Abstract
Heavy Episodic Drinking (HED) and depressive symptoms often co-occur among college students and are associated with significant impairment. However, evidence-based treatments for these common co-occurring conditions are not available for college students. The current study compared the effectiveness of a treatment combining Cognitive-Behavioral Therapy for Depression and Brief Motivational Interviewing (CBT-D+BMI) versus Cognitive-Behavioral Therapy for Depression (CBT-D) alone among 94 college students with HED and depressive symptoms. Both treatment programs were associated with significant reductions of similar magnitude in HED, alcohol-related problems (ARP), and depressive symptoms at the end of treatment, and at the one-month follow-up assessment. Moderation analyses indicated that, among college students with fewer depressive symptoms at baseline, CBT-D was associated with greater sustained reduction in heavy drinking relative to CBT-D+BMI at the one-month follow-up. Although the study did not include a no-treatment condition, the magnitude of improvement during treatment in both groups was greater than what is expected with passage of time. Although clinicians in college counseling centers may lack specialty training for co-occurring conditions, CBT-D is widely implemented in college settings. Our findings suggest that CBT-D may reduce both depressive symptoms and HED in college students and may be used to address a significant public health problem.
Keywords: cognitive behavioral therapy, brief motivational interviewing, depression, heavy episodic drinking, alcohol-related problems, college student mental health
A recent survey by the Substance Abuse and Mental Health Services Administration (2015) indicated that approximately 39% of 18 to 25 year-olds in the US engage in heavy episodic drinking (HED), defined as consumption of 5 or more drinks in 2 hours for males and 4 or more drinks in 2 hours for females (NIAAA, 2004). HED among young adults is a behavior associated with elevated risk for physical injury, sexual and/or physical assault (Hingson et al., 2009), progression to alcohol/substance use disorders (Tubman et al., 1990), premature death (Kim et al., 2012), suicide (Barrios et al., 2000), poor school performance and higher college dropout risk with significant long-term effects (Arria et al., 2013).
Depression is also common among young adults in college. Between 7% to 20% of college students meet criteria for Major Depressive Disorder (MDD; Blanco et al., 2008; Eisenberg et al., 2013; Pedrelli et al., 2016). A considerable number of college students report co-occurring MDD and HED (Cranford et al., 2009; Pedrelli et al., 2016), and college students with depressive symptoms report more frequent HED and consuming more alcohol during a heavy drinking episode than their non-depressed peers (Pedrelli et al., 2016). Given that depressive symptoms and drinking to reduce negative affect among college students significantly increase the risk for short-term and long-term negative consequences (Acuff et al., 2018; Pedrelli et al., 2016), college students with HED and depressive symptoms represent a high-risk population.
A major challenge associated with reducing alcohol misuse in young adults is that most college students with HED do not consider their alcohol consumption concerning and only about 7%, seek treatment for it (Cranford et al., 2009). Conversely, approximately 40% of college students with depressive symptoms seek treatment for their symptoms (Eisenberg and Chung, 2012). Two-thirds of college students with depression and HED acknowledge needing help for their mental health, with more than half of them reporting having taken medications or having been in counseling for depression in the previous year (Cranford et al., 2009). Thus, many heavy drinking depressed students may receive treatment for their mood symptoms but not for their drinking. However, receiving treatment for only one class of symptoms may not lead to improvement due to the persistence of unaddressed symptoms. For example, among individuals with alcohol use disorders (AUDs), depressive symptoms may increase the risk of relapse (Cornelius et al., 2004) and alcohol consumption may prevent improvement of depressive symptoms (Pettinati, 2004).
While some evidence exists in support of treatments for adults with depression and alcohol misuse (Baker et al., 2010), to our knowledge, evidence-based treatments for HED and depressive symptoms among college students are not available. A few interventions have been examined for this population, but they have not been supported (Geisner et al., 2007, 2015). A combination of Brief Motivational Intervention (BMI) and Cognitive Behavioral Therapy for depression (CBT-D) seems potentially useful for young adults with HED and depressive symptoms for several reasons. First, combined interventions have been recommended for co-occurring conditions (Baker et al., 2010). Second, while BMI has the strongest empirical support for reducing alcohol use and problems in college students (Carey et al., 2007), it has not demonstrated consistent efficacy with college students exhibiting depressive symptoms (Merrill et al., 2014). Third, several meta-analyses have shown that CBT-D is superior to wait-list and placebo control in the treatment of unipolar depression in adult patients as well as in young adults (Dobson et al., 1989; Huang et al., 2018). Finally, a meta-analysis showed that Motivational Interviewing plus CBT-D are effective for treating alcohol and depression among adults with comorbid symptoms (Riper et al., 2014).
The current study aimed to examine the feasibility and effectiveness of combined BMI and CBT-D to reduce HED, alcohol related problems (ARP), and depressive symptoms in heavy drinking college students with depressive symptoms. Many heavy drinking college students do not consider their alcohol consumption problematic, thus one of the study’s aims was to assess whether the drop-out rates and satisfaction with therapy in the CBT-D+BMI condition differed from standard CBT-D. Given that combined approaches have been shown to be feasible and effective for co-occurring conditions among adult patients, it was hypothesized that CBT-D+BMI would be well accepted and would lead to greater decreases in heavy drinking and ARP compared to CBT-D alone among college students with HED and depressive symptoms. Furthermore, given the delivery of a higher dosage of an efficacious CBT-D treatment, it was hypothesized that college students would experience greater reduction in depressive symptoms with the CBT-D condition compared to the CBT-D+BMI. We also examined moderators of treatment effects. It was hypothesized that (a) higher baseline depressive symptoms would be associated with greater reduction of HED and ARP in the CBT-D+BMI than in the CBT-D condition and (b) greater HED at baseline would be associated with a larger reduction in ARP and depressive symptoms with the CBT-D+BMI condition compared to CBT-D.
Methods
Procedure
Participants were recruited from colleges in the Boston area between November 2012 and May 2016 via self-referral and advertisements (i.e., online and on public transportation) describing the study as an evaluation of treatments for college students feeling down and/or sad and who were consuming four or five alcoholic drinks in a sitting. Interested individuals were screened for eligibility via a brief telephone interview which included standardized questions on mood and alcohol use. Those who reported depressed mood and HED were scheduled for an in-person screening visit that lasted up to 180 minutes and included informed consent, diagnostic interview, and baseline assessments. Eligible participants were randomized to receive eight in-person, individual sessions of CBT-D alone or CBT-D+BMI. The first follow-up assessment occurred at the end of the therapy sessions (posttreatment assessment), or approximately two months from baseline. The second follow-up (1-month follow-up) occurred one month from the posttreatment assessment or, if they did not complete the posttreatment assessment, three months from baseline. Participants were compensated $40 for the initial assessment, $30 for each follow-up assessment and received an additional $10 bonus at the end for completing of the study. Participants were not compensated for attending therapy sessions. All assessments and therapy visits were conducted at the Depression Clinical and Research Program at the Massachusetts General Hospital (MGH). Computer-generated randomized group assignments were placed in sealed envelopes and opened in sequence by the enrolling research coordinator as participants completed the in-person baseline assessment. Randomization was stratified by gender (male or female) and past month presence of cannabis consumption (yes or no). All study procedures were approved by the MGH Institutional Review Board.
Inclusion criteria were: (a) currently enrolled in college as an undergraduate student; (b) 18–24 years old (inclusive); (c) presence of at least one episode of HED in the past month; and (d) presence of at least mild-to-moderate but not severe depressive symptoms (scores between 10 and 30 on the Beck Depressive Inventory (BDI) Beck, Steer, & Garbin, 1988). Exclusion criteria included: (a) meeting diagnostic criteria for bulimia, psychosis, bipolar disorder, or illicit substance abuse or dependence in the past six months (alcohol abuse was allowed); (b) having received any psychosocial treatment for depression or substance dependence in the past month; (c) having received CBT-D for depression and/or alcohol use in the previous six months; (d) having discontinued or changed dosage on an antidepressant medication less than 1 month prior to screening; and/or (e) posing a serious suicide or homicide risk. Two participants who met criteria for alcohol dependence but did not wish to seek specialized treatment for their alcohol consumption and were not at risk for seizure were allowed to enroll in the study. Participants who had a BDI greater than 30 were encouraged to seek psychopharmacological treatment. Six participants with BDI scores greater than 30 who were not interested in psychopharmacological treatment and demonstrated the ability to maintain activities of daily living (i.e., attending classes, maintaining personal hygiene) were allowed to enroll in the study.
