Abstract
Introduction
People with cystic fibrosis (CF) are living longer, thus complications associated with age, such as hemoptysis, are increasing. The Institute of Medicine has emphasized the importance of patient‐centeredness. Although guidelines about hemoptysis in people with CF are available, these focus on management of the complication and not the patient perspective.
Objective
We sought to understand hemoptysis from the point of view of those who have experienced it.
Methods
We fielded an 11‐question survey to adults with CF and asked those who had hemoptysis to respond. Four questions had open‐ended options: (1) the person’s first experience with hemoptysis, (2) how that experience affected the way they approach their CF, (3) how they deal with hemoptysis when it occurs outside the home and (4) a free text box for general comments.
Results
Thirty‐one of 132 adults with CF who were sent a survey completed it (23% response rate); 63% F), indicated that they had experienced hemoptysis and described their triggers. In response to open questioning, 77% of respondents found their first experience with hemoptysis to be ‘scary,’ ‘frightening,’ ‘worrying’ or ‘jarring.’ Half of respondents reported quality of life being negatively affected by worsening stress or anxiety, fear of bleeding in public or other life impacts.
Conclusions
Focusing on how to cope with future episodes of hemoptysis and the associated anxiety can be helpful to patients. Proactive communication and sensitivity to patient experience may deepen physician‐patient rapport, increase self‐efficacy to cope with future episodes and lead to more comprehensive care of hemoptysis.
Keywords: anxiety, cystic fibrosis, Hemoptysis, patient experience
1. INTRODUCTION
People with cystic fibrosis (CF) are living longer, thus complications associated with age, such as hemoptysis, are increasing.1 Episodes of hemoptysis are acute and occasionally can cause respiratory compromise. They usually occur in patients with severe CF lung disease but can be seen in those with mild to moderate airways obstruction and can be categorized as mild, moderate or severe.2
Families of people with CF assisted the CF Foundation (CFF) to develop consensus guidelines about hemoptysis, however these focused on management of this complication and not patient perspective.3 The Institute of Medicine has emphasized the importance of patient‐centeredness.4 We sought to understand hemoptysis from the point of view of those who have experienced it.
2. MATERIALS AND METHODS
The CFF’s Community Voice program incorporates the life experiences of people with CF and their family members into CFF activities through participation in options such as anonymous surveys, focus groups or committees.5 It includes members from all 50 states. Along with general demographic information, members indicate their interests and preferences when they sign up. In September 2017, a survey was distributed to adults with CF who were members of Community Voice to report their experiences with hemoptysis. This survey was initiated as a response to a physician‐written CFF blogpost6 that elicited an unexpected response from the larger CF community, suggesting that the blogpost did not reflect the real‐life experience of hemoptysis.
We fielded an 11‐question survey (SurveyMonkey, San Mateo, CA; see online supplement). Four questions had open‐ended options: (1) the person’s first experience with hemoptysis, (2) how that experience affected the way they approach their CF, (3) how they deal with hemoptysis when it occurs outside the home and (4) a free text box for general comments. Responses were anonymous unless those completing the survey chose to identify themselves.
The stated purpose of the survey was to inform a new blogpost that would represent the perspective of those who have hemoptysis, not to conduct a research study, thus consent for academic publication was not obtained. However, after results were available they revealed a perspective that had not previously been published, either in our blogpost or in the medical literature.
