Abstract
The effects of work and the conditions of employment on health behaviors and intermediate health conditions have been demonstrated, to the extent that these relationships should be addressed in efforts to prevent chronic disease. However, conventional health promotion practice generally focuses on personal risk factors and individual behavior change. In an effort to find solutions to the myriad of health challenges faced by the American workforce, the U.S. National Institute for Occupational Safety and Health (NIOSH) established the Total Worker Health® (TWH) program. Originally organized around the paradigm of integrating traditional occupational safety and health protections with workplace health promotion, TWH has evolved to a broader emphasis on workplace programs for enhancing worker safety, health, and well-being. Among the research programs and approaches developed by investigators at NIOSH Centers of Excellence for TWH and elsewhere, definitions of ‘integration’ in workplace interventions vary widely. There is no consensus about which organizational or individual outcomes are the most salient, how much to emphasize organizational contexts of work, or which program elements are necessary in order to qualify as ‘Total Worker Health’. Agreement about the dimensions of integration would facilitate comparison of programs and interventions which are self-defined as TWH, although diverse in content. The specific criteria needed to define integration should be unique to that concept—i.e. distinct from and additive to conventional criteria for predicting or evaluating the success of a workplace health program. We propose a set of four TWH-specific metrics for integrated interventions that address both program content and process: (i) coordination and interaction of workplace programs across domains; (ii) assessment of both work and non-work exposures; (iii) emphasis on interventions to make the workplace more health-promoting; and (iv) participatory engagement of workers in pivotal ways during intervention prioritization and planning to develop self-efficacy in addressing root causes, skill transfer, building program ownership, empowerment, and continuous improvement. Thus we find that integration requires organizational change, both to engage two managerial functions with different goals, legal responsibilities, and (often) internal incentives & resources, and also to orient the organization toward salutogenesis. Examples from research activity within the Center for the Promotion of Health in the New England Workplace illustrate how these criteria have been applied in practice.
Keywords: CPH-NEW, intervention, participatory, salutogenesis, Total Worker Health, well-being, work organization
Introduction
The Total Worker Health® (TWH) program of the U.S. National Institute for Occupational Safety and Health (NIOSH) seeks to improve workforce health through integration of ‘health protection’—i.e. preventing work-related disease, injury, and disability—with ‘activities that advance their overall well-being’ (NIOSH, 2018a; Tamers et al., 2019). The initial paradigm for ‘integration’ emphasized the administrative coordination of employer programs for occupational safety and health (OSH) protection and worksite health promotion (WHP). OSH was characterized as workplace-specific activities prioritized according to the standard hierarchy of controls (NIOSH, 2018b) (in descending order): hazard elimination, product substitution, engineering controls, administrative controls, and personal protective equipment. (Note that for organizational stressors—unlike chemical exposures—job redesign would likely be classified under ‘administrative controls’, so the classic hierarchy does not perfectly map onto more modern concerns.) WHP was defined in terms of its traditional practice as individualized health intervention, with an emphasis on health education and policy and environment supports of behavior change to achieve goals such as weight loss, blood pressure control, smoking cessation, and chronic disease screening.
With few exceptions (e.g. DeJoy and Wilson, 2003), these two types of programs have traditionally operated independently in U.S. employer organizations (Hymel et al., 2011), without a common reporting structure or formal coordination of program goals and activities. The divide in institutional responsibility is sufficient to impede implementation of a combined approach, even when upper management supports the concept (Cherniack and Lahiri, 2010; Cherniack et al., 2010). While successful WHP programs may also include attention to workers’ compensation, injury care and duty modification, these have been far less typical elements (Stave et al., 2003). Arguments for combining these two domains range from greater efficiency of resource allocation to greater effectiveness in workforce health and organizational sustainability.
The NIOSH TWH program acknowledges that health problems previously considered unrelated to occupation are affected by the conditions of work, including organizational characteristics such as control over decision-making that traditionally fall into a managerial rather than occupational health framework. There is also explicit recognition of mechanisms by which work and employment conditions affect socioeconomic disparities in health (Schulte et al., 2012; Tamers et al., 2019).
As noted in a recent systematic review, the meaning of program ‘integration’ and the criteria for its assessment are essential for defining what is and is not included, and thus how to assess the value of TWH (Bradley et al., 2016; Feltner et al., 2016). A consensus definition is needed to reduce ambiguity about which programs belong under the TWH umbrella (regardless of how they are labeled) and facilitate comparison of goals and findings from diverse research studies and projects. Agreement about the necessary elements of an integrated program would also support programs in the formative stage to establish a yardstick and help practitioners, management and labor assess their potential value (Lax, 2016).
Sorensen and Barbeau (2012) have asked a fundamental question: whether independent, well-functioning OSH and WHP programs should be assessed as ‘integrated’ merely on the basis of programmatic coexistence. A derivative set of questions has moved us toward a deeper consideration of the TWH potential in workplace programs. These include, in particular, what is unique about integrated programs; how to measure the extent and quality of integration; how to define consistency of goals between (previously separate) functions; how to determine the quality of added value from integration; and how to characterize the organizational changes inherent to the integration process.
Scientific justification for ‘integrated’ TWH programs: overlap of work and non-work health risk factors
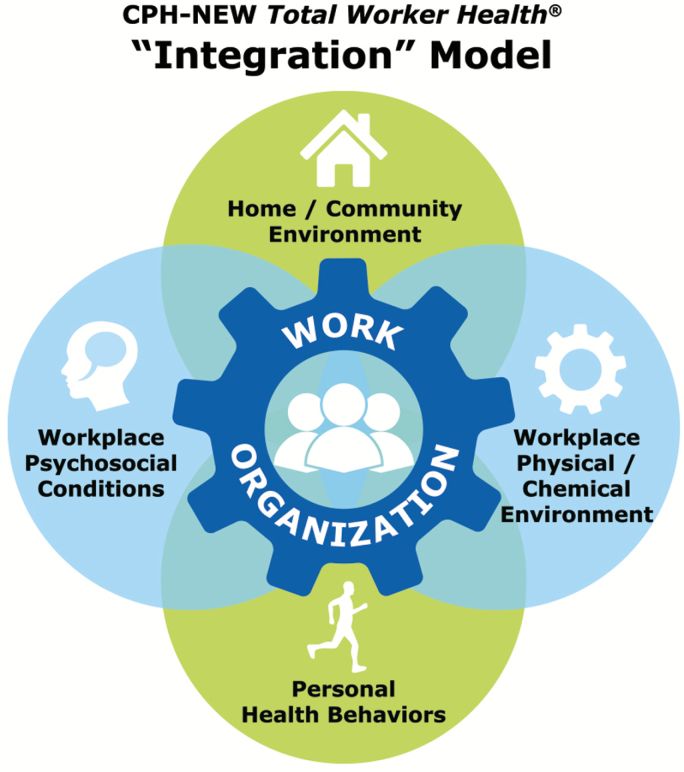
When NIOSH extended the domain of TWH to workforce health and well-being broadly, the set of causes under study by occupational health scientists was expanded. Working conditions, home and community life, and personal health behaviors and conditions all contribute to the risk of injury and disease (Fig. 1). Many possible interactions among these remain unexamined.
