This randomized clinical trial examined the effect of in-person social services navigation assistance vs a written information sheet on caregiver-reported social risk factors and child and caregiver health.
Key Points
Question
Did in-person, longitudinal social services navigation assistance result in greater reduction in social risk factors and better health for children and caregivers than a less intensive approach?
Findings
In this randomized clinical trial including 611 caregiver-child dyads, there were no statistically significant differences between the groups in the effectiveness of the interventions. In post hoc secondary analyses of both groups, there were significant improvements in social risk factors and in child and caregiver health at 6-month follow-up.
Meaning
These findings suggest that delivery of curated, individualized written resources with or without longitudinal, in-person navigation services about social services in pediatric urgent care settings can affect family circumstances and child and caregiver health.
Abstract
Importance
Social and economic contexts shape children’s short- and long-term health. Efforts to address contextual risk factors are increasingly incorporated into pediatric health care.
Objective
To compare the effectiveness of 2 social risk–related interventions.
Design, Setting, and Participants
This randomized clinical trial included English- and/or Spanish-speaking caregiver-child dyads recruited from a pediatric urgent care clinic nested in a large, urban, safety-net hospital. Study recruitment, enrollment, and follow-up were conducted from July 18, 2016, to March 8, 2019. Data analysis was conducted from January 1, 2019, to January 20, 2020.
Interventions
Following standardized social risk assessment, caregivers were randomly assigned to receive either written information regarding relevant government and community social services resources or comparable written information plus in-person assistance and follow-up focused on service access.
Main Outcomes and Measures
Caregiver-reported number of social risk factors and child health 6 months after enrollment.
Results
Among 611 caregiver-child dyads enrolled in the study, 302 dyads were randomized to the written resources group and 309 dyads were randomized to the written resources plus in-person assistance group. The mean (SD) age of children was 6.1 (5.0) years; 483 children (79.1%) were Hispanic; and 315 children (51.6%) were girls. There were no significant differences between groups in the effects of the interventions. In post hoc secondary analyses, the number of reported social risks decreased from baseline to 6-month follow-up in both groups: caregivers who received written resources alone reported a mean (SE) of 1.28 (0.19) fewer risks at follow-up, while those receiving written resources plus in-person assistance reported 1.74 (0.21) fewer risks at follow-up (both P < .001). In both groups, there were small but statistically significant improvements from baseline to follow-up in child health (mean [SE] change: written resources, 0.37 [0.07]; written resources plus in-person assistance, 0.24 [0.07]; both P < .001).
Conclusions and Relevance
This randomized clinical trial compared 2 approaches to addressing social risks in a pediatric urgent care setting and found no statistically significant differences in the social risk and child and caregiver health effects of providing written resources at the point of care with vs without in-person longitudinal navigation services. Caregivers in both groups reported fewer social risks and improved child and caregiver health 6 months after the intervention. These findings deepen understanding of effective doses of social risk–related interventions.
Trial Registration
ClinicalTrials.gov Identifier: NCT02746393
Introduction
Childhood social and economic adversity, such as food insecurity and housing instability, is associated with significant short- and long-term health risks, including higher likelihood of childhood behavioral problems, cognitive delay, unhealthy weight, and asthma, as well as adult obesity, diabetes, and cardiovascular disorders.1,2,3,4,5,6,7,8,9,10,11,12,13,14,15 Moreover, cumulative exposure to social and economic risk factors has been associated with worse health outcomes independent of the effects of individual risks.8,16
In response to consistent and compelling evidence linking social and economic risks to health and well-being, multiple medical professional organizations have endorsed increased attention to social risk factors in the context of clinical care.17,18,19 Although pediatricians have long recognized the influence of social context on health outcomes,20 recent recommendations have accelerated social risk screening and social risk–related interventions in pediatric clinical settings.21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46
Despite considerable diversity in existing pediatric clinical activities aimed at identifying and reducing social risk, little research has rigorously examined program effects or assessed the feasibility of scaling programs across pediatrics clinical settings.47 In this study, we compare the effectiveness of 2 social risk–related interventions that differ in intensity and potential scalability: in-person social services navigation assistance offered for up to 3 months by a trained volunteer vs standardized, written information about community and government social services resources. Based on previous research,23,25,48 we hypothesized that ongoing, in-person assistance would be more likely to reduce social risks and improve both child and caregiver health outcomes than would 1-time receipt of individualized information about relevant social resources.
Methods
This 2-group randomized clinical trial was approved by the institutional review board of the University of California, San Francisco. All adult caregivers completed written informed consent, and assent for participation was obtained from children 7 years or older. The complete study protocol is provided in Supplement 1. This study is reported following the Consolidated Standards of Reporting Trials (CONSORT) reporting guideline.
Study Setting and Participant Eligibility
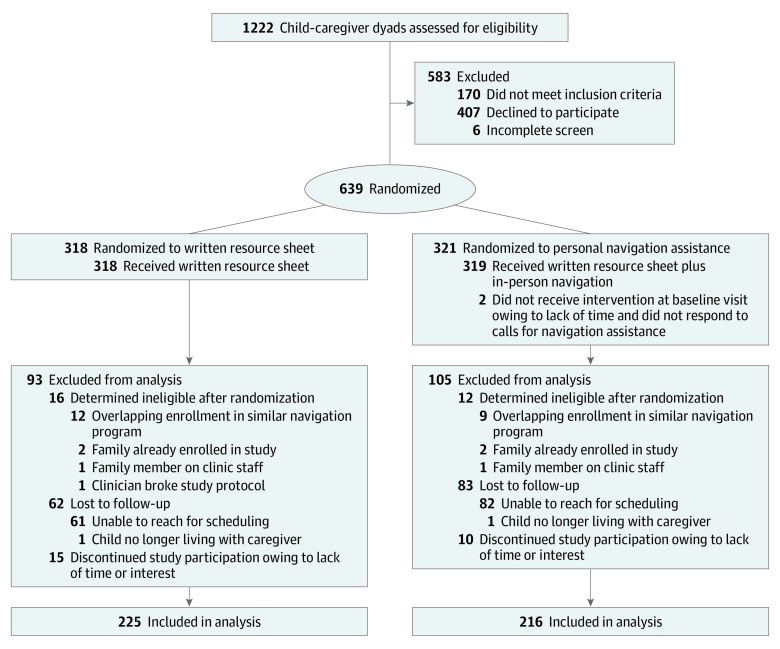
Study recruitment, enrollment, and follow-up were conducted from July 18, 2016, to March 8, 2019, in the pediatric urgent care clinic at an urban safety-net hospital serving primarily low-income, racially and ethnically diverse populations. Eligible participants were caregiver-child dyads with English- or Spanish-speaking caregivers 18 years or older who were familiar with the child’s household environment and residing in the county of enrollment. Eligible children were aged 0 to 17 years. Only 1 child and 1 caregiver per household were enrolled. If 2 caregivers presented with the child, caregivers self-selected 1 to participate in the study. Families enrolled in a similar primary care–based hospital social services navigation initiative in the 6 months prior or subsequent to recruitment, children in foster care, or those being seen for physical abuse evaluations were excluded (Figure).