3. RESULTS
In September of 2017, there were 265 adults with CF in Community Voice. The survey was sent to the 132 adults with CF who indicated that they were comfortable sharing their individual experiences with CF. The survey was in the field between 9/8/2017 and 9/14/2017. Thirty‐one members responded (23% response rate). For demographics see Table 1a and b. Reported triggers are in Figure 1. Many people were performing everyday tasks when hemoptysis first occurred (ie, lying down, traveling, on vacation). In response to open questioning, 20 of 26 respondents (77%) found their first experience with hemoptysis to be ‘scary,’ ‘frightening,’ ‘worrying’ or ‘jarring’. In unprompted responses, 13 of 26 (50%) indicated they called their doctor, were seen in the emergency department or were already hospitalized. Four respondents (25%) noted that the response from their care provider calmed them down. Half of respondents reported quality of life being negatively affected by worsening stress or anxiety, fear of bleeding in public or other life impacts (career, travel, exercise, etc.). Of those who did adapt their lives, key themes were diminished activity, less travel, modification of work schedules and most notably, worsening stress or anxiety. Some respondents broadly called for more research while others specifically mentioned a desire for research on links between hemoptysis and aspergillus, menstruation and mental health. A sample of verbatim responses is in Table 2.
Table 1.
Demographics
| n | |
|---|---|
| a. Gender | |
| Male | 7 |
| Female | 20 |
| Not answered | 5 |
| b. Age range (years) | |
| <25 | 5 |
| 26‐35 | 11 |
| 36‐45 | 7 |
| 46+ | 2 |
| Not answered | 7 |
Figure 1.
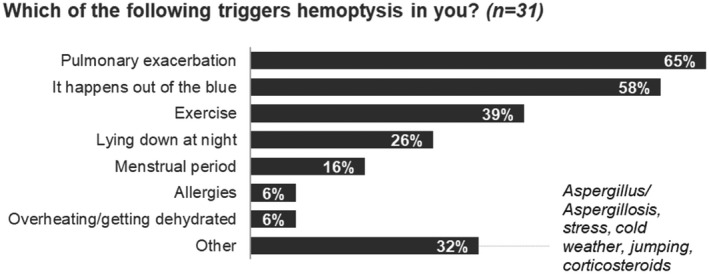
Patient‐reported triggers of hemoptysis. Responses are non‐exclusive.
Table 2.
Notable verbatim responses to open‐ended questions about hemoptysis
| Please describe your first experience with hemoptysis, including your initial reaction |
| It must have been a few years ago, but I laid down quickly or jumped onto my bed (or something) and I experienced a crackly sensation in my chest. I coughed and sure enough, little spatters of red came out. Not a lot, but enough to freak me out. |
| My experience with hemoptysis has all been blood stained or streaked mucus. My initial reaction is always a moment of panic |
| I was in the shower. I remember feeling an odd sort of gurgling feeling in my lungs, something I had never experienced before. I started coughing and could taste the blood. I spit it onto the shower floor and was shocked at the bright red color. Initially I was scared and anxious. I reached out to a friend with CF who had experienced this before and paged my CF doctor |
| I first hemoptysized (sic) 17 years ago and many times since. Whether it’s the first time or the 75th time, it’s always jarring because you don’t know if it will be an isolated incident or something bigger |
| The first time it happened I was in the hospital with very low lung function and had a severe coughing fit. I got really worried until my doctor told me it was common in people with cf. |
| Has your experience with hemoptysis affected how you approach your CF? |
| Not necessarily, but it is a very striking visual reminder of the damage that is occurring invisibly in the lungs. It’s a reminder of how real cystic fibrosis is. |
| My passion in life is travel, and I’m terrified to get in an airplane for fear that perhaps I’ll cough up blood and I won’t have access to an interventional radiologist to save my life… |
| More cautious and watchful when having excruciating coughing spells. Limit NSAIDs and corticosteroids |
| Hemoptysis reminds me that my CF needs extra attention. I try to do all of my treatments, eat plenty of calories for good nutrition, and exercise. I guess it forces me to realize my condition is serious and taking care of my health has to come before everything else in my life |
| Makes my mental health awful, makes me scared to do treatments full force, limits my exercise |
| Has hemoptysis affected life outside your home? If so, how? |
| I started coughing up some blood in a rest stop bathroom and it makes me very anxious, when I got back into the car, I had to explain to my friend I needed some time to relax before driving again. For me, I take deep breathes and stop moving until the crackling/blood stops. |
| Yes, scary and embarrassing when it happens in public |
| Every time it happened, I just stopped and prayed. I got lucky that it never occurred while I was teaching, but I think I would have excused myself. Sometimes it got really messy, and I would have been terrified of scaring my students. It did occur while I was at events or out an about and I always let the people I was with know what was happening and then tried to find a place to go to sit‐bathroom, etc |
