Abstract
On September 20, 2017, Hurricane Maria made landfall on Puerto Rico as a category 4 storm resulting in serious widespread impact across the island, including communication and power outages, water systems impairment, and damage to life-saving infrastructure. In collaboration with the Puerto Rico Department of Health, the Public Health Branch (PHB), operating under the Department of Health and Human Services Incident Response Coordination Team, was tasked with completing assessments of health care facilities in Puerto Rico to determine infrastructure capabilities and post-hurricane capacity. Additionally in response to significant data entry and presentation needs, the PHB leadership worked with the Puerto Rico Planning Board to develop and test a new app-based infrastructure capacity assessment tool.
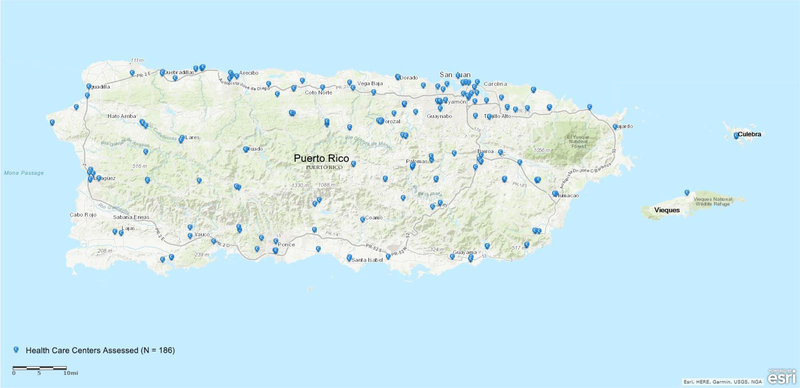
Assessments of hospitals were initiated September 28, 2017 and completed November 10, 2017 (n=64 hospitals, 97%). Assessments of health care centers were initiated on October 7, 2017 with 186 health care centers (87%) assessed through November 18, 2017.
All hospitals had working communications; however, 9% (n=17) of health care centers reported no communication capabilities. For the health care centers, 114 (61%) reported they were operational but had sustainment needs.
In conclusion, health care facility assessments indicated structural damage issues and operational capacity decreases, while health care centers reported loss of communication capabilities post-Hurricane Maria.
Background
Large-scale complex disasters, such as category 4 hurricanes, may result in severe impacts to physical property and operational capacity, including life-saving and life-sustaining services hospitals and selected health care centers, collectively term health care facilities (HCFs)(1). The consequences of large meteorological disasters and specific impacts on HCFs have been described previously in the literature and in damage assessment reports (2–8). Issues in the disaster event’s aftermath include threats to structural integrity (e.g., collapse, damage to roofs or frames), non-structural consequences (e.g., flooding, mold in indoor spaces, equipment damage), and health services impacts (e.g. surgical ward and pharmacy operations, staffing, patient surge) to critical facilities, such as hospitals and health care centers (6–11). After disaster events, the role of HCFs becomes more critical as these facilities provide life-saving and life-sustaining services to both survivors and emergency responders in affected communities. To ensure the availability of health care services to meet these critical public health needs, HCFs’ status and capacity for delivering care must be promptly assessed and reported to medical and emergency management authorities for situational awareness and for immediate determination of needed actions to restore or maintain their operational status.
On September 20, 2017, after causing devastation in other islands in the Caribbean region, Hurricane Maria made landfall on the island of Puerto Rico as a category 4 storm. Entering the southeastern corner of Puerto Rico, the hurricane created a path of destruction north and then westward across the island, affecting approximately three and a half million inhabitants (11). Wind gusts of up to 120mph battered the island for approximately 12 hours. From September 19–21, rainfall amounts totaled more than two feet for some parts of the island, resulting in massive flooding. Impacts from the hurricane were felt in health care facilities across the island and those located in the two adjacent island municipalities of Vieques and Culebra. After the storm, emergency management officials reported that the entire island of Puerto Rico was without power, over 66% of the population lacked access to potable water, and up to 95% of cell and other communication services (e.g., landlines) were not operational (12). Devastation to infrastructure resulted in cascading effects that severely limited both public and private HCFs’ essential functions and services (13). The list of affected HCFs included Centro Medico, the central medical center, and an adjacent conglomerate of hospitals, including the island’s and Caribbean Region’s only trauma center; several regional medical centers; local and municipal facilities; and primary and community health centers.
