Summary
The multidisciplinary International Committee for the Advancement of Procedural Sedation presents the first fasting and aspiration prevention recommendations specific to procedural sedation, based on an extensive review of the literature. These were developed using Delphi methodology and assessment of the robustness of the available evidence. The literature evidence is clear that fasting, as currently practiced, often substantially exceeds recommended time thresholds and has known adverse consequences, for example, irritability, dehydration and hypoglycaemia. Fasting does not guarantee an empty stomach, and there is no observed association between aspiration and compliance with common fasting guidelines. The probability of clinically important aspiration during procedural sedation is negligible. In the post‐1984 literature there are no published reports of aspiration‐associated mortality in children, no reports of death in healthy adults (ASA physical status 1 or 2) and just nine reported deaths in adults of ASA physical status 3 or above. Current concerns about aspiration are out of proportion to the actual risk. Given the lower observed frequency of aspiration and mortality than during general anaesthesia, and the theoretical basis for assuming a lesser risk, fasting strategies in procedural sedation can reasonably be less restrictive. We present a consensus‐derived algorithm in which each patient is first risk‐stratified during their pre‐sedation assessment, using evidence‐based factors relating to patient characteristics, comorbidities, the nature of the procedure and the nature of the anticipated sedation technique. Graded fasting precautions for liquids and solids are then recommended for elective procedures based upon this categorisation of negligible, mild or moderate aspiration risk. This consensus statement can serve as a resource to practitioners and policymakers who perform and oversee procedural sedation in patients of all ages, worldwide.
Keywords: fasting, NPO guidelines, procedural sedation, pulmonary aspiration
Recommendations for best clinical practice
- In these first fasting and aspiration prevention recommendations specific to procedural sedation, we present a consensus‐derived algorithm (Fig. 1) to guide the management of patients of all ages undergoing procedural sedation.
Figure 1.
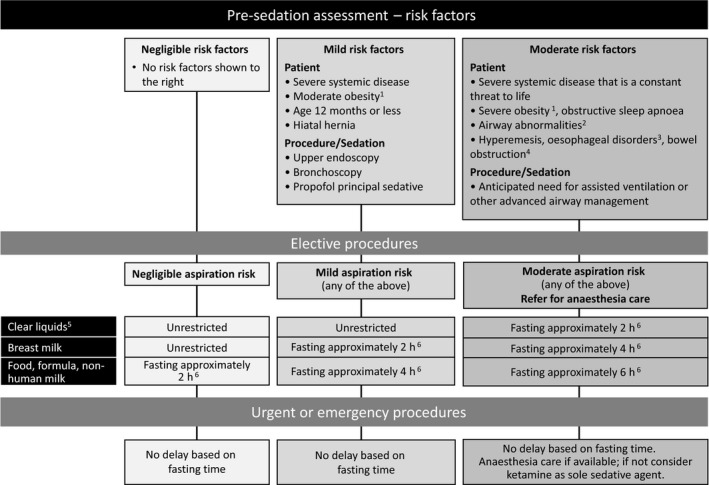 Algorithm linking risk stratification and fasting guidance. Notes: (1) Suggested definitions for moderate obesity are a body mass index (BMI) of 30–39 kg.m−2 in adults or from the 85th up to the 95th BMI percentile based on age/sex in a child, and for severe obesity a BMI of 40 kg.m−2 or higher in an adult or at the 95th percentile or greater in a child. (2) Includes micrognathia, macroglossia and laryngomalacia; (3) Includes gastroparesis, achalasia, atresia, stricture and tracheoesophageal fistula; (4) Includes ileus, pseudo‐obstruction, pyloric stenosis and intussusception. (5) Clear liquids are generally considered to include water, fruit juices without pulp, clear tea, black coffee and specially prepared carbohydrate‐containing fluids. (6) Fasting intervals are not absolute, with exceptions permissible when the volumes of oral intake are minor, or the fasting time reasonably close.
Algorithm linking risk stratification and fasting guidance. Notes: (1) Suggested definitions for moderate obesity are a body mass index (BMI) of 30–39 kg.m−2 in adults or from the 85th up to the 95th BMI percentile based on age/sex in a child, and for severe obesity a BMI of 40 kg.m−2 or higher in an adult or at the 95th percentile or greater in a child. (2) Includes micrognathia, macroglossia and laryngomalacia; (3) Includes gastroparesis, achalasia, atresia, stricture and tracheoesophageal fistula; (4) Includes ileus, pseudo‐obstruction, pyloric stenosis and intussusception. (5) Clear liquids are generally considered to include water, fruit juices without pulp, clear tea, black coffee and specially prepared carbohydrate‐containing fluids. (6) Fasting intervals are not absolute, with exceptions permissible when the volumes of oral intake are minor, or the fasting time reasonably close. In the algorithm, each patient is first risk‐stratified during their pre‐sedation assessment using evidence‐based factors relating to patient characteristics, comorbidities, the nature of the procedure and the nature of the anticipated sedation technique.
Graded fasting precautions for liquids and solids are then recommended for elective procedures based on this assessment of negligible, mild or moderate aspiration risk.
What other guideline statements are available on this topic?
Several anaesthetic, paediatric and dental specialty societies have issued fasting guidelines for elective general anaesthesia and have extrapolated these recommendations to procedural sedation.
Why was this statement developed?
Procedural sedation differs from general anaesthesia in important ways and, accordingly, the committee chose to focus specifically upon procedural sedation.
How does this statement differ from existing guidelines?
This statement presents the first fasting and aspiration prevention recommendations specific to procedural sedation.
Introduction
Procedural sedation is widely performed throughout the world to attenuate pain and anxiety in patients of all ages who undergo diagnostic and therapeutic procedures. These include: fracture reduction; abscess drainage; radiographic imaging; bone marrow aspiration; dental extraction; gastro‐intestinal endoscopy; and neurological diagnostic examinations. Pulmonary aspiration is a rare but potentially life‐threatening complication of procedural sedation. In the hope of reducing such a risk, a period of fasting is typically recommended before these procedures, whenever possible. Fasting intervals identical to those recommended before elective anaesthesia were specified in the first procedural sedation guidelines in 1985 1 and are still authoritatively recommended 2, 3, 4, 5, 6, 7, 8, 9 and widely practised. With respect to pre‐procedural fasting and aspiration risk, sedation and general anaesthesia have historically been viewed on equal terms. Although sedation and anaesthesia are a continuum, it is not clear that the same set of fasting intervals should necessarily be equally applicable to all sedation depths, sedation durations, procedure types and patient conditions or comorbidities. Procedural sedation intentionally targets a state in which protective airway reflexes are retained, while general anaesthesia denotes a state in which they are, by definition, absent. With sedation the procedures are often brief, there is far less active airway manipulation, and potentially emetogenic inhalational anaesthetic drugs are not routinely used. As a result, the aspiration risk for procedural sedation is almost certainly less than that of general anaesthesia (as discussed later in this article), 10, 11, 12, 13 and, in the three decades since those original sedation guidelines were introduced, there has been important research to better clarify the relative magnitude and nature of such a risk. The International Committee for the Advancement of Procedural Sedation (ICAPS, http://www.proceduralsedation.org) is an international and independent consensus committee of prominent sedation researchers whose collective expertise spans patients of all ages and a diverse range of specialties and practice settings. We aimed to develop recommendations for fasting and aspiration prevention specific to procedural sedation, applicable to patients of all ages. We did not aim to produce recommendations for general anaesthesia.