Figure. CONSORT Flow Diagram.
Study Procedures, Randomization, and Follow-up
Trained research assistants screened English- or Spanish-speaking families presenting in pediatric urgent care weekdays from 8:30 am to 5:00 pm. Consenting dyads completed all baseline study activities in the clinical examination room during or directly after the child’s medical visit. Research assistants administered baseline demographic characteristics and child health surveys on a tablet computer using Research Electronic Data Capture tools.49 Caregivers and children were then given the option of self-completing or working with a research assistant to complete additional child and caregiver health questions. Biomarker samples also were collected from consenting families, although results from those analyses are not presented here. Participating dyads received a $50 gift card after completing baseline study activities.
After informed consent forms were completed and baseline data were collected, the research assistant left the room, and a patient navigator administered a brief social risk survey. The navigator then randomly assigned the participating dyad into 1 of 2 study groups using an automated computer-generated algorithm; randomization occurred within blocks (block size, 10 dyads). Navigators were trained to provide social service navigation services and were periodically observed by supervising senior clinical research associates to ensure they followed study protocols. They were not involved with follow-up outcomes assessment.
Written Resources Intervention
Dyads randomized to receive written resources were given information about relevant government, hospital, and community social services. Prewritten informational handouts were populated with data on local resources based on the accumulated knowledge of navigators working in a similar hospital-based linkage program. Navigators individualized the resource sheets by highlighting resources most closely related to the top 3 priority social risk factors endorsed by the caregiver and by providing names of contacts at relevant organizations when available.
In-Person Assistance Intervention
Families randomized to in-person navigation services either received assistance immediately after randomization or were offered a telephone or in-person follow-up appointment at a different time. As in the written resources group, during these visits navigators provided written information about resources related to the caregiver’s prioritized social risk factors. Additionally, navigators helped to schedule appointments, complete forms, or provide other social services–related counseling and assistance. Information about protocols for providing written resources and additional supports is published elsewhere.50 Following the initial visit, caregivers in the in-person assistance group were contacted by navigators by telephone, text message, or email every 2 weeks for 3 months until identified needs were met or caregivers declined further assistance, whichever came first.
Participating caregivers in both groups were contacted by telephone (and text message, email, and/or letters when telephone calls were unsuccessful) to schedule follow-up interviews 6 months after enrollment. Research assistants, still blinded to study group assignment, administered follow-up surveys using tablet computers. Follow-up interviews were conducted primarily in person in the pediatric urgent care clinic or interview rooms located in the same clinical building. If participants were unable to return to the study site (eg, moved out of the area or had work-related barriers), research assistants completed surveys during home visits or administered surveys by telephone. Participating dyads again received $50 gift cards in exchange for time spent on study activities.
Measures
Demographic Characteristics and Social Risk Factors
Caregivers reported caregiver and/or child age, gender, race, Hispanic/Latino ethnicity, preferred language, family income, caregiver education level, and caregiver-child relationship. At baseline and 6-month follow-up, caregivers answered yes or no questions about their child and household’s social situation. The 18-item social risk screening questionnaire was based on surveys used in earlier studies25,26 and included items on housing stability and habitability, food and income security, child care and transportation needs, employment, legal concerns, medical insurance, and other public benefits enrollment (eAppendix in Supplement 2). Additional questions included whether the child and caregiver were connected to primary care, concerns about the child’s experiences of bullying, and adult household members’ mental health.
Child Health
At baseline and 6-month follow-up, child quality of life was assessed with the shortened version of the Pediatric Quality of Life Inventory (PedsQL) 4.0 Generic Core Scales developed for children ages 2 to 18 years,51 the PedsQL 4.0 short form 15,52 or the PedsQL Infant Scales developed for children ages 1 to 24 months.53 The PedsQL uses parent proxy reports to assess child functioning across the following domains: physical functioning, emotional functioning, social functioning, and cognitive or school functioning.54,55 Each item is scored on a 5-point Likert scale ranging from 0, indicating never a problem, to 4, almost always a problem, and converted to a 100-point scale, with higher scores indicating higher quality of life. Child global health was assessed by caregiver report using a single item from the 2016 to 2017 National Survey of Children’s Health. This item is associated with health services use and other measures of child mental and physical health (range, 1-5, with higher score indicating better health).56,57,58 Caregivers also reported the number of days in the past 6 months the child had missed school, camp, or other activities owing to illness.59
Caregiver Physical and Mental Health
At baseline and 6-month follow-up, caregivers’ current and recent physical and mental health status was assessed using a single global health item from the Patient-Reported Outcomes Measurement System Global short form version 1.1 (range, 1-5, with higher score indicating better health), which has been sensitive to change in other intervention studies.60 Caregivers also completed the 4-item Perceived Stress Scale (range, 0-16, with higher score indicating more perceived stress)61,62 and the 8-item Patient Health Questionnaire (range, 0-24, with higher score indicating greater symptoms of depression).63
Sample Size
The initial target sample size was 724 dyads, selected as a conservative sample size to allow for 80% power to detect effects similar to our previous work,25 assuming 30% participant attrition. Owing to limitations in study funding, the study concluded with a sample of 611 dyads. The sample gave us approximately 80% power to detect small to medium standard effect sizes of 0.28 or greater between groups and effect sizes of 0.20 or greater to detect changes from preintervention to postintervention within each group.
Statistical Analysis
Baseline participant characteristics were compared between study groups and tested for significance using χ2 or t tests and appropriate nonparametric tests for nonnormally distributed continuous variables. The cumulative number of social risks and health outcomes were compared by group assignment using generalized linear models with a normal distribution with identity link for continuous outcomes, Poisson distribution with log link for count outcomes, and binomial distribution with logit link for binary outcomes. Hypothesis tests were 2-sided with P < .05 considered statistically significant. Unadjusted differences between groups are presented, and adjustment models built on each other, including (1) adjusted with baseline outcomes entered as covariates and (2) child and caregiver demographic factors (ie, age, gender, and race/ethnicity) entered as covariates. In post hoc secondary analyses, we examined change in outcomes from baseline to follow-up within each group. Statistical analyses were conducted using SPSS statistical software version 25 (IBM Corp). Data were analyzed from January 1, 2019, to January 20, 2020.