Recent responses have successfully demonstrated the utility of standardized public health assessments as part of disaster epidemiologic tools for rapidly collecting data in the aftermath of disasters (14–17). In the United States, well-established methods, guidelines, mandates, and tools on how to carry out HCF-specific post-disaster assessments have yet to be developed and standardized. In the past, damage assessments of HCFs have been limited to predominantly hospitals with reports based largely on anecdotal information, usually from non-structured interviews with sparse descriptions of impacts or from mailed surveys instead of in-person assessments (4). Structured assessments and checklists, similar to those used by the World Health Organization’s “Safe Hospitals programmes”, have been encouraged for facilities at various levels of care. However, most assessments have been used for preparedness or to assess a limited number of facilities outside the United States (3, 5, 10, 18–20).
Federal support following major disasters is part of the activities delineated under the National Response Framework, and assessment of public health and medical needs is one of the core functions of Emergency Support Function-#8 (ESF-8), Public Health and Medical Services responsibilities (21). The United States Department of Health and Human Services (DHHS) serves as the lead agency for ESF-8, with additional federal agencies providing technical support and assistance. Per their procedures during large disasters, the Incident Response Coordination Team (IRCT) is deployed to assist with coordinating and providing support to the affected jurisdictions in assessing response and recovery needs and delivering medical care and public health preventive services (22). As a result of Hurricane Maria’s devastation, additional public health response personnel were deployed, and the existing team transitioned into a public health branch (PHB) operating in collaboration with PRDOH. A management structure was established to organize the branch into several specialized teams capable of performing specific public health assessments and support functions. Teams were formed around the following focus areas: environmental health (Surveillance and Assessment Team), restoration of services (Public Health Restoration Team), health communications (Health Communication Team), health surveillance (Surveillance and Assessment Team), and public health assessments (Public Health Field Team). Determining the damage and operational status of HCFs in Puerto Rico was deemed a priority by the Puerto Rico Department of Health (PRDOH) and DHHS. To address this need, the PHB developed and implemented infrastructure capacity assessment tools (ICAT) specifically for HCFs, including hospitals and health care centers. This manuscript describes the activities and processes to execute assessments of HCFs, provides the findings of those assessments and the impacts to the health care systems, and identifies potential areas of improvement for support and coordination of assessments of critical infrastructure, including HCFs, in post-disaster settings.
Methods
All hospitals on the island were selected for evaluation from an updated list of HCF’s provided by the PRDOH. Preliminary discussions were held with commonwealth, federal, and Department of Defense (DoD) officials to define the scope of the assessments, discuss tools and methods for the assessments, coordinate the necessary logistical support and transportation, and prioritize a current list of facilities for evaluation based on PRDOH needs. Following these discussions, the PHB adapted an existing prototype hospital assessment into a set of paper-based infrastructure capacity assessment tools (ICAT). During the assessment period, the PHB leadership briefed local and federal officials on a daily basis regarding the status of the assessments and presented future planning activities for leadership approval and securing logistical support.
Infrastructure Capacity Assessment Tools
The ICAT were developed by the PHB to evaluate hospitals and health care centers. Development took place in collaboration with PRDOH and included queries from their pre-existing tools. For the ICAT, multiple domains were designed to obtain information on operational unit capacity, structural concerns (e.g., roof damage), and other issues of concern. For the hospital tool, information on current patient census, number of beds lost, number of morgue spaces available, and number of bodies held in the morgue was obtained; for health care centers assessments, the tool collected information regarding the number of patients treated and released and the number treated and transferred. To assess HCFs, the PHB piloted a hospital-specific ICAT that was developed as a prototype from knowledge gained during prior hurricane response activities, but the tool had not previously been used during an actual event. This tool was piloted at several hospitals in Puerto Rico in late September 2017, post-Hurricane Maria. After the pilot work, the tool was finalized for hospital assessments, and a modified version was developed for health care centers. Specifically, the modified version was developed in consultation with members of the health sector and the Federal Emergency Management Agency’s (FEMA) response personnel.