Participants
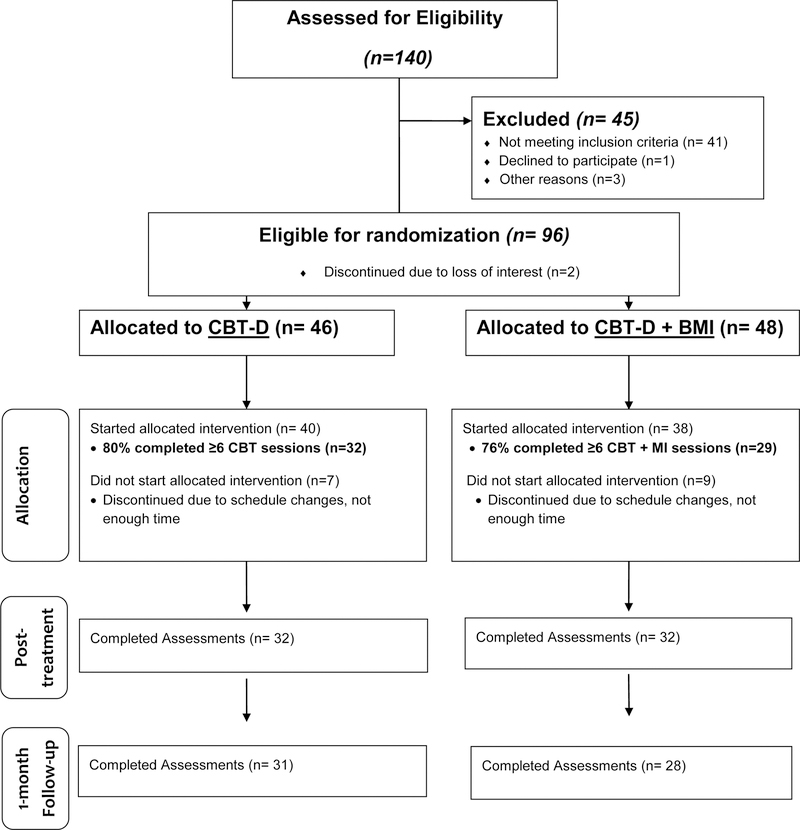
Participants included 94 undergraduate students attending 2- or 4-year colleges in the Boston area. Overall, 1,365 individuals completed a phone screen and 140 completed an in-person screening visit to determine study eligibility. Ninety-four were randomized to either CBT-D alone or CBT-D+BMI (Figure 1). Of the 94 participants who were randomized, the majority were women (68.1%), between 18 and 23 years old (M = 19.9 ± 1.4), who identified as White (54.3%) and non-Hispanic (82.1%). On average, study participants engaged in HED more than once per week (4.9 ± 3.5 past month) and had moderate depressive symptoms (BDI=19.5 ± 6.8) at screen (Table 1).
Figure 1.
Consort Table
Table 1.
Demographics and Clinical Variables of Participants at Baseline
| Total (N=94) M±SD; % | CBT-D (N=46) M±SD; % | CBT-D+BMI (N=48) M+SD; % | p | |
|---|---|---|---|---|
| Age | 19.9 ± 1.4 | 19.7 ± 1.4 | 20.1 ±1.2 | .202 |
| Gender | .457 | |||
| Male | 31.9% | 28.3% | 35.4% | |
| Female | 68.1% | 71.7% | 64.6% | |
| Ethnicity | .588 | |||
| Hispanic/Latino | 14.9% | 10.9% | 18.8% | |
| Not Hispanic/Latino | 82.1% | 87.0% | 81.3% | |
| Wish not to say | 1.1% | 2.2% | 0% | |
| Race | .348 | |||
| White | 54.3% | 60.9% | 47.9% | |
| Black/African American | 14.9% | 13.0% | 16.7% | |
| Asian | 19.1% | 19.6% | 18.8% | |
| Other | 11.7% | 6.5% | 16.7% | |
| Diagnosis | ||||
| MDD | 61.3% | 63.0% | 59.6% | .731 |
| GAD | 44.1% | 39.1% | 48.9% | .341 |
| Alcohol abuse | 15.1% | 21.7% | 8.5% | .074 |
| Alcohol dependence | 2.1% | 2.2% | 2.1% | .976 |
| Cannabis abuse | 5.4% | 4.3% | 6.4% | .664 |
| Eating Disorder | 5.4% | 6.5% | 4.3% | .646 |
| BDI score | 19.5 ± 6.8 | 19.2 ± 6.5 | 19.8 ± 7.1 | .673 |
| # of HED (past mo.) | 4.9 ± 3.5 | 4.7 ± 3.5 | 5.2 ± 3.6 | .520 |
| ARP (past mo.) | 5.6 ± 4.2 | 6.0 ± 4.7 | 5.1 ± 3.8 | .325 |
Note: MDD=Major Depressive Disorder; GAD=Generalized Anxiety Disorders; BDI=Beck depressive Inventory; HED= Heavy Episodic Drinking; ARP=Alcohol related problems
Power Analysis
The sample size was chosen on the bases of a power analyses conducted with the software G*Power (Faul et al., 2007) prior to study initiation. We estimated that a total of 94 participants in a repeated within-between 3×2 ANOVA, provided adequate statistical power (0.89) to detect a small to medium effect size f=0.15 (Cohen’s convention; Cohen, 1977), assuming a correlation of 0.5 and with a two-sided alpha of .05. An effect size of f=0.15 represents an intermediate point between Cohen’s d small and medium (d=.20 and d=.50, respectively) effect sizes for ANOVA (i.e., f=.10 and f=.25, respectively) and was chosen on the bases of previous studies. A small effect size has been observed for the effectiveness of MI in reducing alcohol use among college students (Carey et al., 2007) and a small to medium effect size has been observed for the effectiveness of MI added to CBT relative to CBT alone for reducing alcohol use among adults (d=0.30; Baker et al., 2010).
Measures
Diagnoses.
The Structured Clinical Interview for DSM-IV Axis I disorder (SCID-IV; First et al., 1997) was used to assess presence of psychiatric disorders. The SCID-IV is a semi-structured, clinician administered interview designed to assess current and lifetime diagnoses.
Depressive Symptoms.
The Beck Depression Inventory (BDI; Beck, 1961) is a 21-item self-report measure of depressive symptoms. Responses to the items range from 0 to 3, and total score ranges from 0 to 63, with higher scores indicating greater severity of symptoms. The BDI was also administered at the beginning of each therapy visit to monitor patients’ suicidality.
Alcohol Use.
The Alcohol Timeline Followback (TLFB; Sobell and Sobell, 1979) is an instrument designed to assess daily alcohol consumption in both clinical and non-clinical populations. The TLFB prompts subjects to report retrospective estimates of daily drinking over a specified period of time while using a calendar to enhance recall. Frequency of HED in the previous thirty days was computed on the bases of the TLFB.
A single question was used to ask frequency of HED in the previous month to determine eligibility to the study.
Alcohol-Related Problems.
The Brief Young Adult Alcohol Consequences Questionnaire (B-YAACQ; Kahler et al., 2005) assesses various domains of alcohol-related problems over the past thirty days. The B-YAACQ has shown good internal consistency and high concurrent validity with other established measures of alcohol consumption (Kahler et al., 2008).
Satisfaction and Feasibility.
