Abstract
Background
In sinus augmentation, when remaining bone height is ≤5 mm, a lateral window approach is often the preferred choice; nonetheless, patients prefer to have a less invasive approach such as crestal sinus augmentation (CSA). Prior case reports have described the use of various staged approaches of a CSA technique in cases of limited bone height. The aim of this report was to describe the results of a case series in which a two‐stage CSA technique was used in patients with 4 to 6 mm of bone height.
Methods
Nineteen subjects with 28 sinuses of initial vertical bone height of 4 to 6 mm were included in which a two‐stage CSA technique was used in place of a lateral window approach. In the first surgery, 0.3 mL graft material was inserted into all sites. In the second surgery, 13 sites were filled with 0.2 mL graft material and remaining 15 sites were filled with 0.4 mL.
Results
No damage was observed in the maxillary sinus floor membrane after first 0.2 mL filling; however, one case had Schneiderian membrane perforation after filling 0.4 mL. The average elevation height (EH) after first surgery was 5.81 ± 0.7 mm, 5.15 ± 0.91 mm before second surgery, 6.69 ± 0.89 mm with 0.2 mL filling (total 0.5 mL) and 8.11 ± 1.24 mm with 0.4 mL filling (total 0.7 mL). The thickness of maxillary sinus membrane before first surgery was 2.6 ± 2.59 mm; however, it has become 0.97 ± 1.59 mm before second surgery, with a decrease of 1.6 mm estimate.
Conclusion
This case series that assessed outcomes of staged crestal maxillary sinus augmentation was an effective approach to elevating 6 or 8 mm alveolar bone height without causing major membrane perforation. However, the two‐stage approach was used in the limited residual bone height (4 to 6 mm) and required two separate surgical procedures.
Keywords: crestal sinus augmentation, crestal sinus lift, internal sinus lift, Schneiderian membrane
1. INTRODUCTION
The osteotome‐mediated transcrestal sinus augmentation was first proposed by Tatum in 1986.1 The technique was then modified in 1994 by Summers2 using a set of tapered osteotomes with increasing diameters intended to increase the density of the soft bone and create an up‐fracture of the maxillary sinus floor. It is generally agreed that if the remaining crestal bone height ≤5 mm to the maxillary sinus floor, a staged approach using lateral window technique3 is often recommended. However, maxillary sinus has an anatomical limit such as arteries and septa around the lateral window site and an adhesion of maxillary floor membrane that makes lateral window sinus augmentation more challenging.
With the introduction of cone beam computed tomography (CBCT), clinician now is able to review the anatomical structures before surgery. According to the ABC sinus classification,3 if the residual bone is <5 mm, generally lateral window approach is recommended and when the remaining bone height is 6 to 9 mm then a crestal sinus augmentation (CSA) approach with simultaneous implant placement is preferred. Further, research has reported that the Schneiderian membrane could be elevated 6 mm by filling 0.3 mL bone graft material via CSA.4 Vertical elevation by filling 0.1 to 0.3 mL graft material is relatively easy, but graft material >0.3 mL spread on the sinus floor horizontally and not elevate the membrane vertically. Too much graft material may result in potential membrane perforation that often led to a lower success rate. This is especially true in residual remaining bone height of ≤5 mm.5 In Japan, staged crestal sinus augmentation has been advocated by many private implantologists to avoid aggressive lateral window approaches, and some case reports have been described but with great variability in the clinical cases.6, 7, 8, 9 Nonetheless, there is limited data regarding how this approach can lift sinus floor in the different stages and how effective they are. Hence, the aim of reporting this series of cases was to describe the effect of a two‐stage approach of CSA technique in the cases of limited bone height (4 to 6 mm).
