Abstract
ST-segment elevation myocardial infarction (STEMI) equivalent patterns make the diagnosis of STEMI very challenging. We present a case of de Winter’s pattern (dWp) in a man admitted to the emergency department for chest pain who developed cardiogenic shock despite successful percutaneous coronary intervention. Electrocardiograms performed at arrival, after 10 minutes, and the day after the revascularization demonstrated a dynamic and rapid evolution of dWp. Our case underlines the importance to promptly recognize dWp as a STEMI equivalent pattern to advance the patient to a rapid reperfusion strategy and confirms the high-risk and probably evolutive feature of this sign.
Résumé
Les équivalents STEMI, ces événements qui se présentent comme un infarctus du myocarde avec élévation du segment ST (STEMI), compliquent beaucoup le diagnostic de ce dernier. Nous présentons le cas d’un complexe de « de Winter » chez un homme admis à l’urgence pour une douleur thoracique et ayant présenté un choc cardiogénique malgré une intervention coronarienne percutanée réussie. Les électrocardiogrammes réalisés à l’arrivée, 10 minutes plus tard et le lendemain de la revascularisation montraient une évolution dynamique et rapide d’un complexe de « de Winter ». Le cas présenté fait ressortir l’importance de savoir reconnaître promptement le complexe de « de Winter » comme étant un équivalent STEMI afin d’appliquer sans délai une stratégie de reperfusion appropriée, et confirme le risque élevé et le caractère vraisemblablement évolutif de ce signe.
Electrocardiograms (ECGs) play a pivotal role in the diagnosis of patients with suspected ST-segment elevation myocardial infarction (STEMI), allowing rapid treatment. In some cases, patients may have an initial ECG without ST-segment elevation, making the diagnosis very challenging.1 This is the case of STEMI equivalent patterns, such as hyperacute T waves, de Winter’s pattern (dWp), Wellens syndrome, and posterior STEMI.1 Among these, dWp is characterized by loss of R waves in the precordial leads associated with up-sloping ST-segment depression at J-point > 1 mm and tall positive symmetrical T waves.2,3 Additional features are a notch in the negative limb of the QRS complexes in the precordial leads and slight ST-elevation in the augmented vector right lead.2,3
Case
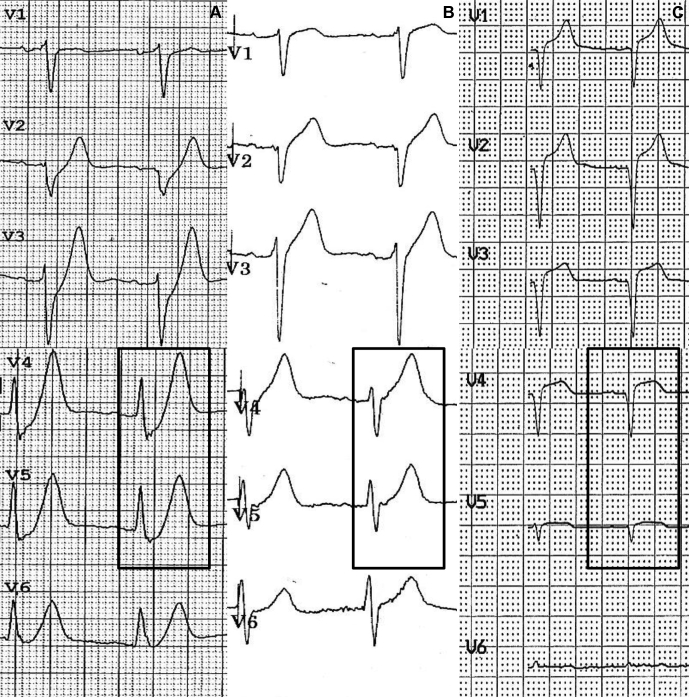
A 47-year-old man was urgently admitted to the emergency department reporting chest pain for 20 minutes. The patient was a smoker, without previous cardiovascular disease. ECG showed dWp in precordial leads, especially in leads V4 and V5 (Fig. 1, A and B), and urgent coronary angiography, performed within 40 minutes from the emergency department admission, showed the occlusion of the proximal left anterior descending coronary artery (Fig. 1C). Despite prompt and successful revascularization with primary percutaneous coronary intervention not complicated by no-reflow phenomenon, the patient developed acute pulmonary oedema. Invasive ventilation was started, and the circulation was supported by an intra-aortic balloon pump and dobutamine and norepinephrine infusions. Laboratory test results revealed a dramatic increase of troponin I (peak 639,000 ng/L, normal values < 60 ng/L), and transthoracic echocardiography showed a moderate reduction of left ventricular ejection fraction (40%) due to mid septum, mid anterior wall, and apical segmental akinesia, confirming what was observed in a focused cardiac ultrasound examination performed in the emergency department before the percutaneous revascularization (Fig. 1D; Video 1 , view video online). The analysis of the ECGs performed at arrival in the emergency department, at 10 minutes, and the day after the revascularization (Fig. 2) demonstrated dynamic and rapid evolution of dWp in precordial leads (Fig. 2A) with the regression of up-sloping ST-segment depression (Fig. 2B) and the subsequent appearance of Q waves (Fig. 2C), indicating the development of necrosis despite complete revascularization. Despite the dramatic acute decompensation, the patient was discharged on day 17 in good general condition.
, view video online). The analysis of the ECGs performed at arrival in the emergency department, at 10 minutes, and the day after the revascularization (Fig. 2) demonstrated dynamic and rapid evolution of dWp in precordial leads (Fig. 2A) with the regression of up-sloping ST-segment depression (Fig. 2B) and the subsequent appearance of Q waves (Fig. 2C), indicating the development of necrosis despite complete revascularization. Despite the dramatic acute decompensation, the patient was discharged on day 17 in good general condition.
