Abstract
Background
While physical frailty and malnutrition/obesity (parameters easily measured by a nurse) are not the same, older persons who are malnourished/obese are more likely to be frail and there is a potential overlap between these conditions. The objective was to examine the relationship between gait speed (GS) and body mass index (BMI) in men and women aged 75 years and older.
Design
Cross-sectional analysis.
Setting, participants
Data from the Aging Multidisciplinary Investigation (AMI), a French prospective cohort study with participants randomly selected from the farmer Health Insurance rolls.
Measurements
Usual GS was measured over a 4 meters-track. BMI was categorized using clinical cut-points for European populations: (e.g, <20.0 kg/m2; 20.0–24.9 kg/m2; 25.0–29.9 kg/m2; 30.0–34.9 kg/m2; ≥35.0 kg/m2).
Results
The current analyses were performed in 449 participants. Mean age was 81 years. Being malnourished/obese was significantly associated with slow GS. Unadjusted and age-adjusted models showed that underweight, overweight and obesity statuses were significantly associated with slow GS for both women (0.83m/s [0.61; 1.04], 0.87m/s [0.72; 1.02], 0.70 m/s [0.41; 0.98], respectively) and men (0.83m/s [0.61; 1.04], 1.11m/s [1.03; 1.20], 0.97m/s [0.75; 1.19], respectively).
Conclusion
Malnourished/obese are associated with slow GS in older persons. These variables could be contributed at comprehensively and complementarily assessing the older person.
Introduction
Slowness is one of the fundamental characteristics of aging[1] and one of the main components of the decline in physical function. Loss of physical function represents a major public health issue, especially considering the growing number of older persons in Western countries[2,3]. Gait speed (GS) is among the most commonly used instruments for measuring physical performance in population studies of aging[4]. GS is increasingly indicated as an important parameter to measure in the clinical and research evaluation of older persons[2]. It is associated with clinical comorbidity[4] (such as multiple brain lacunae) and subclinical (eg, inflammation[5], oxidative damage[6]) conditions, and predictive of major health-related outcomes (eg, disability, hospitalization, mortality)[7].
The 3C-Dijon and 3C-Bordeaux studies[8] have already shown that GS is specifically associated with the risk of incident dementia[1]. GS is also included in the most common operational definitions of frailty as one of the key criteria to measure[9]. Obesity represents a major priority for healthcare systems as well, due its social, clinical, and economic burdens[10]. In fact, it has shown to significantly predict negative outcome (including disability and mortality). Obesity is an incresingly prevalent disease at all ages, including among older persons[11–14]. Both GS and BMI could be considered as general markers of wellbeing. Although previous studies have demonstrated a U-shaped relationship between body mass index (BMI) and frailty phenotypes[15,16], few others studies have explored the relationship between BMI and GS[17–19] but no study has yet explored this relationship in 75 years and older in rural area. This latter may represent a clinical friendly parameter to adopt in the identification of the "biologically aged" (or frail) individuals.
In the present study, we hypothesize that GS and BMI are associated following a U-shaped relationship (ie, individuals with slow GS are malnourished or obese). While physical frailty and malnutrition/obese (consider as easy-to-access parameter collected by a nurse) are not the same, older person who are malnourished/obese are more likely to be frail and there is a potential overlap between these conditions. The objective of this study was to test whether BMI and 4-meters GS are associated or not among community-dwelling older adults aged 75 years and older. To achieve these goals, we used the Aging Multidisciplinary Investigation (AMI) cohort study data, a French longitudinal population-based cohort.
Methods
The data used in this study were collected as part of the Agrica-MSA-IFR de Santé Publique, Aging Multidisciplinary Investigation (AMI) study, a French prospective cohort study on health and aging including older farmers living in rural areas. The AMI cohort started in 2007 and included 1,002 older farmers retired from agriculture, living in rural areas. Participants aged 65 years and older were randomly recruited from the Farmer Health Insurance System (Mutualité Sociale Agricole [MSA]). At baseline, trained nurses and psychologists collected information including socio-demographics, self-reported chronic diseases, depressive symptoms, and functional status during face-to-face interviews at the participants’ home. In addition, participants underwent a comprehensive cognitive evaluation. A detailed description of the methodology used for the AMI study can be found in a previous publication[20].
The Ethical Committee of the University Hospital of Bordeaux (Bordeaux, France) approved the AMI study according to the principles embodied on the Declaration of Helsinki and all participants provided written informed consent.