2. MATERIALS AND METHODS
2.1. Study design and population
This is a report of a series of cases in which subjects who needed sinus augmentation, with remaining bone height of 4 to 6 mm, for implant‐supported prostheses were treated and agreed to take part in reporting the results of their treatment. The case series was conducted in accordance with the Helsinki Declaration of 1975, as revised in 2000. Before initiating the patient's therapy, the treatment plan and procedure, potential risks, and need for obtaining several CBCTs were explained and written informed consent forms obtained. Patients were informed that this staged crest sinus augmentation procedure was a common approach advocated by many private dentists to avoid the much wider and traumatic lateral window approach. This procedure is also a routine procedure performed in our clinic with high success rate. The patient inclusion criteria were: patients between 18 and 80 years old, nonsmokers, without presence of systemic infectious diseases at the time of implant insertion and any serious medical diseases or conditions known to alter bone formation. In addition, patients who presented ongoing periodontitis, sinus pathology, skeletal disorder or taking medications that would influence bone metabolism were excluded.
2.2. Study protocol
Before patient treatment, the treatment plan with detailed procedure as well as the potential risks was given and the treatment consent forms were obtained. Radiation exposure as a risk of the study and other risks including sinus penetration were clearly explained. Parameters, including patient age, sex, medical and dental history, distance from the alveolar ridge to the sinus floor, amount of sinus lift needed, type of bone grafting materials used, type and size of implants used, type of prosthetics used, and time of follow‐up were recorded, as a standard part of our clinical protocol for managing complex cases. Diagnostic records (panoramic x‐ray, diagnostic casts, and surgical guides) were taken on all patients before surgery. Surgical procedures were performed under local anesthesia.
2.3. Surgical procedure
Treatment was carried out, by the same operator (TS), under local anesthesia with local infiltration buccally and palatally. A crestal incision was made in the surgical area, and additional releasing incisions distal to the defect area were made if needed. A full thickness periosteal flap was elevated. The proposed implant site was first marked with a 1.5 mm round bur, followed by a series of preparation twisted drill with increasing diameters from 1.6 to 3.2 mm, finished by the 3.7 mm to a depth of about 1 mm from the maxillary sinus floor as measured from the preoperative radiograph (Figure 3A). A piezoelectric device with a curved cutting tip1 was used for the osteotomy of the 1 mm remaining bone. The sinus membrane was subsequently elevated with a 3.2 mm osteotome.2 The Valsalva maneuver test was used to confirm whether the sinus membrane was intact after the osteotome procedure.
Figure 3.
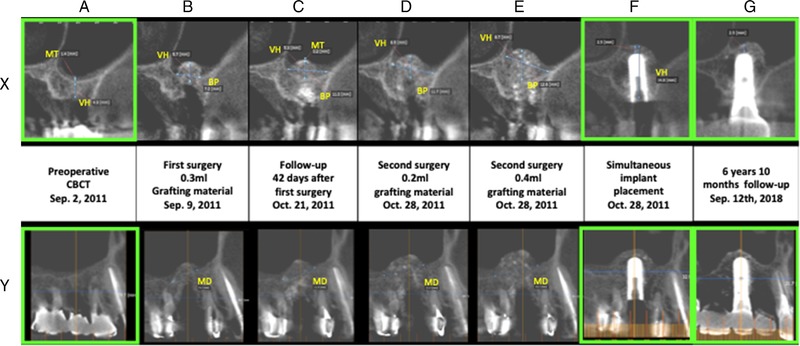
A representative clinical case. (A) Preoperative CBCT shows a crestal bone height of <5 mm. CSA was indicated. (B) The first surgery was performed after osteotome, 0.3 mL grafting material (a mixture of HA and osteogen) inserted into the sinus without elevating the sinus membrane. (C) Follow‐up CBCT of 42 days after the first surgery shows new bone regeneration at the grafted area. (D) Second surgery was performed 1 week later. At first 0.2 mL new grafting material (DFDBA) was inserted after osteotome procedure, then 0.4 mL grafting material was added before implant placement (E). (F) 4.7 × 12 mm implant was placed at the same second surgery after second bone grafting at the sinus. (G) six‐years follow‐up shows a minimum bone resorption after implant placement after CSA. X shows images in sagittal plane, while Y shows images in coronal plane. Magnification of images in green is available in the next figure
After sinus‐floor in fracture, a mixture at 1:1 ratio of bone substitute materials of hydroxyapatite (HA)3 and demineralized freeze‐dried bone allografts (DFDBA)4 was added to the osteotomy site. The rationales for using this graft combination is because of the slow resorbing property of HA helps maintain the space that is needed for the bone to form. Additionally, the quick resorption ability of DFDBA can promote bone turnover to quickly form bone in the sinus cavity.