Participants who attended therapy completed the Client Satisfaction Questionnaire (CSQ; Larsen et al., 1979, Nguyen et al., 1983) at the end of treatment. The CSQ includes seven items inquiring about likability and satisfaction with a treatment received. Items are rated on a 4-point Likert scale, with higher scores indicating higher satisfaction. CSQ total score can range from seven to twenty-eight. The CSQ has good test retest reliability, internal consistency, and sensitivity to treatment (Nguyen et al., 1983). In the current sample, internal consistency was high (.89). The CSQ was used to assess feasibility of the treatment programs. Number of sessions attended was also considered a measure of feasibility.
Interventions
Sessions for both interventions were 50–60 minutes long. A treatment manual was developed for each intervention and both treatment protocols targeted developmental problems common to college students, (e.g., academic pressures). Although standard CBT-D protocols with adults are 12 to 16 weeks long, support for the choice of eight sessions was based on research indicating that individuals with mild-to-moderate depressive symptoms may improve with brief CBT-D interventions (Brown et al., 1997; Nyer et al., 2015; Seligman et al., 2007).
CBT-D+BMI.
The CBT-D + BMI manual described CBT for depression treatment while integrating Motivational Interviewing (MI; Miller & Rollnick, 1991) which is defined as a clientcentered, directive clinical method that is designed to enhance intrinsic motivation to change by exploring and resolving ambivalence through the evocation and strengthening of client change talk (or personal argument for change; Miller & Rollnick, 1991; Miller & Rose, 2009). BMI content. The alcohol-focused content was based on the Brief Alcohol Screening and Intervention for College Students (BASICS) program, which has been effective in reducing alcohol use and alcohol problems (Dimeff at al., 1999; Marlatt et al., 1998). Specifically, session one reviewed psychoeducation of depression and the CBT-D model. Session two reviewed a Personalized Feedback Form (PFF) that included a description of the participants’ alcohol use, a comparison of their use with normative consumption, education about blood alcohol concentration, and a list of alcohol-related consequences they endorsed at the screening visit. Participants’ reactions to the information provided and to the relationship between their alcohol use and their depressive symptoms were explored using MI. Session three reviewed alcohol use during the previous week, the PFF from session two and cognitive distortions; session four reviewed goals of treatments and techniques to identify alternative balanced thoughts; session five focused on behavioral activation; session six reviewed relaxation strategies; session seven focused on practicing cognitive restructuring; and session eight reviewed progress and relapse prevention strategies. In the CBT-D+BMI program, reduction of alcohol use was explored as being one of the possible goals for treatment due to its association with mood symptoms. Throughout the CBT-D+BMI protocol, clinicians used MI-consistent skills such as open-ended questions, affirmations, reflective listening to evoke and strengthen the participants change talk.
CBT-D.
The CBT-D alone sessions reviewed the same topics covered in the CBT-D+BMI program with the exclusions of reviewing drinking behaviors and the PFF. Alcohol use was discussed only if the patient was interested in reviewing the topic. When discussing alcohol use, the conversation was limited to providing education, and evocation or strengthening of change talk was not facilitated during the CBT-D sessions. Instead, therapists were instructed to use the technique of Socratic questioning which is used in CBT to facilitate personal exploration of personal thoughts and behaviors and make unique realizations or insight (a process also called guided discovery).
Therapists and Treatment Fidelity
A total of 5 therapists (4 females and 1 male; all White) delivered treatment. Two of the therapists were licensed clinical psychologists, one was a postdoctoral fellow, and two were advanced clinical psychology doctoral students with a Master’s degree. All therapists had previous experience with the administration of CBT and all received training from the principal investigator (first author) in the delivery of BMI. To ensure competent provision of the treatments, all therapists received a minimum of 6 hours of training on BMI techniques and on how to best deliver the treatment protocols. The postdoctoral fellow and the doctoral students in clinical psychology received weekly supervision from the principal investigator during which audiotaped sessions were reviewed. The principal investigator monitored and ensured adherence to the treatment manuals by listening to part of the audiotaped sessions prior to conducting supervision and by providing feedback. To examine whether satisfaction differed among participants who received therapy from less experienced therapists, a series of t-tests were performed to compare the CSQ scores of participants who received therapy by the study investigator (first author) and those who were administered therapy by the other clinicians. No significant differences were found between participants who received therapy from the PI and those who were administered therapy by the other therapists on the CSQ total score (all ps>.05).
Data Analysis Plan
Feasibility of CBT-D+BMI relative to CBT-D was examined by conducting t-test analyses comparing number of sessions attended and CSQ total scores among participants in the two conditions. To test our CBT-D+BMI effectiveness relative to CBT-D, hierarchical linear models (HLM) were run using the HLM 7.01 program (Raudenbush, Bryk, & Congdon, 2013). Analyses relied on intent-to-treat principles, with 94 participants randomized to treatment conditions (one participant was missing baseline data on two of three outcomes and dropped). Therefore, the person-period data set was represented by 279 possible observations (N=93 participants*3 assessments). Primary outcomes were HED, alcohol related problems and BDI total scores, and their distributions were normal. Due to the flexibility of HLM in handling missing data at the within-person level, we could retain for analysis any of the remaining participants that contributed at least one assessment. Data were available for a total of 217 HED assessments, 192 measures of alcohol problems, and 215 BDI assessments-out of 279 assessment points (69–78%). All models were run with full maximum likelihood estimation.
Fully unconditional HLM models (i.e., no predictors) were run first, in order to determine intraclass correlations (ICCs) for outcomes, which provides information on the percentage of variation in each outcome at the between-person level vs within person. Next, in order to run piecewise models that adequately reflected timing of assessments, two-time component variables were created and added at Level 1. The first, allowing for a test of change between baseline and follow-up assessments, coded the three time points (baseline, posttreatment assessment, 1-month follow-up) as follows: baseline=0, posttreatment assessment =number of months (in decimals) since baseline at the posttreatment assessment, 1-month follow-up=0. The second, allowing for a test of change between baseline and the 1-month follow-up, coded the three time points as follows: baseline=0, posttreatment assessment=0, 1-month follow-up =number of months since baseline at 1-month follow-up. To test main effects, condition (0=CBT-D, 1= CBT-D+BMI) was added at Level 2 as a predictor of the intercept (i.e., effect of group on the outcome at baseline) and both time effects (i.e., effect of group on the outcome at posttreatment and at 1-month follow-up).
In each model, we also examined whether baseline depressive symptoms and/or HED frequency differentially affected outcomes in the two conditions. Specifically, we examined baseline HED as a putative moderator of the effect of condition on both alcohol problems and BDI, and baseline BDI as a moderator of the effect of condition on both HED and alcohol problems. These interaction tests were conducted by including the moderator and interaction term as additional predictors of the intercept and both time components. Prior to creating interaction terms, continuous predictors were mean-centered and we used effects coding for categorical predictors (e.g., condition) in order to interpret intercept effects at average levels of predictors and collapsing across both groups. Significant interactions were probed at one standard deviation above and below the mean on the moderator (Aiken & West, 1991). In reporting model results, we relied on robust standard errors. All intercept and slope effects were initially specified as random, to allow for individual variation in baseline levels and change over time in the outcomes; however, in one case, the slope was fixed due to non-significant variance (i.e., posttreatment slope in the prediction of HED, both follow-up slopes in prediction of alcohol problems). Of note, as a sensitivity test, models for all outcomes described above were also run without inclusion of interaction effects.
Data analyses for clinical change.