Methods
In developing this statement we adhered to the principles and methodology advocated by the US Institute of Medicine (now the National Academy of Medicine) 14. First, we identified six specific questions to address, as presented later in this document. A medical librarian conducted a search of PubMed, Web of Science and the Cochrane Library from January 1985 to 14 August 2019, limited to human subjects and the English language. Our specific search strategy in PubMed was: (sedation [tiab] OR ‘monitored anesthesia care’ [tiab]) AND aspiration [All Fields] AND ‘humans’ [MeSH Terms], and for the other two sources was: (sedation OR ‘monitored anesthesia care’) AND aspiration. We searched references of pertinent articles identified by our search strategy for additional relevant papers. We selected publications with an emphasis on the past 10 years, but we did not exclude commonly referenced and influential older publications. Seventeen out of the 20 ICAPS members agreed to participate in this project, and all had full access to the search results and articles identified.
We defined procedural sedation as “the use of anxiolytic, sedative, analgesic or dissociative drugs to attenuate pain, anxiety and motion to facilitate the performance of a necessary diagnostic or therapeutic procedure, provide an appropriate degree of amnesia or decreased awareness and ensure patient safety” 15, 16, 17. We considered only procedural sedation performed outside the operating room administered with the intent of maintaining the patient's own airway (i.e. without tracheal intubation or supraglottic, oropharyngeal or nasophayryngeal airways). Pulmonary aspiration is defined as “inhalation of oropharyngeal or gastric contents into the larynx and lower respiratory tract” 18. Aspiration pneumonitis is defined as an “event where emesis was noted or food material was found in the oral/pharyngeal cavity—associated with any or the following: new cough, wheeze, increase in respiratory effort, change in chest radiograph indicative of aspiration or new need for oxygen therapy after recovery from sedation” 19.
A subcommittee drafted summaries of literature evidence for six specific questions pertinent to this topic, and tentatively expressed its confidence in the evidence available using the four‐point nomenclature of the Grading of Recommendations Assessment, Development and Evaluation (GRADE) Working Group (http://www.gradeworkinggroup.org): high: further research very unlikely to change confidence in result; moderate: further research likely to have important impact on confidence, may change estimate of effect; low: further research very likely to have important impact on confidence in estimate of effect, may change estimate of effect; and very low: any estimate of effect is uncertain (includes expert opinion, no direct research evidence).
Although the focus of this statement is procedural sedation specifically, the general anaesthesia context is highly relevant. Accordingly, when appropriate, we sought and appraised the general anaesthesia evidence for the topic (the findings are presented in the online Supplementary Material); in the main document, we provide the corroborating or contrasting evidence for procedural sedation. Our committee then reviewed these summaries and initiated a sequential consensus generation process using the Delphi method. Specifically, we conducted an iterative series of document reviews that took place over a period of 16 months, with a later additional cycle following peer review. After each round, the anonymised responses from all members were displayed to all. Committee members could then revise their earlier responses based upon ongoing feedback, with our co‐chairs serving as moderators to guide the direction of consensus.
Participants graded each item using a 5‐point Likert scale: ‘strongly disagree’, ‘disagree’, ‘no strong opinion’, ‘agree’ or ‘strongly agree’. We defined agreement a priori as at least 80% of respondents choosing ‘agree’ or ‘strongly agree’. If at least 90% of respondents chose ‘agree’ or ‘strongly agree’, this was considered ‘strong consensus’. Once we achieved consensus on the evidentiary statements, we then used these literature summaries to generate, debate and refine a list of essential facts to guide the generation of recommendations. We then drafted, debated and refined the recommendations themselves, again with sequential Delphi review. We chose to use an algorithmic format to provide optimal clarity and practicality for clinicians.
The resulting provisional statement was then submitted for external review to professional societies from multiple specialties and nationalities, and other organisations with special interest in procedural sedation (http://proceduralsedation.org/liaisons/). Our members then reviewed the provisional document in light of this outside feedback, with additional revision and Delphi review.
Results
We attained ‘strong consensus’ on all statement elements (see also Supporting Information, Table S1).
Question 1: Is there a difference in the incidence and outcome of pulmonary aspiration events between patients who receive general anaesthesia and those who undergo procedural sedation, and are the associated risks different between the two?
There are theoretical and practical reasons why the risk of aspiration during sedation is almost certainly lower than that during general anaesthesia. First, unconsciousness without response to painful stimuli is not a targeted endpoint in either ‘moderate’ 6, 7, 11, 16, 17 or ‘deep’ 6, 7, 11, 16, 17 sedation. Although non‐responsiveness is typical with ketamine, this unique dissociative state helps maintain protective airway reflexes, and aspiration has not been previously reported with ketamine monotherapy except in compromised neonates 20, 21. Accordingly, protective airway reflexes should be more consistently retained with moderate, deep and dissociative sedation than during general anaesthesia, in which complete or substantial loss of protective airway reflexes is implicit. Second, most elective sedations are performed on patients who are generally healthy in spite of their active procedural indication. Greater patient comorbidities have been identified as a risk factor for aspiration in both adults 22, 23, 24 and children 25, 26. In many or most settings, ASA physical status 3 and 4 patients often receive anaesthesia when possible. Third, aspiration during general anaesthesia most frequently occurs during airway manoeuvres such as tracheal intubation and extubation, use of muscle relaxants and following positive pressure bag/mask ventilation which can cause gas insufflation of the stomach 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37. Such high‐risk events are less relevant to procedural sedation, where they only occur as part of rescue for significant airway or respiratory adverse events. Fourth, most procedures performed under sedation are relatively brief, which results in less time for aspiration risk. Finally, inhalational anaesthetics can be emetogenic, with nausea and vomiting common during post‐anaesthesia recovery. Most procedural sedation is performed without inhalational agents and with a substantially lower frequency of emesis. The commonly used sedative, propofol, is anti‐emetic 38.
Incidence and outcomes of aspiration associated with general anaesthesia and procedural sedation
The evidence relating to general anaesthesia is presented in the online Supplementary Material. The corresponding estimates of procedural sedation aspiration risk are more challenging to obtain than those for anaesthesia, as few studies have similarly large sample sizes (Table 1) 19, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53. None of these studies report occurrences of aspiration‐related mortality.
Table 1.