Data collection
Assessments of HCFs began on September 28, 2017 and October 7, 2017, respectively. Phase one of the assessments used a hierarchical tiered approach ranging from tiers 1 through 3; the priority HCFs included in tiers 1–3 were determined based on population density, critical services offered, and access to other health care facilities. Tiers 1 and 2 were hospital facilities; Tier 3 included larger health care center facilities and regional medical centers. Phase 2 encompassed all other health care clinic facilities, including private and public facilities and those facilities with mental health in-patient services. Each assessment team consisted of 2 to 3 public health specialists, including environmental health scientists, engineers, and sanitarians, some of whom had experience working with HCFs. When required, translators provided by FEMA were used.
For consistency during the data collection efforts, all field teams received training in the administration of the assessment tools. During staff rotations, existing staff trained new field assignees; this allowed for appropriate survey techniques and methods to be grasped by team members before deploying to the field. Assessment data were gathered through face-to-face interviews with hospital and health care center administrators or their assigned personnel (e.g., facility safety officer). Hospital administrators self-reported structural damage using a qualitative scale, specifically categorized as none, minor, moderate, severe, and total. Information on flood/water damage was obtained and included damage due to water intrusion from a variety of issues (e.g., roof damage, broken windows). Other information collected by the field assessment teams included photographs of damage, lists of supply needs, and immediate issues and needs identified by the HCF administrator. Teams debriefed and compiled a synopsis of the most critical findings, which was provided to HHS, FEMA, and PRDOH on a daily basis. The paper forms, along with a brief summary of high-level findings, were also compiled and delivered to HHS, FEMA, and PRDOH daily. At the end of each day, assessment forms were entered into a secure database for analysis. Due to the need for updated status, a limited number of HCFs were assessed a second time. Health care facility assessments were completed on November 17, 2017.
Survey123 App development
In collaboration with the Puerto Rico Planning Board, the ICAT paper assessment tools were translated into an app-based ICAT suite available in both Spanish and English, using the ESRI Survey123 (ICAT app) for ArcGIS software (ESRI, Redlands, CA). The ICAT app was downloaded on IPads (Apple, Inc., Cupertino, CA) and piloted October 31, 2017 to November 18, 2017. The HCF assessment data and photographs of damages to the facilities were directly entered and uploaded into the app by the field teams. Whenever a stable internet signal was available, the survey data were uploaded to the server. Due to the island-wide power outages, this activity was often only possible upon return to the base of operations (the Joint Field Office). Once uploaded, the survey data were immediately available for viewing online and in several file formats (e.g., Excel, CSV, fileGDB).
Results
Hospital Facilities
The Tier 1 and 2 hospital assessments were completed on 64 (97%) hospitals in Puerto Rico (Figure 1). One of the 64 (2%) hospitals reported being closed as a result of damages from the hurricane. At the time of assessment, 51 (80%) hospitals reported they were on the power grid, and 57 (89%) reported they had an operable generator. Of the 64 hospitals assessed, four (6%) reported a shortage of safe drinking water, and one hospital reported having no safe drinking water. The average patient census at the time of assessment was 111 (range 0–370). Hospitals reported losing an average of 6.9 beds (range 0–100). In addition to patient census and beds lost, the assessment contained queries regarding facility morgues. The average number of total morgue spaces was 6.4, and the average number of deceased being held was 1.4 (range 0–8). For facility needs and shortages, medication was the most commonly reported shortage followed by oxygen, 22% (n=14) and 20% (n=13), respectively. No hospitals reported shortages of blood, and few hospitals reported shortages of personal protective equipment (PPE) and vaccines, 5% (n=3) and 11% (n=7), respectively. Approximately 6% (n=4) of hospitals reported shortages of medical staff and 5% (n=3) reported shortages of administrative staff; no hospitals reported a complete absence of medical or administrative staff.