To ensure that the hypothesized change in depressive symptoms was not due to measuring error, the Jacob and Truax (1991) procedure for calculating reliable change in depressive symptoms was computed. This procedure is recommended as a standard reporting strategy for all published research involving psychological interventions (Evans et al., 1998). Reliable change indicates that the change is not due to measuring error, and the Reliable Change Index (RCI) is an indication that the change is clinically significant. Specifically, reliable change consists in a pre-to post-treatment improvement in scores that is unlikely due to the inherent unreliability of the measure. The RCI cut off was calculated using the following formula: 1.96× √ 2(SDpre√1−α) 2, where SDpre represents the measure total score standard deviation at baseline and α represents the scale reliability. To calculate reliable significant change criteria for our study, we used the BDI standard deviation of our sample (6.81) and the reliability estimate (Cronbach’s alpha, α) of our data (0.77) and a reliable change cut-off of 9 was computed. Hence, a reliable change was considered any change of ≥9 BDI points. Importantly, our reliable BDI change cut-off was the same found by others (Busch et al., 2013). We categorized participants as experiencing a reliable improvement in depression (≥ 9 BDI point decrease), a reliable worsening of depression (≥ 9 BDI point increase), and no reliable change (< 9 point change in either direction). We also examined the number of participants who recovered, defined as reaching a BDI lower than 10 at each follow-up in each group (Beck, Steer, and Garbin 1988). Chi-squared tests were used to test differences between the two conditions in proportion of participants who recovered at each follow-up and who experienced reliable change. Effect sizes for the BDI, HED, and ARP at each follow-up were computed consistent with Cohen’s d statistic formula: (Mean2-Mean1)/SDpooled.
Results
Sample Characteristics
T-tests (not accounting for the multilevel nature of the data) did not reveal any significant group differences in the outcomes (HED, ARP, BDI) at any time point. There were no differences between treatment groups in number of days between baseline and posttreatment assessment and between posttreatment assessment and the 1-month follow-up (both ps > .30). Average number of days between baseline assessment and the posttreatment assessment was 81.88 ± 24.84 and between posttreatment assessment and the 1-month follow-up was 37.25 + 12.60. Groups also did not differ on age, gender, race, or ethnicity (Table 1). However, there were significantly more first year college students in the CBT-D than the CBT-D+BMI group (χ2 = 10.50, p=.03). As such, all models control for year in school. With respect to attrition bias, the number of follow-ups completed was not significantly related to treatment condition, age, gender, race, ethnicity, year in school, or any of the outcome variables (all p values >.22). The intraclass correlation coefficient (ICC) for HED was .49, indicating that 49% of the variability in HED was due to between-person differences, while 51% was due to within-person variability across time points. The ICCs for alcohol problems and depression were .35 and .38, respectively. In all cases, adequate variability at both the between- and within-person levels suggested that multilevel modeling was appropriate.
Treatment feasibility and satisfaction
On average, participants attended 5.4 (SD=3.4) sessions and 64% attended at least 6 sessions. Approximately 68% of the participants completed the posttreatment assessment and 63% completed the 1-month posttreatment follow-up. There were no differences between participants who received CBT-D and CBT-D+BMI in number of sessions attended (CBT-D=5.6 ± 3.3 sessions; CBT-D+BMI=5.4 ± 3.4 sessions; t(1,92)=.31, p=.76). Participants in both CBT-D and CBT-D+BMI rated the quality of the service received as high (24.77±3.68; 26.03±2.18, respectively), and there were no difference in treatment satisfaction between participants in the conditions (t(1,59)=2.68; p=.11).
Primary Outcome Models: Testing Group Effects and Moderators
Heavy episodic drinking (past month).
Results of the model predicting HED are shown in Table 2. The intercepts of change in HED from baseline to posttreatment (B= −0.66, p<.001) and baseline to 1-month follow-up (B=−0.64, p<.001) indicate significant reductions in HED at average levels of BDI and collapsing across both groups. There was no significant effect of treatment condition on change in HED at either follow-up, which indicates participants in both conditions reported a significant reduction in HED over time.
Table 2.
Hierarchical model predicting heavy episodic drinking
| Fixed Effect | B | SE | t | p |
|---|---|---|---|---|
| Baseline HED | ||||
| Intercept | 3.28 | 0.63 | 5.19 | <0.001 |
| Year in School | 0.64 | 0.24 | 2.64 | 0.010 |
| BDI | 0.06 | 0.06 | 1.02 | 0.309 |
| Condition | 0.14 | 0.70 | 0.20 | 0.844 |
| Condition x BDI | −0.04 | 0.12 | −0.35 | 0.730 |
| Change from Baseline to Posttreatment | ||||
| Intercept | −0.66 | 0.11 | −5.89 | <0.001 |
| BDI | 0.00 | 0.02 | 0.17 | 0.864 |
| Condition | −0.12 | 0.22 | −0.53 | 0.605 |
| Condition x BDI | 0.00 | 0.03 | 0.08 | 0.936 |
| Change from Baseline to 1-month Follow-up | ||||
| Intercept | −0.64 | 0.14 | −4.55 | <0.001 |
| BDI | −0.05 | 0.02 | −1.33 | 0.187 |
| Condition | 0.38 | 0.28 | 1.35 | 0.180 |
| Condition x BDI | −0.09 | 0.04 | −2.06 | 0.042 |
Note: BDI=Beck Depression Inventory, HED= Heavy Episodic Drinking
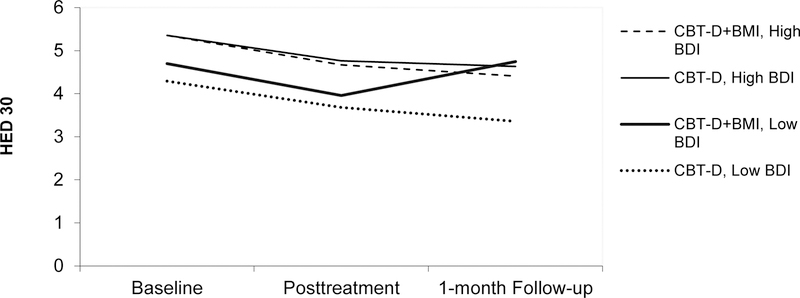
There was a significant condition x depression interaction on change in HED between baseline and the 1-month follow-up. Probing this interaction revealed that participants with high levels of depressive symptoms experienced reductions in HED of similar magnitude in both conditions, at both follow-ups (B=−.22, p=.51) (see Figure 2). At lower levels of depressive symptoms, participants in the two conditions experienced reductions in HED of similar magnitude at the posttreatment assessment but not at the 1-month follow-up. Specifically, at the 1-month follow-up, participants in the CBT-D condition continued to lower their alcohol use while those in the CBT-D+BMI condition slightly increased their HED (relative to the CBT-D group) (B=.97, p=.04).
Figure 2.
Heavy episodic drinking in the two conditions at high and low levels of depressive symptoms
Note: BDI=Beck Depression Inventory; HED= Heavy Episodic Drinking.
Alcohol Related Problems (past month).
Results of models examining differential effects on alcohol problems of the two conditions (one with HED and one with depression as a moderator of the effect of condition on problems) are presented in Table 3. In both models, the intercepts of change in ARPs from baseline to posttreatment and from baseline to 1-month follow-up indicate significant reductions in ARPs at average levels of either HED or BDI and collapsing across both groups. There was no significant effect of treatment condition on change in ARPs at either follow-up, suggesting that individuals in both groups reduced ARPs at a similar magnitude. Participants in both groups reported a significant reduction of ARPs at the posttreatment assessment as well as the 1-month follow-up.
Table 3.