Literature estimates of aspiration risk during procedural sedationa
| Study | Population | Principal Agent | Endoscopy? | Total Subjects | Aspiration overall | Aspiration during non‐fasted procedures | Aspiration mortality |
|---|---|---|---|---|---|---|---|
| Bhatt 39 | Children | Ketamine | No | 6295 | None | None | None |
| Beach 19 | Children | Propofol | Some | 139,142 | 1:13,914 | 1:12,701 | None |
| Chiaretti 40 | Children | Propofol | Some | 36,516 | None | None | None |
| Friedrich 41 | Adults | Propofol | All | 15,690 | 1:541 | Not stated | None |
| Rajasekaran 42 | Children | Propofol | All | 12,447 | None | None | None |
| Agostoni 43 | Mixed | Propofol | All | 17,999 | 1:1,000 | Not stated | None |
| Dean 44 | Mostly adults | Propofol | None | 62,125 | None | Not stated | None |
| Green 45 | Children | Ketamine | None | 8282 | None | None | None |
| Rex 46 | Adults | Propofol | All | 646,080 | Not stated | Not stated | None |
| Horiuchi 47 | Adults | Propofol | All | 10,662 | None | None | None |
| Vespasiano 48 | Children | Propofol | None | 7304 | 1:7,304 | Not stated | None |
| Onody 49 | Mostly Children | Nitrous oxide | Some | 35,828 | None | None | None |
| Tohda 50 | Adults | Propofol | All | 27,500 | 1:6,875 | Not stated | None |
| Sanborn 51 | Children | Pentobarbital | None | 16,467 | 1:8,234 | None stated | None |
| Walker 52 | Adults | Propofol | All | 9152 | 1:9,152 | Not stated | None |
| Gall 53 | Children | Nitrous oxide | Some | 7511 | None | None | None |
To include just the largest studies, we display those with 5000 or more patients. We also exclude studies which report duplicate subsets of patients.
The best available study is a 139,142‐patient, multicentre registry of paediatric sedation using primarily propofol, with an overall aspiration incidence of 1:13,914 with zero mortality (< 1:139,142) 19. The authors studied ‘high‐performance sedation teams’ whose outcomes might be better than those from other settings; however, contrasting factors that might reasonably promote poorer outcomes were the higher risk nature of the sample (17% were ASA physical status 3 or 4) and that, in ‘many of the cases’, the targeted depth of sedation was actually general anaesthesia rather than moderate or deep sedation.
A 646,080‐patient meta‐analysis of gastroenterologist‐administered propofol sedation for upper endoscopy and colonoscopy has been reported, with about two‐thirds of the data previously unpublished 46. It did not report the frequency of overall aspiration, but stated that none of the four reported deaths were attributable to aspiration.
A recent systematic review of the literature identified 35 papers describing one or more occurrences of procedural sedation‐associated aspiration between 1985 and 2016 20. These reports included 292 occurrences of aspiration during gastro‐intestinal upper endoscopy, with eight deaths. For procedures other than upper endoscopy, there were 34 unique occurrences, with one death in a moribund patient, full recovery in 31 and unknown recovery status in two. A study of this format cannot determine an incidence of aspiration, although it would be assumed that many millions of patients received procedural sedation worldwide during this three‐decade period. It is possible that these literature reports underestimate aspiration frequency due to under‐reporting. However, a compilation of anecdotal ‘sedation disasters’ and subsequent critical incident analysis failed to identify a single instance of sedation‐associated aspiration during a 27‐year study period 54, 55.
Contrast between data for general anaesthesia and procedural sedation
As noted above, reasonable point estimates for the incidence of aspiration associated with general anaesthesia (1:7103 for adults and 1:4800 for children) are higher than the best available procedural sedation point estimate (1:13,914 in children), which may itself be an overestimate given the frequent targeting of a depth similar to general anaesthesia rather than deep sedation 19. The limitations of contrasting such estimates must again be recognised, as they include aggregate patients without factoring in the presence or absence of specific aspiration risk factors (discussed in Question 2). Only 34 occurrences of non‐endoscopic sedation‐associated aspiration have been reported in the medical literature from 1985 to 2016, 20 affirming the rarity of this event. As noted earlier, reasonable point estimates for aspiration mortality associated with general anaesthesia are 1:78,732 for adults and immeasurably small for children. No corresponding estimate for procedural sedation is available; however, there were only nine sedation‐associated aspiration deaths reported in the medical literature from 1985 to 2016, only one of which was for a non‐endoscopic procedure 20. None of these nine deaths were in children or in low‐risk adult patients.
Question 2: What are the known risk factors for pulmonary aspiration with general anaesthesia and with procedural sedation?
The evidence relating to general anaesthesia is presented in the online Supplementary Material. The evidence regarding sedation‐associated aspiration risk factors comes mainly from case series in which aspiration occurrences, when present, were contrasted with patients who did not suffer aspiration 19, 41, 42, 43, 44, 45, 46, 47, 48, 50, 51, 52. The most reliable of these is the 139,142‐subject, multicentre registry of paediatric sedation using primarily propofol referred to earlier 19. Additional information comes from a systematic review of the 326 occurrences of sedation‐associated aspiration reported from 1985 to 2016, in which the authors describe patient characteristics and procedural features that seem to be over‐represented in the aspiration events, which may thus be thought of as possible risk factors 20.
Compared with the general anaesthesia studies (see also Supporting Information, Table S3), most sedation studies have smaller sample sizes and a lower incidence of aspiration. Despite this, the two main contributing studies 19, 20 are of higher methodological quality than many of the anaesthesia studies and systematically assessed multiple clinical variables. We summarise findings from these reports in Table 2 and discuss specific items in the context of both the general anaesthesia and sedation literature below.
Table 2.
Risk factors for pulmonary aspiration associated with procedural sedation
| Risk factor repeatedly reported without conflicting data (Quality of evidence: High): |
| Oesophageal endoscopy in adults 20, 41, 43, 50, 52 |
| Risk factors reported more than once and not specifically refuted elsewhere (Quality of evidence – Moderate) |
| Greater comorbidities in children 19 and adults 20, 50 |
| Propofol as the sedative choice 19, 20 |
| Risk factors reported in a single study and not specifically corroborated or refuted elsewhere (Quality of evidence – Moderate) |
| Infant 12 months of age or less 19 |
| Obstructive sleep apnoea in children 19 |
| Oesophageal endoscopy in children 19 |
| Bronchoscopy in children 19 |
| Clinical features found to not be risk factors, with no conflicting data (Quality of evidence – Moderate) |
| Emergency procedure in children 19, 20 and in adults 20 |
| Absence of fasting in children 19, 20 and in adults 20 |
| Upper respiratory infection in children 94 |
| Pregnancy in teenagers and adults 44 |
Greater patient comorbidities
When a medical illness that could pose a risk to life was reported (i.e. ASA physical status of 3 or greater), there were consistent observations of increased aspiration risk for both general anaesthesia 22, 23, 24, 56 and procedural sedation 19, 20, 50.
Tracheal intubation/extubation/airway manipulation
Numerous general anaesthesia studies have observed occurrences of aspiration temporally associated with tracheal intubation/extubation, insertion of supraglottic airway devices, or other airway manipulation 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 56, 57.
Emergency surgery or procedure
Most studies observed that aspiration was more common during emergency surgery in adults 22, 23, 24, 28, 30, 31, 35, with mixed results in children 25, 26, 36, 56.
In contrast, emergency procedures were not identified as risk factors for procedural sedation (Table 2). This probably reflects the fact that emergency sedation is usually of short duration, performed with an intact airway, and without rapid sequence tracheal intubation or other airway manipulation.
Oesophageal endoscopy/surgery
Multiple studies have identified oesophageal endoscopy/surgery as presenting greater aspiration risk in both general anaesthesia (adults 23, 24, 35, 57 and children 26) and procedural sedation (adults 20, 41, 43, 50, 52 and children 19).