Figure 1.
The CPH-NEW Total Worker Health model of integration.
A substantial literature documents the impact of working conditions on health outcomes not traditionally attributed to work. The importance of work quality and organization to health has been especially articulated for psychosocial job strain and cardiovascular disease outcomes such as myocardial infarction (Bosma et al., 1997; Belkic et al., 2004; Taouk et al., 2020). One important mediating relationship is through the association of organizational stressors with contributory behaviors such as physical inactivity and smoking (Albertsen et al., 2006; Choi et al., 2010; Heikkilä et al., 2012a; Nyberg et al., 2013; Miranda et al., 2015; Nobrega et al., 2016). Job strain also reduces sleep quality and quantity (Zhang et al., 2016)—in turn potentially influencing eating and exercise habits—and may increase alcohol intake for self-medication (Heikkilä et al., 2012b; Barnes and Zimmerman, 2013). Chronic health conditions affected by job strain, overtime, and night shifts, and lack of control over work schedules include hypertension (Babu et al., 2014), obesity (Gram Quist et al., 2013), mental health (Virtanen et al., 2008; Marchand and Blanc, 2010; Too et al., 2019), sleep disorders (Kalimo et al., 2000), and diabetes (Nyberg et al., 2014). Conversely, social networks—including those at work—have positive buffering effects on mental health and overall mortality (Holt-Lunstad et al., 2010). Another problem is excessive noise at work, responsible for hearing loss and safety problems through interference with communication and loss of mental concentration (Mital et al., 1992; Ljungberg et al., 2007). Noise also causes hypertension, sleep disruption, and psychological stress (Münzel et al., 2014; Skogstad et al., 2016). The high-level implication of this literature, taken together, is that occupational conditions represent generally unrecognized risk factors for unhealthy behaviors that are traditionally classified purely as individual choices or ‘personal lifestyle’, and for chronic disease outcomes that are rarely recognized as work-related. This point underlies the second and third criteria proposed below for defining Total Worker Health.
The 21st century trends toward longer work weeks, proliferation of contingent work, diminished stable income, and the decline of the self-contained firm have introduced job insecurity, loss of employment benefits, underemployment, and a more transitory association between workers and managers (Weil, 2014; Howard, 2017). These dynamic transformations in work relationships (variously described as the ‘gig’ economy, precarious employment, the postcapitalist long wave, and creative or permanent disruption) have important effects on mental health (Kim et al., 2015; Milner et al., 2016; Juliá et al., 2017; Milner and LaMontagne, 2017) as well as other chronic disease risks (Monsivais et al., 2015; Hougaard et al., 2017; Waynforth et al., 2018; Wahrendorf et al., 2019). Extended and irregular schedules impact personal time for rest and family life, further affecting health and well-being of workers (Obidoa et al., 2011) as well as that of their children (Schneider and Harknett, 2019). Employed family caregivers report increased work–family conflict from coincident care of older adults and children (Hammer et al., 2008), a sometimes-overlooked stressor with additional adverse physical and psychological health effects (Fortinsky et al., 2007).
The relationship between the workplace and the community is also relevant to population health and well-being. Not all of these issues can be captured by measures of integration, but evaluators of TWH programs should be alert to the potential effects of regional demographics, employment patterns, and community resources as powerful external modifiers of morbidity and mortality. Population data show strong associations between the quality of community and family life and mental health (Strine et al., 2009). Workplace-specific influences on health and disease inevitably interact with other social mechanisms such as unsafe neighborhoods, lack of access to exercise facilities or healthy food choices in the community, and social discrimination (Largo-Wight, 2011; Bennett and Tetrick, 2013). Simultaneously and not coincidentally, there are important health trends in the American adult population, including high rates of drug overdoses, suicide, and cirrhosis (Case and Deaton, 2015) and racial/ethnicity disparities in severe maternal morbidity (Leonard et al., 2019) which demonstrate persistent and increasing health inequalities by region, race/ethnicity, and socioeconomic status.
Prior models of ‘integrated’ workplace programs
The NIOSH publication, ‘Fundamentals of Total Worker Health® Approaches’ (2016), provided relatively modest guidance on integration, centered on a baseline assessment of ‘existing workplace policies, programs, and practices relevant to safety, health, and well-being.’ Five defining elements were listed: (i) leadership commitment, (ii) workplace design to promote health and lower risk, (iii) worker engagement, (iv) confidentiality, and (v) integration of relevant systems. The document illustrated multiple possible meanings of integration, such as that between previously separate programs or services, labor and management decision-making, and prescribed sets of risk factors.
The American Heart Association’s Position Statement on Effective Worksite Wellness Programs (Carnethon et al., 2009) called for ‘supportive social and physical environments’ at work as one component. This element emphasized both facilitating healthy behaviors and minimizing hazards in the workplace. Similarly, the World Health Organization (2010) endorsed the concept of the ‘health-promoting workplace’, wherein the conditions of employment protect against physical and psychosocial risks in the workplace. These models place some responsibility for workforce health on working conditions, including but going beyond the workplace as a venue for WHP service delivery.
The American College of Occupational and Environmental Medicine proposed an Integrated Health and Safety (IHS) Index, a performance assessment tool with three categorical domains: economics, metrics, and environment (Loeppke et al., 2015). The quantifying and synthesizing of both OSH and WHP functions is exemplified by hazard recognition (volume of inspections and reports); recognition of chronic health conditions (health risk stratification); and assessment of presenteeism (simple coefficients for weighting specific health conditions). The IHS Index is a managerially oriented framework for placing implicit value on workforce health and well-being; it does not assess integration directly or propose a formula for combining OSH and WHP.
Sorensen et al. (2013; 2016) offered an overall framework and metric focusing on organizational and program characteristics: Leadership commitment, accountability, and resources; Program participation at multiple levels; Policies, programs, and practices for positive working conditions; Adherence to ethical norms, federal and state regulations; and Data-driven change. These conditions are all desirable and may be necessary to achieve meaningful improvement, but several are not specific to the definition of TWH—i.e. they could apply equally to any form of workforce health or safety program. Further, an effort that is truly integrative might fail to obtain leadership buy-in precisely because it identifies the workplace as the source of health problems not previously recognized as work-related.
