shows verteporfin activates tumor cell apoptosis, as evidenced by reduced procaspase-3, −8 and −9, and PARP, and increased cleaved/active caspase-3 and −9 levels. CA3 also reduces tumor formation (Fig. 3E/F). Moreover, as with verteporfin, there is a substantial reduction in YAP1, TAZ, pan-TEAD. Slug and Snail (EMT markers) levels are also reduced (Fig. 3G). Apoptosis is increased, as evidenced by loss of procaspase 9 and accmulation of cleaved caspase 9, and reduced procaspase 8 and PARP (Fig. 3H).
Fig. 3.
Verteporfin and CA3 suppress tumor formation. A/B Spheriod-derived Meso-1 cells (3 million) were were injected subcutaneously in NSG mice and verteporfin treatment was initiated at the time of first tumor appearance. Tumor volumes are mean ± SEM (n = 10) and the asterisks indicate a significant reduction in tumor size compared to control (p < 0.005). The images are of 11 wk tumors. C/D Extracts were prepared from two independent (11 wk) tumors for immunoblot detection of YAP1/TAZ signaling proteins and from one tumor for detection of apoptotic markers. E/F Spheroid-derived Meso-1 cells (3 million) were injected subcutaneously in NSG mice and CA3 treatment was initiated at the time of tumor appearance. Tumor volumes are mean ± SEM (n = 10) and the asterisks indicate a significant reduction in tumor size compared to control (p < 0.005). The images are of 12 wk tumors. G/H Extracts were prepared from 12 wk tumors for immunoblot detection of YAP1/TAZ signaling proteins and apoptotic markers.
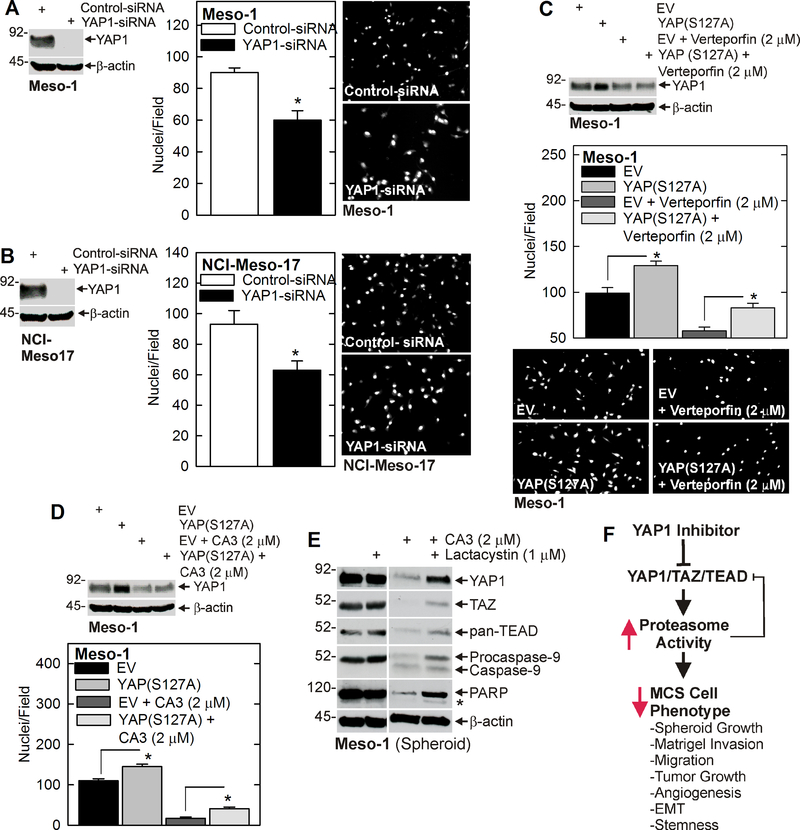
YAP1 is required to maintain the MCS cell phenotype and can antagonize verteporfin and CA3 action
If YAP1 has a key role in maintaining mesothelioma cancer cell function, YAP1 knockdown should reduce MCS cell survival and overexpression of constitutively active YAP1, YAP(S127A), should antagonize verteporfin and CA3 action. To assess these concepts, we treated Meso-1 and NCI-Meso-17 cells with control- or YAP1-siRNA and monitored the impact on matrigel invasion. Fig. 4A/B show that YAP1 knockdown reduces Meso-1 and NCI-Meso-17 cell matrigel invasion. Moreover, Fig. 4C shows that forced expression of YAP(S127A) enhances Meso-1 MCS cell matrigel invasion and partially reverses the suppression of migration observed in verteporfin-treated cells. Forced YAP(S127A) expresion also antagonized CA3 suppression of matrigel invasion (Fig. 4D). Note that YAP1 levels in verteporfin and CA3 treated cells is only marginally elevated (Fig. 4C/D), but this is not suprising since inhibitor treatment suppresses YAP1 level. The above findings are consistent with recent reports suggesting that YAP1/TAZ/TEAD signaling is required mesothelioma cancer cell survival [21,27,28].