Oesophageal disorders and bowel obstruction
There are repeated reports of aspiration in anaesthetised patients with oesophageal disorders (both structural and motility‐related) in adults 24, 27, 57 and children, 26 and with bowel obstruction in adults 22 and children 36.
Obesity
Contrary evidence regarding obesity was observed in studies of general anaesthesia (for 23, 25, 28, 57 with against 22), with no specific data for procedural sedation.
Co‐administered opioids
Contrary evidence regarding co‐administered opioids was observed in studies of general anaesthesia (for 27, 28 and against 22), with no specific data for procedural sedation.
Age
No consistent age‐based profiles for risk were apparent for either anaesthesia or procedural sedation. Any observed over‐representation of children or older adults may simply reflect the higher baseline prevalence of surgery or procedures in these populations.
Specific sedative drugs
Propofol is the most common sedative associated with aspiration during procedural sedation 19, 20 despite its anti‐emetic effects. It is unclear whether this is a result of the more widespread application of this agent, the use of concomitant opioids or the targeting of deep sedation and the potential for rapid overshoot in sedation depth. Ketamine, unlike other sedatives, helps preserve protective airway reflexes, 21 and there were no reports of aspiration (despite its association with vomiting and, particularly with gastro‐intestinal endoscopy, laryngospasm) in patients receiving this agent alone except in compromised neonates 20, 21.
Sedation duration
The risk of overall complications is known to increase with the duration of anaesthesia 58, 59. However, any such association with aspiration remains to be established. Morbidity and mortality resulting from aspiration occur more frequently when endoscopy includes extended procedures, for example, percutaneous gastrostomy tube placement, submucosal dissection, endoscopic retrograde cholangiopancreatography, active gastro‐intestinal bleeding. 20 There are no corresponding data for other procedural sedation indications, although most such procedures are brief.
Physician specialty
Intensive care specialists as the sedation provider have been identified in a disproportionate number of aspiration occurrences 19, 20, although this is probably confounded by the higher proportion of critically ill patients undergoing sedation, and by their disproportionate contribution of sedation data to the literature. No other appreciable differences are evidence‐based upon the specialty of the sedation provider. 60.
Pharmacologial pre‐treatment
The anaesthetic literature provides no persuasive evidence that therapeutic prophylaxis (e.g. antacids, histamine antagonists, prokinetics, anticholinergics) lowers aspiration risk or improves outcomes 6. There are no corresponding data for procedural sedation.
Fasting
Non‐compliance with fasting guidelines was not identified as a risk factor in either the anaesthesia 22, 26 or procedural sedation literature 19, 20, and this area is discussed in detail in Question 3 below.
Pregnancy
Pregnancy might present greater aspiration risk due to the associated physiological changes, including prolonged gastric emptying and increased gastro‐esophageal reflux. 44 General anaesthesia data are mixed (for 23 and against 22). A study of 62,125 fasted women receiving deep sedation with propofol for elective termination of pregnancy (including 11,039 s trimester) observed no occurrences of aspiration 44.
Patient position
There is inadequate evidence to support or refute the contention that placing the patient on their left side or in a head‐down position might decrease aspiration risk 61.
Absent risk factors
Multiple authors have noted occurrences of aspiration in healthy patients without apparent risk factors, suggesting that aspiration may be either idiosyncratic or due to unknown, unrecognised factors 23, 25, 29, 31, 36, 57. It should also be noted that, whilst risk factors can predict problems, the absence of risk factors neither logically nor clinically implies that any particular hazard cannot occur.
Question 3: What is the evidence that fasting before general anaesthesia or procedural sedation improves outcomes?
The longstanding tradition of fasting before elective surgery and procedural sedation has minimal scientific support and was instead prompted by early reports of aspiration 62 and the logical presumption that regurgitation of gastric contents cannot physically occur if the stomach is empty 7, 12, 13, 63. There are no prospective, controlled trials to guide decision making concerning the impact of fasting intervals on aspiration; therefore, conclusions regarding association or causal relationships rely on observational series and indirect evidence as outlined below. There is no conclusive evidence to support assertions about safe fasting intervals and thus current fasting recommendations from prominent specialty societies 2, 3, 4, 5, 6, 7, 8, 9 (see also Supporting Information, Table S4) are largely consensus driven.
As noted in Question 2, large general anaesthesia studies have not identified an association between aspiration and non‐compliance with typical fasting recommendations in either adults 22 or children 26. The best available corresponding evidence for procedural sedation similarly notes no apparent association between aspiration and non‐compliance with fasting recommendations in adults 20 or children. 19, 20. A limitation of studies contrasting patients with and without fasting compliance is that few in the latter sub‐group are non‐compliant to the point of having a ‘full stomach’; most are non‐compliant due to lesser intake of fluids or solids 19, 64.
Further evidence pertinent to fasting and general anaesthesia is presented in the online Supplementary Material, with evidence relating to procedural sedation below.
Acutely ill or injured patients presenting to Emergency Departments often require procedures that are extremely painful (e.g. abscess incision and drainage, fracture and dislocation reduction) or that are unduly frightening (e.g. facial laceration repair or neuroimaging in a child). General anaesthesia is often impractical, unwarranted and unavailable for these typically brief and simple procedures. Procedural sedation is required to compassionately and expeditiously perform these procedures, even when patients do not comply with existing fasting guidelines intended for elective interventions. Despite this regular ongoing performance of non‐fasted sedation over past decades, Emergency Department patients have not been identified as at undue risk for aspiration 19, 20. Although under‐reporting may occur in any setting, emergency procedures appear to have no higher risk than elective ones in either children 19, 20 or adults 20. Indeed, there have been only two cases of aspiration reported in the emergency department setting; both patients had been fasted (2 hours liquids, 6 hours solids) before sedation, and both made a full recovery 20. Multiple Emergency Department observational series have not identified any association between non‐compliance with elective fasting guidelines and complications or adverse outcomes 11, 64, 65, 66, 67, 68, 69, 70, 71.
Although it is suggested, despite contrary evidence 72, 73, 74, that gastric emptying is delayed by acute stress or anxiety, the rarity of Emergency Department aspiration suggests that, even if this is true, it is not clinically important. Similarly, fasting time before adult colonoscopy is being widely reduced due to the popularity of superior split‐ and large‐volume bowel preparations in which the last dose is typically completed 3 hours before the procedure. Such shorter fasting does not increase gastric volume or acidity 75, 76, 77, 78, and does not appear to increase aspiration risk during the associated propofol deep sedation or anaesthesia 75, 76, 77, 78, 79.
Procedural sedation is regularly performed in other settings in which fasting is frequently incomplete: cardiac catheterisation 80; therapeutic abortions 81; eye surgery 82, 83, 84, 85; and abdominal imaging in children who have first received oral contrast 86, 87, 88. None of these settings have been identified as showing an increased aspiration risk.
Question 4: Does compliance with pre‐anaesthesia and pre‐sedation fasting guidelines negatively impact patient comfort, patient health, the anaesthesia or sedation experience or workflow?
The evidence relating to general anaesthesia is presented in the online Supplementary Material. There is substantially less evidence available specific to procedural sedation; however, fasting has been associated with decreased sedation efficacy 89 and an increased incidence of sedation failure 90, 91. Hypoglycaemia has been reported after pre‐procedural fasting in an adult diabetic patient 92.