| Absolutely. I love to travel – it’s my reason for living. And I’m terrified to get on a plane in fear that I’ll have a major episode (my FEV1 is 77% btw) and I won’t have access to an interventional radiologist to be embolized. I have panic attacks from PTSD from coughing up blood for 15+ years with no answers as to why, no research, but knowing that CFer’s die from this every year |
| I am less active |
| Yes, it has made me have to miss work and not work as much |
| Made me develop severe anxiety |
| Would you like to share anything else? |
| Please research this more. From the pulmonary and mental perspectives |
| Even after my procedure I still experience hemoptysis and my doctor has no idea why which makes it quite scary |
| After the first time I coughed up blood, my doc told me what a frank episode of hemoptysis at home could be worst case. He told me what to do and how to do it and where to go. As I had more episodes of coughing up streaks or clots of blood, he reiterated his information. By the time I did cough up frank blood (no mucus) at home, I was able to be fairly calm and knew what to do, because he’d been preparing me. I am so thankful for that approach. I feel empowered rather than afraid |
| Underlying causes of hemoptysis should be explored more. Physicians focus on the ‘traditional CF organisms’ such as pseudomonas as being the culprit. Fungus is often overlooked, especially when a normal IgE is present. I am living proof that someone with CF can in fact have invasive aspergillosis without ABPA. I am also proof that an FEV1 in the 90s does not exempt someone with CF from nearly dying from an untreated fungal infection due to massive hemoptysis |
4. DISCUSSION
Anxiety is a significant issue for people with CF.7 Our survey results indicate that episodes of hemoptysis can contribute to worsening anxiety at the time of the event and in anticipation of future events. Even if future events cannot be predicted and medical management is based primarily on consensus, understanding the perception of the person who experiences hemoptysis may lead clinicians to ask about and consider management of anxiety as an adjunctive support.
Recognizing the distress caused by hemoptysis and communicating sympathetically can be supportive therapy in and of itself. In an older review, the quality of communication both in the history‐taking segment of visits and during discussion of the management plan was found to influence patient health outcomes.8 More recently, a review of studies that focused on communication methods to improve patients’ and families’ understanding of medical conditions and treatment decisions and found a range of positive effects.9 However, the focus of these studies was a traditional medical model of increasing patient and family knowledge‐based on physician expertise, not patient experience.
Proactive communication about future events may be helpful. One community member’s physician recommended these steps,10 which she found helpful:
If you’re home, stop your treatments until you call us. We can help you figure out a game plan.
Spit into a cup, so you can estimate the amount of blood you’re bringing up and how quickly.
If you’re bringing up too much blood too quickly to measure, call an ambulance and try to lie with the lung you suspect is bleeding facing the floor.
In addition, community members would like to encourage more research focused on hemoptysis. A better understanding of the triggers of hemoptysis may also help to alleviate anxiety.
The results presented here are limited by the small sample size and overrepresentation of females. Recent hemoptysis has been reported to be associated with higher levels of anxiety in females but not males.11 Additionally, as noted above, our survey was designed to elicit information to answer a community concern and was not a formal research study.
Many of the adults with CF who responded to this survey noted that their first episode of hemoptysis was an emotionally traumatic event. Awareness of and a focus on the anxiety associated with hemoptysis can be helpful to patients. Sensitivity to patient experience may deepen physician‐patient rapport, increase self‐efficacy to cope with future episodes and lead to more comprehensive care of hemoptysis.
CONFLICT OF INTEREST
None of the authors have conflicts of interest to declare.
AUTHOR CONTRIBUTIONS
CMR: Survey concept and design; assisted in collecting and analyzing data; manuscript preparation and review.