Body mass index
Standardized measures of weight and size were recorded and used to calculate BMI. BMI was operationalized as the ratio between [weight in kg/height (in m)2]. Participants were considered as malnourish and obese if presenting a BMI <21 kg/m2 and BMI >30 kg/m2, respectively. Indeed, BMI< 21kg/m2 is mainly used for the identification of people at risk of malnutrition in the Mini Nutritional Assessment (a validated tool to assess malnutrition and risk for malnutrition among elderly participants of epidemiological studies)[21,22].
Gait speed
Participants were then asked to walk a distance of 4 meter at their usual pace starting from a still position. GS was operationalized as the ratio between distance and time, and expressed in meters by seconds (m/s).
Other variables
Disability for the basic activities of the daily living (ADL) and instrumental ADL (IADL) was assessed using the Katz index[23] and Lawton & Brody scales[24], respectively. Cognitive status was measured using the Mini Mental State Examination (MMSE)[25] 17 and depressive symptom by the CES-D[26] 18.
Exclusion criterion
We are interested only about a sample of 75 years and older because as people aged 65 to 74 years have no alteration of gait speed in a complementary analyze.
Statistical analysis
The sample characteristics are presented as the means and standard deviations (+/−SD) for continuous variables and as frequencies and percentages for categorical variables. Given the well-established gender differences for body composition and physical performance, all the present analyses were separately conducted for men and women. BMI was categorized using the well-established clinical cut-points for European populations: <20.0 kg/m2; 20.0–24.9 kg/m2; 25.0–29.9 kg/m2; 30.0–34.9 kg/m2; ≥35.0 kg/m2. Unadjusted and adjusted analyses of covariance were performed to estimate the gender-specific means (and 95% confidence intervals) of GS (in m/s) according to BMI categories. After having provided results from the unadjusted analyses, age-adjusted models were performed. Pearson correlation coefficients were used to examine the associations between BMI and GS. P-values < 0.05 were considered statistically significant and 95% confidence intervals (95% CI) are provided. All analyses were performed using SAS, version 9.4 (SAS Institute, Inc., Cary, NC).
Results
Among the 1,002 participants enrolled in the AMI study, 538 were aged 75 years or older at baseline. We are interested only about a sample of 75 years and older because as people aged 65 to 74 years have no alteration of gait speed in a complementary analyze. The current analyses were performed in 449 (83.5%) participants, after exclusion of 89 (16.5%) individuals with missing data for the main variables of interest (GS or/and BMI).
Table 1 shows that, compared to participants considered in the present analyses, the excluded 89 were older (83.1±5.4 versus 81.0±4.4), had a lower MMSE (20.5±7.9 versus 24.4±4.0) and higher disability in ADLs and IADLs. There were no significant differences for BMI and gait speed between the two groups.
Table 1. Main characteristics of the study sample according to participation or missing values.
| Participants N = 449 | Non participants N = 89 | P* | |
|---|---|---|---|
| Age (years) | 81.0 (4.4) | 83.1 (5.4) | 0.0008 |
| Sex (men) | 290 (64.6) | 51 (57.3) | 0.19 |
| Height (m) | 1.65 (0.08) | N = 32 1.64 (0.09) | 0.54 |
| Weight (kg) | 74.6 (14.5) | N = 34 71.4 (14.7) | 0.21 |
| Body Mass Index (kg/m2) | 27.4 (4.3) | N = 30 26.8 (5.0) | 0.45 |
| Mini Mental State Examination | N = 440 24.4 (4.0) | N = 88 20.5 (7.9) | <0.0001 |
| CES-D | N = 396 5.2 (7.2) | N = 57 5.9 (7.8) | 0.48 |
| Instrumental Activities of Daily Living | N = 444 153 (34.5) | 54 (60.7) | <0.0001 |
| Activities of Daily Living | N = 445 33 (7.4) | N = 88 32 (36.4) | <0.0001 |
Data are expressed as means (standard deviations), or n (percentages).
CES-D: Center for Epidemiologic Studies-Depression Scale
*T-test or chi-square or Fisher test as appropriate
Table 2 shows the socio-demographic characteristics and health status according to gender at the baseline. The mean age of the 449 participants [159 women (35.4%) and 290 men (64.6%)] was 81.2 years (SD 5.0) for women and 80.8 years (SD 4.0) for men. Women had more depressive symptoms (p<.001), lower BMI (p = .02), more disability for IADL (p<.0001) and ADL (p = .006) compared to men. No difference between men and women was reported for age and cognitive status.