No autogenous graft was used in our approach since it injects another trauma to the oral cavity and most of our patients prefer not to go with this option.
A precise amount of 0.1 mL column of bone was aspirated into a periodontal defect graft syringe and filled into the implant bed and pushed with gentle force into the sinus cavity by the osteotome instruments. After a total of 0.3 mL of bone was filled (Figures 3B and 5A), CBCT scanning procedure was performed before the flap closure. The flap was then secured with 4‐0 Vicryl interrupted and horizontal mattress sutures to obtain tension free primary wound healing.
Figure 5.
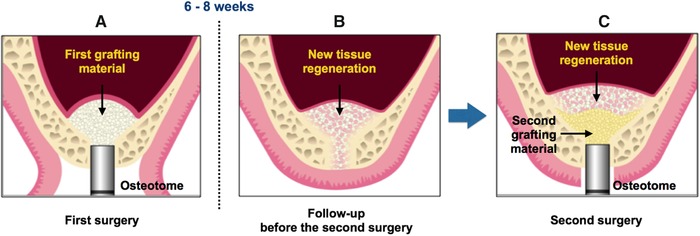
Diagram illustrating the surgical steps of CSA. (A) Step 1. Osteotome followed by sinus augmentation with the first grafting material (HA mixed with osteogen with high contrast). (B) Follow‐up right before the second surgery. (C) Step 2. Second surgery is performed by inserting the second amount of grafting material (DFDBA without high contrast) after osteotome. Implant placement is simultaneously performed
2.4. Evaluation of wound healing
Sutures were removed after 2 weeks. Soft tissue healing was monitored and recorded carefully during healing period to evaluate any complications at the surgical site and the effect of these complications, if any.
2.5. Second stage
Six to 8 weeks after the first surgery, second‐stage surgery with implant placement was performed. The reason for using the 6 to 8 weeks is to allow the soft tissue to completely heal as well as reduce inflammatory response11, 12 that occurred after first surgery so we can ensure undisturbed wound healing under primary wound closure. A crestal incision was made to expose the previous surgical site. Similar procedure of osteotome was performed at the proposed implant placement site. Before the implant was placed, the grafted materials previously in the osteotomy site was carefully removed with trephine and samples were saved for another planned study. The removed grafted materials were 2 to 3 mm deep from the sinus floor to evaluate the characteristics of grafted material in the maxillary sinus. An implant bed was prepared in the proposed position identified by previous CBCT scan result. To replace the removed grafting materials, a precise amount of 0.2 mL column of bone was aspirated into a syringe and filled in the implant bed, once or twice to obtain optimal bone grafting. The surgical site was subjected to CBCT scanning after every 0.2 mL bone placement (Figures 3D, 3E, and 5C). Cover screws for all the implants were placed. Patients were sent for prosthetic treatment 6 months post‐surgery.
2.6. CBCT measurement
All radiographic images were obtained by CBCT.5 Coronal and cross sectional images were integrated to measure the vertically elevated heights. Maximum mesio‐distal elevated distance (MD) was measured on the coronal place and the maximum bucco‐palatal elevated height (BP) and maximum vertically elevated height (VH) were measured on the cross sectional plane.