Fig. 4.
Role of YAP1 in maintaining the MCS cell phenotype. A/B Meso-1 or NCI-Meso-17 cells were treated with control- or YAP1-siRNA and then plated for invasion assay. C/D Meso-1 cells were electroporated with 3 μg of empty vector (EV) or YAP(S127A) expression vector, plated for a 24 h invasion assay during treatment with 0 or 2 μM verteporin or CA3. After 24 h, extracts prepared to monitor YAP1 level. The values are mean ± SEM, and that asterisks indicate a significant increase (p < 0.005) compared to the EV group. E Meso-1 spheroids were grown for 3 d on ultra-low attachment plates and then treatment was initiated with with lactacystin followed 1 h later by CA3. At 72 h the cells were harvestsed and assayed for the indicated proteins. The asterisk indicates cleaved PARP. Similar results were observed in two experiments. F Mechanism of YAP1 inhibitor action in mesothelioma. YAP1, TAZ and TEAD levels are elevated in MCS cells and act to maintain the MCS cell phenotype characterized by enhanced spheroid formation, matrigel invasion, migration, tumor formation, angiogenesis, epithelial mesenchymal transition (EMT) and stemness. The YAP1/TEAD inhibitors (verteporfin, CA3) reduce YAP1/TAZ/TEAD signaling leading to apoptosis which results in a further reduction of YAP1/TAZ/TEAD level. These events attentuate the MCS cell phenotype.
We next studied the relationsihip between YAP1, TAZ and pan-TEAD level and proteasome activity. Pre-formed spheroids were treated with CA3 in the presence or absence of lactacystin, a proteasome inhibitor. Fig. 4E shows CA3 reduces YAP1, TAZ, pan-TEAD, procaspase-9 and PARP levels, and that co-treatment wih lactacystin reverses these changes suggesting that proteosome degradation reduces YAP1, TAZ and pan-TEAD signaling.