Results
Sample Characteristics
Of the 1222 families approached, 611 caregiver-child dyads were eligible and agreed to participate (Figure). Child mean (SD) age was 6.1 (5.0) years; 438 children (79.1%) were Hispanic; and 315 children (51.6%) were girls (Table 1). In total, 302 dyads were randomized to the written resources group and 309 dyads to the in-person assistance group. Attrition at follow-up was 27.8%, comparable to similar studies in safety-net settings,22,64,65 with no differences between groups. A total of 225 dyads in the written resource sheet group and 216 dyads in the in-person assistance group were included in 6-month follow-up (Figure). There were no statistically significant differences between participants with follow-up data vs participants who dropped out. Using multiple imputation models to estimate missing follow-up data, we also found no significant differences in the number of social risk factors or health measures between caregivers who reported follow-up data vs those who did not.
Table 1. Participant Characteristics at Baseline.
| Characteristic | No. (%) | |
|---|---|---|
| Resource Sheet (n = 302) | Resource Sheet With Navigator Intervention (n = 309) | |
| Child | ||
| Age, mean (SD), y | 6.1 (5.1) | 6.1 (4.9) |
| Girls | 152 (50.3) | 163 (52.8) |
| Race/ethnicity | ||
| Non-Hispanic white | 11 (3.6) | 9 (2.9) |
| Hispanic | 240 (79.5) | 243 (78.6) |
| Non-Hispanic black | 22 (7.2) | 32 (10.4) |
| Other or mixed | 29 (9.7) | 25 (8.1) |
| General health status rating, mean (SD)a | 3.6 (1.0) | 3.6 (1.0) |
| PedsQL functioning score, mean (SD)b | ||
| Physical | 82.8 (19.4) | 82.2 (20.6) |
| Emotional | 69.2 (23.4) | 70.7 (21.1) |
| Social | 82.2 (22.3) | 80.6 (22.2) |
| Cognitive | 84.3 (22.7) | 89.4 (17.4) |
| School | 73.5 (25.7) | 69.1 (26.4) |
| Missed school days, mean (SD) | 2.7 (3.1) | 2.7 (3.3) |
| Caregiver | ||
| Age, y | ||
| 18-24 | 38 (12.7) | 36 (11.7) |
| 25-34 | 109 (36.5) | 125 (40.6) |
| 35-44 | 117 (39.1) | 117 (38.0) |
| 45-74 | 35 (11.7) | 30 (9.7) |
| Relationship to child | ||
| Mother | 264 (87.5) | 276 (89.3) |
| Father | 27 (8.9) | 28 (9.1) |
| Other caregiver | 11 (3.6) | 5 (1.6) |
| Spanish-speaking | 224 (74.2) | 210 (68.0) |
| Race/ethnicity | ||
| Non-Hispanic white | 6 (2.0) | 12 (3.9) |
| Hispanic | 254 (84.1) | 247 (79.7) |
| Non-Hispanic black | 21 (7.0) | 34 (11.0) |
| Other or mixed | 21 (7.0) | 16 (5.4) |
| Education level | ||
| <High school | 162 (53.7) | 147 (47.8) |
| High school graduate or GED | 71 (23.5) | 101 (32.8) |
| Some college or college graduate | 69 (22.8) | 60 (19.4) |
| Household income <$35 000/y | 242 (89.6)c | 245 (87.8)d |
| Reported social risks, mean (SD), No.e | 4.1 (3.2) | 4.5 (3.1) |
| Self-rated general health status, mean (SD)f | 2.8 (0.9) | 2.8 (0.8) |
| Perceived Stress Scale score, mean (SD)g | 5.6 (3.2) | 5.8 (3.1) |
| Depression symptoms score, mean (SD)h | 6.4 (5.3) | 6.1 (4.8) |
Abbreviations: GED, general educational development; PedsQL, Pediatric Quality of Life Inventory.
Range, 1 to 5, with higher score indicating better health.
Range, 0 to 100, with higher score indicating higher quality of life.
Includes data for 270 dyads.
Includes data for 279 dyads.
Range, 0 to 18.
Measured using the Patient-Reported Outcomes Measurement System short form version 1.1 (range, 1-5, with higher score indicating better health).
Range, 0 to 16, with higher score indicating more perceived stress.
Measured using the 8-item Patient Health Questionnaire (range, 0-24, with higher score indicating greater symptoms of depression).
The number of social risks reported at baseline ranged from 0 to 18 of 18 total possible items, and the mean (SD) was 4.3 (3.2) risks (Table 2). Of the 611 dyads, 47 dyads (7.7%) endorsed no social risks and 310 dyads (50.7%) reported 4 or more risks. At baseline, most caregivers reported child global health as excellent (123 dyads [21.6%]), very good (167 dyads [27.4%]), or good (246 dyads [40.3%]), 51 caregivers (8.4%) reported their child’s health was fair, and 14 caregivers (2.3%) reported their child’s health was poor. Caregivers characterized their own global health more negatively: 25 caregivers (4.1%) reported their global health was excellent, and 69 caregivers (11.3%) reported their global health was very good, while 307 caregivers (50.3%) reported good health, 179 caregivers (29.3%) reported fair health, and 30 caregivers (4.9%) reported poor health. The total number of social risk factors reported was inversely associated with child baseline health indicators and caregiver baseline health indicators (r = −0.23; P < .001), with a greater total number of social risk factors significantly associated with worse child health (r = −0.15; P < .001) and caregiver health (r = −0.23; P < .001), greater caregiver perceived stress (r = 0.31; P < .001), more caregiver depressive symptoms (r = 0.35; P < .001), more missed school days (r = 0.15; P < .001), and lower functioning scores on multiple dimensions of the PedsQL (physical: r = −0.18; P < .001; emotional: r = –0.26; P < .001; social: r = –0.19; P < .001; school: r = –0.24; P < .001). Frequencies of each social risk at baseline and 6 months after the intervention are presented in Table 2.
Table 2. Caregiver-Reported Social Risk Factors at Baseline and 6-Month Follow-up Stratified by Intervention Group .