Hierarchical models predicting alcohol problems
| Model testing | Condition and Condition x HED | Model testing | Condition and Condition x BDI | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Fixed Effect | B | SE | t | p | Fixed Effect | B | SE | t | p |
| Baseline Problems | |||||||||
| Intercept | 5.89 | 0.81 | 7.29 | <0.001 | Intercept | 4.93 | 0.84 | 5.88 | <0.001 |
| Year in School | −0.11 | 0.25 | −0.42 | 0.673 | Year in School | 0.29 | 0.26 | 1.09 | 0.279 |
| HED | 0.47 | 0.11 | 4.25 | <0.001 | BDI | 0.09 | 0.08 | 1.24 | 0.218 |
| Condition | −1.04 | 0.78 | −1.33 | 0.187 | Condition | −1.28 | 0.91 | −1.41 | 0.162 |
| Condition x HED | −0.19 | 0.22 | −0.86 | 0.391 | Condition x BDI | −0.21 | 0.16 | −1.38 | 0.172 |
| Change from Baseline to Posttreatment | |||||||||
| Intercept | −0.53 | 0.16 | −3.23 | 0.002 | Intercept | −0.48 | 0.19 | −2.51 | 0.014 |
| HED | −0.01 | 0.05 | −0.17 | 0.869 | BDI | −0.01 | 0.03 | −0.33 | 0.742 |
| Condition | 0.08 | 0 | 0.23 | 0.821 | Condition | −0.09 | 0.39 | −0.24 | 0.810 |
| Condition x HED | −0.22 | 0.10 | −2.20 | 0.030 | Condition x BDI | 0.01 | 0.06 | 0.23 | 0.822 |
| Change from Baseline to 1-month Follow-up | |||||||||
| Intercept | −0.61 | 0.17 | −3.60 | <0.001 | Intercept | −0.61 | 0.19 | −3.18 | 0.002 |
| BDI | −0.01 | 0.04 | −0.22 | 0.82 | BDI | −0.02 | 0.03 | −0.69 | 0.494 |
| Condition | 0.32 | 0.34 | 0.94 | 0.35 | Condition | 0.13 | 0.39 | 0.34 | 0.732 |
| Condition x HED | 0.13 | 0.08 | 1.50 | 0.14 | Condition x BDI | −0.05 | 0.06 | −0.90 | 0.373 |
Note: MDD= Major Depressive Disorder; GAD=Generalized Anxiety Disorders; BDI=Beck Depression Inventory; HED= Heavy Episodic Drinking; ARP=Alcohol Related Problems
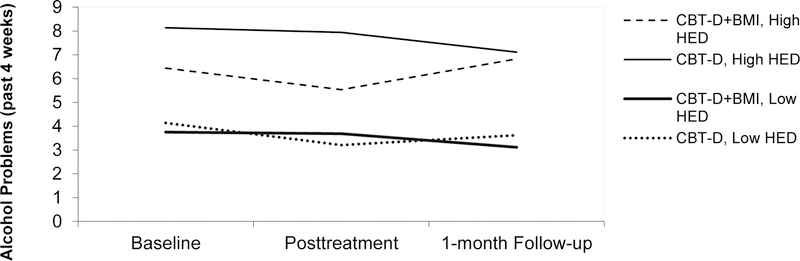
Inclusion of moderators of treatment effects in these models indicated that baseline depressive symptom severity did not interact with treatment condition in the prediction of change in ARPs. However, there was a significant interaction between baseline HED and treatment condition on change in ARPs between baseline and posttreatment (Table 3). Probing this interaction revealed that at high levels of baseline HED, there was a non-significant difference in ARPs between groups between baseline and 1-month follow up (B=−.71, p=.18) (Figure 3). At low levels of baseline HED, those in the CBT-D+BMI condition reported marginally smaller (B=.86, p=.07) reductions in alcohol problems (relative to CBT-D) at posttreatment.
Figure 3.
Alcohol related problems in the two conditions at high and low levels of HED
Note: HED= Heavy Episodic Drinking; ARP=Alcohol Related Problems.
Depression.
Results of the model predicting depression is shown in Table 4. The intercepts of change in depression from baseline to posttreatment and from baseline to 1-month follow-up indicated significant reductions in depression at average levels of HED and collapsing across both groups. There was no significant effect of treatment condition on change in depressive symptoms at either follow-up, suggesting that members of the CBT-D+BMI group experienced similar reductions in depression as those in the CBT-D group. There was no significant interaction between baseline HED and treatment condition on depressive symptoms.
Table 4.
Hierarchical model predicting depression
| Fixed Effect | B | SE | t | p |
|---|---|---|---|---|
| Baseline BDI | ||||
| Intercept | 18.27 | 1.68 | 10.88 | <0.001 |
| Year in School | 0.36 | 0.57 | 0.64 | 0.525 |
| HED | 0.20 | 0.22 | 0.92 | 0.360 |
| Condition | −0.06 | 1.32 | −0.04 | 0.966 |
| Condition x HED | −0.02 | 0.42 | −0.06 | 0.957 |
| Change from Baseline to Posttreatment | ||||
| Intercept | −3.05 | 0.34 | −9.00 | <0.001 |
| HED | 0.07 | 0.10 | 0.71 | 0.478 |
| Condition | 0.02 | 0.68 | 0.03 | 0.978 |
| Condition x HED | 0.08 | 0.21 | 0.38 | 0.709 |
| Change from Baseline to 1-month Follow-up | ||||
| Intercept | −3.21 | 0.33 | −9.69 | <0.001 |
| BDI | 0.08 | 0.09 | 0.83 | 0.407 |
| Condition | −0.59 | 0.66 | −0.90 | 0.373 |
| Condition x HED | −0.12 | 0.19 | −0.66 | 0.514 |
All the previous models were run without inclusion of interaction effects (between treatment condition and either HED or BDI), and effects of treatment group on outcomes remained non-significant.
Clinically Significant Change.
Table 5 illustrates rates of recovery, reliable improvement, no change, and worsening of depressive symptoms at the posttreatment assessment and at the 1-month follow-up by condition. No significant differences were found between the two conditions in rates of participants who experienced a reliable improvement posttreatment (χ2(1,63)=1.16, p=.56) and at the 1-month follow-up (χ2(1,63)=.49, p=.59) and in rates of recovery posttreatment (χ2(1,63)=.56, p=.62) and at the 1-month follow-up (χ2(1,56)=.13, p=.79). Table 6 illustrates effect sizes of the changes in symptom severity during the study. In both conditions, there were small to medium effect sizes for changes in HED posttreatment and at the 1-month follow-up. While at posttreatment small effect sizes in ARPs were found for both conditions, at the 1-month follow-up effect sizes for change in ARPs were of medium size in the CBT-D+BMI condition and of small size in the CBT-D condition (Table 6). Large effect sizes were present for changes in depressive symptoms from baseline to posttreatment and from baseline to the 1-month follow-up in both conditions.
Table 5.
Proportion of participants who recovered from depression and with reliable change.
| Conditions | Recovered (%) | Improved (%) | No Change (%) | Worsened (%) |
|---|---|---|---|---|
| Posttreatment | ||||
| CBT-D | 56.3 | 53.1 | 34.4 | 9.5 |
| CBT-D +BMI | 46.9 | 46.9 | 37.5 | 12.5 |
| 1-month Follow-up | ||||
| CBT-D | 56.7 | 50 | 43.3 | 10 |
| CBT-D +BMI | 51.9 | 59.3 | 33.3 | 7.4 |
Table 6.
Pre-Post Means (SD) and Effect sizes for the Outcome Variables
| CBT-D | CBT-D + BMI | |||||
|---|---|---|---|---|---|---|
| Mean ± SD | ES (d): Baseline to Posttreatment | ES (d): Baseline to 1-month Follow-Up | Mean ± SD | ES (d): Baseline to Posttreatment | ES (d): Baseline to 1-month Follow-Up | |
| BDI | ||||||
| Baseline | 19.2 ± 6.8 | 19.8 ± 7.1 | ||||
| Posttreatment | 10.8 ± 8.3 | 1.06 | 11.8 ± 8.9 | 1.05 | ||
| 1-month Follow-up | 10.7 ± 8.9 | 1.03 | 9.4 ± 5.6 | 1.72 | ||
| HED | ||||||
| Baseline | 4.7 ± 3.5 | 5.2 ± 3.6 | ||||
| Posttreatment | 3.1 ± 3.2 | 0.56 | 3.1 ± 2.9 | 0.64 | ||
| 1-month Follow-up | 2.3 ± 2.4 | 0.76 | 3.5 ± 3.8 | 0.33 | ||
| ARP | ||||||
| Baseline | 6.0 ± 4.7 | 5.1 ± 3.8 | ||||
| Posttreatment | 4.8 ±4.6 | 0.14 | 4.4 ± 3.7 | 0.26 | ||
| 1-month Follow-up | 4.2 ± 3.7 | 0.19 | 3.9 ± 3.5 | 0.43 | ||
Note: MDD= Major Depressive Disorder; GAD=Generalized Anxiety Disorders; BDI=Beck Depression Inventory; HED= Heavy Episodic Drinking; ARP=Alcohol Related Problems
Discussion
Although the CBT-D+BMI intervention examined heavy alcohol use, a topic young adults may not want to discuss, it was not associated with lower treatment satisfaction or lower adherence, suggesting that it is a feasible approach for this high-risk population. Contrary to study hypotheses, the combined intervention was not superior to CBT-D in reducing heavy drinking and alcohol problems. Notably, both conditions demonstrated significant reductions in heavy drinking with small to medium effect sizes, which are larger than those found in previous studies examining BMI. Two meta-analyses found that, among college students, BMI exerted a small short-term effect (<13 weeks) on frequency of HED relative to controls, ranging from d=0.16 to d=0.18 (Carey et al., 2007; Samson et al., 2015). Similarly, participants in both treatment programs reported significant reductions in alcohol problems corresponding with small to medium effect sizes.