Table 2. Main characteristics of the study sample according to gender.
| Women 159 (35.4) | Men 290 (64.6) | P* | |
|---|---|---|---|
| Age (years) | 81.2 (5.0) | 80.8 (4.0) | 0.46 |
| Height (m) | 1.58 (0.06) | 1.68 (0.07) | <0.001 |
| Weight (kg) | 66.9 (13.5) | 78.9 (13.2) | <0.001 |
| Body Mass Index (kg/m2) | 26.7 (4.9) | 27.8 (3.9) | 0.02 |
| Mini Mental State Examination | 24.4 (3.9) | 24.5 (4.1) | 0.82 |
| CES-D | 6.8 (8.6) | 4.3 (6.1) | 0.002 |
| Disability on Instrumental Activities of Daily Living | 73 (46.5) | 80 (27.9) | <0.001 |
| Disability on Activities of Daily Living | 19 (12.0) | 14 (4.9) | 0.006 |
| 4-meter gait speed (m/sec) | 0.98 (0.42) | 1.12 (0.37) | <0.001 |
Data are expressed as means (standard deviations), or n (percentages).
CES-D: Center for Epidemiologic Studies-Depression Scale
*T-test or chi-square or Fisher test as appropriate
The relationship between the GS and BMI categories in analyses of covariance is presented in Table 3. The unadjusted means of GS were 0.83 (95% CI 0.61–1.04) m/sec in underweight participants, 0.87 (95% CI 0.72–1.02) m/sec in normal BMI, and 0.70 (95% CI 0.41–0.98) m/sec in overweight/obese individuals. After adjustment for age, the reported trends between GS and BMI in categories were largely confirmed. See adjustment for age and comorbidity in complementary analyses (S1 Annexe).
Table 3. Results from unadjusted and adjusted analyses of covariance presenting means (and 95% confidence intervals) of 4-meter gait speed according to body mass index (BMI) categories, stratified by gender.
| Unadjusted | Adjusted for age | |
|---|---|---|
| Women (n = 159) | ||
| a. BMI <20.0 kg/m2 (n = 14) | 0.83 [0.61; 1.04] | 0.95 [0.74; 1.16] |
| b. BMI 20.0–24.9 kg/m2 (n = 47) | 1.11 [0.99; 1.23] | 1.09 [0.98; 1.20] |
| c. BMI 25.0–29.9 kg/m2 (n = 62) | 1.00 [0.90; 1.10] | 1.00 [0.91; 1.10] |
| d. BMI 30.0–34.9 kg/m2 (n = 28) | 0.87 [0.72; 1.02] | 0.82 [0.67; 0.97] |
| e. BMI ≥35.0 kg/m2 (n = 8) | 0.70 [0.41; 0.98] | 0.70 [0.43; 0.98] |
| P | 0.02 | <0.001 |
| Men (n = 290) | ||
| a. BMI <20.0 kg/m2 (n = 7) | 0.83 [0.55; 1.10] | 0.85 [0.58; 1.12] |
| b. BMI 20.0–24.9 kg/m2 (n = 62) | 1.10 [1.01; 1.20] | 1.13 [1.04; 1.22] |
| c. BMI 25.0–29.9 kg/m2 (n = 140) | 1.16 [1.10; 1.22] | 1.16 [1.10; 1.22] |
| d. BMI 30.0–34.9 kg/m2 (n = 70) | 1.11 [1.03; 1.20] | 1.11 [1.02; 1.19] |
| e. BMI ≥35.0 kg/m2 (n = 11) | 0.97 [0.75; 1.19] | 0.94 [0.73; 1.16] |
| P | 0.08 | <0.001 |
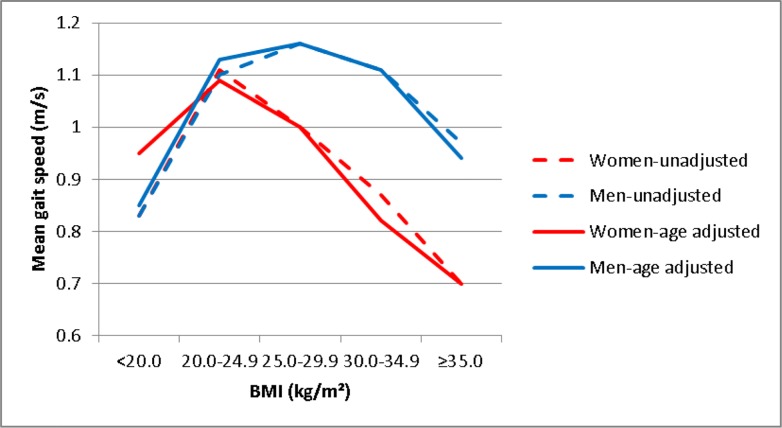
GS and BMI (continuous variables) were not significantly correlated (P = 0.16). Non-linear trends between BMI and GS were reported for men and women (Fig 1).