| Social Risk | Resource Sheet Group (n = 225) | Resource Sheet With In-Person Assistance Group (n = 216) | ||||||
|---|---|---|---|---|---|---|---|---|
| No. (%) | Change, % | P Value | No. (%) | Change, % | P Value | |||
| Baseline | 6 mo | Baseline | 6 mo | |||||
| Food insecurity | 88 (39.1) | 60 (26.6) | −12.4 | <.001 | 77 (35.8) | 51 (23.6) | −12.2 | <.001 |
| Unstable housing | 94 (41.7) | 47 (20.9) | −20.8 | <.001 | 76 (35.2) | 42 (19.4) | −15.7 | <.001 |
| Utility or telephone bills | 83 (36.8) | 51 (22.7) | −14.2 | <.001 | 81 (37.5) | 57 (26.4) | −11.1 | .004 |
| Housing quality | 61 (27.1) | 45 (20.0) | −7.1 | .03 | 78 (36.1) | 51 (23.8) | −12.3 | .001 |
| Difficulty finding job | 63 (28.0) | 34 (15.1) | −12.9 | <.001 | 64 (29.6) | 34 (15.7) | −13.9 | <.001 |
| Disability interfering with work | 37 (16.5) | 23 (10.2) | −6.3 | .02 | 29 (13.4) | 23 (10.6) | −2.8 | .35 |
| Problem with job | 12 (5.4) | 17 (7.6) | 2.2 | .41 | 23 (10.6) | 13 (6.0) | −4.6 | .10 |
| Difficulty with unemployment insurance | 19 (8.4) | 8 (3.6) | −4.9 | .03 | 16 (7.4) | 10 (4.6) | −2.8 | .24 |
| Denied income support programs | 29 (12.8) | 30 (13.4) | 0.6 | .99 | 43 (19.9) | 28 (12.9) | −7.0 | .049 |
| Health insurance | 45 (20.0) | 48 (21.3) | 1.3 | .77 | 53 (24.5) | 45 (20.9) | −3.6 | .35 |
| Primary care cliniciana | 24 (12.4) | 21 (10.9) | −1.6 | .78 | 30 (17.2) | 13 (7.5) | −9.7 | .007 |
| Medical or pharmacy bills | 35 (15.6) | 30 (13.3) | −2.2 | .55 | 46 (21.3) | 21 (9.8) | −11.5 | .001 |
| Afterschool activities | 58 (26.0) | 32 (14.3) | −11.7 | <.001 | 70 (32.4) | 20 (9.3) | −23.1 | <.001 |
| Childcarea | 46 (23.8) | 24 (12.5) | −11.3 | <.001 | 48 (27.5) | 21 (12.1) | −15.5 | <.001 |
| Bullying | 24 (10.6) | 19 (8.4) | −2.2 | .42 | 34 (15.7) | 21 (9.7) | −6.0 | .05 |
| Adult in household mental or behavioral health | 43 (19.1) | 23 (10.2) | −8.9 | .003 | 42 (19.4) | 30 (14.0) | −5.5 | .15 |
| Transportation | 68 (30.2) | 41 (18.3) | −11.9 | <.001 | 64 (29.6) | 37 (17.0) | −12.5 | <.001 |
| Other legal issues | 60 (26.8) | 46 (20.4) | −6.4 | .76 | 71 (33.0) | 52 (24.1) | −8.9 | .02 |
This item was added after initial study initiation. Data for families missing this item at baseline were not included in 6-month follow-up analyses for this social risk factor or for analyses examining total number of social risks.
In the in-person assistance group, caregivers met with navigators a mean of 4.34 (SD, 2.76; range, 0-10) times after the initial visit, and 1228 of 1289 visits (95.3%) were conducted by telephone. Visit duration ranged from 5 to 45 minutes. Forty-five dyads (14.4%) did not engage in any navigation follow-up, and 35 dyads (11.2%) engaged in 8 or more contacts.
Change in Social Risk Factors
There were no statistically significant differences between intervention groups in the number of social risk factors reported at follow-up with or without adjustment (Table 3). The number of successful navigator contacts was not significantly associated with decreases in number of social risks (r = −0.10; P = .15). In post hoc secondary analyses examining change within group, caregivers in the resource sheet group reported a significant decrease in number of social risks at 6-month follow-up relative to baseline with a mean (SE) difference of –1.28 (0.19) social risk factors (P < .001); caregivers in the in-person assistance intervention reported a mean (SE) change of –1.74 (0.21) social risk factors (P < .001) (Table 3). Among the individual social risk factors, significant improvement was seen on 13 of 18 risk factors within the in-person assistance intervention and 11 of 18 risk factors in the resource sheet intervention (Table 2). At follow-up, 192 caregivers in the resource sheet group (63.6%) and 191 caregivers in the in-person assistance group (61.8%) reported that their top social risk priority area was no longer an issue.
Table 3. Outcomes at 6-Month Follow-up Stratified by Intervention Group .
| Outcome | Resource Sheet, Mean (SE) | Resource Sheet With In-Person Assistance, Mean (SE) | Unadjusted Difference | Model 1 Adjusted Differencea | Model 2 Adjusted Differenceb | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 6 mo | Change | Baseline | 6 mo | Change | Mean (SE) [95% CI] | P Value | Mean (SE) [95% CI] | P Value | Mean (SE) [95% CI] | P Value | |
| Social risks endorsedc | 3.95 (0.21) | 2.66 (0.17) | −1.28 (0.19) | 4.37 (0.20) | 2.63 (0.20) | −1.74 (0.21) | −0.02 (0.16) [−0.28 to 0.33] | .86 | −0.19 (0.22) [−0.61 to 0.24] | .39 | −0.19 (0.22) [−0.62 to 0.23] | .92 |
| Child Health | ||||||||||||
| Child general health | 3.51 (0.07) | 3.88 (0.06) | 0.37 (0.07) | 3.53 (0.07) | 3.77 (0.06) | 0.24 (0.07) | 0.10 (0.09) [−0.07 to 0.27] | .25 | 0.11 (0.08) [−0.04 to 0.27] | .16 | 0.12 (0.09) [−0.04 to 0.27] | .13 |
| Pediatric Quality of Life Inventory scored | ||||||||||||
| Physical functioning | 82.97 (1.29) | 85.64 (1.28) | 2.67 (1.63) | 81.87 (1.36) | 84.18 (1.39) | 2.31 (1.71) | 1.26 (1.90) [−2.45 to 4.98] | .51 | 1.23 (1.85) [−2.41 to 4.87] | .51 | 1.58 (1.85) [−2.03 to 5.19] | .39 |
| Emotional functioning | 69.17 (1.57) | 74.99 (1.35) | 5.82 (1.37) | 70.19 (1.44) | 74.54 (1.23) | 4.35 (1.26) | 0.45 (1.83) [−3.15 to 4.03] | .81 | .94 (1.52) [−2.04 to 3.93] | .53 | 1.40 (1.51) [−1.55 to 4.26] | .35 |
| Social functioning | 81.87 (1.50) | 83.27 (1.34) | 1.39 (1.37) | 79.90 (1.54) | 80.58 (1.46) | 0.68 (1.74) | 2.68 (1.98) [−1.19 to 6.57] | .18 | 1.90 (1.79) [−1.61 to 5.42] | .29 | 2.20 (1.80) [−1.32 to 5.73] | .22 |
| Cognitive functioninge | 84.30 (3.10) | 88.76 (1.90) | 4.46 (2.89) | 90.14 (2.78) | 85.74 (3.21) | −4.29 (4.18) | 4.10 (3.58) [−2.91 to 11.12] | .25 | 4.06 (3.56) [−3.00 to 11.11] | .26 | 4.99 (3.56) [−1.99 to 11.96] | .16 |
| School functioningf | 73.86 (2.46) | 72.43 (2.38) | −1.42 (2.41) | 68.15 (2.31) | 71.31 (2.31) | 3.16 (2.52) | −0.41 (2.86) [−6.03 to 5.20] | .89 | −1.43 (2.99) [−7.32 to 4.47] | .63 | −0.49 (2.94) [−6.25 to 5.28] | .87 |
| Missed school or camp d in past 6 mo, No. | 2.82 (0.23) | 2.12 (0.20) | −0.70 (0.25) | 2.80 (0.24) | 2.38 (0.22) | −0.42 (0.22) | −0.36 (0.28) [−0.91 to 0.19] | .20 | −0.27 (0.31) [−0.79 to 0.27] | .31 | −0.27 (0.27) [−0.79 to 0.25] | .31 |
| Caregiver Health | ||||||||||||
| General health scoreg | 2.87 (0.06) | 3.00 (0.07) | 0.14 (0.07) | 2.80 (0.5) | 2.97 (0.6) | 0.17 (0.06) | 0.03 (0.09) [−0.14 to 0.22] | .68 | 0 (0.08) [−0.16 to 0.16] | .98 | −0.01 (0.08) [−0.17 to 0.15] | .90 |
| Perceived Stress Scale scoreh | 5.61 (0.21) | 5.02 (0.22) | −0.59 (0.21) | 5.73 (0.20) | 4.75 (0.21) | −0.99 (0.22) | 0.27 (0.30) [−0.87 to 0.31] | .36 | 0.34 (0.21) [−0.19 to 0.86] | .21 | 0.38 (0.27) [−0.90 to 0.15] | .16 |
| Depression symptoms scorei | 6.52 (0.36) | 4.82 (0.33) | −1.71 (0.31) | 5.96 (0.31) | 4.35 (0.29) | −1.60 (0.26) | 0.45 (0.45) [−0.42 to 1.33] | .30 | 0.13 (0.35) [−0.56 to 0.81] | .72 | 0.16 (0.34) [−0.51 to 0.83] | .63 |
Calculated as the difference between groups in the outcomes at 6-month follow-up after adjusting for baseline outcomes.