Discussion
Mesothelioma is an aggressive and unforgiving asbestos and nanotube-induced cancer [1,2]. Current treatment is surgical resection with chemotherapy, but this is only marginally successful [3]. This fact has led to the search for new therapeutic options. The Hippo signaling cascade is a centrally important cancer cell survival cascade [10]. Mst1/2 kinase phosphorylates LATS1/2 kinase which phosphorylates/inactivates YAP1 and TAZ [10]. This cascade controls many cellular processes, including organ development [10,29]. In growing cells Mst1/2 and LATS1/2 kinases are silent which permits unphosphorylated YAP1 and TAZ transcription adaptor proteins to accumulate in the nucleus where they bind to TEAD transcription factors and activate expression of pro-proliferation genes [10]. In contrast, in senescent cells, Mst1/2 and LATS1/2 kinases are active, and phosphorylate YAP1 and TAZ which are then released to the cytoplasm where they are degraded by the proteasome - thereby relieving the growth stimulus [10]. This cascade is extremely important in cancer where LATS1/2 signaling is reduced leading to enhance accumulation of active YAP1 in the nucleus. For example, highly aggressive hepatocellular carcinoma developes in mice in response to constitutive YAP1/TAZ activity [30]. YAP1/TAZ/TEAD are also important in human cancers [10,31] including mesothelioma where they drive the malignant phenotype [19–21]. We confirm that YAP1 maintains the MCS cell phenotype, such that loss of YAP1 reduces MCS cell spheroid formation, matrigel invasion and migration. Moreover, expression of constitutively active YAP1 angatonizes veteporfin and CA3 suppression of matrigel invasion, suggesting that loss of YAP1 is a requirement for action of these agents.
YAP1/TEAD signaling as a therapy target
Because of the pro-cancer activity of this pathway [19–21] YAP1/TAZ signaling is an important cancer therapy target. Verteporfin is a photosensitizer that is used to treat excess vascularization in eye disease [32,33], but has been shown to inhibit YAP1/TEAD interaction to reduce YAP1 signaling [12,16,34–36]. In the present study we show that verteporfin suppresses cell proliferation, spheroid formation, matrigel invasion and migration of MCS cells derived from Meso-1 (peritoneal mesothelioma) and NCI-Meso-17 (pleural mesothelioma) cells. A common theme is suppression of LATS1, LATS1-P, YAP1, YAP1, TAZ and pan-TEAD levels. It is interesting that verteporfin, which inhibits YAP1/TEAD interaction [16], reduces the level of both LATS1 and LATS1-P. This is surprising as LATS1/LATS1-P are upstream of YAP1 in the signaling cascade [16]. We are not certain why inhibition of YAP1/TEAD function reduces LATS1/LATS1-P; however, LATS1/LATS1-P loss is not likely to be important because verteporfin treatment reduces the level of the penultimate regulators, YAP1, TAZ and TEAD.
Photosensitizers, like verteporfin, have been used to treat mesothelioma [37,38]. In this procedure, the tumor is surgically removed and the body cavity is bathed in photosensitizer which is then activated by laser irradiation [39–42]. The goal is use of the photosensitizer to kill residual tumor cells that could not be removed by surgery. The drawback is that these photoactive agents cause photosensitivity in light-exposed patients. This feature makes it difficult to use such agents as therapeutics. Thus, other YAP1-targeting agents must be considered. CA3 was identified as reducing YAP1 level and YAP1/TEAD-dependent transcription as measured by suppression of TEAD-dependent transcription [17]. The mechanism whereby CA3 inhibits YAP1 function is not clear, and may include interfering with signaling events upstream of YAP1/TEAD. Our findings show that CA3 suppresses YAP1/TAZ/TEAD signaling by reducing LATS1, LATS1-P, YAP1, YAP1-P, TAZ, TAZ-P and pan-TEAD levels,
The fact that forced expression of constitutively-active YAP1 reverses CA3 (and verteporfin) suppression of the MCS cell phenotype suggests that YAP1/TAZ/TEAD signaling is a biologically important target of these agents. In addition, treatment of cells with lactacystin, a proteasome inhibitor, partially reverses YAP1 inhibitor-associated loss of YAP1, TAZ and pan-TEAD, suggesting that loss of these proteins is via apoptotic degradation.
Inhibitor suppression of tumor formation
To have clinical importance, any candidate therapeutic agent must suppress in vivo tumor formation. We show that verteporfin and CA3 suppress tumor formation (Fig. 3). Verteporfin treatment is associated with reduced YAP1/TAZ/TEAD signaling as evidence by reduced TAZ and pan-TEAD levels in verteporfin treated tumors. However, in contrast to the studies in cultured cells, YAP1 level is not altered. In addition, we observe enhanced tumor cell apoptosis as shown by reduced procaspase-3, −8 and −9, and PARP, and increased active caspase-3 and −9. CA3 also suppresses tumor formation and this is associated with reduced YAP1, TAZ and pan-TEAD levels. Apoptosis is increased as indicated by loss of procaspase 9 and 8 and PARP and enhance levels of active caspase 3.