VH was measured from the implant bed of the crestal bone to the highest point of the bone level below the sinus membrane. BP, as buccal–palatal new bone formation, was measured from the most buccal to the most palatal level of bone on cross‐sectional images. MD, as mesial–distal new bone formation, was measured from the most mesial to the most distal level of bone on sagittal images (Figures 1E and 1F).
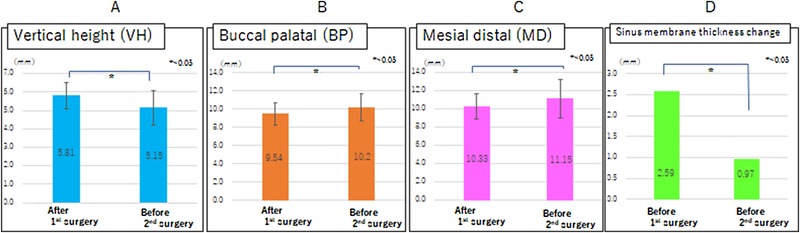
Figure 1.

New bone regeneration after the first and the second surgery of CSA procedure. (A) The vertical height of bone formation. (B) Bone formation measured at the buccal–palatal (BP) dimension. (C) Bone formation measured at the medial–distal (MD) dimension. (D) and (E) show the method used to measure needed data. Vertical height (VH) was measured from the crestal bone to the grafted bone at the midline saggital plane. At the same plane, buccal–palatal (BP) bone was measured at the meeting point of grafted bone and the buccal and palatal limits of the sinus. Medial–distal (MD) bone formation was measured at the most grafted bone shown on the coronal plane
2.7. Data analysis
All the parameters were presented as mean ± SD (mm). ANOVA test using statistical software for Macintosh6 was analyzed to identify the difference of new bone height in different surgical stages with different amount of grafting materials.
3. RESULTS
Overall we are reporting on 19 subjects who were treated in a similar manner (11 females and 8 males, average age of 55.3 ± 9.48), of which 28 sites were included: 1 in the first premolar sites, 4 in the second premolar sites, 11 in the first molar sites and the remaining 12 in the second molar sites. Initial mean vertical bone height before sinus augmentation procedure was 4.95 ± 1.26 m.
3.1. New bone formation
New bone formation after the first and the second surgeries was summarized in Table 1. In the first surgery, 0.3 mL grafting material was inserted into all sites (Figure 3B). In the second surgery, 13 sites were filled with 0.2 mL grafting material (Figure 3D) and 15 sites were filled with 0.4 mL grafting material (Figure 3E). The goal of the two‐stage approach is to achieve 12 mm of total bone height from the crestal ridge to facilitate 10 mm implant placement (Figures 3F and 4B), hence either 0.2 or 0.4 mL of bone graft materials was placed to ensure this height was achieved but also control the amount of materials placed. No damage was observed in the maxillary sinus floor membrane after 0.2 mL filling. One case was reported to have sinus membrane perforation after filling 0.4 mL grafting material (success rate 14/15). The case was successfully managed without further surgical intervention. Only post‐surgery antibiotics (Amoxicillin 500 mg t.i.d. for 7 days) were prescribed. The sites healed uneventfully after 6‐month with implant placement. The average period between the first and the second surgery was 49.04 ± 8.11 days (41 to 63 days) (Figures 3C and 5B).
Table 1.
Amount of vertical bone height gained (via cone beam computed tomography) after graft insertion at different stages
| New vertical bone height (VH) (mean ± SD) | Bucco‐palatal bone height (BP) (mean ± SD) | Mesio‐distal bone height (MD) (mean ± SD) | |
|---|---|---|---|
| First surgery–0.3 mL grafting material | 5.81 ± 0.7 (mm) | 9.54 ± 1.22 (mm) | 10.33 ± 1.4 (mm) |
| Before second surgery– | 5.15 ± 0.91 (mm) | 10.20 ± 1.46 (mm) | 11.15 ± 2.09 (mm) |
| Second surgery–0.2 mL grafting material | 6.69 ± 0.89 (mm) | 11.10 ± 1.3 (mm) | 12.01 ± 2.27 (mm) |
| Second surgery–0.4 mL grafting material | 8.11 ± 1.24 (mm) | 12.47 ± 1.5 (mm) | 13.94 ± 2.97 (mm) |
Figure 4.