Adjusted for model 1 and additional baseline covariates.
Range, 0 to 18.
Range, 0 to 100, with higher score indicating higher quality of life.
Includes data for 102 children based on applicability to specific age groups.
Includes data for 246 children based on applicability to specific age groups.
Measured using the Patient-Reported Outcomes Measurement System short form version 1.1 (range, 1-5, with higher score indicating better health).
Range, 0-16, with higher score indicating more perceived stress.
Measured using the 8-item Patient Health Questionnaire (range, 0-24, with higher score indicating greater depression symptoms).
Change in Child Health
At follow-up, there were no statistically significant differences between intervention groups in the child health outcomes with or without adjustment (Table 3). Post hoc analyses indicated that caregiver report of child global health significantly improved (mean [SE]: written resources, 0.37 [0.07]; P < .001; in-person assistance, 0.24 [0.07]; P < .001). Similarly, both groups showed statistically significant improvement in caregiver report of children’s emotional functioning scores (mean [SE]: written resources, 5.82 [1.37]; P < .001; in-person assistance, 4.35 [1.26]; P < .001) and missed school or camp days (mean [SE]: written resources, −0.70 [0.25] days; P = .006; in-person assistance, −0.42 [0.22] days; P = .048) (Table 3). There were no significant changes in children’s physical, social, or cognitive or school functioning based on the PedsQL in either group.
Change in Caregiver Health
Similar to the child health measures, there were no statistically significant differences at follow-up in caregiver general health, depression symptoms, or perceived stress between intervention groups with or without adjustment (Table 3). Post hoc analyses indicated that at follow-up, caregivers in both interventions reported significant improvement in their own general health (mean [SE]: written resource, 0.14 [0.07]; P = .04; in-person assistance, 0.17 [0.07]; P = .005), decreases in their perceived stress (mean [SE]: written resource, −0.59 [0.21]; P < .001; in-person assistance, −0.99 [0.22]; P < .001), and decreases in their reported depressive symptoms (mean [SE]: written resource, −1.71 [0.31]; P < .001; in-person assistance, −1.60 [0.26]; P < .001). Limiting the in-person assistance analytic sample to participants with 1 or more successful postenrollment contacts with a navigator resulted in a nearly identical pattern of results.
Discussion
This medium-sized randomized clinical trial examined the effects of 2 clinical interventions designed to reduce families’ social and economic risks, a standardized handout that included information on available clinic, community, and government resources compared with the handout plus social services navigation assistance provided by a trained navigator for up to 3 months. There were no significant differences in the degree of change in social risk factors or child or caregiver health between the 2 interventions. Analyses within each trial arm showed significant decreases in reported social risk factors and improvements in both child and caregiver health from before to after the intervention. Social risk factors showing substantial reductions in both intervention groups included food insecurity, unstable or low-quality housing, problems paying bills, and difficulty affording transportation. These topics overlap with domains covered in common social risk screening tools endorsed by major professional organizations.66,67
There have been several other trials in pediatric settings that examine the effectiveness of multidomain social risk screening and interventions,22,23,24 although we are aware of only 1 that has included an intervention limited to providing written social resource information.25 In this randomized clinical trial, the lack of significantly greater benefit when adding longitudinal, in-person navigator services to the delivery of written social resources information was unexpected, given that an earlier trial in this area25 found significant differences between groups. Subtle but potentially important differences between these studies could help explain the disparate findings. It is possible that results of this study were affected by historical context,68 including increased federal immigration enforcement and anti-immigrant rhetoric. This might have lowered the likelihood of risk disclosure or assistance-seeking behaviors, although the interaction is unlikely to have differentially affected trial groups. A second difference between studies may be the quality of the information contained in the resource sheets. Handouts used in the prior trial25 relied on information developed by a county-contracted information and referral service and were updated only occasionally. In contrast, handouts used in this study were compiled by the navigators and included more regularly updated information about local social service providers. Handouts also incorporated 2 techniques recommended by the Agency for Healthcare Research and Quality to increase the usability of patient educational materials: adding contact names at relevant agencies and highlighting the resources most relevant to caregiver priorities.69 The provision of more up-to-date, targeted information may have increased the effect of the handouts in the written resources–only group of this trial relative to the effect in the prior trial.25 In brief, the greater the usefulness of the written resources, the less benefit may have been added by providing additional navigator services.
Limitations
There are multiple limitations of this study. First, the study was conducted in only 1 urgent care setting, and it is unclear whether our findings are generalizable to other locations and clinical settings. Second, 27.8% of study participants were lost to follow-up at 6 months. Notably, this represents less attrition than in comparable studies undertaken in low-resource settings.22,25,64,65 Moreover, attrition did not differ between study groups and was not associated with key participant characteristics. Third, it is possible that the gift cards provided as part of the study influenced the positive postintervention outcomes in each group, although these should not have influenced the primary null findings between groups. Fourth, the surveys are based on participant self-report; they are therefore subject to classic respondent bias, which could have included underreporting or overreporting of social risks or health status. Fifth, the study compared the effect of different doses of a clinic-based intervention needed to decrease social risks. It would have been desirable to have a no-treatment control group to determine whether either or both levels of intervention significantly improved outcomes compared with screened but untreated controls. We did not add this condition owing to ethical concerns about assessing social risks without responding to endorsed needs.