Question 5: What is the impact of published guidelines and clinical strategies for pre‐operative or pre‐procedural care (including fasting) on the prevention of pulmonary aspiration?
The incidence of aspiration associated with general anaesthesia has been declining over recent decades (see also Supporting Information, Table S2); however, it is not clear whether this is due to pre‐operative fasting or simply improved airway management and other anaesthetic techniques 24, 25, 31. Given this rarity of aspiration, in 1990, Cote argued that the amount of resources directed at preventing it seemed unjustified, asking: “Is aspiration pneumonia in routine healthy patients a nonissue?” 93. As noted in question 3, there is no confirmation that specific strategies (including pre‐procedural fasting) have a clinically important impact in preventing pulmonary aspiration. Although it is possible that pre‐procedural restrictions on solid food (rather than liquids) may be protective, current evidence suggests that there may be trivial or no impact from either food or liquid restriction, with the greater contributing factor being the prior identification of patients with risk factors (Table 2 and see also Supporting Information, Table S3) and increased precautions with their airway management. We suggest that the current overriding focus on fasting may be largely misguided.
Question 6: Are there barriers to the development of fasting recommendations for procedural sedation that differ from existing guidelines designed for general anaesthesia?
The evidence relating to general anaesthesia is presented in the online Supplementary Material. Similar barriers exist to procedural sedation practitioners who desire, based on evidence previously discussed, to deviate from fasting guidelines stipulated for anaesthesia. Despite the differences between sedation and anaesthesia and the compelling evidence and basis for differential aspiration risk, in the past it has been near‐universal to specify identical fasting precautions for both 1, 4, 6, 7, 16, 17. Given these many decades of precedent and an unwillingness for institutions to appear to be ‘breaking the rules’, individual clinicians are likely to be challenged and could face censure if applying the evidence contrary to existing guidelines.
The algorithm we designed to support our recommendations (Fig. 1) summarises the approach we advocate. In this flow chart, each patient is risk stratified during their pre‐sedation assessment using evidence‐based factors relating to patient characteristics, comorbidities, the nature of the procedure and the nature of the anticipated sedation technique. For elective procedures, graded fasting precautions for liquids and solids are then recommended based upon this assessment of negligible, mild or moderate aspiration risk. We did not include a high‐risk category, because even with the most notable risk factors, the evidence suggests that aspiration remains uncommon.
Discussion
We present the first recommendations for fasting and aspiration prevention specific to procedural sedation, based upon rigorous literature review and consensus generation. These were designed to apply to patients of all ages and settings and are not intended for general anaesthesia.
Our recommendations are not a substitute for physician judgement or clinical assessment, and we expect that there will be situations in which clinicians will appropriately deviate from them due to unique clinical circumstances. This statement is not intended to assert a legal standard of practice or absolute requirement and cannot be expected to guarantee any specific outcome. No single document can rigidly categorise appropriate practice in this setting and, therefore, we offer this as a clinical guide combined with practical suggestions.
We recognised in advance when planning this project that our literature search would be unlikely to identify randomised, controlled trials of preventative interventions, given the rarity of aspiration in both procedural sedation and general anaesthesia, and the prohibitive sample sizes thus required for any such effort. Accordingly, as has been necessary for earlier fasting guidelines for general anaesthesia (see also Supporting Information, Table S4), we were required to rely upon evidence less rigorous than would ordinarily be preferred. Large observational studies and indirect evidence make up the literature supporting this statement, with such evidence then framed using an international, multidisciplinary panel and a rigorous Delphi consensus process. We were unable to use guideline methodologies designed to evaluate and grade randomised, controlled trials and, given the diversity of articles and content areas required to frame this multiple questions addressing this topic, it was not practical or appropriate to attempt to grade the methodological quality of each study. Accordingly, we selected the GRADE approach, which permitted us to express our confidence in the evidence supporting specific statements. We are unaware of another methodological technique likely to be more valid for this topic area. We believe that the process was fair and transparent and demonstrated a measurable degree of final consensus.
Supporting information
Data S1. Context summary for general anaesthesia.
Acknowledgements
We thank S. Tamares, MLIS for her expert production of the literature search, and the multiple liaisons from outside organisations who kindly provided their expert input.
This manuscript had no outside funding or support. MI has received travel support from Fresenius Kabi and is an editor of Anaesthesia. FB has research grants from the National Health and Medical Research Council, Canberra, Australia and the Royal Children's Hospital Foundation, Melbourne, Australia. LC has research grants from Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) e Fundação de Amparo à Pesquisa do Estado de Goiás (FAPEG). AA has sponsored research and consultancy fees from The Medicines Company, Orion, and Johnson and Johnson, and unrestricted research grants from Carefusion and Drager. PC is supported by the Brazilian National Research Scientific Research Council. KM receives support from Hospira for investigator‐initiated studies and unrestricted educational support for conferences. Upon project completion one committee member elected to not be included in the authorship list. He expressed that the development process was fair, that his views were heard and that he supported the quality of the literature summaries. His decision was based on his caution in making specific recommendations based upon the reported degree of incomplete evidence.
References
- 1. American Academy of Pediatrics Committee on Drugs . Guidelines for the elective use of conscious sedation, deep sedation, and general anesthesia in pediatric patients. Pediatrics 1985; 76: 317–21. [PubMed] [Google Scholar]
- 2. Safe Sedation Practice for Healthcare Procedures . Academy of Medical Royal Colleges. 2013. https://www.rcoa.ac.uk/system/files/PUB-SafeSedPrac2013.pdf (accessed 11/08/2019).
- 3. Royal College of Anaesthetists . Safe Sedation of Adults in the Emergency Department. 2012. http://www.rcoa.ac.uk/document-store/safe-sedation-of-adults-the-emergency-department (accessed 11/08/2019).