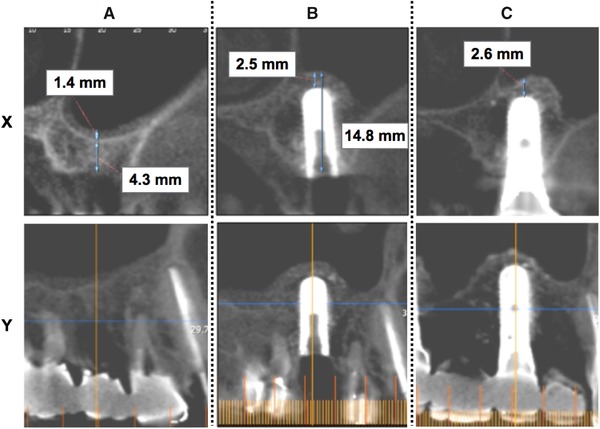
High magnification of images A, F, and G in Figure 3. The crestal bone height before CSA procedure was 4.3 mm. Sinus membrane thickness was 1.4 mm (A). After implant placement, crestal bone height including implant and underneath newly formed tissue is 14.8 mm. The newly formed tissue including newly regenerated bone is 2.5 mm (B). In 6‐year 10 months follow‐up (C), the newly formed tissue is 2.6 mm. X shows images in sagittal plane, while Y shows images in coronal plane
3.2. New vertical bone height (VH)
CBCT results showed an increase of 5.81 ± 0.7 mm vertical bone height after 0.3 mL grafting material was added in the first stage surgery and 5.15 ± 0.91 mm before the second surgery (Figure 2A). All 28 sites received 0.2 mL grafting material at the second surgery, an average of 6.69 ± 0.89 mm new bone height was reported. Meanwhile, 15 sites required an additional 0.2 mL bone graft to achieve additional 8.11 ± 1.24 mm new bone height to have 12 mm total vertical height to allow a 10 mm implant placement (Table 1 and Figure 1A).
Figure 2.
Comparison of the bone formation between the first and the second surgery during the CSA procedure. (A) Vertical bone height (VH), (B) buccal–palatal (BP) bone height, (C) mesial‐distal (MD) bone height, and (D) changes of the sinus membrane thickness (MT) at the first and the second surgery. *P < 0.05 analyzed by t‐test
3.3. Bucco‐palatal new bone height (BP)
At the first surgery where 0.3 mL grafting material was added, new bone height was reported as 9.54 ± 1.22 mm bucco‐palatally (Table 1). Before the second surgery, interestingly, bucco‐palatal new bone height was reported as 10.20 ± 1.46 mm (Figure 2B). After 0.2 and 0.4 mL grafting material were added, 11.10 ± 1.3 and 12.47 ± 1.5 mm new bucco‐palatal bone height were reported, respectively (Figure 1B).
3.4. Mesio‐distal new bone height (MD)
At the first surgery where 0.3 mL grafting material was added, new mesial–distal bone height was reported as 10.33 ± 1.4 mm. Six to 8 weeks later, before the second surgery, interestingly, mesio‐distal new bone height increased up to 11.15 ± 2.09 mm (Figure 2C). After 0.2 and 0.4 mL grafting material were added, 12.01 ± 2.27 mm and 13.94 ± 2.97 mm new mesio‐distal bone height were reported, respectively (Figure 1C).
3.5. Shrinkage of maxillary sinus membrane
The maxillary sinus membrane thickness before the first surgery was 2.6 ± 2.59 mm. However, before the second surgery the sinus membrane thickness has shrinkage to 0.97 ± 1.59 mm, a significant reduction of 1.6 mm sinus membrane thickness between the two surgeries was observed (Figure 2D).