Figure 1:
Map of hospitals assessed in Puerto Rico from September through November 2017
Operational Units
Operational units perform services, including emergency care, obstetrics, intensive care, and pediatrics. The majority of the hospitals reported being operational; however, specific operational unit capability varied (Table 1). Surgical units and X-ray were the units most frequently reported as being partially open or having limited capacity (n=7, 11%). Very few hospitals reported any of the operational units as being closed (maximum of three hospitals for a specific operational unit closure).
Table 1:
Operational unit capability at hospitals reported during initial hospital assessment, September through November 2017
| Operational Unit | Fully operational | Partially operational | Closed | Unknown/Not applicable* |
|---|---|---|---|---|
| ED** | 53 (83%) | 3 (5%) | 1 (2%) | 7 (11%) |
| Laboratory | 55 (86%) | 0 (0%) | 0 (0%) | 9 (14%) |
| X-ray | 48 (75%) | 7 (11%) | 1 (2%) | 8 (13%) |
| ICU*** | 46 (72%) | 5 (8%) | 3 (5%) | 10 (16%) |
| Med surgical | 47 (73%) | 4 (6%) | 3 (5%) | 10 (16%) |
| Neonatal | 26 (41%) | 1 (2%) | 3 (5%) | 34 (53%) |
| Pediatric | 44 (69%) | 0 (0%) | 3 (5%) | 17 (27%) |
| Dialysis | 38 (60%) | 2 (3%) | 1 (2%) | 23 (36%) |
| Mental | 16 (25%) | 1 (2%) | 2 (3%) | 45 (70%) |
| Maternity | 34 (53%) | 0 (0%) | 3 (5%) | 27 (42%) |
| Operating | 44 (69%) | 7 (11%) | 3 (5%) | 10 (16%) |
| Outpatient | 46 (72%) | 2 (3%) | 2 (3%) | 14 (22%) |
| Pharmacy | 60 (94%) | 2 (3%) | 1 (3%) | 1 (2%) |
| Disinfection | 55 (86%) | 0 (0%) | 2 (3%) | 7 (11%) |
For the purpose of information presentation, both unknown and not applicable are combined; however, these were reported separately in the assessment. Some fields may total >100% due to rounding.
Emergency Department
Intensive Care Unit
Structural damage
The majority of hospitals reported no damage to foundation, road access, walls, or lighting; however, more than half (65%) reported damage to the roof. Specifically, 23%, 23%, and 19% of facilities reported minor, moderate, and severe roof damage, respectively. The most common structural damage reported was minor damage to windows, n=24 (Table 2). Additionally, 35 hospitals (55%) reported flood/water damage and 42 (66%) reported wind damage.
Table 2:
Hospitals reporting structural damage* at the time of initial assessment, September through November 2017 (n=64)**
| Structure | No damage | Minor | Moderate | Severe |
|---|---|---|---|---|
| Windows | 32 (50%) | 24 (38%) | 4 (6%) | 4 (6%) |
| Foundation | 62 (97%) | 0 (0%) | 1 (2%) | 0 (0%) |
| Road access | 58 (91%) | 4 (6%) | 2 (3%) | 0 (0%) |
| Roof | 22 (34%) | 15 (23%) | 15 (23%) | 12 (19%) |
| Walls | 41 (64%) | 14 (22%) | 6 (9%) | 3 (5%) |
| Lighting | 53 (83%) | 7 (11%) | 3 (5%) | 1 (2%) |
| HVAC*** | 37 (58%) | 11 (17%) | 10 (16%) | 5 (8%) |
| Damage | No | Yes | ||
| Flood/Water**** | 29 (45%) | 35 (55%) | ||
| Wind | 22 (34%) | 42 (66%) | ||
Damage to the structure could be the result of wind damage, flood/water damage, or both.
Not all rows will total 100% due to rounding
Heating, ventilation, and air conditioning
Damage could be the result of flood or water intrusion from a variety of issues (e.g., roof damage, window damage).