Another approach to defining TWH scope required that individual worker health outcomes should be drawn from both the ‘work-related’ and the ‘non-work-related’ categories (Anger et al., 2015). Since the scientific rationale for TWH begins with the fact that exposures and hazards from all areas of life impact health, the attribution of chronic health conditions to either work or non-work causes necessarily implies that these are mutually exclusive. Thus, using the choice of health outcomes as indicative of an integrated approach would be incompatible with the current state of the science.
Several European colleagues have taken an approach to workforce health that addresses both the hazards faced by many in the work environment and the potential benefits of well-designed jobs and workplaces. In particular, Jenny et al. (2017) have advanced the concept of ‘salutogenesis’ at work, meaning that job design could ‘not only… mitigate the pathogenic effects of stressors at work, but have a distinct effect on positive health outcomes,’ especially through optimizing job demands and increasing job resources to enhance sense of coherence. von Thiele Schwarz et al. (2015) explicitly seek to evaluate the possible effects of integrating workplace health protection and health promotion. They have involved employees in participatory design of interventions for continuous improvement in both domains, with management responsible for larger and more difficult changes in work organization that could not be made at the unit level.
New proposed core indicators of ‘integration’
Investigators in the Center for the Promotion of Health in the New England Workplace (CPH-NEW), a TWH Center of Excellence, have formulated four indicators arising from the core concept of combining approaches from two domains that have predominantly been implemented separately. The focus is on efforts to create a health-promoting work environment and work organization in ways that are specific and unique to the construct of integration. These indicators are drawn from our direct experience in field interventions, contrasted with other experience with traditional occupational health and safety or workplace health promotion. These criteria should be equally useful for evaluating employer services and researcher-designed programs.
Coordination of goals and activities between the occupational safety and the health promotion functions, e.g. using a common reporting structure and systematic examination of how risk factors from the two domains interact with each other.
Assessment activities are designed to identify both work and non-work hazards that impact employee safety, health, and well-being.
Interventions seek to prioritize mitigation of workplace contributors to poor health, safety, or well-being, such as improving organizational safety and health policies and practices, to make the workplace health-promoting.
Participatory engagement processes empower workers to collaborate to prioritize goals, identify root causes, join in decision-making about intervention activities and design of programs, and interpret findings in light of both labor and management perspectives.
These criteria have been operationalized and applied across CPH-NEW research and outreach activities (e.g. Robertson et al., 2015; Dugan et al., 2016; Nobrega et al., 2017). They are incorporated into the program implementation and evaluation materials of our Healthy Workplace Participatory Program (HWPP) and its step-by-step, interactive guide for the participatory design of interventions, the ‘IDEAS Tool’ (www.uml.edu/Research/CPH-NEW/Healthy-Work-Participatory-Program). We use the term ‘Design Teams’ (DTs) to designate employee groups who apply this program to engage in problem identification, root causes analysis, and intervention design, implementation, and evaluation. This approach to involving line-level employees is modeled after participatory ergonomics (Cherniack and Punnett, 2019). A management ‘Steering Committee’ reviews proposals developed by the DT and presented in a business case format; the managers are responsible for marshaling resources and providing oversight of interventions approved for implementation. Our experience with HWPP illustrates that it is feasible to train workers and supervisors to develop participatory structures to support quality of work life and quality of life interventions within the workplace. However, effective facilitation of the HWPP with its two-committee structure is not without its challenges, especially if Steering Committee support is inadequate (e.g. Strickland et al., 2019). In our projects, workers have readily grasped the concept of integration, as their own lived experiences of health and safety problems do not necessarily involve partitioning between working conditions and non-work factors.
The examples that follow illustrate how the above core indicators can be operationalized in utilizing the proposed definition of TWH.
1. Coordination of programs and activities
Total Worker Health refers to ‘policies, programs, and practices that integrate protection from work-related safety and health hazards with promotion of injury and illness prevention efforts to advance worker well-being’ (NIOSH, 2018a). While program coordination is not sufficient, it was the original concept defining TWH. It is common practice for employer organizations to manage OSH programs and policies separately from health promotion and behavioral health programs which address ‘wellness’ or ‘well-being’. It follows that coordination of these program areas would be necessary to comprehensively and coherently address safety, health, and well-being. However, simply having parallel programs is not sufficient; there must be opportunities for each one to inform and influence the other recursively over time.
CPH-NEW case examples
A study of nursing home employee health was conducted in a large long-term care company (Zhang et al., 2011, 2014; Miranda, 2015). The larger organization instituted programs to reduce manual resident handling, disseminate personal health information, and improve quality of supervision through training of key facility personnel. In three centers, the investigators assisted in development of worker teams to brainstorm root causes of health problems and possible interventions. These teams committed to activities to support workers’ healthy behaviors both at and away from work, including community gardens, improved offerings in vending machines, facility kitchens selling food (e.g. salads) to staff members, recipe swaps, and weight loss campaigns. Despite obstacles to long-term program sustainability in a low-wage and precarious sector (Kotejoshyer et al., 2019), there was a high level of employee interest and creativity. The integration concept had high face validity for participants and program coordination was feasible within the organization at both the facility and corporate levels.
Building on those experiences, the ‘Safety and Health through Integrated Facilitated Teams’ study (2016–21) seeks to evaluate HWPP effectiveness in the healthcare sector. DTs are explicitly instructed to include both occupational and non-occupational risk factors for workforce health, spanning topics that are traditionally addressed separately in OSH and WHP. The program has been integrated into the existing organizational safety or Environment of Care committees, with the goal of broadening the scope of safety interventions to incorporate prevention activities that might ordinarily be developed and managed through human resource functions. In this way, the occupational safety activities now overlap organizationally with the health promotion activities in each institution.
2. Assessment of work and non-work exposures affecting health, safety, and well-being
Because working conditions affect risk of health outcomes not usually attributed to work, as discussed above, it follows that an integrated program needs to identify risk factors inside as well as outside the workplace. Exposure assessment should span chemical, physical, and psychosocial domains, as combined exposures have consequences for appropriate selection of workplace intervention approaches. Multiple instruments and methods are needed to pinpoint where risks are located, along with their upstream determinants. Organization-level assessment often begins with a global inventory of the organization and any safety or health programs as described by upper and middle management. It is essential also to assess the qualitative experience of individual workers to understand the workplace factors that underlie health and safety issues but which may be unrecognized. Upstream determinants could be any workplace policies and practices that lead to unhealthy behaviors, whether intentionally or not. For example, irregular work schedules may interfere with leisure-time exercise, and unpredictable meal breaks lead people to over-eat in order to avoid becoming hungry later in the shift (Nobrega et al., 2016). Low participation in WHP activities has been associated with low job control in combination with high physical and emotional demands (Jørgensen et al., 2016). In Connecticut Department of Corrections facilities, a policy intended to ensure adequate staffing prohibits corrections officers (COs) from refusing extra shifts if they are on site when a staffing gap arises (Namazi et al., 2019). This induces COs to leave the premises as quickly as possible when their shifts end, rather than utilizing the facility gym during permitted hours.