These findings are consistent with the observations in cultured cells in that verteporfin suppresses YAP1/TAZ/TEAD signaling and enhances apoptosis. The subtle differences in YAP1/TAZ/TEAD signaling protein modulation in cultured cells versus tumors is likely due to differences in cellular environment. Verteporfin and CA3 also reduce Slug and Snail, which are positive regulators of EMT, suggesting that verteporfin suppresses tumor cell EMT.
Suppression of the MCS cell phenotype by verteporfin and CA3
We have shown that MCS cells comprise 0.15% of the mesothelioma cell population and that these cells can be enriched by growth as unattached spheroids [8]. MCS cells display a highly aggressive phenotype including enhanced spheroid growth, matrigel invasion, migration and tumor formation [8]. Our present studies show that verteporfin and CA3 suppress the MCS cell phenotype. Moreover, verteporfin and CA3 suppression of the MCS cell phenotype requires reduced YAP1/TAZ/TEAD signaling, as demonstrated by the fact that overexpression of constitutively active YAP1 antagonizes the action of these agents. It is encouraging that the highly aggressive MCS cell subpopulation is responsive to these agents. Based on these studies, we suggest that verteporfin and CA3 suppresses YAP1/TAZ/TEAD signaling leading to induction of apoptosis which further compromises YAP1/TAZ/TEAD signaling to suppress the highly aggressive MCS cell phenotype (Fig. 4F). These findings suggest that use of YAP1/TEAD targeting agents may be useful in the treatment of mesothelioma. Additional experiments should study combination therapy of chemotherapeutic agents and YAP1/TEAD inhibitors.
Acknowledgements:
This work was supported by the NIH (CA211909 and CA184027) to R.L. Eckert.
Footnotes
Conflict of Interest: The authors declare no conflict of interest
Reference List
- 1.Cao S, Jin S, Cao J et al. Advances in malignant peritoneal mesothelioma. Int J Colorectal Dis 2015; 30:1–10. [DOI] [PubMed] [Google Scholar]
- 2.Hassan R, Alexander R, Antman K et al. Current treatment options and biology of peritoneal mesothelioma: meeting summary of the first NIH peritoneal mesothelioma conference. Ann Oncol 2006; 17:1615–1619. [DOI] [PubMed] [Google Scholar]
- 3.Hubert J, Thiboutot E, Dube P et al. Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy with oxaliplatin for peritoneal mesothelioma: preliminary results and survival analysis. Surg Oncol 2015; 24:41–46. [DOI] [PubMed] [Google Scholar]
- 4.Vogelzang NJ, Rusthoven JJ, Symanowski J et al. Phase III study of pemetrexed in combination with cisplatin versus cisplatin alone in patients with malignant pleural mesothelioma. J Clin Oncol 2003; 21:2636–2644. [DOI] [PubMed] [Google Scholar]
- 5.Al-Hajj M, Becker MW, Wicha M, Weissman I, Clarke MF. Therapeutic implications of cancer stem cells. Curr Opin Genet Dev 2004; 14:43–47. [DOI] [PubMed] [Google Scholar]
- 6.Alison MR, Lin WR, Lim SM, Nicholson LJ. Cancer stem cells: In the line of fire. Cancer Treat Rev 2012. [DOI] [PubMed] [Google Scholar]
- 7.Baik I, Becker PS, DeVito WJ et al. Stem cells and prenatal origin of breast cancer. Cancer Causes Control 2004; 15:517–530. [DOI] [PubMed] [Google Scholar]
- 8.Adhikary G, Grun D, Alexander HR et al. Transglutaminase is a mesothelioma cancer stem cell survival protein that is required for tumor formation. Oncotarget 2018; 9:34495–34505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Varghese S, Whipple R, Martin SS, Alexander HR. Multipotent cancer stem cells derived from human malignant peritoneal mesothelioma promote tumorigenesis. PLoS One 2012; 7:e52825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harvey KF, Zhang X, Thomas DM. The Hippo pathway and human cancer. Nat Rev Cancer 2013; 13:246–257. [DOI] [PubMed] [Google Scholar]