Health Care Centers
A total of 193 assessments were performed on 186 health care centers (Figure 2). Tier 3 facilities (n=16) were assessed initially, followed by assessment of the majority of health care centers on the island (Phase 2, n=170). Of the 186 health care centers, 14 (7%) reported being closed, 114 (61%) were operational but had sustainment needs, and 56 (29%) were fully operational. Seventeen health care centers reported having no communication capability. Only 63 health care centers (34%) reported they were fully on the electrical grid, and 58 (31%) reported intermittent service on the grid. Eighty-three health care centers (45%) reported a generator-only power source; of these, nine facilities (11%) reported inoperable generators. Sixty-three facilities (45%) reported a shortage of safe drinking water, and 11 (6%) reported having no safe drinking water. The number of patients treated in the last 24 hours ranged from 0 to 891, with an average of 98.5. The number of morgue spaces available ranged from 0 to 11, with an average of 0.5. For health care center needs and shortages, medications were the most commonly reported shortage (n=73, 40%), followed by vaccines (n=65, 35%). Additionally, 28 health care centers reported having no vaccines. Less than 10% of health care centers reported a shortage of medical staff.
Figure 2:
Map of health care centers assessed in Puerto Rico from October through November 2017
Operational Units
While the majority of the health care centers reported being at least partially operational, the specific operational unit capability varied (Table 3). Outpatient was the unit most often reported being partially operational (29%), followed by X-ray (22%). However, not all operational units were present at all health care centers. For example, only 109 health care centers contained emergency departments. Of the 109 centers with EDs, 26 reported their center was partially operational. For all operational units being reported as partially operational, the ED was the unit least frequently reported.
Table 3:
Health care center reported operational unit capability at the time of assessment, October through November 2017*
| Operational unit | Fully operational | Partially operational | Closed | Not applicable/Unknown** |
|---|---|---|---|---|
| ED*** | 83 (43%) | 26 (13%) | 0 (0%) | 69 (36%) |
| Outpatient | 95 (49%) | 56 (29%) | 0 (0%) | 24 (12%) |
| Pediatrics | 88 (46%) | 40 (21%) | 0 (0%) | 50 (26%) |
| Maternity | 45 (23%) | 22 (11%) | 0 (0%) | 109 (56%) |
| Metal health | 62 (32%) | 28 (15%) | 0 (0%) | 89 (46%) |
| Pharmacy | 66 (34%) | 30 (16%) | 1 (0.5%) | 79 (41%) |
| Laboratory | 76 (39%) | 32 (17%) | 0 (0%) | 65 (34%) |
| X-ray | 65 (34%) | 42 (22%) | 2 (1%) | 60 (31%) |
The number of assessments was 193 as a small number of facilities were assessed twice. Not all fields will equal 193 as some facilities did not report specific items
Due to missing data not all fields will total 193
For the purpose of information presentation, both unknown and not applicable are combined; however, these were reported separately in the assessment.
Emergency Department
Structural damage
The majority of facilities reported no damage to the foundation and walls. The most commonly reported structural damages of any severity were roof and window damage, n=124 and n=46, respectively (Table 4). For roof damage, 19%, 25%, 17%, and 3% of health care centers reported minor, moderate, severe and total damage, respectively. Over 50% of health care centers reported flood/water damage, n=100, and wind damage, n=101. Overall, 32 health care centers reported collapsed structures, three of which were closed.
Table 4:
Number of health care centers reporting structural damage* October through November 2017 (total number of health care centers assessed, n=186)**
| Structure | Minor | Moderate | Severe | Total |
|---|---|---|---|---|
| Windows | 32 (17%) | 8 (4%) | 5 (3%) | 1 (0.5%) |
| Foundation | 4 (2%) | 3 (2%) | 1 (0.5%) | 0 (0%) |
| Road access | 17 (9%) | 6 (3%) | 7 (4%) | 0 (0%) |
| Roof | 37 (19%) | 48 (25%) | 33 (17%) | 6 (3%) |
| Walls | 13 (7%) | 12 (6%) | 5 (3%) | 4 (2%) |
| Lighting | 25 (13%) | 13 (7%) | 4 (2%) | 4 (2%) |
| HVAC*** | 21 (11%) | 23 (12%) | 18 (9%) | 12 (6%) |
| Damage | No | Yes | ||
| Flood/Water**** | 77 (40%) | 100 (52%) | ||
| Wind | 75 (39%) | 101 (52%) | ||
Damage to the structure could be the result of wind damage, flood/water damage, or both.