Conclusions
This randomized clinical trial of pediatric urgent care social risk interventions revealed no significant differences between provision of high-quality, personalized social service written information with vs without the addition of 1-on-1 longitudinal navigation services. The health care sector’s broad enthusiasm around activities to reduce patients’ social risks has contributed to an urgent need to identify effective and scalable interventions, particularly in pediatric settings where innovation in this area has outpaced the availability of evidence. However, counterbalancing this enthusiasm are the costs of screening and referral programs. The finding of this randomized clinical trial of pediatric urgent care social risk interventions should be encouraging to systems that are considering these kinds of programs. These findings suggest that a relatively low-dose and lower-cost intervention—high-quality, written information provided in the context of a single encounter—could be efficacious for pediatric populations, but similar interventions should be examined in studies designed to assess their effectiveness.
Trial Protocol
eAppendix. Social Risk Screening
Data Sharing Statement
References
- 1.National Forum on Early Childhood Policy and Programs, National Scientific Council on the Developing Child The foundations of lifelong health are built in early childhood. https://developingchild.harvard.edu/resources/the-foundations-of-lifelong-health-are-built-in-early-childhood/. Accessed July 19, 2019.
- 2.Shonkoff JP, Garner AS; Committee on Psychosocial Aspects of Child and Family Health; Committee on Early Childhood, Adoption, and Dependent Care; Section on Developmental and Behavioral Pediatrics . The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129(1):-. doi: 10.1542/peds.2011-2663 [DOI] [PubMed] [Google Scholar]
- 3.Meyers A, Cutts D, Frank DA, et al. Subsidized housing and children’s nutritional status: data from a multisite surveillance study. Arch Pediatr Adolesc Med. 2005;159(6):551-556. doi: 10.1001/archpedi.159.6.551 [DOI] [PubMed] [Google Scholar]
- 4.Black MM, Cutts DB, Frank DA, et al. ; Children’s Sentinel Nutritional Assessment Program Study Group . Special Supplemental Nutrition Program for Women, Infants, and Children participation and infants’ growth and health: a multisite surveillance study. Pediatrics. 2004;114(1):169-176. doi: 10.1542/peds.114.1.169 [DOI] [PubMed] [Google Scholar]
- 5.Wood PR, Smith LA, Romero D, Bradshaw P, Wise PH, Chavkin W. Relationships between welfare status, health insurance status, and health and medical care among children with asthma. Am J Public Health. 2002;92(9):1446-1452. doi: 10.2105/AJPH.92.9.1446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cook JT, Frank DA, Berkowitz C, et al. Welfare reform and the health of young children: a sentinel survey in 6 US cities. Arch Pediatr Adolesc Med. 2002;156(7):678-684. doi: 10.1001/archpedi.156.7.678 [DOI] [PubMed] [Google Scholar]
- 7.Fieldston ES, Zaniletti I, Hall M, et al. Community household income and resource utilization for common inpatient pediatric conditions. Pediatrics. 2013;132(6):e1592-e1601. doi: 10.1542/peds.2013-0619 [DOI] [PubMed] [Google Scholar]
- 8.Bauman LJ, Silver EJ, Stein RE. Cumulative social disadvantage and child health. Pediatrics. 2006;117(4):1321-1328. doi: 10.1542/peds.2005-1647 [DOI] [PubMed] [Google Scholar]
- 9.Secrest AM, Costacou T, Gutelius B, Miller RG, Songer TJ, Orchard TJ. Associations between socioeconomic status and major complications in type 1 diabetes: the Pittsburgh Epidemiology of Diabetes Complication (EDC) Study. Ann Epidemiol. 2011;21(5):374-381. doi: 10.1016/j.annepidem.2011.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Colvin JD, Zaniletti I, Fieldston ES, et al. Socioeconomic status and in-hospital pediatric mortality. Pediatrics. 2013;131(1):e182-e190. doi: 10.1542/peds.2012-1215 [DOI] [PubMed] [Google Scholar]
- 11.Wood DL, Valdez RB, Hayashi T, Shen A. Health of homeless children and housed, poor children. Pediatrics. 1990;86(6):858-866. [PubMed] [Google Scholar]
- 12.Alaimo K, Olson CM, Frongillo EA Jr. Food insufficiency and American school-aged children’s cognitive, academic, and psychosocial development. Pediatrics. 2001;108(1):44-53. [PubMed] [Google Scholar]
- 13.Advisory Committee on Childhood Lead Poisoning Prevention (ACCLPP) Recommendations for blood lead screening of young children enrolled in Medicaid: targeting a group at high risk. MMWR Recomm Rep. 2000;49(RR-14):1-13. [PubMed] [Google Scholar]
- 14.Beebe-Dimmer J, Lynch JW, Turrell G, Lustgarten S, Raghunathan T, Kaplan GA. Childhood and adult socioeconomic conditions and 31-year mortality risk in women. Am J Epidemiol. 2004;159(5):481-490. doi: 10.1093/aje/kwh057 [DOI] [PubMed] [Google Scholar]
- 15.Wise PH. Child poverty and the promise of human capacity: childhood as a foundation for healthy aging. Acad Pediatr. 2016;16(3)(suppl):S37-S45. doi: 10.1016/j.acap.2016.01.014 [DOI] [PubMed] [Google Scholar]
- 16.Larson K, Russ SA, Crall JJ, Halfon N. Influence of multiple social risks on children’s health. Pediatrics. 2008;121(2):337-344. doi: 10.1542/peds.2007-0447 [DOI] [PubMed] [Google Scholar]
- 17.COUNCIL ON COMMUNITY PEDIATRICS Poverty and child health in the United States. Pediatrics. 2016;137(4):e20160339. doi: 10.1542/peds.2016-0339 [DOI] [PubMed] [Google Scholar]
- 18.American Academy of Family Physicians The EveryONE Project toolkit. 2018; https://www.aafp.org/patient-care/social-determinants-of-health/everyone-project/eop-tools.html. Accessed July 19, 2019.