CPH-NEW case examples
A survey of health and safety committee (HSC) members in Connecticut showed that an integrated approach to exposure assessment was generally lacking. The Connecticut Council on Occupational Safety and Health (ConnectiCOSH), a coalition of labor unions, health and technical professionals, evaluated HSCs in organizations where members were employed and served as labor representatives. Survey items covering the four CPH-NEW TWH integration indicators were developed and pretested. These asked whether the HSC assessed physical risk factors such as ergonomic hazards, noise, and chemical exposures; organizational factors including shift work, scheduling, work pace, job control, and overtime; social/interpersonal factors including incivility, harassment, and bullying; and well-being factors traditionally considered non-work related, such as chronic health conditions, sleep, and substance abuse. The 116 respondents (48% workers, 52% management) reported that hazard assessments and interventions addressed the first set of traditional health and safety topics but less often work organization, social/interpersonal risk factors, or worker well-being. These data were used to inform ConnectiCOSH training to increase HSC awareness and practice of TWH. Similar surveys elsewhere could identify the level and extent of employer TWH practice, to guide outreach and resource planning.
In a rural community hospital, an Occupational Health and Safety Nurse Manager used the HWPP Toolkit to initiate a DT of nurses in one hospital unit with a high patient handling injury rate. They implemented a root causes analysis exercise and surveyed nurses on the unit to identify key factors on and off the job that might lead to patient handling injuries. The team identified key risk factors as inaccessibility of lift equipment (slings and lift equipment), staff scheduling gaps that prevented rest breaks, and fatigue from inadequate sleep caused by 12-h shifts closely spaced and irregular rotation schedules. The intervention proposed by the DT included improvements in shift scheduling rules and education about sleep hygiene. Engaging the nurses was essential to identify work organization issues that had not been previously recognized. According to the nurse manager, ‘We had no clue about the scheduling, the amount of sleep people get, and that these guys don’t actually schedule breaks and coverage for breaks. That turned out to be the biggest issue we needed help with, which was a surprise to everyone.’
3. Interventions to mitigate workplace contributors to poor safety, health, and well-being
This criterion reflects the increasing evidence about the role of healthy work organization as a necessary precondition for worker health, as briefly summarized above. It follows that genuine efforts to mitigate workplace safety and health risk factors represent a necessary precondition to more effective health promotion in the occupational setting. Prioritization of interventions should first seek to eliminate or mitigate workplace contributions to chronic health outcomes, before focusing on individual-level behaviors. As in the hierarchy of controls, changes at higher levels, such as elimination of a hazard, should be prioritized over changes in employee behavior. For example, work schedules and sleep–rest patterns should be intervened upon before relying upon individual relaxation practices to improve sleep hygiene or reduce blood pressure.
CPH-NEW case examples
A property management firm supported their building maintenance technicians to develop a DT (Robertson et al., 2015). Following administration of surveys and focus groups, the technicians prioritized job stress from work overload for interventions, highlighting problems with organizational communication, such as unpredictable and duplicate work orders. They recommended (and helped with developing) education for residents and office staff. They also recommended policy and practice standards for adhering to the company’s computerized work order system. The technicians identified these interventions as critical for addressing the underlying drivers of stress and overwork on the job.
Correctional workers have high rates of work–family conflict, depression, anxiety substance misuse, stress-related health problems and suicide (Cherniack et al., 2016). In our corrections research, three different DTs are developing interventions to improve personnel mental health, with primary focus on workplace risk factors. One intervention included policies and procedures to reduce workforce stress and trauma following critical incidents such as assaults. The DTs also sought improve interpersonal relationships, in a harsh work climate with systemic pressures not to show vulnerability, as a way to buffer the health impacts of stress and trauma. One DT coordinated with clinical experts to increase peer proficiency in recognizing signs, symptoms, and causes of trauma and mental health difficulties. Immediate goals are to increase mental health literacy, reduce stigma, and provide resources for treatment, while seeking to facilitate identification and treatment in a work environment that prizes confidentiality and emotional suppression (i.e. restricting the display of emotions). Longer-term goals include procedures for conflict de-escalation, improved inter-workforce communications, and targeted response to traumatic events.
4. Participatory research processes
If addressing workplace barriers to health is a foundational principle of Total Worker Health, then participatory engagement of workers is essential for identifying those barriers and conceptualizing meaningful, practical solutions that are complete and sustainable. In the example of COs who cannot legally refuse extra shifts while they are physically on campus, this is an administrative staffing policy rather than a health-directed policy. Without worker input, we might not have recognized that it interferes with usage of physical exercise facilities before and after work.
We have observed numerous examples of creative ideas developed to address root causes. The structure provided by the HWPP facilitates communication and mutual learning between workers and management; we observe that workers’ opinions are delivered more effectively and have more credibility as a result. Placing workers at the center of the intervention design process has many benefits: identifying a wider scope of intervention targets, improving intervention fit with the workplace context, enhanced opportunities for organizational learning, and enhancing workers’ sense of ownership and self-efficacy (belief in one’s own capacity to improve and maintain health). The very act of participating in a team that is empowered to take decisions and make changes can improve social capital in the work environment and thus be health-promoting (Henning et al., 2009; Punnett et al., 2009, 2013; Cherniack et al., 2016). Taken together, these benefits of participatory interventions can offer greater impact than those initiated top-down.
CPH-NEW case examples
A correctional supervisors’ DT developed and administered a comprehensive survey to assess correctional supervisors’ health, in collaboration with the supervisors’ bargaining unit. A high prevalence of sleep problems emerged, along with novel survey findings about financial pressures to work extended hours. Three-quarters of the supervisors were interested in making behavior changes to improve sleep. The DT created a union-based sleep education training program to improve sleep quantity and quality through practicing sleep hygiene and guided meditation, which was delivered to 101 supervisors. The DT also worked with a university programmer to develop a smartphone app and trained supervisors in its use. The full intervention was incorporated into the collective bargaining agreement as a sleep training day with attendance and content monitored by the union. With strong advocacy by the supervisors’ union, senior administration has fully accommodated coverage and designated training time.
Separately, in a high security-level correctional facility, a DT of non-supervisory correctional staff investigated the root causes of workers’ respiratory symptoms through an employee survey and industrial hygiene consultation. They identified air quality problems and convection shifts from a dusty, antiquated air-handling system. They also discovered that furniture was being used to block air vents in order to prevent over-cooling in some areas. They proposed three intervention components: heating, ventilation and air conditioning (HVAC) maintenance with certification for inmates and officers; a zone-based approach to environmental control; and replacement of the HVAC system. The DT’s persistence resulted in HVAC housekeeping shared by staff and inmates, which continues to the present day, and an eventual agreement by management to replace the entire system. Without collecting the experience of the front-line officers, and the structured participatory process that built a foundation for respectful communication, system overhaul would likely never have been seriously considered.