Not all rows will total 100% due to rounding
Heating, ventilation, and air conditioning
Damage could be the result of flood or water intrusion from a variety of issues (e.g., roof damage, window damage).
App-based ICAT pilot testing
The ICAT app was piloted at 76 health care centers (41%) from October 31, 2017 through November 18, 2017. The teams examined the utility of the app by simultaneously administering paper and app-based ICAT assessment at each location. The pilot work indicated that use of the app resulted in an estimated time savings of 1 hour per survey. Specifically, the need for rewriting of paper-based surveys (due to legibility issues) at the end of the daily assessments was eliminated, resulting in an estimated 15 minutes of time saved per survey. The need for data entry from paper-based surveys into the electronic database was eliminated, along with quality assurance/quality control of data entry. The elimination of these data entry steps resulted in an estimated 45 minutes per survey saved. Additionally, the use of the ICAT app allowed for immediate database download and dissemination to federal partners. A dashboard was also created allowing for rapid viewing of high-priority field data, specifically communication status, power status, and other critical information needs (Figure 3).
Figure 3:
Dashboard of high-priority information collected during pilot testing of the ICAT app, November 2017
Discussion
The current investigation reports on damage and operational assessments of a large number of hospitals and health care centers in Puerto Rico following Hurricane Maria. The information collected as part of the HCF assessments was used to drive response-related activities for various federal and local agencies. For example, the information was used to initiate immediate action in specific cases for the designated Tier 1 and 2 hospitals and Tier 3 clinics (e.g., delivery of a satellite phone for a clinic without any communication capabilities). The assessments were also used to prioritize temporary repairs (e.g., installation or repair of temporary “blue” roof structures) and the initiation and submission of Resource Request Forms. Information on HCF operational status and capabilities was used to aid the DoD strategic planning for establishing temporary medical treatment sites in Puerto Rico.
The impacts as indicated in the results from the HCF assessments are similar to those reported in previous events involving other types of natural disasters, including earthquakes and floods (2–5). For example, a majority of hospitals and health care centers reported damage to the roof. This is similar to a survey conducted by the Florida Hospital Association in 2004, which noted the most significant damage to hospitals post-hurricane was to the roof (5).
A decrease in medical care and treatment capacity and other issues, such as loss of communications and utilities, are known to occur as a result of the direct impacts from a natural disaster or the cascading effects from the lack of power, inability to procure adequate supplies of fuel, and failure of auxiliary power generation equipment. Flooding and water intrusion may result in loss of sterilization capabilities; heating, ventilation, and air conditioning; and basic sanitary and hygienic systems all of which are necessary for hospital safety and infection prevention and control. Water damage could also contribute to the development of mold and other pathogen growth. Wind damage, as reported in some facilities, may also cause significant loss of medical equipment and structural damage leading to water intrusion and other issues.
During the Hurricane Maria Response, the PHB conducted the environmental assessments of hospitals and health care centers and provided summaries of these assessments, including a list of critical needs, on a daily basis to HHS, FEMA, and PRDOH. Daily feedback is essential during the early phase of the response as facilities’ status may change unexpectedly and can fluctuate from fully operational to a non-operational status in a short time span. Specifically for the Tier 1 and 2 hospitals, the data collected as part of the assessments was used for documenting the need for various temporary field medical facilities, including DoD facilities, in Puerto Rico. The information was also used to initiate immediate action in specific cases for the high-priority hospitals and health care centers, especially those experiencing shortages of critical supplies such as fuel, water, and staffing. Furthermore, as the event shifted from response to recovery, the information compiled from the assessments, along with other sources of information including pictures and diagrams of damages and effects, was used to prioritize temporary repairs and for initiation and submission of applications for additional assistance with damage.