Fig 1. Association between gait speed and BMI.
Red lines represent women. Blue lines represent men. Dashed lines show unadjusted results. Continuous lines show age-adjusted results.
Discussion
In this cross-sectional analysis of persons aged 75 years and older, we found that GS follows a non-linear pattern across BMI groups. Our findings show that underweight and overweight/obese individuals are significantly slower in GS compared to persons with normal BMI. These relationships are independent of age.
Malnutrition is considered as a core feature of the frailty vicious cycle and contributes to the deterioration of the physical condition (including the mobility capacity) of older people[9].
The elderly population experiences a wide array of physical changes over time. Among these changes, loss of motor neurons, loss of muscle mass and lower aerobic capacity may greatly impact adaptation to everyday life situations. Indeed, they lead to a decrease in muscle strength, which is associated with slower gait speed[27,28] 19+ (REF). Several longitudinal studies suggest a link between BMI and GS[16,29–33]. Our results are partly consistent with these previous reports, but add knowledge in the field under specific aspects. In the present study, we explored the patterns of GS across BMI levels. High and low BMI is here shown to constitute a risk factor for being a slow walker, thus more vulnerability to stressors and exposed to negative outcomes.
Being overweight and obesity have been previously linked to sarcopenia[34]. Thus, individuals with obesity may spontaneously become slow walkers due to the growing balance impairment and physical fatigue. The excess of adipose tissue may alter the optimal ratio with lean mass and affect the quality and function of the skeletal muscle. Consistently, malnourished individuals may reduce their GS because of quantitative and qualitative deficits of the skeletal muscle[5,35].
BMI and GS can be considered two major markers of wellbeing in older people. They indeed provide comprehensive information about the helath status of the individual, even beyond the specific domain they are designed to measure (i.e., nutritional status and mobility function). Our study indicates a tendency [limited size of subjects in the categories (BMI<20 and BMI>30)] to nonlinear association between GS and BMI. Nevertheless, this finding could have an important implication in research. In fact, future works in the field may require the statistical models taking into account the non-linear relationship between BMI and GS.
This study had some limitations. First, the participants were recruited among persons aged 75 years and older living in rural areas. This may introduce a representativeness bias for external validation of our results. Second, the limited sample size may have affected the possibility to conduct more detailed analyses. Third, no conclusion in regard to cause or consequence can be drawn, due to the cross-sectional approach.
A tendency of non-linear relationship between gait speed and BMI is here demonstrated. The two variables are not correlated to one another and may provide complementary information in the comprehensive assessment of older persons.
Supporting information
(DOCX)
Data Availability
All relevant data are within the paper.
Funding Statement
The AMI project was funded by AGRICA(CAMARCA, CRCCA, CCPMA PREVOYANCE, CPCEA, AGRI PREVOYANCE), la Mutualité Sociale Agricole(MSA) de Gironde, la Caisse Centrale de la Mutualité Sociale Agricole (CCMSA). The AGRICA Group is a specialist for companies and employees of the agricultural world seeking supplemental pension, savings and healthcare insurance. AGRICA is one of the major French insurance providers offering protection for people employed in the agricultural sector. The other fundings come from the Mutualité Sociale Agricole (MSA), which is the unique Farmer Health Insurance System in France. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript."