- 19.Daniel H, Bornstein SS, Kane GC; Health and Public Policy Committee of the American College of Physicians . Addressing social determinants to improve patient care and promote health equity: an American College of Physicians position paper. Ann Intern Med. 2018;168(8):577-578. doi: 10.7326/M17-2441 [DOI] [PubMed] [Google Scholar]
- 20.Ligon-Borden BL. Abraham Jacobi, MD: father of American pediatrics and advocate for children’s health. Semin Pediatr Infect Dis. 2003;14(3):245-249. doi: 10.1016/S1045-1870(03)00055-4 [DOI] [PubMed] [Google Scholar]
- 21.Beck AF, Cohen AJ, Colvin JD, et al. Perspectives from the Society for Pediatric Research: interventions targeting social needs in pediatric clinical care. Pediatr Res. 2018;84(1):10-21. doi: 10.1038/s41390-018-0012-1 [DOI] [PubMed] [Google Scholar]
- 22.Sege R, Preer G, Morton SJ, et al. Medical-legal strategies to improve infant health care: a randomized trial. Pediatrics. 2015;136(1):97-106. doi: 10.1542/peds.2014-2955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Garg A, Toy S, Tripodis Y, Silverstein M, Freeman E. Addressing social determinants of health at well child care visits: a cluster RCT. Pediatrics. 2015;135(2):e296-e304. doi: 10.1542/peds.2014-2888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Garg A, Butz AM, Dworkin PH, Lewis RA, Thompson RE, Serwint JR. Improving the management of family psychosocial problems at low-income children’s well-child care visits: the WE CARE Project. Pediatrics. 2007;120(3):547-558. doi: 10.1542/peds.2007-0398 [DOI] [PubMed] [Google Scholar]
- 25.Gottlieb LM, Hessler D, Long D, et al. Effects of social needs screening and in-person service navigation on child health: a randomized clinical trial. JAMA Pediatr. 2016;170(11):e162521. doi: 10.1001/jamapediatrics.2016.2521 [DOI] [PubMed] [Google Scholar]
- 26.Gottlieb L, Hessler D, Long D, Amaya A, Adler N. A randomized trial on screening for social determinants of health: the iScreen study. Pediatrics. 2014;134(6):e1611-e1618. doi: 10.1542/peds.2014-1439 [DOI] [PubMed] [Google Scholar]
- 27.Beck AF, Henize AW, Kahn RS, Reiber KL, Young JJ, Klein MD. Forging a pediatric primary care-community partnership to support food-insecure families. Pediatrics. 2014;134(2):e564-e571. doi: 10.1542/peds.2013-3845 [DOI] [PubMed] [Google Scholar]
- 28.Klein MD, Beck AF, Henize AW, Parrish DS, Fink EE, Kahn RS. Doctors and lawyers collaborating to HeLP children—outcomes from a successful partnership between professions. J Health Care Poor Underserved. 2013;24(3):1063-1073. doi: 10.1353/hpu.2013.0147 [DOI] [PubMed] [Google Scholar]
- 29.Garg A, Sarkar S, Marino M, Onie R, Solomon BS. Linking urban families to community resources in the context of pediatric primary care. Patient Educ Couns. 2010;79(2):251-254. doi: 10.1016/j.pec.2009.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Garg A, Marino M, Vikani AR, Solomon BS. Addressing families’ unmet social needs within pediatric primary care: the health leads model. Clin Pediatr (Phila). 2012;51(12):1191-1193. doi: 10.1177/0009922812437930 [DOI] [PubMed] [Google Scholar]
- 31.Dubowitz H, Feigelman S, Lane W, Kim J. Pediatric primary care to help prevent child maltreatment: the Safe Environment for Every Kid (SEEK) model. Pediatrics. 2009;123(3):858-864. doi: 10.1542/peds.2008-1376 [DOI] [PubMed] [Google Scholar]
- 32.Feigelman S, Dubowitz H, Lane W, Grube L, Kim J. Training pediatric residents in a primary care clinic to help address psychosocial problems and prevent child maltreatment. Acad Pediatr. 2011;11(6):474-480. doi: 10.1016/j.acap.2011.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dubowitz H, Lane WG, Semiatin JN, Magder LS, Venepally M, Jans M. The safe environment for every kid model: impact on pediatric primary care professionals. Pediatrics. 2011;127(4):e962-e970. doi: 10.1542/peds.2010-1845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dubowitz H, Lane WG, Semiatin JN, Magder LS. The SEEK model of pediatric primary care: can child maltreatment be prevented in a low-risk population? Acad Pediatr. 2012;12(4):259-268. doi: 10.1016/j.acap.2012.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fox CK, Cairns N, Sunni M, Turnberg GL, Gross AC. Addressing food insecurity in a pediatric weight management clinic: a pilot intervention. J Pediatr Health Care. 2016;30(5):e11-e15. doi: 10.1016/j.pedhc.2016.05.003 [DOI] [PubMed] [Google Scholar]
- 36.Fleegler EW, Lieu TA, Wise PH, Muret-Wagstaff S. Families’ health-related social problems and missed referral opportunities. Pediatrics. 2007;119(6):e1332-e1341. doi: 10.1542/peds.2006-1505 [DOI] [PubMed] [Google Scholar]
- 37.Cullen D, Woodford A, Fein J. Food for thought: a randomized trial of food insecurity screening in the emergency department. Acad Pediatr. 2019;19(6):646-651. doi: 10.1016/j.acap.2018.11.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Knowles M, Khan S, Palakshappa D, et al. Successes, challenges, and considerations for integrating referral into food insecurity screening in pediatric settings. J Health Care Poor Underserved. 2018;29(1):181-191. doi: 10.1353/hpu.2018.0012 [DOI] [PubMed] [Google Scholar]
- 39.Palakshappa D, Doupnik S, Vasan A, et al. Suburban families’ experience with food insecurity screening in primary care practices. Pediatrics. 2017;140(1):e20170320. doi: 10.1542/peds.2017-0320 [DOI] [PubMed] [Google Scholar]
- 40.Palakshappa D, Strane D, Griffis H, Fiks AG. Determining food-insecure families’ resource access with health system and public data. J Health Care Poor Underserved. 2019;30(1):265-279. doi: 10.1353/hpu.2019.0020 [DOI] [PubMed] [Google Scholar]
- 41.Sanders LM, Gershon TD, Huffman LC, Mendoza FS. Prescribing books for immigrant children: a pilot study to promote emergent literacy among the children of Hispanic immigrants. Arch Pediatr Adolesc Med. 2000;154(8):771-777. doi: 10.1001/archpedi.154.8.771 [DOI] [PubMed] [Google Scholar]
- 42.Silverstein M, Mack C, Reavis N, Koepsell TD, Gross GS, Grossman DC. Effect of a clinic-based referral system to head start: a randomized controlled trial. JAMA. 2004;292(8):968-971. doi: 10.1001/jama.292.8.968 [DOI] [PubMed] [Google Scholar]
- 43.Silverstein M, Iverson L, Lozano P. An English-language clinic-based literacy program is effective for a multilingual population. Pediatrics. 2002;109(5):E76-E6. doi: 10.1542/peds.109.5.e76 [DOI] [PubMed] [Google Scholar]
- 44.Sandel M, Sheward R, Ettinger de Cuba S, et al. Unstable housing and caregiver and child health in renter families. Pediatrics. 2018;141(2):e20172199. doi: 10.1542/peds.2017-2199 [DOI] [PubMed] [Google Scholar]
- 45.Weintraub D, Rodgers MA, Botcheva L, et al. Pilot study of medical-legal partnership to address social and legal needs of patients. J Health Care Poor Underserved. 2010;21(2)(suppl):157-168. doi: 10.1353/hpu.0.0311 [DOI] [PubMed] [Google Scholar]
- 46.Saxe-Custack A, LaChance J, Hanna-Attisha M, Ceja T. Fruit and vegetable prescriptions for pediatric patients living in Flint, Michigan: a cross-sectional study of food security and dietary patterns at baseline. Nutrients. 2019;11(6):E1423. doi: 10.3390/nu11061423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gottlieb LM, Wing H, Adler NE. A systematic review of interventions on patients’ social and economic needs. Am J Prev Med. 2017;53(5):719-729. doi: 10.1016/j.amepre.2017.05.011 [DOI] [PubMed] [Google Scholar]
- 48.Lindau ST, Makelarski JA, Abramsohn EM, et al. CommunityRx: A real-world controlled clinical trial of a scalable, low-intensity community resource referral intervention. Am J Public Health. 2019;109(4):600-606. doi: 10.2105/AJPH.2018.304905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.University of California, San Francisco ZSFG Health Advocates Program. https://healthadvocates.ucsf.edu/. Accessed July 19, 2019.