- 4. Smith I, Kranke P, Murat I, et al. Perioperative fasting in adults and children: guidelines from the European Society of Anaesthesiology. European Journal of Anaesthesiology 2011; 28: 556–69. [DOI] [PubMed] [Google Scholar]
- 5. Thomas M, Morrison C, Newton R, Schindler E. Consensus statement on clear fluids fasting for elective pediatric general anesthesia. Pediatric Anesthesia 2018; 28: 411–14. [DOI] [PubMed] [Google Scholar]
- 6. American Society of Anesthesiologists . Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures. Anesthesiology 2017; 126: 376–93. [DOI] [PubMed] [Google Scholar]
- 7. Cote CJ, Wilson S. Guidelines for monitoring and management of pediatric patients before, during, and after sedation for diagnostic and therapeutic procedures: update 2016. American academy of pediatrics. Pediatrics 2016; 138: e20161212–2. [DOI] [PubMed] [Google Scholar]
- 8. American College of Emergency Physicians . Clinical Policy: procedural Sedation and Analgesia in the Emergency Department. Annals of Emergency Medicine 2014; 63: 247–58. [DOI] [PubMed] [Google Scholar]
- 9. American Academy of Pediatric Dentistry . Guidelines for monitoring and management of pediatric patients before, during, and after sedation for diagnostic and therapeutic procedures: update 2016. Pediatric Dentistry 2016; 38: 13–39. [PubMed] [Google Scholar]
- 10. American Academy of Pediatrics . Guidelines for monitoring and management of pediatric patients during and after sedation for diagnostic and therapeutic procedures: an update. Pediatrics 2006; 118: 2587–602. [DOI] [PubMed] [Google Scholar]
- 11. Green SM, Krauss B, Mason KP. Reevaluating fasting for procedural sedation [Editorial]. Journal of the American Medical Association Pediatrics 2018; 172: 622–3. [DOI] [PubMed] [Google Scholar]
- 12. Green SM, Krauss B. Pulmonary aspiration risk during ED procedural sedation – An examination of the role of fasting and sedation depth. Academic Emergency Medicine 2002; 9 : 35–42. [DOI] [PubMed] [Google Scholar]
- 13. Green SM, Roback MG, Miner JR, Burton JH, Krauss B. Fasting and emergency department procedural sedation and analgesia: a consensus‐based clinical practice advisory. Annals of Emergency Medicine 2007; 49: 454–61. [DOI] [PubMed] [Google Scholar]
- 14. Graham R, Mancher M, Miller Wolman D, Greenfield S, Steinberg E. Clinical practice guidelines we can trust – Institute of Medicine (US) committee on standards for developing trustworthy clinical practice guidelines. Washington, DC: National Academies Press (US) 2011; ISBN‐13: 978‐0‐309‐16423‐8. [PubMed] [Google Scholar]
- 15. Bhatt M, Kennedy R, Osmond M, et al. Consensus‐based recommendations for standardizing terminology and reporting adverse events for emergency department procedural sedation and analgesia in children. Annals of Emergency Medicine 2009; 53: 426–35. [DOI] [PubMed] [Google Scholar]
- 16. Krauss B, Green SM. Sedation and analgesia for procedures in children. New England Journal of Medicine 2000; 342: 938–45. [DOI] [PubMed] [Google Scholar]
- 17. Krauss B, Green SM. Procedural sedation and analgesia in children. Lancet 2006; 367: 766–80. [DOI] [PubMed] [Google Scholar]
- 18. Marik PE. Aspiration pneumonitis and aspiration pneumonia. New England Journal of Medicine 2001; 344: 665–71. [DOI] [PubMed] [Google Scholar]
- 19. Beach ML, Cohen DM, Gallagher SM, Cravero JP. Major adverse events and relationship to nil per os status in pediatric sedation/anesthesia outside the operating room: a report of the pediatric sedation research consortium. Anesthesiology 2016; 124: 80–8. [DOI] [PubMed] [Google Scholar]
- 20. Green SM, Mason KP, Krauss BS. Pulmonary aspiration during procedural sedation: a comprehensive systematic review. British Journal of Anaesthesia 2017; 118: 344–54. [DOI] [PubMed] [Google Scholar]
- 21. Green SM, Roback MG, Kennedy RM, Krauss BS. Clinical practice guideline for emergency department ketamine dissociative sedation: 2011 update. Annals of Emergency Medicine 2011; 57: 449–61. [DOI] [PubMed] [Google Scholar]
- 22. Warner MA, Warner ME, Weber JG. Clinical significance of pulmonary aspiration during the perioperative period. Anesthesiology 1993; 78: 56–62. [DOI] [PubMed] [Google Scholar]
- 23. Olsson GL, Hallen B, Hambraeus‐Jonzon K. Aspiration during anaesthesia—a computer‐aided study in 185, 358 anaesthetics. Acta Anaesthesiologica Scandinavica 1986; 30: 84–92. [DOI] [PubMed] [Google Scholar]
- 24. Sakai T, Planinsic RM, Quinlan JJ, Handley LJ, Kim T‐Y, Hilmi IA. The incidence and outcome of perioperative pulmonary aspiration in a university hospital: a 4‐year retrospective analysis. Anestheisa and Analgesia 2006; 103: 941–7. [DOI] [PubMed] [Google Scholar]
- 25. Walker RWM. Pulmonary aspiration in pediatric anesthetic practice in the UK: a prospective survey of specialist pediatric centers over a one‐year period. Pediatric Anesthesia 2013; 23: 702–11. [DOI] [PubMed] [Google Scholar]
- 26. Borland LM, Sereika SM, Woelfel SK, et al. Pulmonary aspiration in pediatric patients during general anesthesia; incidence and outcome. Journal of Clinical Anesthesia 1998; 10: 95–102. [DOI] [PubMed] [Google Scholar]
- 27. Søreide E, Bjornestad E, Steen PA. An audit of perioperative aspiration pneumonitis in gynaecological and obstetric patients. Acta Anaesthesiologica Scandinavica 1996; 40: 14–19. [DOI] [PubMed] [Google Scholar]
- 28. Kluger MT, Short TG. Aspiration during anaesthesia: a review of 133 cases from the Australian Anaesthetic Incident Monitoring Study (AIMS). Anaesthesia 1999; 54: 19–26. [DOI] [PubMed] [Google Scholar]
- 29. Cook TM, Woodall N, Frerk C. Major complications of airway management in the UK: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 1: anaesthesia. British Journal of Anaesthesia 2011; 106: 617–31. [DOI] [PubMed] [Google Scholar]
- 30. Cook TM, Scott S, Mihai R. Litigation related to airway and respiratory complications of anaesthesia: an analysis of claims against the NHS in England 1995–2007. Anaesthesia 2010; 65: 556–63. [DOI] [PubMed] [Google Scholar]
- 31. Tan Z, Lee SY. Pulmonary aspiration under GA: a 13‐year audit in a tertiary pediatric unit. Pediatric Anesthesia 2016; 26: 547–52. [DOI] [PubMed] [Google Scholar]
- 32. Jimenez N, Posner KL, Cheney FW, Caplan RA, Lee LA, Domino KB. An Update on pediatric anesthesia liability: a closed claims analysis. Anesthesia and Analgesia 2007; 104: 147–53. [DOI] [PubMed] [Google Scholar]
- 33. Kallar SK. Aspiration pneumonitis: fact or fiction? Problems in Anesthesia 1988; 2: 29–36. [Google Scholar]
- 34. Leigh JM, Tytler JA. Admissions to the intensive care unit after complications of anaesthetic techniques over 10 years. Anaesthesia 1990; 45: 814–20. [DOI] [PubMed] [Google Scholar]