References
- 1.Kuate-Tegueu C, Avila-Funes J-A, Simo N, et al. Association of Gait Speed, Psychomotor Speed, and Dementia. J Alzheimers Dis. 2017;60(2):585–592. 10.3233/JAD-170267 [DOI] [PubMed] [Google Scholar]
- 2.Cesari M. Role of gait speed in the assessment of older patients. JAMA. 2011;305(1):93–94. 10.1001/jama.2010.1970 [DOI] [PubMed] [Google Scholar]
- 3.Guralnik JM, Fried LP, Salive ME. Disability as a public health outcome in the aging population. Annu Rev Public Health. 1996;17:25–46. 10.1146/annurev.pu.17.050196.000325 [DOI] [PubMed] [Google Scholar]
- 4.Cesari M, Onder G, Russo A, et al. Comorbidity and physical function: results from the aging and longevity study in the Sirente geographic area (ilSIRENTE study). Gerontology. 2006;52(1):24–32. 10.1159/000089822 [DOI] [PubMed] [Google Scholar]
- 5.Cesari M, Penninx BWJH, Pahor M, et al. Inflammatory markers and physical performance in older persons: the InCHIANTI study. J Gerontol A Biol Sci Med Sci. 2004;59(3):242–248. 10.1093/gerona/59.3.m242 [DOI] [PubMed] [Google Scholar]
- 6.Semba RD, Ferrucci L, Sun K, et al. Oxidative stress and severe walking disability among older women. Am J Med. 2007;120(12):1084–1089. 10.1016/j.amjmed.2007.07.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cesari M, Kritchevsky SB, Penninx BWHJ, et al. Prognostic value of usual gait speed in well-functioning older people—results from the Health, Aging and Body Composition Study. J Am Geriatr Soc. 2005;53(10):1675–1680. 10.1111/j.1532-5415.2005.53501.x [DOI] [PubMed] [Google Scholar]
- 8.3C Study Group. Vascular factors and risk of dementia: design of the Three-City Study and baseline characteristics of the study population. Neuroepidemiology. 2003;22(6):316–325. 10.1159/000072920 [DOI] [PubMed] [Google Scholar]
- 9.Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–156. 10.1093/gerona/56.3.m146 [DOI] [PubMed] [Google Scholar]
- 10.Seidell JC. The impact of obesity on health status: some implications for health care costs. Int J Obes Relat Metab Disord. 1995;19 Suppl 6:S13–16. [PubMed] [Google Scholar]
- 11.Seidell JC. Obesity in Europe: scaling an epidemic. Int J Obes Relat Metab Disord. 1995;19 Suppl 3:S1–4. [PubMed] [Google Scholar]
- 12.Gill SV, Narain A. Quantifying the effects of body mass index on safety: reliability of a video coding procedure and utility of a rhythmic walking task. Arch Phys Med Rehabil. 2012;93(4):728–730. 10.1016/j.apmr.2011.09.012 [DOI] [PubMed] [Google Scholar]
- 13.Gill SV, Hicks GE, Zhang Y, Niu J, Apovian CM, White DK. The association of waist circumference with walking difficulty among adults with or at risk of knee osteoarthritis: the Osteoarthritis Initiative. Osteoarthr Cartil. 2017;25(1):60–66. 10.1016/j.joca.2016.07.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Forhan M, Gill SV. Obesity, functional mobility and quality of life. Best Pract Res Clin Endocrinol Metab. 2013;27(2):129–137. 10.1016/j.beem.2013.01.003 [DOI] [PubMed] [Google Scholar]
- 15.Blaum CS, Xue QL, Michelon E, Semba RD, Fried LP. The association between obesity and the frailty syndrome in older women: the Women’s Health and Aging Studies. J Am Geriatr Soc. 2005;53(6):927–934. 10.1111/j.1532-5415.2005.53300.x [DOI] [PubMed] [Google Scholar]
- 16.Hubbard RE, Lang IA, Llewellyn DJ, Rockwood K. Frailty, body mass index, and abdominal obesity in older people. J Gerontol A Biol Sci Med Sci. 2010;65(4):377–381. 10.1093/gerona/glp186 [DOI] [PubMed] [Google Scholar]
- 17.Kamiya Kentaro, Hamazaki Nobuaki, Matsuzawa Ryota,. Sarcopenia: prevalence and prognostic implications in elderly patients with cardiovascular disease. JCSM Clinical Reports. 2017;2(2). [Google Scholar]