- 11.Fisher ML, Ciavattone N, Grun D, Adhikary G, Eckert RL. Sulforaphane reduces YAP/Np63alpha signaling to reduce cancer stem cell survival and tumor formation. Oncotarget 2017; 8:73407–73418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fisher ML, Grun D, Adhikary G, Xu W, Eckert RL. Inhibition of YAP function overcomes BRAF inhibitor resistance in melanoma cancer stem cells. Oncotarget 2017; 8:110257–110272. [DOI] [PMC free article] [PubMed] [Google Scholar] [Research Misconduct Found]
- 13.Song S, Ajani JA, Honjo S et al. Hippo coactivator YAP1 upregulates SOX9 and endows esophageal cancer cells with stem-like properties. Cancer Res 2014; 74:4170–4182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Felley-Bosco E, Stahel R. Hippo/YAP pathway for targeted therapy. Transl Lung Cancer Res 2014; 3:75–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zanconato F, Battilana G, Cordenonsi M, Piccolo S. YAP/TAZ as therapeutic targets in cancer. Curr Opin Pharmacol 2016; 29:26–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu-Chittenden Y, Huang B, Shim JS et al. Genetic and pharmacological disruption of the TEAD-YAP complex suppresses the oncogenic activity of YAP. Genes Dev 2012; 26:1300–1305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Song S, Xie M, Scott AW et al. A Novel YAP1 Inhibitor Targets CSC-Enriched Radiation-Resistant Cells and Exerts Strong Antitumor Activity in Esophageal Adenocarcinoma. Mol Cancer Ther 2018; 17:443–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Newman DK. Photodynamic therapy: current role in the treatment of chorioretinal conditions. Eye (Lond) 2016; 30:202–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sekido Y Molecular pathogenesis of malignant mesothelioma. Carcinogenesis 2013; 34:1413–1419. [DOI] [PubMed] [Google Scholar]
- 20.Matsushita A, Sato T, Mukai S et al. TAZ activation by Hippo pathway dysregulation induces cytokine gene expression and promotes mesothelial cell transformation. Oncogene 2018. [DOI] [PubMed] [Google Scholar]
- 21.Zhang WQ, Dai YY, Hsu PC et al. Targeting YAP in malignant pleural mesothelioma. J Cell Mol Med 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kalra N, Zhang J, Thomas A et al. Mesothelioma patient derived tumor xenografts with defined BAP1 mutations that mimic the molecular characteristics of human malignant mesothelioma. BMC Cancer 2015; 15:376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chew YC, Adhikary G, Wilson GM, Xu W, Eckert RL. Sulforaphane induction of p21(Cip1) cyclin-dependent kinase inhibitor expression requires p53 and Sp1 transcription factors and is p53-dependent. J Biol Chem 2012; 287:16168–16178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fisher ML, Adhikary G, Grun D, Kaetzel DM, Eckert RL. The Ezh2 polycomb group protein drives an aggressive phenotype in melanoma cancer stem cells and is a target of diet derived sulforaphane. Mol Carcinog 2015; 55:2024–2036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dupont S, Morsut L, Aragona M et al. Role of YAP/TAZ in mechanotransduction. Nature 2011; 474:179–183. [DOI] [PubMed] [Google Scholar]