- 35. Mellin‐Olsen J, Fasting S, Gisvold SE. Routine preoperative gastric emptying is seldom indicated. A study of 85,594 anaesthetics with special focus on aspiration pneumonia. Acta Anaesthesiologica Scandinavica 1996; 40: 1184–8. [DOI] [PubMed] [Google Scholar]
- 36. Warner MA, Warner ME, Warner DO, Warner LO, Warner EJ. Perioperative pulmonary aspiration in infants and children. Anesthesiology 1999; 90: 66–71. [DOI] [PubMed] [Google Scholar]
- 37. Habre W, Disma N, Virag K, et al. Incidence of severe critical events in paediatric anaesthesia (APRICOT): a prospective multicentre observational study in 261 hospitals in Europe. Lancet Respiratory Medicine 2017; 5: 412–25. [DOI] [PubMed] [Google Scholar]
- 38. Sahinovic MM, Struys MMRF, Absalom AR. Clinical pharmacokinetics and pharmacodynamics of propofol. Clinical Pharmacokinetics 2018; 57: 1539–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Bhatt M, Johnson DW, Chan J, et al. Sedation Safety Study Group of Pediatric Emergency Research Canada (PERC). Risk factors for adverse events in emergency department procedural sedation for children. Journal of the American Medical Association Pediatric 2017; 171: 957–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Chiaretti A, Benini F, Pierri F, et al. Safety and efficacy of propofol administered by paediatricians during procedural sedation in children. Acta Paediatrica 2013; 103: 182–7. [DOI] [PubMed] [Google Scholar]
- 41. Friedrich K, Scholl SG, Beck S, et al. Respiratory complications in outpatient endoscopy with endoscopist‐directed sedation. Journal of Gastrointestinal Liver Diseases 2014; 23: 255–9. [DOI] [PubMed] [Google Scholar]
- 42. Rajasekaran S, Hackbarth RM, Davis AT, et al. The safety of propofol sedation for elective nonintubated esophagogastroduodenoscopy in pediatric patients. Pediatric Critical Care Medicine 2014; 15: e261–9. [DOI] [PubMed] [Google Scholar]
- 43. Agostoni M, Fanti L, Gemma M, Pasculli N, Beretta L, Testoni PA. Adverse events during monitored anaesthesia care for GI endoscopy: an 8‐year experience. Gastrointestinal Endoscopy 2011; 74: 266–75. [DOI] [PubMed] [Google Scholar]
- 44. Dean G, Jacobs AR, Goldstein RC, Gevirtz CM, Paul ME. The safety of deep sedation without intubation for abortion in the outpatient setting. Journal of Clinical Anesthesia 2011; 23: 437–42. [DOI] [PubMed] [Google Scholar]
- 45. Green SM, Roback MG, Krauss B, et al. Predictors of airway and respiratory adverse events with ketamine sedation in the emergency department: an individual‐patient data meta‐analysis of 8,282 children. Annals of Emergency Medicine 2009; 54: 158–168.e4. [DOI] [PubMed] [Google Scholar]
- 46. Rex DK, Deenadayalu VP, Eid E, et al. Endoscopist‐directed administration of propofol: a worldwide safety experience. Gastroenterology 2009; 137: 1229–37. [DOI] [PubMed] [Google Scholar]
- 47. Horiuchi A, Nakayama Y, Hidaka N, Ichise Y, Kajiyama M, Tanaka N. Low‐dose propofol sedation for diagnostic esophagogastroduodenoscopy: results in 10,662 adults. American Journal of Gastroenterology 2009; 104: 1650–5. [DOI] [PubMed] [Google Scholar]
- 48. Vespasiano M, Finkelstein M, Kurachek S. Propofol sedation: intensivists’ experience with 7304 cases in a children's hospital. Pediatrics 2007; 120: e1411–7. [DOI] [PubMed] [Google Scholar]
- 49. Onody P, Gil P, Hennequin M. Safety of inhalation of a 50% nitrous oxide/oxygen premix: a prospective survey of 35 828 administrations. Drug Safety 2006; 29: 633–40. [DOI] [PubMed] [Google Scholar]
- 50. Tohda G, Higashi S, Wakahara S, Morikawa M, Sakumoto H, Kane T. Propofol sedation during endoscopic procedures: safe and effective administration by registered nurses supervised by endoscopists. Endoscopy 2006; 38: 360–7. [DOI] [PubMed] [Google Scholar]
- 51. Sanborn PA, Michna E, Zurakowski D, et al. Adverse cardiovascular and respiratory events during sedation of pediatric patients for imaging examinations. Radiology 2005; 237: 288–94. [DOI] [PubMed] [Google Scholar]
- 52. Walker J. Nurse‐administered propofol sedation without anesthesia specialists in 9152 endoscopic cases in an ambulatory surgery center. American Journal of Gastroenterology 2003; 98: 1744–50. [DOI] [PubMed] [Google Scholar]
- 53. Gall O, Annequin D, Benoit G, Glabeke E, Vrancea F, Murat I. Adverse events of premixed nitrous oxide and oxygen for procedural sedation in children. Lancet 2001; 358: 1514–15. [DOI] [PubMed] [Google Scholar]
- 54. Cote CJ, Alderfer RJ, Notterman DA, et al. Sedation disasters: adverse drug reports in pediatrics—FDA, USP, and others [abstract]. Anesthesiology 1995; 83: A1183. [Google Scholar]
- 55. Coté CJ, Notterman DA, Karl HW, Weinberg JA, McCloskey C. Adverse sedation events in pediatrics: a critical incident analysis of contributing factors. Pediatrics 2000; 105: 805–14. [DOI] [PubMed] [Google Scholar]
- 56. Eisler L, Huang G, Lee K‐EM, et al. Identification of perioperative pulmonary aspiration in children using quality assurance and hospital administrative billing data. Pediatric Anesthesia 2018; 17: 19–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Neelakanta G, Chikyarappa A. A review of patients with pulmonary aspiration of gastric contents during anesthesia reported to the Departmental Quality Assurance Committee. Journal of Clinical Anesthesia 2006; 18: 102–7. [DOI] [PubMed] [Google Scholar]
- 58. Asai T. Who is at increased risk of pulmonary aspiration? British Journal of Anaesthesia 2004; 93: 497–500. [DOI] [PubMed] [Google Scholar]
- 59. Tiret L, Desmonts JM, Hatton F, Vourc'h G. Complications associated with anaesthesia—a prospective survey in France. Canadian Anaesthetists Society Journal 1986; 33: 336–44. [DOI] [PubMed] [Google Scholar]
- 60. Couloures KG, Beach M, Cravero JP, Monroe KK, Hertzog JH. Impact of provider specialty on pediatric procedural sedation complication rates. Pediatrics 2011; 127: e1154–60. [DOI] [PubMed] [Google Scholar]
- 61. Takenaka I, Aoyama K, Iwagaki T. Combining head–neck position and head‐down tilt to prevent pulmonary aspiration of gastric contents during induction of anaesthesia. European Journal of Anaesthesiology 2012; 29: 380–5. [DOI] [PubMed] [Google Scholar]
- 62. Mendelson CL. The aspiration of stomach contents into the lungs during obstetric anesthesia. American Journal of Obstetrics and Gynecology 1946; 52: 191–204. [DOI] [PubMed] [Google Scholar]
- 63. Ljungqvist O. Soreide E: Preoperative fasting. British Journal of Surgery 2003; 90: 400–6. [DOI] [PubMed] [Google Scholar]
- 64. Roback MG, Bajaj L, Wathen JE, Bothner J. Preprocedural fasting and adverse events in procedural sedation anad analgesia in a pediatric emergency department: are they related? Annals Emergency Medicine 2004; 44: 454–9. [DOI] [PubMed] [Google Scholar]