3.6. Bone height change during the procedure time
A slight change of bone height in all dimensions was recorded during the procedure, after the first surgery and before the second surgery (Figure 2). Specifically, the vertical bone height decreased from 5.41 to 5.15 mm (Figure 2A). Bucco‐palatal and mesio‐distal bone, on the other hand, increased in height from 9.54 to 10.2 mm and from 10.33 to 11.15 mm (Figures 2B and 2C), respectively.
4. DISCUSSION
Results from this clinical series of cases demonstrated that vertical elevation of 6.7 mm maxillary sinus floor membrane was possible without membrane perforation by a staged crestal approach (first surgery: 0.3 mL bone graft and second surgery: 0.2 mL bone graft insertion). Similarly, data from this study also indicated that a 0.7 mL of bone graft (first surgery: 0.3 mL bone graft and second surgery: 0.4 mL bone graft insertion) might lead to an elevation height of 8.11 mm with only one out of 15 cases of membrane perforation. This case series introduced a new technique in which staged crestal bone augmentation was applied as an alternative to lateral window sinus augmentation approach. Two‐staged crestal sinus elevation has been reported in a case report,8 in which sinus membrane was elevated ≈8 to 9 mm with a waiting time between sinus augmentation and implant placement. Our findings are in agreement with above report. As mentioned by Bragger et al. (2004),13 who reported 2 mm of graft shrinkage after SCA, hence to place 10 mm length of implant, generally 12 mm of height is needed. Based upon our observations in this clinical series of patients, staged SCA approaches are possible to safely place 10 mm length of implant in case with remaining bone height of 4 to 6 mm. Therefore, the advantages of proposed staged crestal approach include but are not limited to being less invasive compared with the lateral window sinus augmentation, minimized membrane perforation with a significant amount vertical height elevation (6 to 8 mm). However, the limitations of this approach are the two surgical procedures and the potential for the thinning the sinus membrane. Hence, the staged crestal sinus approach should only be indicated in patients with moderate remaining bone (4 to 6 mm) and prefer to have a more conservative approach via crestal wall instead of lateral window approach.
It is noted that new bucco‐palatal bone height increased to 10.20 ± 1.46 mm before the second surgery compared with that of after the first surgery, which was 9.54 ± 1.22 mm (Figure 2B). Similarly, new mesio‐distal bone height increased from 10.33 ± 1.4 to 11.15 ± 2.09 mm 6 to 8 weeks after 0.3 mL bone was grafted into the sinus floor (Figure 2C). One study reported a positive correlation between sinus graft volume and membrane swelling i early phases.14 These authors found an increased membrane thickness 3 months after the surgery14 whereas the SCA studies reported a normal thickness value after 1 month.15, 16 According to these data, it seems that the less invasive surgery and less membrane de‐attachment, the faster recovery of normal thickness values and sinus function. Temmerman et al. reported that both SCA, lateral sinus lift and intra‐lift techniques caused a temporary thickening of the membrane, with a statistically significant change in membrane volume for the lateral sinus lift versus SCA.17 In this situation, the very limited trauma caused by surgery in our study with a progressive de‐attachment of the membrane may explain that only some membranes suffered with inflammatory thickening and most, even with shrinkage. Nonetheless, it should be noted that higher accuracy than 0.5 mm cannot be expected with a clinical use of CBCT18 and that CBCT measurement might overestimate the histologic real thickness of the membrane19; therefore, measurement of thinner structures like SM might not be totally precise and should be taken cautiously. These findings can be explained by the graft condensation. Another possible explanation for this is a rebounding tension produced by the elevated sinus floor that makes the graft material spread more horizontally and reduce its height.