The lack of an observed additional benefit of CBT-D+BMI on HED was consistent with previous research. An online BMI-based personalized feedback on alcohol use was not found to be effective among college students with depressive symptoms engaging in hazardous drinking (Geisner et al., 2007; 2015). In another study with college students, a BMI did not facilitate significant reductions in HED among depressed women in college (Merrill et al., 2014). Among adults, a study found that among patients receiving treatment for depression and reporting heavy drinking or drug use in the past 30 days, three sessions of MI were not more effective in reducing alcohol use than providing printed information about alcohol and drug use (Satre et al. 2016). Moreover, the addition of MI was not associated with better outcomes for depression. Another study with an adult sample examining combined treatments presented mixed results. At the 15-week follow-up, integrated MI+CBT treatment was associated with greater alcohol reduction than a single focused CBT treatment (Baker et al., 2010), but the beneficial effect of the integrated treatment was no longer present at the 18-week follow-up (Baker et al., 2014).
Findings from the present study and previous research may differ from reports showing that combined treatments are better for co-occurring AUD and MDD for several reasons. Individuals engaging in heavy drinking have less severe symptoms relative to individuals with AUDs, including lesser loss of control and cravings, and hence may drink for different reasons. Individuals with more severe AUD may improve when receiving MI because they may benefit from additional skills to reduce alcohol use. Individuals with AUD may have experienced more severe negative consequences than heavy drinking college students, and MI may be helpful in increasing their readiness to reduce alcohol use. Thus, BMI or MI may exert an additional effect on alcohol misuse and/or depression among individuals with depressive symptoms and AUD but not HED.
One of the primary goals of BMI is to facilitate readiness to change behavior (e.g., lower alcohol use) by highlighting the discrepancy between goals (e.g., getting good grades, being healthy) and current behavior (e.g., engaging in heavy drinking instead of studying, going to the gym). BMI may have not provided additional benefits to college students because they may have not experienced enough dissonance between their goals and their drinking behavior. In our sample, participants reported a lower number of ARPs compared to other studies examining the effectiveness of BMI for HED (Borsari and Carey, 2005; Murphy et al., 2012). College students with fewer alcohol-related problems and less frequent HED may be less concerned about their drinking behavior and thus less interested in changing it. As the degree of aversiveness of ARPs predicts change in drinking behavior (Barnett et al., 2014; Qi et al., 2014), the college students in our study may have not found their problems aversive enough to reduce personal alcohol use. Participants assigned to CBT-D received a higher dosage of behavioral activation, instead of BMI, which may have helped to identify alternative behaviors to drinking and facilitated reduction of HED and ARPs.
No significant differences between the two treatments were found in reduction of depressive symptoms at the two follow-up assessments. It is noteworthy that the reduction in depressive symptoms in both conditions corresponded to large effect sizes, which is greater than a recent meta-analysis of psychosocial treatments for mental health problems among college students that documented a medium effect size for CBT-D (Hedge’s g=−0.59, 95% CI:0.72—0.45; Huang et al., 2018). In addition, approximately half of the participants in both treatment groups were no longer depressed and experienced clinically reliable change at the two follow-ups even though the treatment protocol was relatively short compared to most standardized CBT-D treatment protocols (e.g., 12 or 16 weeks with 2 or more sessions per week; see Cuijpers et al., 2013). Hence, identifying short and effective interventions may be critical for this population.
Differences between the two treatment programs emerged when we examined the role of baseline symptoms. For example, among participants with fewer depressive symptoms, the two treatments were associated with equal improvement at posttreatment, but at the one-month follow-up, CBT-D was associated with a greater preservation of reduction in HED relative to CBT-D+BMI. Hence, long-term, college students with lower depressive symptoms benefitted more from CBT-D and did not gain from the additional BMI module. Conversely, participants with higher baseline depressive symptoms reduced the frequency of HED at a similar magnitude in the two treatments at both two follow-ups. Baseline severity of heavy drinking did not have an effect on the efficacy of the two treatment programs on depressive symptoms as well as alcohol problems. Specifically, college students in both treatment programs experienced reductions in depressive symptoms as well as ARP of similar magnitude, independent from baseline HED. Future studies may further investigate whether CBT-D and CBT-D+BMI are more effective for college students with more or less severe heavy drinking.
Several theoretical models may help explain our findings of reduced HED as well as ARPs in the context of CBT-D. The motivational model describes alcohol consumption as a strategy to cope with negative affect and regulate mood (Cooper et al., 1995). As depressive symptoms improved in the context of receiving CBT-D, participants may have engaged in less drinking to cope with their symptoms and consequently also experienced a reduction of ARPs. The behavioral economic theory conceptualizes alcohol misuse as reinforcer pathology, where there is a pattern of persistent overvaluation of the immediate rewards associated with substance use despite the experience of delayed health and social problems, in spite of engaging in other activities with delayed rewards (Bickel et al., 2011). In our study, CBT-D content focused on identifying goals for treatment (e.g., have a high GPA, have healthy relationships), which may have been incompatible with heavy drinking. Consistently, a previous study found that a behavioral economic intervention focused on reducing alcohol use by increasing saliency of long-term goals was efficacious in reducing ARPs as well as HED among college students with depressive symptoms (Murphy et al., 2012). Moreover, consistent evidence showed that drinking to cope mediates the association between depression and alcohol problems (Pedrelli et al., 2016b). These treatments may have provided strategies to cope with distress as alternatives to drinking.
The current study’s findings should be considered in the context of some limitations. Self-report assessments may be associated with biases. However, there is little indication that college students misrepresent alcohol use or other problems when confidentiality is clearly explained (Borsari and Muellerleile, 2009). The lack of a condition where participants did not receive any treatment does not allow us to discern whether changes were due to the treatment or passage of time. Outcomes were only measured at the end of treatment and at one month after completing treatment. Therefore, it is unknown whether the positive outcomes associated with the treatments would be sustained over the long-term. When interpreting the results and evaluating the generalizability of our findings, it is important to consider the possible presence of a selection bias and the fact that approximately one third of participants did not complete the study. The absence of objective assessments of therapists’ adherence to the treatments did not allow the determination of whether the lack of differences between conditions was due to low adherence or treatment contamination. Treatment satisfaction was reported primarily by participants who completed treatment (93.4%), thus results about satisfactions may not be generalizable to those who did not complete the program. Finally, level of experience of trainee may have affected the outcome.
In sum, college students with HED and depressive symptoms may benefit from a brief course of CBT-D or CBT-D+BMI. In cases where college students have fewer depressive symptoms and reduction of heavy drinking is the primary goal of treatment, CBT-D may be a good option because reduction of heavy drinking may persist for a longer period. Given the lack of clinicians trained in multiple treatment models (i.e., both BMI and CBT-D) in college counseling centers, the fact that CBT-D was associated with reduction of depressive symptoms as well as heavy drinking suggests that college students with depression may be encouraged to seek CBT-D treatment for their depressive symptoms because their alcohol use may decrease as well. Approximately half of the participants in both groups no longer reported significant depressive symptoms and reported a reliable improvement in depressive symptoms at the two follow-ups, highlighting the importance of providing standardized CBT-D to college students. Notably, while both treatments were associated with similar gains, they may have worked through different mechanisms. Future studies may be conducted to shed light into mechanisms contributing to reduction in alcohol use, alcohol problems, and depressive symptoms in the context of CBT-D and BMI.