- 65. Bhatt M, Johnson DW, Taljaard M, et al. Association of preprocedural fasting with outcomes of emergency department sedation in children. Journal of the American Medical Association Pediatrics 2018; 172: 678–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Agrawal D, Manzi SF, Gupta R, Krauss B. Preprocedural fasting state and adverse events in children undergoing procedural sedation and analgesia in a pediatric emergency department. Annals of Emergency Medicine 2003; 42: 636–46. [DOI] [PubMed] [Google Scholar]
- 67. Treston G. Prolonged pre‐procedure fasting time is unnecessary when using titrated intravenous ketamine for paediatric procedural sedation. Annals of Emergency Medicine 2004; 16: 145–50. [DOI] [PubMed] [Google Scholar]
- 68. Babl FE, Puspitadewi A, Barnett P, et al. Preprocedural fasting state and adverse events in children receiving nitrous oxide for procedural sedation and analgesia. Pediatric Emergency Care 2005; 21: 736–43. [DOI] [PubMed] [Google Scholar]
- 69. McKee MR, Sharieff GQ, Kanegaye JT, et al. Oral analgesia before pediatric ketamine sedation is not associated with an increased risk of emesis and other adverse events. Journal of Emergency Medicine 2008; 35: 23–8. [DOI] [PubMed] [Google Scholar]
- 70. Bell A, Treston G, McNabb C, et al. Profiling adverse respiratory events and vomiting when using propofol for emergency department procedural sedation. Emergency Medicine Australasia 2007; 19: 405–10. [DOI] [PubMed] [Google Scholar]
- 71. Chumpitazi CE, Camp EA, Bhamidipati DR, et al. Shortened preprocedural fasting in the pediatric emergency department. American Journal of Emergency Medicine 2018; 36: 1577–80. [DOI] [PubMed] [Google Scholar]
- 72. Lydon A, McGinley J, Cooke T, Duggan PF, Shorten GD. Effect of anxiety on the rate of gastric emptying of liquids. British Journal of Anaesthesia 1998; 81: 522–5. [DOI] [PubMed] [Google Scholar]
- 73. Kallar SK, Everett LL. Potential risks and preventive measures for pulmonary aspiration – New concepts in preoperative fasting guidelines. Anaesthesia and Analgesia 1993; 77: 171–82. [DOI] [PubMed] [Google Scholar]
- 74. Simini B. Preoperative fasting [letter]. Lancet 1999; 353: 862. [DOI] [PubMed] [Google Scholar]
- 75. Shaukat A, Malhotra A, Greer N, MacDonald R, Wels J, Wilt TJ. Systematic Review: outcomes by Duration of NPO Status prior to Colonoscopy. Gastroenterology Research and Practice 2017; 2017: 3914942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Tandon K, Khalil C, Castro F, et al. Safety of large‐volume, same‐day oral bowel preparations during deep sedation: a prospective observational study. Anesthesia and Analgesia 2017; 125: 469–76. [DOI] [PubMed] [Google Scholar]
- 77. Alghamry A, Ponnuswamy SK, Agarwal A, et al. Split‐dose bowel preparation with polyethylene glycol for colonoscopy performed under propofol sedation. Is there an optimal timing? Journal of Digestive Diseases 2017; 18: 160–8. [DOI] [PubMed] [Google Scholar]
- 78. Huffman M, Unger RZ, Thatikonda C, Amstutz S, Rex DK. Split‐dose bowel preparation for colonoscopy and residual gastric fluid volume: an observational study. Gastrointestinal Endoscopy 2010; 72: 516–22. [DOI] [PubMed] [Google Scholar]
- 79. Prieto‐Frías C, Muñoz‐Navas M, Betés MT, et al. Split‐dose sodium picosulfate‐magnesium citrate colonoscopy preparation achieves lower residual gastric volume with higher cleansing effectiveness than a previous‐day regimen. Gastrointestinal Endoscopy 2016; 83: 566–73. [DOI] [PubMed] [Google Scholar]
- 80. Hamid T, Aleem Q, Lau Y, et al. Pre‐procedural fasting for coronary interventions: is it time to change practice? Heart 2014; 100: 658–61. [DOI] [PubMed] [Google Scholar]
- 81. Wiebe ER, Byczko B, Kaczorowski J, McLane AL. Can we safely avoid fasting before abortions with low‐dose procedural sedation? A retrospective cohort chart review of anesthesia‐related complications in 47,748 abortions. Contraception 2013; 87: 51–4. [DOI] [PubMed] [Google Scholar]
- 82. Popovic M, Schlenker MB, Goldshtein D, Rai A, El‐Defrawy S. Preoperative fasting for ambulatory cataract surgery: asystematic review. Canadian Journal of Ophthalmology 2019; 54: 145–9. [DOI] [PubMed] [Google Scholar]
- 83. Sanmugasunderam S, Khalfan A. Is fasting required before cataract surgery? A retrospective review. Canadian Journal of Ophthalmology 2009; 44: 655–6. [DOI] [PubMed] [Google Scholar]
- 84. Maltby JR, Hamilton RC. Preoperative fasting guidelines for cataract surgery under regional anaesthesia. British Journal of Anaesthesia 1993; 71: 167. [DOI] [PubMed] [Google Scholar]
- 85. Dowling JL. Nulla per os [NPO] after midnight reassessed. Rhode Island Medical Journal 1995; 78: 339–41. [PubMed] [Google Scholar]
- 86. Teshome G, Braun JL, Lichenstein R. Ketamine sedation after administration of oral contrast: a retrospective cohort study. Hospital Pediatrics 2015; 5: 495–500. [DOI] [PubMed] [Google Scholar]
- 87. Kharazmi SA, Kamat PP, Simoneaux SF, Simon HK. Violating traditional NPO guidelines with PO contrast before sedation for computed tomography. Pediatric Emergency Care 2013; 29: 979–81. [DOI] [PubMed] [Google Scholar]
- 88. Mahmoud M, McAuliffe J, Kim H‐Y, et al. Oral contrast for abdominal computed tomography in children: the effects on gastric fluid volume. Anaesthesia and Analgesia 2010; 111: 1252–8. [DOI] [PubMed] [Google Scholar]
- 89. Ghaffar S, Haverland C, Ramaciotti C, Scott WA, Lemler MS. Sedation for pediatric echocardiography: evaluation of preprocedure fasting guidelines. Journal of the American Society of Echocardiography 2002; 15: 980–3. [DOI] [PubMed] [Google Scholar]
- 90. Hoffman GM, Nowakowski R, Troshynski TJ, Berens RJ, Weisman SG. Risk reduction in pediatric procedural sedation by application of an AAP/ASA process mode. Pediatrics 2002; 109: 236–43. [DOI] [PubMed] [Google Scholar]
- 91. Keidan I, Gozal D, Minuskin T, Weinberg M, Barkaly H, Augarten A. The effect of fasting practice on sedation with chloral hydrate. Pediatric Emergency Care 2004; 20: 805–7. [DOI] [PubMed] [Google Scholar]
- 92. Wickerham AL, Schultz EJ, Lewine EB. Nil per os orders for imaging: a teachable moment. JAMA Internal Medicine 2017; 177: 1670–1. [DOI] [PubMed] [Google Scholar]
- 93. Cote CJ. NPO after midnight for children—a reappraisal. Anesthesiology 1990; 72: 589–92. [DOI] [PubMed] [Google Scholar]
- 94. Mallory MD, Travers C, McCracken CE, Hertzog J, Cravero JP. Upper respiratory infections and airway adverse events in pediatric procedural sedation. Pediatrics 2017; 140: e20170009–12. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Context summary for general anaesthesia.