Several limitations and challenges were identified in the initiation, implementation, and continuation of HCF assessments. Immediate initiation of assessments was not possible due to safety concerns; once teams were allowed to initiate the assessments, all teams were required to be escorted by law enforcement due to safety concerns and mandatory curfew. The field teams often lacked Spanish-speaking assessors, which resulted in the need for translators and a smaller number of teams available for assessments. Another limitation that has been documented in previous disaster responses is the issue of redundancy and lack of coordination between assessment entities (23). Multiple agencies were conducting assessments using a variety of forms and interview methods, resulting in redundancy of efforts and confusion. Many facilities administrators reported feeling overwhelmed by the number of entities asking for similar information which resulted in time taken away from their other essential activities related to the disaster. Stronger agency collaboration and coordination and data sharing could reduce redundancy and improve situational awareness in future responses, and reduce burden on facility administrators. The real-time GIS capabilities of the ICAT app will allow for multi-agency collaboration and coordination which may improve situational awareness and diminish redundancy, duplication of efforts, and participant fatigue.
In contrast to other groups conducting assessments during this response, the use of standardized data collection tools and training allowed for more consistent data collection and resulted in improved data quality. Additionally, the ICAT app piloted during the response demonstrated the feasibility and utility of using app-based survey tools during response activities. Specifically the use of the ICAT app in lieu of paper-based surveys allowed for elimination of database entry needs, resulting in an increase in efficiency and data quality.
In conclusion, health care facility infrastructure was affected, including reduced capabilities and medication and medical supply shortages, post-Hurricane Maria as determined by assessment of 97% of hospitals and 87% of health care centers in Puerto Rico. However, only a small percent of hospitals and health care centers reported being closed due to damages from the hurricane. As situational awareness and assessment data are of the essence in disaster response and recovery, the use of standardized assessment tools resulted in consistent, high-quality data collection, and the tools should be considered as a model for environmental assessments of health care facilities in future disaster response situations. The development and piloting of the ICAT app indicated that electronic-based surveys provide an opportunity for improved efficiency and speed of data collection and data management, specifically with the elimination of the data entry step and increased data quality with the reduction of data entry errors. Recently, a pilot scale project was completed for the development and implementation of the Comprehensive Disaster Assessment and Readiness Tools (CDART) for health care facilities in Puerto Rico. The pilot CDART project, conducted in collaboration with the PRDOH and Puerto Rico Planning Board, resulted in an increased capacity within the PRDOH for preparedness and response activities. Currently, efforts to develop a comprehensive question/variable databank and set of survey templates and to expand and standardize CDART are underway. The tools, including app-based surveys, can be requested, and modifications can be made specific for agency and response needs. Once finalized, the CDART tools and platform will enable state, local, territorial, tribal, and federal public health officials to collect geospatial and assessment data and disseminate key information in near real-time, while increasing efficiency and reducing redundancy during disaster responses.
Footnotes
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Agency for Toxic Substances and Disease Registry/Centers for Disease Control and Prevention.
References
- 1.Noji EK: The public health consequences of disasters. Prehosp Disaster Med 2000;15:147–15. [PubMed] [Google Scholar]
- 2.Ochi S, Kato S, Kobayashi KI, Kanatani Y. The Great East Japan Earthquake: Analyses of Disaster Impacts on Health Care Clinics. Disaster Med Public Health Prep 2017. Aug 29:1–5. doi: 10.1017/dmp.2017.82 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 3.Matsumura T, Osaki S, Kudo D, Furukawa H, Nakagawa A, Abe Y, Yamanouchi S, Egawa S, Tominaga T, Kushimoto S. Water supply facility damage and water resource operation at disaster base hospitals in Miyagi Prefecture in the wake of the Great East Japan Earthquake. Prehosp Disaster Med 2015;30:193–198. [DOI] [PubMed] [Google Scholar]
- 4.Kirsch TD, Mitrani-Reiser J, Bisseli R, Sauer LM, Mahoney M, Holmes WT, Cruz NS, De La Maza F. Impact on hospital functions following the 2010 Chilean earthquake. Disaster Med Public Health Preparedness, 2010:4;122–128. [DOI] [PubMed] [Google Scholar]
- 5.Florida Hospital Association. Eye of the Storm: Impact of the 2004 hurricane season on Florida hospitals [Google Scholar]
- 6.Nates JL. Combined external and internal hospital disaster: impact and response in a Houston trauma center intensive care unit. Crit Care med 2004;32:686–690. [DOI] [PubMed] [Google Scholar]
- 7.Norcross ED, Elliott BM, Adams DB, Crawford FA. Impact of a major hurricane on surgical services in a university Hospital. The American Surgeon, November 1993;59:28–33. [PubMed] [Google Scholar]
- 8.Tran P, Weireter L, Sokolowski W, Lawsure K, Sokolowski J. HAZUS modeling for hurricane effect on a health care campus: implications for health care planning. The American Surgeon, November 2009;75:1059–1064. [PubMed] [Google Scholar]
- 9.Downey EL, Andress K, Schultz CH. Initial management of hospital evacuations caused by Hurricane Rita: a systematic investigation. Prehosp Disaster Med 2013; 28:257–263. [DOI] [PubMed] [Google Scholar]
- 10.WHO. Safe hospitals in emergencies and disasters Available at: http://www.wpro.who.int/emergencies_disasters/documents/SafeHospitalsinEmergenciesandDisastersweboptimized.pdf Accessed November 2017.