HCL: Assisted in analyzing data; manuscript review.
EA: Survey concept and design; assisted in collecting and analyzing data; manuscript review.
RJF: Assisted with survey concept; assisted in analyzing data; manuscript review.
QTT: Survey concept and design; assisted in analyzing data; manuscript review.
DB: Wrote first draft, coordinated reviews.
ETHICS
We took two steps to assure the ethics of publication of results. The first was to query all members of Community Voice (not just those who had experienced hemoptysis) during a general end‐of‐the‐year survey to gauge their attitude towards publication of results; none of the 94 respondents objected to sharing survey results in an academic publication. The second was to obtain a formal Ethics Consultation through the Treuman Katz Center for Pediatric Bioethics, Seattle Children’s Hospital Institute for Translational Health Services (Seattle WA) and all recommendations have been implemented (available upon request).
Supporting information
ACKNOWLEDGMENT
The authors would like to thank the adults with cystic fibrosis and cystic fibrosis family members across the United States for sharing their insights through Community Voice, especially those who completed this survey.
Romàn CM, Loughlin HC, Aliaj E, Fay RJ, Tran QT, Borowitz D. Hemoptysis from the perspective of people with cystic fibrosis. Clin Respir J. 2020;14:299–303. 10.1111/crj.13132
REFERENCES
- 1. Cystic Fibrosis Foundation Patient Registry . 2016 Annual Data Report. Bethesda, MD: ©2017 Cystic Fibrosis Foundation; https://www.cff.org/Research/Researcher-Resources/Patient-Registry/2018-Patient-Registry-Annual-Data-Report.pdf. Accessed December 17, 2019. [Google Scholar]
- 2. Flume PA, Yankaskas JR, Ebeling M, Hulsey T, Clarke LL. Massive hemoptysis in cystic fibrosis. Chest. 2005;128:729‐738. [DOI] [PubMed] [Google Scholar]
- 3. Flume PA, Mogayzel PJ Jr., Robinson KA, Rosenblatt RL, Quittell L, Marshall BC. Clinical practice guidelines for pulmonary therapies committee; cystic fibrosis foundation pulmonary therapies committee. Cystic fibrosis pulmonary guidelines: pulmonary complications: hemoptysis and pneumothorax. Am J Respir Crit Care Med. August 1, 2010;182(3):298‐306. [DOI] [PubMed] [Google Scholar]
- 4. Committee on Quality Health Care in America, Institute of Medicine . Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; March 2001; Qual Lett Healthc Lead. 13(3):14‐5. [Google Scholar]
- 5. https://www.cff.org/Get-Involved/Community/Community-Voice/. Accessed December 17, 2019.
- 6. https://www.cff.org/CF-Community-Blog/Posts/2017/Setting-the-Record-Straight-About-Coughing-Up-Blood/. Accessed December 17, 2019.
- 7. Quittner AL, Goldbeck L, Abbott J, et al. Prevalence of depression and anxiety in patients with cystic fibrosis and parent caregivers: results of The International Depression Epidemiological Study across nine countries. Thorax. 2014;69:1090‐1097. [DOI] [PubMed] [Google Scholar]
- 8. Stewart MA. Effective physician‐patient communication and health outcomes: a review. Can Med Assoc J. 1995;152(9):1423: ‐1433. [PMC free article] [PubMed] [Google Scholar]
- 9. Fawole OA, Dy SM, Wilson RF, et al. A systematic review of communication quality improvement interventions for patients with advanced and serious illness. J Gen Intern Med. 2012;28(4):570‐577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. https://www.cff.org/CF-Community-Blog/Posts/2018/What-To-Do-Before-You-Start-Coughing-Up-Blood/. Accessed December 17, 2019.
- 11. Duff AJ, Abbott J, Cowperthwaite C, et al. Depression and anxiety in adolescents and adults with cystic fibrosis in the UK: a cross‐sectional study. J Cyst Fibros. December 2014;13(6):745‐753. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