- 26.Mohamed A, Sun C, De MV, et al. The Hippo effector TAZ (WWTR1) transforms myoblasts and TAZ abundance is associated with reduced survival in embryonal rhabdomyosarcoma. J Pathol 2016; 240:3–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hsu PC, Miao J, Wang YC et al. Inhibition of yes-associated protein down-regulates PD-L1 (CD274) expression in human malignant pleural mesothelioma. J Cell Mol Med 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tranchant R, Quetel L, Tallet A et al. Co-occurring Mutations of Tumor Suppressor Genes, LATS2 and NF2, in Malignant Pleural Mesothelioma. Clin Cancer Res 2017; 23:3191–3202. [DOI] [PubMed] [Google Scholar]
- 29.Kodaka M, Hata Y. The mammalian Hippo pathway: regulation and function of YAP1 and TAZ. Cell Mol Life Sci 2015; 72:285–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Halder G, Johnson RL. Hippo signaling: growth control and beyond. Development 2011; 138:9–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Johnson R, Halder G. The two faces of Hippo: targeting the Hippo pathway for regenerative medicine and cancer treatment. Nat Rev Drug Discov 2014; 13:63–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Michels S, Schmidt-Erfurth U. Photodynamic therapy with verteporfin: a new treatment in ophthalmology. Semin Ophthalmol 2001; 16:201–206. [DOI] [PubMed] [Google Scholar]
- 33.Tatar O, Adam A, Shinoda K et al. Influence of verteporfin photodynamic therapy on inflammation in human choroidal neovascular membranes secondary to age-related macular degeneration. Retina 2007; 27:713–723. [DOI] [PubMed] [Google Scholar]
- 34.Wang C, Zhu X, Feng W et al. Verteporfin inhibits YAP function through up-regulating 14–3-3sigma sequestering YAP in the cytoplasm. Am J Cancer Res 2016; 6:27–37. [PMC free article] [PubMed] [Google Scholar]
- 35.Wei H, Wang F, Wang Y et al. Verteporfin suppresses cell survival, angiogenesis and vasculogenic mimicry of pancreatic ductal adenocarcinoma via disrupting the YAP-TEAD complex. Cancer Sci 2017; 108:478–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ma YW, Liu YZ, Pan JX. Verteporfin induces apoptosis and eliminates cancer stem-like cells in uveal melanoma in the absence of light activation. Am J Cancer Res 2016; 6:2816–2830. [PMC free article] [PubMed] [Google Scholar]
- 37.Finlay JC, Zhu TC, Dimofte A, Friedberg JS, Hahn SM. Diffuse reflectance spectra measured in vivo in human tissues during Photofrin-mediated pleural photodynamic therapy. Proc SPIE Int Soc Opt Eng 2006; 6139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Maehara S, Usuda J, Ishizumi T et al. Combination effect of photodynamic therapy using NPe6 with pemetrexed for human malignant pleural mesothelioma cells. Int J Oncol 2015; 46:741–749. [DOI] [PubMed] [Google Scholar]
- 39.Simone CB, Cengel KA. Photodynamic therapy for lung cancer and malignant pleural mesothelioma. Semin Oncol 2014; 41:820–830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wang Y, Perentes JY, Schafer SC et al. Photodynamic drug delivery enhancement in tumours does not depend on leukocyte-endothelial interaction in a human mesothelioma xenograft model. Eur J Cardiothorac Surg 2012; 42:348–354. [DOI] [PubMed] [Google Scholar]
- 41.Friedberg JS, Mick R, Culligan M et al. Photodynamic therapy and the evolution of a lung-sparing surgical treatment for mesothelioma. Ann Thorac Surg 2011; 91:1738–1745. [DOI] [PubMed] [Google Scholar]
- 42.Friedberg JS. Photodynamic therapy for malignant pleural mesothelioma: the future of treatment? Expert Rev Respir Med 2011; 5:49–63. [DOI] [PubMed] [Google Scholar]