- 18.Chiles Shaffer N, Simonsick EM, Thorpe RJ, Studenski SA. The Roles of Body Composition and Specific Strength in the Relationship Between Race and Physical Performance in Older Adults. J Gerontol A Biol Sci Med Sci. December 2019. 10.1093/gerona/glz103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Perez-Sousa MA, Venegas-Sanabria LC, Chavarro-Carvajal DA, et al. Gait speed as a mediator of the effect of sarcopenia on dependency in activities of daily living. J Cachexia Sarcopenia Muscle. 2019;10(5):1009–1015. 10.1002/jcsm.12444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pérès K, Matharan F, Allard M, et al. Health and aging in elderly farmers: the AMI cohort. BMC Public Health. 2012;12:558 10.1186/1471-2458-12-558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Féart C, Jutand MA, Larrieu S, et al. Energy, macronutrient and fatty acid intake of French elderly community dwellers and association with socio-demographic characteristics: data from the Bordeaux sample of the Three-City Study. Br J Nutr. 2007;98(5):1046–1057. 10.1017/S0007114507756520 [DOI] [PubMed] [Google Scholar]
- 22.Guigoz Y, Vellas B, Garry PJ. Assessing the nutritional status of the elderly: The Mini Nutritional Assessment as part of the geriatric evaluation. Nutr Rev. 1996;54(1 Pt 2):S59–65. 10.1111/j.1753-4887.1996.tb03793.x [DOI] [PubMed] [Google Scholar]
- 23.Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. STUDIES OF ILLNESS IN THE AGED. THE INDEX OF ADL: A STANDARDIZED MEASURE OF BIOLOGICAL AND PSYCHOSOCIAL FUNCTION. JAMA. 1963;185:914–919. 10.1001/jama.1963.03060120024016 [DOI] [PubMed] [Google Scholar]
- 24.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9(3):179–186. [PubMed] [Google Scholar]
- 25.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. 10.1016/0022-3956(75)90026-6 [DOI] [PubMed] [Google Scholar]
- 26.Tabue-Teguo M, Le Goff M, Avila-Funes JA, et al. Walking and psychomotor speed in the elderly: concordance, correlates and prediction of death. J Nutr Health Aging. 2015;19(4):468–473. 10.1007/s12603-014-0560-y [DOI] [PubMed] [Google Scholar]
- 27.Andersen JL, Aagaard P. Effects of strength training on muscle fiber types and size; consequences for athletes training for high-intensity sport. Scand J Med Sci Sports. 2010;20 Suppl 2:32–38. 10.1111/j.1600-0838.2010.01196.x [DOI] [PubMed] [Google Scholar]
- 28.Mendes J, Borges N, Santos A, et al. Nutritional status and gait speed in a nationwide population-based sample of older adults. Sci Rep. 2018;8(1):4227 10.1038/s41598-018-22584-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rietman ML, van der A DL, van Oostrom SH, et al. The Association between BMI and Different Frailty Domains: A U-Shaped Curve? J Nutr Health Aging. 2018;22(1):8–15. 10.1007/s12603-016-0854-3 [DOI] [PubMed] [Google Scholar]
- 30.Stenholm S, Sainio P, Rantanen T, et al. High body mass index and physical impairments as predictors of walking limitation 22 years later in adult Finns. J Gerontol A Biol Sci Med Sci. 2007;62(8):859–865. 10.1093/gerona/62.8.859 [DOI] [PubMed] [Google Scholar]
- 31.Stenholm S, Shardell M, Bandinelli S, Guralnik JM, Ferrucci L. Physiological factors contributing to mobility loss over 9 years of follow-up—results from the InCHIANTI study. J Gerontol A Biol Sci Med Sci. 2015;70(5):591–597. 10.1093/gerona/glv004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Visser M, Langlois J, Guralnik JM, et al. High body fatness, but not low fat-free mass, predicts disability in older men and women: the Cardiovascular Health Study. Am J Clin Nutr. 1998;68(3):584–590. 10.1093/ajcn/68.3.584 [DOI] [PubMed] [Google Scholar]
- 33.Zoico E, Di Francesco V, Mazzali G, et al. High baseline values of fat mass, independently of appendicular skeletal mass, predict 2-year onset of disability in elderly subjects at the high end of the functional spectrum. Aging Clin Exp Res. 2007;19(2):154–159. 10.1007/bf03324682 [DOI] [PubMed] [Google Scholar]
- 34.Woo J, Leung J. Sarcopenic Obesity Revisited: Insights From the Mr and Ms Os Cohort. J Am Med Dir Assoc. 2018;19(8):679–684.e2. 10.1016/j.jamda.2018.03.003 [DOI] [PubMed] [Google Scholar]
- 35.Dufour AB, Hannan MT, Murabito JM, Kiel DP, McLean RR. Sarcopenia definitions considering body size and fat mass are associated with mobility limitations: the Framingham Study. J Gerontol A Biol Sci Med Sci. 2013;68(2):168–174. 10.1093/gerona/gls109 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
Data Availability Statement
All relevant data are within the paper.