Discussion
The four criteria proposed here for defining ‘integration’ are specific to the core idea of combining approaches from at least two domains of activity (OSH and WHP) that are predominantly implemented separately. The proposed criteria recognize the contributory roles of work, the individual and the community in health and well-being; and the company as a hierarchical, largely economic, entity and as a social organization. The concept of integration has meaning only if it applies to coordination of parallel programs in such a way that each one informs and influences the other. Worker health programs, regardless of which corporate function owns them, should attend to the influence of working conditions as risk factors, regardless of whether or not the outcomes may traditionally have been classified as ‘work-related’.
We have intentionally not included criteria related to program efficacy or effectiveness, or ethical considerations, which can equally well be applied to other types of worker health or safety programs. For example, the factor of management support is a generic indicator of the likely success of any program, regardless of its particular health or safety goal or domain. This concept of leadership commitment is reflected in NIOSH’s Fundamentals of Total Worker Health Approaches (NIOSH, 2016), and it is important to establish at the beginning of and during an intervention study, but it is not per se a defining feature of ‘integration’.
There are certainly overlaps between our four indicators and TWH criteria suggested by others. These include synthesis of organizational structures, attention to worker engagement, bringing a holistic perspective to the work-relatedness of health and disease, and communications within the workplace and with the community. However, unlike many other authors in this domain, we require attention to the causal contribution of occupational exposures and upstream organizational characteristics, in order to go beyond traditional WHP practice and create conditions that support healthy behaviors (salutogenesis). In this regard, we find the closest parallel to be the work of von Thiele Schwarz et al. (2015) and Jenny et al. (2017) noted above, because of their explicit attention to the effects of work on a broad set of health outcomes and their emphasis on workers as agents of change.
The emphasis on worker empowerment and skill transfer through participatory processes is a signature feature of the CPH-NEW definition of TWH. It goes beyond simply obtaining buy-in from management and workers (Henning et al., 2009; Robertson et al., 2015). We believe that integration cannot be achieved without a mechanism for learning from workers about their experiences of risk factors, how those interact with each other, and what obstacles they experience to being healthy and safe. We have built the HWPP approach on a foundation of engaging workers in the entire process, from needs assessment to selecting health and/or safety goals, to prioritization of intervention alternatives, to program evaluation and learning from the results to inform the next effort. This requires that they are afforded the opportunity to systematically look into and learn about health and safety issues most salient to them. Noting that they may lack organizational experience, confidence, or awareness of fiscal and material constraints, the HWPP communications structure seeks to bridge those gaps over time.
The needs expressed by workers themselves are often similar among workplaces, but the solutions may be unique to each setting because of local features. Thus, worker involvement is also necessary to understand specific job characteristics and work processes that impede health behaviors or participation in specific activities (Jørgensen et al., 2016) and what solutions would be feasible and meaningful for them. The potential benefits involve not only the immediate impact of specific workplace interventions, but also general improvement in the psychosocial work environment.
Worker well-being and quality of life are long-term outcomes that can only be measured partially at a point in time and are modified by stage of life. Well-being includes the freedom from health conditions with a long latency, which is not the same as an intermediate outcome evaluable within a 5-year research grant timeframe. Whereas the costs of an integrated intervention program and its targeted outcomes, such as hospital admissions or costs of medications, can be evaluated with a common cost metric, for example, well-being cannot. Yet well-being is highly relevant to employers. Australian researchers estimated total national annual employer costs for lost productivity due to depression of $AUD 8 billion, most due to mild depression. Their findings suggest that even subclinical levels of depression represent a significant productivity and economic burden not previously recognized (McTernan et al., 2013). Although ideally TWH would represent employer commitment throughout work and postwork lifetime, that would not seem realistic in light of the evolving conditions of employment.
Given the criteria proposed here, two important secondary questions follow: which characteristics are important to measure in each of those dimensions; and what method(s) to use to assess those factors. This is not a peripheral issue, as the results may be quite different if assessed by managers, workers, or researchers (Zhang et al., 2011). CPH-NEW projects involve collection of data from multiple sources over time, in order to triangulate perspectives from different levels, compare findings and data quality among methods, and identify leading indicators of changes in health behaviors and health conditions. We have elsewhere offered scoring systems (Dugan et al., 2016) and continue to revise these with accruing experience.
This proposal for defining TWH programs seeks to remedy the current lack of consistent measurement standards and definitions. A recent attempt at systematic review and meta-analysis of TWH programs concluded that pooling of results was not feasible because of the tremendous diversity in goals, methods, and outcomes (Bradley et al., 2016; Feltner et al., 2016). This conclusion was not unexpected, as the wide range of program activities is evident from even a cursory review of the NIOSH-funded Centers of Excellence for TWH. Ideally, ongoing dialogue among investigators and with NIOSH would lead over time to development of a consensus on primary research questions, methods and outcomes. This would be helpful in focusing the challenge to future researchers and reviewers, as well as to practitioners, management and labor with an interest in adopting TWH programs to tackle challenging problems of workforce health.
This discussion pertains to an approach that is still under development. Many research questions deserve more attention to better determine the feasibility and effectiveness of integrating workforce health protection and well-being. Participatory health improvement programs in the workplace face challenges related to the diversity of perspectives among organizational levels (Zhang et al., 2011; Hasson et al., 2013) and feedback control dynamics around intervention priority-setting and implementation (Cherniack et al., 2019) in the context of power structures within the workplace (Lax, 2016). Evaluation methods are needed to analyze the ways that management and labor representatives influence the implementation process and outcomes (Nielsen, 2013). Characterization of factors affecting uptake and implementation, continuous improvement processes, and related long-term challenges of program scale-up and sustainability, can benefit from dissemination and implementation science approaches (Dugan and Punnett, 2017; Schulte et al., 2017). The manner in which researchers withdraw from field sites at study end is likely to have specific consequences that affect the viability and long-term health of these TWH programs (Kotejoshyer et al., 2019). Beyond creating mechanisms to provide expert support on demand, what degree of management involvement in participatory intervention design will maintain their commitment to program goals and continuous improvement, while still supporting ‘bottom-up’ root cause analysis and solutions? Additionally, as the boundary between work and non-work settings becomes increasingly blurred, distinctions between work and non-work exposures may become harder to delineate. As in other areas of occupational health, surveillance through wearable devices, telecommuting, and other modern technologies could produce valuable data for TWH programs but also introduce a host of new privacy issues that could complicate achievement of fully integrated approaches.