Acknowledgements:
This study was supported by grants from the National Institute on Alcohol Abuse and Alcoholism (K23AA020064) to the first author Paola Pedrelli. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Alcohol Abuse and Alcoholism or the National Institutes of Health, the Department of Veterans Affairs, or the United States Government.
Research Support:
Acadia Pharmaceuticals, Allergan, Alkermes, Inc., Aptinyx, Avanir Pharmaceuticals Inc., Axsome, Benckiser Pharmaceuticals, Inc., Biogen, BioHaven, Cerecor, Johnson & Johnson, Lundbeck Inc., Marinus Pharmaceuticals, Methylation Sciences, Inc., Millennium Pharmaceutics, Inc. Minerva Neurosciences, Neuralstem, NeuroRX Inc., Novartis, Otsuka, Pfizer, Relmada Therapeutics Inc., Reckitt, Shenox Pharmaceuticals, Stanley Medical Research Institute (SMRI), Taisho, Takeda, Vistagen, National Institute of Drug Abuse (NIDA); National Institute of Mental Health (NIMH), and PCORI.
Dr. Fava has not done any personal consulting. Any consulting he has done has been on behalf of Massachusetts General Hospital.
Stock/Other Financial Options:
Equity Holdings: Compellis; Psy Therapeutics
Royalty/patent, other income: Patents for Sequential Parallel Comparison Design (SPCD), licensed by MGH to Pharmaceutical Product Development, LLC (PPD) (US_7840419, US_7647235, US_7983936, US_8145504, US_8145505); and patent application for a combination of Ketamine plus Scopolamine in Major Depressive Disorder (MDD), licensed by MGH to Biohaven. Patents for pharmacogenomics of Depression Treatment with Folate (US_9546401, US_9540691).
Copyright for the MGH Cognitive & Physical Functioning Questionnaire (CPFQ), Sexual Functioning Inventory (SFI), Antidepressant Treatment Response Questionnaire (ATRQ), Discontinuation-Emergent Signs & Symptoms (DESS), Symptoms of Depression Questionnaire (SDQ), and SAFER; Lippincott, Williams & Wilkins; Wolkers Kluwer; World Scientific Publishing Co. Pte.Ltd.
Footnotes
Publisher's Disclaimer: Disclaimer: This work was prepared while Benjamin G. Shapero was employed at the Massachusetts General Hospital / Harvard Medical School. The opinions expressed in this article are the author’s own and do not reflect the view of the National Institutes of Health, the Department of Health and Human Services, or the United States government.
Some of the data in this article were presented at the 40th Research Society on Alcoholism annual conference, Denver, Colorado.
Maurizio Fava:
Reports 3-year disclosures as below -
(All lifetime disclosures can be view on line at: http://mghcme.org/faculty/faculty-detail/maurizio_fava )
References
- Acuff SF, Soltis KE, Luciano MT, Meshesha LZ, Pedrelli P, Dennhardt AA, Murphy JG. Depressive symptoms as predictors of alcohol problems domains and reinforcement among heavy drinking college students. Psychol Addict Behav. 2018. November;32(7):792–799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken LS, & West SG. (1991). Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA US: Sage Publications, Inc. [Google Scholar]
- Arria AM, Caldeira KM, Vincent KB, Winick ER, Baron RA, O’Grady KE. (2013). Discontinuous college enrollment: associations with substance use and mental health. Psychiatr Serv, 64(2), 165–72. doi: 10.1176/appi.ps.201200106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arria AM. Caldeira KM, Vincent KB, Winick ER, Baron RA, O’ Grady Baker AL, Kavanagh DJ, Kay-Lambkin FJ, Hunt SA, Lewin TJ, Carr VJ, Connolly J. (2010). Randomized controlled trial of cognitive behavioural therapy for coexisting depression and alcohol problems: short-term outcome. Addiction, 105(1), 87–99. [DOI] [PubMed] [Google Scholar]
- Baker AL, Kavanagh DJ, Kay-Lambkin FJ, Hunt SA, Lewin TJ, Carr VJ, & Connolly J. (2010). Randomized controlled trial of cognitive-behavioural therapy for coexisting depression and alcohol problems: Short-term outcome. Addiction, 105, 87–99. 10.1111/j.1360-0443.2009.02757.x [DOI] [PubMed] [Google Scholar]
- Baker AL, Kavanagh DJ, Kay-Lambkin FJ, Hunt SA, Lewin TJ, Carr VJ, McElduff P. (2014). Randomized controlled trial of MICBT for co-existing alcohol misuse and depression: outcomes to 36-months. J Subst Abuse Treat, 46(3), 281–90. [DOI] [PubMed] [Google Scholar]
- Baker AL, Thornton LK., Hiler S., Hides L., Lubman DI. Psychological interventions for alcohol misuse among people with co-occurring depression or anxiety disorders: a systematic review. J Affect Disord. 2012. August;139(3):217–29. doi: 10.1016/j.jad.2011.08.004. [DOI] [PubMed] [Google Scholar]
- Barnett NP, Clerkin EM, Wood M, et al. (2014). Description and predictors of positive and negative alcohol-related consequences in the first year of college. J Stud Alcohol Drugs, 75, 103–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrios LC, Everett SA, Smon TR, Brener ND. (2000). Suicide ideation among US college students. Associations with other injury risk behaviors. J Am Coll Health, 48(5), 229–33. [DOI] [PubMed] [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. (1961). An inventory for measuring depression. Archives of General Psychiatry, 4, 53–61. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Garbin MG. (1988). Psychometric properties of the Beck Depression Inventory Twenty-five years of evaluation. Clin. Psych. Review, 8, 77–100. [Google Scholar]
- Bickel WK, Jarmolowicz DP, Mueller ET, Gatchalian KM. (2011). The behavioral economics and neuroeconomics of reinforcer pathologies: implications for etiology and treatment of addiction. Curr Psychiatry Rep, 13, 406–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanco C, Okuda M, Wright C, Hasin DS, Grant BF, Liu SM, Olfson M. (2008). Mental health of college students and their noncollege-attending peers: Results from the National Epidemiologic Study on Alcohol and Related Conditions. Archives of General Psychiatry, 65, 1429–1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsari B, & Carey KB. (2005). Two brief alcohol interventions for mandated college students. Psychology of Addictive Behaviors, 19, 296–302. 10.1037/0893-164X.19.3.296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsari B, Muellerleile P. (2009). Collateral reports in the college setting: a meta-analytic integration. Alcohol Clin Exp Res 33(5):826–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown AR, Evans DM, Miller WI, Burgess SE, Muelle IT. (1997). Cognitive-Behavioral Treatment for Depression in Alcoholism. J Consult Clin Psychol, 5, 715–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Busch AM, Whited MC, Appelhans BM, Schneider KL, Waring ME, DeBiasse MA, … Pagoto SL. (2013). Reliable change in depression during behavioral weight loss treatment among women with major depression. Obesity (Silver Spring), 21(3), E211–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Scott-Sheldon LA, Carey MP, DeMartini KS. (2007). Individual-level interventions to reduce college student drinking: a meta-analytic review. Addict Behav, 32(11), 2469–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. (1977). Statistical power analysis for the behavioral sciences, revised edition. New York: Academic Press. [Google Scholar]
- Cooper ML, Frone MR, Russell M, Mudar P. (1995). Drinking to regulate positive and negative emotions: A motivational model of alcohol use. Journal of Personality and Social Psychology, 69, 990–1005. [DOI] [PubMed] [Google Scholar]
- Cornelius R, Maisto AS, Martin SC, Bukstein GO, Salloum MI, Daley CD, Wood DS, Clark BD. Major depression associated with earlier alcohol relapse in treated teens with AUD. Addict Behav. 2004; 29 (5), 1035–1038. [DOI] [PubMed] [Google Scholar]
- Cranford JA, Eisenberg D, Serras AM. (2009). Substance use behaviors, mental health problems, and use of mental health services in a probability sample of college students. Addict Behav, 34(2), 134–45. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Berking M, Andersson G, Quigley L, Kleiboer A, Dobson KS. A meta-analysis of cognitive-behavioural therapy for adult depression, alone and in comparison with other treatments. Can J Psychiatry. 2013. July;58(7):376–85. [DOI] [PubMed] [Google Scholar]