In our case series, we observed an average of 1.6 mm reduction in thickness of the sinus membrane which occurred 6 weeks after the crestal sinus lift procedure (Figure 2D). In one study by Quirynen et al.,13 a clear and transient swelling and thickening of sinus membrane after a crestal sinus lift procedure was reported. Similarly, a transient thickening of sinus membrane after a lateral sinus lift procedure was also reported.15 In our cases, a 5 to 10 times increase in thickness of the sinus membrane was noted and that effect decreased through time, specifically 1 month after the second surgery without any types of complication. It is reported that the inflammation degree of sinus floor membrane after lateral sinus augmentation is severe and long‐lasting because of the large elevation area.3, 10, 11 On the other hand, the crestal sinus approach has been reported to cause less swelling and discomfort to the patients because of minimal invasion and smaller elevated areas.19 An explanation for the reduced degree of inflammation in crestal sinus augmentation was because of the reduced number of inflammatory factors that could be activated by peeling off the large area of membrane during the procedure.11 This also explains the significant shrinkage of maxillary sinus membrane before the second surgery, which identifies 6 to 8 weeks as an appropriate waiting time between the two procedures.
Within the limitations of this case series, the new proposed staged crestal maxillary sinus elevation is an effective and safe approach in elevating 6 or 8 mm alveolar bone height without causing membrane perforation (Figures 3G and 4C). However, the two‐stage approach was only used in the limited residual bone height (4 to 6 mm) and required two separate surgical procedures. Further, patients with systemic disease, sinusitis, and anatomic limitation such as septum, posterior alveolar artery, partial lack of sinus floor bone, aberration of sinus floor membrane into sinus floor bone are contraindications for the procedure. Future randomly controlled clinical trials with larger sample size and long‐term follow‐up are needed to verify the observations reported in this case series.
ACKNOWLEDGMENT
The authors do not have any financial interests, either directly or indirectly, in the products or information listed in the paper.
Sonoda T, Yamamichi K, Harada T, Yamamichi N. Effect of staged crestal maxillary sinus augmentation: A case series. J Periodontol. 2020;91:194–201. 10.1002/JPER.18-0632
Footnotes
VarioSurg SG16B, Nakanishi, Japan.
Osteotome‐G No.37, Kyocera, Japan.
HA, Osteogen, Impladent Ltd., Holliswood, NY.
DFDBA Salvin Dental, Charlotte, NC.
PreVista, Kyocera Medical, Osaka, Japan.
Rstudio Version 1.1.383, Rstudio, Inc., Boston, MA.
REFERENCES
- 1. Boyne PJ, James RA. Grafting of the maxillary sinus floor with autogenous marrow and bone. J Oral Surg. 1980;38:613‐616. [PubMed] [Google Scholar]
- 2. Summers RB. A new concept in maxillary implant surgery: the osteotome technique. Compendium. 1994;15:154‐156. [PubMed] [Google Scholar]
- 3. Wang HL, Katranji A. ABC sinus augmentation classification. Int J Periodontics Restorative Dent. 2008;28:383‐389. [PubMed] [Google Scholar]
- 4. Sonoda T, Harada T, Yamamichi N, Monje A, Wang HL. Association between bone graft volume and maxillary sinus membrane elevation height. Int J Oral Maxillofac Implants. 2017;32:735‐740. [DOI] [PubMed] [Google Scholar]
- 5. Peleg M, Garg AK, Mazor Z. Predictability of simultaneous implant placement in the severely atrophic posterior maxilla: a 9‐year longitudinal experience study of 2132 implants placed into 731 human sinus grafts. Int J Oral Maxillofac Implants. 2006;21:94‐102. [PubMed] [Google Scholar]