Conclusions
The effectiveness of TWH programs has been difficult to evaluate, due in part to a lack of established metrics that clearly define and measure essential program elements across studies. CPH-NEW has defined a means to assess TWH integration based on a set of constructs that seek to identify what is unique about ‘integrated’ programs compared to traditional occupational health or health promotion efforts. By using these criteria for program design and evaluation, workplace safety and health practitioners can align their activities with TWH principles, regardless of which health and/or safety outcomes are under study, and future reviewers will be able to delineate the scope of the relevant literature more clearly.
Acknowledgments
This article was supported by Grant Number 1 U19 OH008857 from the National Institute for Occupational Safety and Health. The contents are solely the responsibility of the authors and do not necessarily represent the official views of NIOSH. The authors thank Dr Pouran Faghri for comments on earlier drafts, and all of the CPH-NEW researchers and students since 2006 whose field work that has informed the development and refinement of these principles.
Conflict of interest
The authors declare no conflict of interest relating to the material presented in this article.
References
- Albertsen K, Borg V, Oldenburg B (2006) A systematic review of the impact of work environment on smoking cessation, relapse and amount smoked. Prev Med; 43: 291–305. [DOI] [PubMed] [Google Scholar]
- Anger WK, Elliot DL, Bodner T et al. (2015) Effectiveness of Total Worker Health interventions. J Occup Health Psychol; 20: 226–47. [DOI] [PubMed] [Google Scholar]
- Babu GR, Jotheeswaran AT, Mahapatra T et al. (2014) Is hypertension associated with job strain? A meta-analysis of observational studies. Occup Environ Med; 71: 220–7. [DOI] [PubMed] [Google Scholar]
- Barnes AJ, Zimmerman FJ (2013) Associations of occupational attributes and excessive drinking. Soc Sci Med; 92: 35–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belkic KL, Landsbergis PA, Schnall PL et al. (2004) Is job strain a major source of cardiovascular disease risk? Scand J Work Environ Health; 30: 85–128. [DOI] [PubMed] [Google Scholar]
- Bennett JB, Tetrick LE (2013) The “We” in wellness: workplace health promotion as a positive force for health in society. In Olson-Buchanan J, Bryan LK, Thompson LF, editors. Using industrial-organizational psychology for the greater good. New York, NY: Routledge; pp 245–76. ISBN 978-0-203-06926-4 [Google Scholar]
- Bosma H, Marmot MG, Hemingway H et al. (1997) Low job control and risk of coronary heart disease in Whitehall II (prospective cohort) study. BMJ; 314: 558–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley CJ, Grossman DC, Hubbard RA et al. (2016) Integrated interventions for improving total worker health: a panel report from the National Institutes of Health Pathways to Prevention Workshop: total worker health-what’s work got to do with it? Ann Intern Med; 165: 279–83. [DOI] [PubMed] [Google Scholar]
- Carnethon M, Whitsel LP, Franklin BA et al. ; American Heart Association Advocacy Coordinating Committee; Council on Epidemiology and Prevention; Council on the Kidney in Cardiovascular Disease; Council on Nutrition, Physical Activity and Metabolism. (2009) Worksite wellness programs for cardiovascular disease prevention: a policy statement from the American Heart Association. Circulation; 120: 1725–41. [DOI] [PubMed] [Google Scholar]
- Case A, Deaton A (2015) Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci U S A; 112: 15078–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherniack M, Berger S, Namazi S et al. ; CPH-NEW Research Team. (2019) A participatory action research approach to mental health interventions among corrections officers: standardizing priorities and maintaining design autonomy. Occup Health Sci; 3: 387–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherniack M, Dussetschleger J, Dugan A et al. (2016) Participatory action research in corrections: the HITEC 2 program. Appl Ergon; 53 (Pt A): 169–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherniack M, Lahiri S (2010) Barriers to implementation of workplace health interventions: an economic perspective. J Occup Environ Med; 52: 934–42. [DOI] [PubMed] [Google Scholar]
- Cherniack M, Morse T, Henning R et al. (2010) Health promotion site selection blues: barriers to participation and implementation. J Occup Environ Med; 52: 626–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherniack M, Punnett L (2019) A participatory framework for integrated interventions. Chapter 7. In Hudson HL, Nigam JAS, Sauter SL, Chosewood LC, Schill AL, Howard J, editors. Total Worker Health: integrative approaches to safety, health, and well-being. Washington, DC: American Psychology Association Press. [Google Scholar]
- Choi B, Schnall PL, Yang H et al. (2010) Psychosocial working conditions and active leisure-time physical activity in middle-aged US workers. Int J Occup Med Environ Health; 23: 239–53. [DOI] [PubMed] [Google Scholar]
- DeJoy DM, Wilson MG (2003) Organizational health promotion: broadening the horizon of workplace health promotion. Am J Health Promot; 17: 337–41. [DOI] [PubMed] [Google Scholar]
- Dugan AG, Farr DA, Namazi S et al. (2016) Process evaluation of two participatory approaches: implementing Total Worker Health® interventions in a correctional workforce. Am J Ind Med; 59: 897–918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dugan AG, Punnett L (2017) Dissemination and implementation research for occupational safety and health. Occup Health Sci; 1: 29–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feltner C, Peterson K, Palmieri Weber R et al. (2016) The effectiveness of total worker health interventions: a systematic review for a National Institutes of Health Pathways to Prevention Workshop. Ann Intern Med; 165: 262–9. [DOI] [PubMed] [Google Scholar]
- Fortinsky RH, Tennen H, Frank N et al. (2007) Health and psychological consequences of caregiving. In Aldwin CM, Park CL, Spiro A, editors. Handbook of health psychology and aging. New York, NY: The Guilford Press; pp. 227–49. ISBN 1-59385-057-3. [Google Scholar]
- Gram Quist H, Christensen U, Christensen KB et al. (2013) Psychosocial work environment factors and weight change: a prospective study among Danish health care workers. BMC Public Health; 13: 43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammer LB, Neal MB (2008) Working sandwiched-generation caregivers: prevalence, characteristics, and outcomes. Psychologist-Manager J; 11: 93–112. [Google Scholar]
- Hasson H, Tafvelin S, von Thiele Schwarz U (2013). Comparing employees and managers’ perceptions of organizational learning, health, and work performance. Adv Dev Hum Resour; 15: 163–76. [Google Scholar]