- 11.NOAA. National Hurricane Center. Hurricane Maria Available at: http://www.nhc.noaa.gov/archive/2017/al15/al152017.update.09201034.shtml Accessed November 2017.
- 12.FEMA. Hurricane Maria. Statistics Progress in Puerto Rico Available at: https://www.fema.gov/hurricane-maria Accessed November 2017.
- 13.HHS. Hurricane Maria Press Release Available at: https://www.hhs.gov/about/news/2017/10/12/hhs-fema-dod-and-va-continue-provide-sustained-and-critical-medical-care.html Accessed October 2018.
- 14.Malilay J Public health assessments in disaster settings: Recommendations for a multidisciplinary approach. Prehosp Disaster Med 2000;15:167–172. [PubMed] [Google Scholar]
- 15.Malilay J, Heumann M, Perrotta D, Wolkin AF, Schnall AH, et al. The Role of Applied Epidemiology Methods in the Disaster Management Cycle. Am J Public Health 2014;104:2092–2102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention (CDC). Hurricane Ike rapid needs assessment - Houston, Texas, September 2008. MMWR 2009;58:1066–71. [PubMed] [Google Scholar]
- 17.Cruz MA, Garcia S, Chowdhury MA, Malilay J, Perea N, Williams OD. Assessing the Congregate Disaster Shelter: Using Shelter Facility Assessment Data for Evaluating Potential Hazards to Occupants during Disasters. J Public Health Manag Pract 2017. Jan/Feb;23:54–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ardalan A, Keleh M Kandi, Saberinia A, Khorasani-Zavareh D, Khankeh H, Miadfar J, et al. (2016) 2015 Estimation of Hospitals Safety from Disasters in I.R.Iran: The Results from the Assessment of 421 Hospitals. PLoS ONE 11: e0161542. doi: 10.1371/journal.pone.0161542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Djalali A, Ardalan A, Ohlen G, Ingrassia PL, Corte F Della, Castren M, Kurland L. nonstructural safety of hospitals for disasters: a comparison between two capital cities. Disaster Med Public Health Preparedness 2014;8:179–184. [DOI] [PubMed] [Google Scholar]
- 20.Bulson J, Bulson T. How can hospitals be better prepared? A case study of an exercise design program and its effect on a real-life event. Journal of Health Care Protection Management 2010;26:89–94. [PubMed] [Google Scholar]
- 21.National Response Framework Retrieved from: https://www.fema.gov/media-library-data/1466014682982-9bcf8245ba4c60c120aa915abe74e15d/National_Response_Framework3rd.pdf Accessed January 2018.
- 22.HHS. Public health emergency. HHS Concept of operations for ESF-8 Available at: https://www.phe.gov/Preparedness/planning/mscc/handbook/chapter7/Pages/hhsconcept.aspx Accessed: January 2018.
- 23.Deitchman S:What Have We Learned?—Needs Assessment. Prehosp Disast Med 2005;20(6):468–470. [DOI] [PubMed] [Google Scholar]
- 24.Kile J, Skowronski S, Miller MD, Reissman SG, Balaban V, Klomp RW, Reissman DB, Mainzer HM, Dannenberg AL: Impact of 2003 Power Outages on Public Health and Emergency Response. Prehosp Disast Med 2005;20(2):93–97. [DOI] [PubMed] [Google Scholar]