- Dimeff LA, Baer JS, Kivlahan DR, Marlatt GA. (1999). Brief alcohol screening and intervention for college students (BASICS): A harm reduction approach. New York: Guilford Press. [Google Scholar]
- Dobson KS. et al. (1989). A meta-analysis of the efficacy of cognitive therapy for depression. J Consult Clin Psychol, 57(3), 414–9. [DOI] [PubMed] [Google Scholar]
- Eisenberg D, Chung H. (2012). Adequacy of depression treatment among college students in the United States. Gen Hosp Psychiatry, 34(3), 213–20. [DOI] [PubMed] [Google Scholar]
- Evans C, Margison F, & Barkham M. (1998). The contribution of reliable and clinically significant change methods to evidence-based mental health. Evidence-Based Mental Health, 1, 70–72. [Google Scholar]
- Faul F, Erdfelder E, Lang A-G, & Buchner A. (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39, 175–191. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Williams JBW, and Gibbon M. (1995). Structured Clinical Interview for DSM-IV. American Psychiatric Press, Washington, DC. [Google Scholar]
- Geisner IM, Neighbors C, Lee CM, Larimer ME. (2007). Evaluating personal alcohol feedback as a selective prevention for college students with depressed mood. Addictive Behaviors, 32, 2776–2787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geisner IM, Varvil-Weld L, Mittmann AJ, Mallett K, Turrisi R. (2015). Brief web-based intervention for college students with comorbid risky alcohol use and depressed mood: does it work and for whom? Addict Behav, 42, 36–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hingson RW, Zha W, Weitzman ER. (2009). Magnitude of and trends in alcohol-related mortality and morbidity among U.S. college students ages 18–24, 1998–2005. J Stud Alcohol Drugs Suppl, 16, 12–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang J, Nigatu YT, Smail-Crevier R, Zhang X, Wang J. (2018). Interventions for common mental health problems among university and college students: A systematic review and meta-analysis of randomized controlled trials. J Psychiatr Res, 107, 1–10. doi: 10.1016/j.jpsychires.2018.09.018 [DOI] [PubMed] [Google Scholar]
- Jacobson NS & Truax P. (1991). Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J Consult Clin Psychol, 59(1), 12–9. [DOI] [PubMed] [Google Scholar]
- Kahler CW, Strong DR, Read JP. (2005). Toward efficient and comprehensive measurement of the alcohol problems continuum in college students: the brief young adult alcohol consequences questionnaire. Alcohol Clin Exp Res, 29(7), 1180–9. [DOI] [PubMed] [Google Scholar]
- Kahler CW, Hustad J, Barnett NP, Strong DR, & Borsari B. (2008). Validation of the 30-Day version of the Brief Young Adult Alcohol Consequences Questionnaire for use in longitudinal studies. Journal of Studies on Alcohol and Drugs, 69(4), 611–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim JY, Asrani SK, Shah ND, Kim WR, Schneekloth TD. (2012). Hospitalization for underage drinkers in the United States. J Adolesc Health, 50(6), 648–50. [DOI] [PubMed] [Google Scholar]
- Larsen DL, Attkisson CC, Hargreaves WA, Nguyen TD. (1979). Assessment of client/patient satisfaction: development of a general scale. Eval Program Plann, 2(3), 197–207. [DOI] [PubMed] [Google Scholar]
- Marlatt GA, Baer JS, Kivlahan DR, Dimeff LA, Larimer ME, Quigley LA, … Williams E. (1998). Screening and brief intervention for high-risk college student drinkers: results from a 2-year follow-up assessment. J Consult Clin Psychol, 66(4), 604–15. [DOI] [PubMed] [Google Scholar]
- Merrill JE, Reid AE, Carey MP, & Carey KB. (2014). Gender and depression moderate response to brief motivational intervention for alcohol misuse among college students. Journal of Consulting and Clinical Psychology, 82, 984–992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR & Rollnick S. (1991). Motivational Interviewing: Preparing People to Change Addictive Behaviour. New York: Guilford Press. [Google Scholar]
- Miller WR, & Rose GS. (2009). Toward a theory of motivational interviewing. American Psychologist, 64(6), 527–537. doi:2009-13007-002 [pii] 10.1037/a0016830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy JG, Dennhardt AA, Skidmore JR, Borsari B, Barnett NP, Colby SM, Martens MP. A randomized controlled trial of a behavioral economic supplement to brief motivational interventions for college drinking. J Consult Clin Psychol. 2012. October;80(5):876–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen TD, Attkison CC, Stegner B. (1983). Assessment of patient satisfaction: Development and refinement of a service evaluation questionnaire. Evaluation and Program Planning, 6, 299–314. doi: 10.1016/0149-7189(83)90010-1 [DOI] [PubMed] [Google Scholar]
- Nyer M, Cassiello C, Nock M, Petrie S, Holt DJ, Fisher F, …Farabaugh A. (2015). A case series of individual six-week cognitive behavioral therapy with flexible manual-based treatment delivery for depressed college students with or without suicidal ideation. J Ration Emot Cogn Behav Ther, 33(2), 134–147. [Google Scholar]
- Pedrelli P, Borsari B, Lipson SK, Heinze JE, Eisenberg D. (2016). Gender Differences in the Relationships Among Major Depressive Disorder, Heavy Alcohol Use, and Mental Health Treatment Engagement Among College Students. J Stud Alcohol Drugs 77(4):620–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedrelli P, Collado A, Shapero BG, Brill C, & MacPherson L. (2016b). Different pathways explain alcohol-related problems in female and male college students. Journal of American College Health, 64, 535–544. 10.1080/07448481.2016.119101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pettinati HM. Antidepressant treatment of co-occurring depression and alcohol dependence. Biol Psychiatry. 2004. November 15;56(10):785–92. [DOI] [PubMed] [Google Scholar]
- Qi D, Pearson MR, Hustad JT. Predictors of motivation to change in mandated college students following a referral incident. Psychol Addict Behav. 2014. June;28(2):524–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS, & Congdon R. (2013). HLM 7.01 for Windows [Computer software]. Skokie, IL: Scientific Software International, Inc. [Google Scholar]
- Riper H, Andersson G, Hunter SB, de Wit J, Berking M, Cuijpers P. (2014). Treatment of comorbid alcohol use disorders and depression with cognitive-behavioural therapy and motivational interviewing: a meta-analysis. Addiction, 109, 394–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samson JE, Tanner-Smith EE. (2015). Single-Session Alcohol Interventions for Heavy Drinking College students: A Systematic Review and Meta-Analyses. J Stud Alcohol Drugs, 76(4), 530–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satre DD, Leibowitz A, Sterling SA, Lu Y, Travis A, Weisner C. (2016). A randomized clinical trial of Motivational Interviewing to reduce alcohol and drug use among patients with depression. J Consult Clin Psychol, 84(7), 571–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seligman ME, Schulman P. Tryon AM. Group prevention of depression and anxiety symptoms. Behav Res Ther. 2007. June;45(6):1111–26. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Maisto SA. Sobell MB, & Cooper AM. (1979). Reliability of alcohol abusers’ self reports of drinking behavior. Behavior Research and Therapy, 17, 157–160. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2015 National Survey on Drug Use and Health (NSDUH). Table Table 2.20B Alcohol Use, Binge Alcohol Use, and Heavy Alcohol Use in Past Month, by Detailed Age Category: Percentages, 2014 and 2015. Available at https://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015.pdf
- Tubman JG, Vicary JR, von Eye A, & Lerner JV. (1990). Longitudinal substance use and adult adjustment. Journal of Substance Abuse, 2, 317–334. [DOI] [PubMed] [Google Scholar]