- Heikkilä K, Nyberg ST, Fransson EI, et al. ; IPD-Work Consortium. (2012a) Job strain and tobacco smoking: an individual-participant data meta-analysis of 166 130 adults in 15 European studies. PLOS One; 7: e35463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heikkilä K, Nyberg ST, Fransson EI et al. ; IPD-Work Consortium. (2012b) Job strain and alcohol intake: a collaborative meta-analysis of individual-participant data from 140,000 men and women. PLoS One; 7: e40101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henning R, Warren N, Robertson M et al. ; CPH-NEW Research Team. (2009) Workplace health protection and promotion through participatory ergonomics: an integrated approach. Public Health Rep; 124 (Suppl. 1): 26–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TB, Layton JB (2010) Social relationships and mortality risk: a meta-analytic review. PLoS Med; 7: e1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hougaard CØ, Nygaard E, Holm AL et al. (2017) Job mobility and health in the Danish workforce. Scand J Public Health; 45: 57–63. [DOI] [PubMed] [Google Scholar]
- Howard J. (2017) Nonstandard work arrangements and worker health and safety. Am J Ind Med; 60: 1–10. [DOI] [PubMed] [Google Scholar]
- Hymel PA, Loeppke RR, Baase CM et al. (2011) Workplace health protection and promotion: a new pathway for a healthier—and safer—workforce. J Occup Envir Med; 53: 695–702. [DOI] [PubMed] [Google Scholar]
- Jenny GJ, Bauer GF, Vinje HF et al. (2017) The Application of Salutogenesis to Work. Chapter 20 In Mittelmark MB, Sagy S, Eriksson M, Bauer GF, Pelikan JM, Lindström B, Espnes GA, editors. The handbook of salutogenesis [Internet]. Cham (CH): Springer. [PubMed] [Google Scholar]
- Jørgensen MB, Villadsen E, Burr H et al. (2016) Does employee participation in workplace health promotion depend on the working environment? A cross-sectional study of Danish workers. BMJ Open; 6: e010516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juliá M, Vives A, Tarafa G, Benach J (2017) Changing the way we understand precarious employment and health: precarisation affects the entire salaried population. Saf Sci; 100: 66–73. [Google Scholar]
- Kalimo R, Tenkanen L, Härmä M et al. (2000) Job stress and sleep disorders: findings from the Helsinki Heart Study. Stress Med; 16: 65–75. [Google Scholar]
- Kim TJ, von dem Knesebeck O (2015) Is an insecure job better for health than having no job at all? A systematic review of studies investigating the health-related risks of both job insecurity and unemployment. BMC Public Health; 15: 985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotejoshyer R, Zhang Y, Flum M et al. (2019) Prospective evaluation of fidelity, impact and sustainability of participatory workplace health teams in skilled nursing facilities. Int J Environ Res Public Health; 16: 1494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Largo-Wight E. (2011) Cultivating healthy places and communities: evidenced-based nature contact recommendations. Int J Environ Health Res; 21: 41–61. [DOI] [PubMed] [Google Scholar]
- Lax MB. (2016) The perils of integrating wellness and safety and health and the possibility of a worker-oriented alternative. New Solut; 26: 11–39. [DOI] [PubMed] [Google Scholar]
- Leonard SA, Main EK, Scott KA et al. (2019) Racial and ethnic disparities in severe maternal morbidity prevalence and trends. Ann Epidemiol; 33: 30–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ljungberg JK, Neely G (2007) Stress, subjective experience and cognitive performance during exposure to noise and vibration. J Environ Psychol; 27: 44–54. [Google Scholar]
- Loeppke RR, Hohn T, Baase C et al. (2015) Integrating health and safety in the workplace: how closely aligning health and safety strategies can yield measurable benefits. J Occup Environ Med; 57: 585–97. [DOI] [PubMed] [Google Scholar]
- Marchand A, Blanc ME (2010) The contribution of work and non-work factors to the onset of psychological distress: an eight-year prospective study of a representative sample of employees in Canada. J Occup Health; 52: 176–85. [DOI] [PubMed] [Google Scholar]
- McTernan WP, Dollard M, LaMontagne AD (2013) Depression in the workplace: an economic cost analysis of depression-related productivity loss attributable to job strain and bullying. Work Stress; 27: 321–38. [Google Scholar]
- Milner A, Aitken Z, Kavanagh A et al. (2016) Persistent and contemporaneous effects of job stressors on mental health: a study testing multiple analytic approaches across 13 waves of annually collected cohort data. Occup Environ Med; 73: 787–93. [DOI] [PubMed] [Google Scholar]
- Milner A, LaMontagne AD (2017) Underemployment and mental health: comparing fixed-effects and random-effects regression approaches in an Australian working population cohort. Occup Environ Med; 74: 344–50. [DOI] [PubMed] [Google Scholar]
- Miranda H, Gore RJ, Boyer J et al. (2015) Health behaviors and overweight in nursing home employees: contribution of workplace stressors and implications for worksite health promotion. ScientificWorldJournal; 2015: 915359. doi: 10.1155/2015/915359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mital A, McGlothlin JD, Faard HF (1992) Noise in multiple-workstation open-plan computer rooms: measurements and annoyance. J Hum Ergol (Tokyo); 21: 69–82. [PubMed] [Google Scholar]
- Monsivais P, Martin A, Suhrcke M et al. (2015) Job-loss and weight gain in British adults: evidence from two longitudinal studies. Soc Sci Med; 143: 223–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Münzel T, Gori T, Babisch W et al. (2014) Cardiovascular effects of environmental noise exposure. Eur Heart J; 35: 829–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Namazi S, Dugan AG, Fortinsky RH et al. (2019) Examining a comprehensive model of work and family demands, work-family conflict, and depressive symptoms in a sample of correctional supervisors. J Occup Environ Med; 61: 818–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute for Occupational Safety and Health. (2016). In Lee MP, Hudson H, Richards R, Chang CC, Chosewood LC, Schill AL, on behalf of the NIOSH Office for Total Worker Health , editor. Fundamentals of Total Worker Health® approaches: essential elements for advancing worker safety, health, and well-being. Cincinnati, OH: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health; DHHS (NIOSH) Publication No. 2017-112. Available at https://www.cdc.gov/niosh/docs/2017–112/pdfs/2017_112.pdf. Accessed 8 May 2019. [Google Scholar]
- National Institute for Occupational Safety and Health (2018a). What is Total Worker Health? Available at https://www.cdc.gov/niosh/twh/default.html. Accessed 8 May 2019.
- National Institute for Occupational Safety and Health (2018b). Hierarchy of controls applied to NIOSH Total Worker Health. Available at https://www.cdc.gov/niosh/twh/letsgetstarted.html. Accessed 8 May 2019.