- 51.Varni JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care. 2001;39(8):800-812. doi: 10.1097/00005650-200108000-00006 [DOI] [PubMed] [Google Scholar]
- 52.Chan KS, Mangione-Smith R, Burwinkle TM, Rosen M, Varni JW. The PedsQL: reliability and validity of the short-form generic core scales and Asthma Module. Med Care. 2005;43(3):256-265. doi: 10.1097/00005650-200503000-00008 [DOI] [PubMed] [Google Scholar]
- 53.Varni JW, Limbers CA, Neighbors K, et al. The PedsQL Infant Scales: feasibility, internal consistency reliability, and validity in healthy and ill infants. Qual Life Res. 2011;20(1):45-55. doi: 10.1007/s11136-010-9730-5 [DOI] [PubMed] [Google Scholar]
- 54.Varni JW, Limbers CA, Burwinkle TM. Parent proxy-report of their children’s health-related quality of life: an analysis of 13,878 parents’ reliability and validity across age subgroups using the PedsQL 4.0 Generic Core Scales. Health Qual Life Outcomes. 2007;5:2. doi: 10.1186/1477-7525-5-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Varni JW, Limbers CA, Burwinkle TM. How young can children reliably and validly self-report their health-related quality of life: an analysis of 8,591 children across age subgroups with the PedsQL 4.0 Generic Core Scales. Health Qual Life Outcomes. 2007;5:1. doi: 10.1186/1477-7525-5-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Data Resource Center for Child and Adolescent Health National Survey of Children’s Health, 2011/12. https://www.childhealthdata.org/browse/survey/archive. Published 2012. Accessed July 19, 2019.
- 57.Minkovitz CS, O’Campo PJ, Chen YH, Grason HA. Associations between maternal and child health status and patterns of medical care use. Ambul Pediatr. 2002;2(2):85-92. doi: [DOI] [PubMed] [Google Scholar]
- 58.Monette S, Séguin L, Gauvin L, Nikiéma B. Validation of a measure of maternal perception of the child’s health status. Child Care Health Dev. 2007;33(4):472-481. doi: 10.1111/j.1365-2214.2006.00713.x [DOI] [PubMed] [Google Scholar]
- 59.Fowler MG, Johnson MP, Atkinson SS. School achievement and absence in children with chronic health conditions. J Pediatr. 1985;106(4):683-687. doi: 10.1016/S0022-3476(85)80103-7 [DOI] [PubMed] [Google Scholar]
- 60.Schalet BD, Hays RD, Jensen SE, Beaumont JL, Fries JF, Cella D. Validity of PROMIS physical function measured in diverse clinical samples. J Clin Epidemiol. 2016;73:112-118. doi: 10.1016/j.jclinepi.2015.08.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Cohen S, Janicki-Deverts D. Who’s stressed? Distributions of psychological stress in the United States in probability samples from 1983, 2006, and 2009. J Appl Soc Psychol. 2012;42(6):1320-1334. doi: 10.1111/j.1559-1816.2012.00900.x [DOI] [Google Scholar]
- 62.Warttig SL, Forshaw MJ, South J, White AK. New, normative, English-sample data for the Short Form Perceived Stress Scale (PSS-4). J Health Psychol. 2013;18(12):1617-1628. doi: 10.1177/1359105313508346 [DOI] [PubMed] [Google Scholar]
- 63.Kroenke K, Spitzer RL, Williams JB, Löwe B. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: a systematic review. Gen Hosp Psychiatry. 2010;32(4):345-359. doi: 10.1016/j.genhosppsych.2010.03.006 [DOI] [PubMed] [Google Scholar]
- 64.Katz KS, El-Mohandes PA, Johnson DM, Jarrett PM, Rose A, Cober M. Retention of low income mothers in a parenting intervention study. J Community Health. 2001;26(3):203-218. doi: 10.1023/A:1010373113060 [DOI] [PubMed] [Google Scholar]
- 65.Krieger JW, Takaro TK, Song L, Weaver M. The Seattle-King County Healthy Homes Project: a randomized, controlled trial of a community health worker intervention to decrease exposure to indoor asthma triggers. Am J Public Health. 2005;95(4):652-659. doi: 10.2105/AJPH.2004.042994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Alley DE, Asomugha CN, Conway PH, Sanghavi DM. Accountable Health Communities—addressing social needs through Medicare and Medicaid. N Engl J Med. 2016;374(1):8-11. doi: 10.1056/NEJMp1512532 [DOI] [PubMed] [Google Scholar]
- 67.National Association of Community Health Centers, Association of Asian Pacific Community Health Organizations, Oregon Primary Care Association, Institute for Alternative Futures Protocol for Responding to and Assessing Patients’ Assets, Risks, and Experiences (PRAPARE). http://www.nachc.org/research-and-data/prapare/. Accessed July 18, 2019.
- 68.Campbell DT, Stanley JC. Experimental and Quasi-experimental Designs for Research. Chicago, IL: R. McNally; 1963. [Google Scholar]
- 69.Agency for Healthcare Research and Quality Health Literacy Universal Precautions Toolkit, 2nd edition. https://www.ahrq.gov/health-literacy/quality-resources/tools/literacy-toolkit/healthlittoolkit2-tool12.html. Accessed July 19, 2019.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol
eAppendix. Social Risk Screening
Data Sharing Statement