- 6. Soardi CM, Spinato S, Zaffe D, Wang HL. Atrophic maxillary floor augmentation by mineralized human bone allograft in sinuses of different size: a histologic and histomorphometric analysis. Clin Oral Implants Res. 2011;22:560‐566. [DOI] [PubMed] [Google Scholar]
- 7. Chen L, Cha J. An 8‐year retrospective study: 1,100 patients receiving 1,557 implants using the minimally invasive hydraulic sinus condensing technique. J Periodontol. 2005;76:482‐491. [DOI] [PubMed] [Google Scholar]
- 8. Bernardello F, Massaron E, Spinato S, Zaffe D. Two‐Stage crestal sinus elevation by sequential drills in less than 4 mm of residual ridge height: a clinical and histologic case report. Implant Dentistry. 2014;23:378‐386. [DOI] [PubMed] [Google Scholar]
- 9. Friedmann A, Dard M, Kleber BM, Bernimoulin JP. Bosshardt DD. Ridge augmentation and maxillary sinus grafting with a biphasic calcium phosphate: histologic and histomorphometric observations. Clin Oral Implants Res. 2009;20:708‐714. [DOI] [PubMed] [Google Scholar]
- 10. Insua A, Monje A, Chan H‐L, Wang H‐L. Association of inflammatory status and maxillary sinus Schneiderian membrane thickness. Clin Oral Investig. 2018;22:245‐254. 10.1007/s00784-017-2105-3. [DOI] [PubMed] [Google Scholar]
- 11. Aimetti M, Romagnoli R, Ricci G, Massei G. Maxillary sinus elevation: the effect of macrolacerations and microlacerations of the sinus membrane as determined by endoscopy. Int J Periodontics Restorative Dent. 2001;21:581‐589. [PubMed] [Google Scholar]
- 12. Bragger U, Gerber C, Joss A, et al. Patterns of tissue remodeling after placement of ITI dental implants using an osteotome technique: a longitudinal radiographic case cohort study. Clin Oral Implants Res. 2004;15:158‐166. [DOI] [PubMed] [Google Scholar]
- 13. Quirynen M, Lefever D, Hellings P, Jacobs R. Transient swelling of the Schneiderian membrane after transversal sinus augmentation: a pilot study. Clin Oral Implants Res. 2014;25:36‐41. [DOI] [PubMed] [Google Scholar]
- 14. Makary C, Rebaudi A, Menhall A, Naaman N. Changes in sinus membrane thickness after lateral sinus floor elevation: a radiographic study. Int J Oral Maxillofac Implants. 2016;31:331‐337. [DOI] [PubMed] [Google Scholar]
- 15. Scala A, Botticelli D, Rangel IG, Jr , de Oliveira JA, Okamoto R, Lang NP. Early healing after elevation of the maxillary sinus floor applying a lateral access: a histological study in monkeys. Clin Oral Implants Res. 2010;21:1320‐1326. [DOI] [PubMed] [Google Scholar]
- 16. Temmerman A, Van Dessel J, Cortellini S, Jacobs R, Teughels W, Quirynen M. Volumetric changes of grafted volumes and the Schneiderian membrane after transcrestal and lateral sinus floor elevation procedures: a clinical, pilot study. J Clin Periodontol. 2017;44:660‐671. [DOI] [PubMed] [Google Scholar]
- 17. Insua A, Monje A, Chan HL, Zimmo N, Shaikh L, Wang HL. Accuracy of Schneiderian membrane thickness: a cone‐beam computed tomography analysis with histological validation. Clin Oral Implants Res. 2017;28:654‐661. [DOI] [PubMed] [Google Scholar]
- 18. Monje A, Tatiana K, Aranda L, Insua A, Garcia‐Nogales Wang H‐L. Schneiderian membrane thickness and clinical implications for sinus augmentation: a systematic review and meta‐regression analysis. J Periodontol. 2016;87:888‐899. 10.1902/jop.2016.160041. [DOI] [PubMed] [Google Scholar]
- 19. Wen SC, Lin YH, Yang YC, Wang HL. The influence of sinus membrane thickness upon membrane perforation during transcrestal sinus lift procedure. Clin Oral Implants Res. 2015;26:1158‐1164. [DOI] [PubMed] [Google Scholar]