- Nielsen KM. (2013) How can we make organizational interventions work? Employees and line managers as actively crafting interventions. Hum Relat; 66: 1029–50. [Google Scholar]
- Nobrega S, Champagne N, Abreu M et al. (2016) Obesity/overweight and the role of working conditions: a qualitative, participatory investigation. Health Promot Pract; 17: 127–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nobrega S, Kernan L, Plaku-Alakbarova B et al. ; CPH-NEW Research Team. (2017) Field tests of a participatory ergonomics toolkit for Total Worker Health. Appl Ergon; 60: 366–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyberg ST, Fransson EI, Heikkilä K et al. ; IPD-Work Consortium. (2013) Job strain and cardiovascular disease risk factors: meta-analysis of individual-participant data from 47,000 men and women. PLoS One; 8: e67323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyberg ST, Fransson EI, Heikkilä K et al. ; IPD-Work Consortium. (2014) Job strain as a risk factor for type 2 diabetes: a pooled analysis of 124,808 men and women. Diabetes Care; 37: 2268–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obidoa C, Reeves D, Warren N et al. (2011) Depression and work family conflict among corrections officers. J Occup Environ Med; 53: 1294–301. [DOI] [PubMed] [Google Scholar]
- Punnett L, Warren N, Henning R et al. ; CPH-NEW Research Team. (2013) Participatory ergonomics as a model for integrated programs to prevent chronic disease. J Occup Environ Med; 55 (12 Suppl.): S19–24. [DOI] [PubMed] [Google Scholar]
- Robertson MM, Henning RA, Warren N et al. (2015) Participatory design of integrated safety and health interventions in the workplace: a case study using the Intervention Design and Analysis Scorecard (IDEAS) tool. Int J Hum Factors Ergon; 3: 303–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider D, Harknett K (2019) It’s about time: how work schedule instability matters for workers, families, and racial inequality. The Shift Project Research Brief, October 2019 Available at https://shift.berkeley.edu/its-about-time-how-work-schedule-instability-matters-for-workers-families-and-racial-inequality/. Accessed 12 December 2019.
- Schulte PA, Cunningham TR, Nickels L et al. (2017) Translation research in occupational safety and health: a proposed framework. Am J Ind Med; 60: 1011–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulte PA, Pandalai S, Wulsin V et al. (2012) Interaction of occupational and personal risk factors in workforce health and safety. Am J Public Health; 102: 434–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skogstad M, Johannessen HA, Tynes T et al. (2016) Systematic review of the cardiovascular effects of occupational noise. Occup Med (Lond); 66: 500. [DOI] [PubMed] [Google Scholar]
- Sorensen G, Barbeau E (2012) Steps to a healthier U.S. workforce: integrating occupational health and safety and worksite health promotion: state of the science. In Research compendium: the NIOSH Total Worker Health™ Program: seminal research papers 2012. Washington DC: US Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, DHHS (NIOSH) Publication No. 2012-146. Available at https://www.cdc.gov/niosh/docs/2012–146/pdfs/2012–146.pdf. Accessed 8 May 2019. [Google Scholar]
- Sorensen G, McLellan D, Dennerlein JT et al. (2013) Integration of health protection and health promotion: rationale, indicators, and metrics. J Occup Environ Med; 55 (12 Suppl.): S12–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorensen G, McLellan DL, Sabbath EL et al. (2016) Integrating worksite health protection and health promotion: a conceptual model for intervention and research. Prev Med; 91: 188–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stave GM, Muchmore L, Gardner H (2003) Quantifiable impact of the contract for health and wellness: health behaviors, health care costs, disability, and workers’ compensation. J Occup Environ Med; 45: 109–17. [DOI] [PubMed] [Google Scholar]
- Strickland JR, Kinghorn AM, Evanoff BA et al. (2019) Implementation of the Healthy Workplace Participatory Program in a retail setting: a feasibility study and framework for evaluation. Int J Environ Res Public Health; 16: 590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strine TW, Kroenke K, Dhingra S et al. (2009) The associations between depression, health-related quality of life, social support, life satisfaction, and disability in community-dwelling US adults. J Nerv Ment Dis; 197: 61–4. [DOI] [PubMed] [Google Scholar]
- Tamers SL, Chosewood LC, Childress L et al. (2019) Total Worker Health® 2014–2018: the novel approach to worker safety, health, and well-being evolves. J Environ Res Pub Health; 16: 321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taouk Y, Spittal MJ, LaMontagne AD et al. (2020) Psychosocial work stressors and risk of all-cause and coronary heart disease mortality: a systematic review and meta-analysis. Scand J Work Environ Health; 46: 19–31. [DOI] [PubMed] [Google Scholar]
- Too LS, Leach L, Butterworth P (2019) Is the association between poor job control and common mental disorder explained by general perceptions of control? Findings from an Australian longitudinal cohort. Scand J Work Environ Health 2019; e-pub ahead of print 05 December 2019. doi:10.5271/sjweh.3869 [DOI] [PubMed] [Google Scholar]
- Virtanen M, Koskinen S, Kivimäki M et al. (2008) Contribution of non-work and work-related risk factors to the association between income and mental disorders in a working population: the Health 2000 Study. Occup Environ Med; 65: 171–8. [DOI] [PubMed] [Google Scholar]
- von Thiele Schwarz U, Augustsson H, Hasson H et al. (2015) Promoting employee health by integrating health protection, health promotion, and continuous improvement: a longitudinal quasi-experimental intervention study. J Occup Environ Med; 57: 217–25. [DOI] [PubMed] [Google Scholar]
- Wahrendorf M, Hoven H, Goldberg M et al. (2019) Adverse employment histories and health functioning: the CONSTANCES study. Int J Epidemiol; 48: 402–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waynforth D. (2018) Unstable employment and health in middle age in the longitudinal 1970 British Birth Cohort Study. Evol Med Public Health; 2018: 92–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weil D. (2014) The fissured workplace: why work became so bad for so many and what can be done to improve it. Cambridge MA: Harvard University Press; ISBN 0 470 02725 8. [Google Scholar]
- World Health Organization (2010) Healthy workplaces: a model for action: for employers, workers, policymakers and practitioners. Geneva, Switzerland: World Health Organization; ISBN 978 92 4 159931 3 Available at https://apps.who.int/iris/handle/10665/44307. Accessed 8 May 2019. [Google Scholar]
- Zhang Y, Flum M, Nobrega S et al. (2011) Work organization and health issues in long-term care centers: comparison of perceptions between caregivers and management. J Gerontol Nurs; 37: 32–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Punnett L, Gore R; CPH-NEW Research Team (2014) Relationships among employees’ working conditions, mental health, and intention to leave in nursing homes. J Appl Gerontol; 33: 6–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Punnett L, McEnany GP et al. (2016) Contributing influences of work environment on sleep quantity and quality of nursing assistants in long-term care facilities: a cross-sectional study. Geriatr Nurs; 37: 13–8. [DOI] [PMC free article] [PubMed] [Google Scholar]