Figure 1.
(A) Electrocardiogram showing de Winter’s pattern (dWP). (B) Magnification of precordial leads presenting the typical features of dWP: loss of R waves in V1-V3 associated with up-sloping ST-segment depression at J-point, tall positive symmetrical T waves, and a notch in the negative limb of the QRS complexes in V4-V5 leads (asterisks). (C) Coronary angiography showing the occlusion of the left anterior descending coronary artery. (D) Transthoracic echocardiography showing moderate reduction of left ventricular ejection fraction due to mid septum, mid anterior wall, and apical segmental akinesia (white arrows).
Figure 2.
Evolution in dWP in 3 consecutive ECGs (black box focalizes the evolution in V4-V5 leads). (A) ECG registered at the arrival to the emergency department displays the typical dWP. (B) ECG performed after 10 minutes shows the regression of up-sloping ST-segment depression and the persistence of hyperacute T waves. (C) ECG obtained the day after the revascularization demonstrates the appearance on Q waves in the precordial leads.
Discussion
The dWp was first described by de Winter and colleagues2 in 2008 as an equivalent of STEMI due to proximal left anterior descending coronary artery occlusion. Its prevalence is approximately 1.6% to 2% of anterior STEMIs,2,4 but a recent study suggests a higher prevalence.5 This pattern is associated with a mortality of approximately 27% within the first week.4 A clear explanation of this ECG pattern remains elusive. The lack of activation of the sarcolemmal adenosine triphosphate–sensitive potassium channel is believed to be the cause of the absence of ST-segment elevation, as observed in adenosine triphosphate–sensitive potassium channel knock-out animal models.2 It has also been proposed that the absence of ST-segment elevation could be due to subendocardial localization of the ischemia. According to this explanation, the loss of R waves in the precordial leads and the notch in the negative limb of QRS complexes would be due to conduction slowing over the anterior subendocardium with initial activation of the opposite wall and late activation of the anterior subepicardium. The ST-segment depression would be related to the negative voltage difference between the subendocardial and the subepicardial action potentials during the plateau phase, and the peaked T waves would be the expression of the shorter time duration between subendocardial and subepicardial repolarization.6 Although dWp has been considered as a static ECG pattern in previous observational studies,2,3 a recent retrospective study seems to demonstrate that it is a transient ECG phenomenon related to the first phases of myocardial ischemia.5
Conclusion
Our clinical case underlines the importance of promptly recognizing dWp as a STEMI equivalent pattern to advance the patient to a rapid reperfusion strategy and confirms the high-risk and the probable evolutive feature of this sign.
Novel Teaching Points.
-
•
STEMI equivalent patterns make the diagnosis of STEMI very challenging.
-
•
dWP is characterized by loss of R waves in the precordial leads associated with up-sloping ST-segment depression at J-point > 1 mm and tall positive symmetrical T waves; additional features are a notch in the negative limb of the QRS complexes in the precordial leads and a slight ST elevation in the augmented vector right lead.
-
•
dWP is associated with a high mortality within the first week, and it seems to be a transient ECG phenomenon.
-
•
It is fundamental to promptly recognize dWP as a STEMI equivalent pattern to advance the patient to a rapid reperfusion strategy.
Funding Sources
The authors have no funding sources to disclose.
Disclosures
The authors have no conflicts of interest to disclose.
Footnotes
Ethics Statement: The research reported has adhered to the relevant ethical guidelines.
See page 24 for disclosure information.
To access the supplementary material accompanying this article, visit CJC Open at https://www.cjcopen.ca/ and at https://doi.org/10.1016/j.cjco.2019.11.001.
Supplementary Material
Transthoracic echocardiography: Apical 4-chamber view focused on left ventricle showing moderate reduction of left ventricular ejection fraction due to mid septum and apical segmental akinesia.
References
- 1.Lawner B.J., Nable J.V., Mattu A. Novel patterns of ischemia and STEMI equivalents. Cardiol Clin. 2012;30:591–599. doi: 10.1016/j.ccl.2012.07.002. [DOI] [PubMed] [Google Scholar]
- 2.de Winter R.J., Verouden N.J., Wellens H.J., Wilde A.A. for the Interventional Cardiology Group of the Academic Medical Center. A new ECG sign of proximal LAD occlusion. N Engl J Med. 2008;359:2071–2073. doi: 10.1056/NEJMc0804737. [DOI] [PubMed] [Google Scholar]
- 3.de Winter R.W., Adams R., Verouden N.J., de Winter R.J. Precordial junctional ST-segment depression with tall symmetric T-waves signifying proximal LAD occlusion, case reports of STEMI equivalence. J Electrocardiol. 2016;49:76–80. doi: 10.1016/j.jelectrocard.2015.10.005. [DOI] [PubMed] [Google Scholar]
- 4.de Winter R.W., Adams R., Amoroso G. Prevalence of junctional ST-depression with tall symmetrical T-waves in a pre-hospital field triage system for STEMI patients. J Electrocardiol. 2019;52:1–5. doi: 10.1016/j.jelectrocard.2018.10.092. [DOI] [PubMed] [Google Scholar]
- 5.Xu J., Wang A., Liu L., Chen Z. The de Winter electrocardiogram pattern is a transient electrocardiographic phenomenon that presents at early stage of ST-segment elevation myocardial infarction. Clin Cardiol. 2018;41:1177–1184. doi: 10.1002/clc.23002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gorgels A.P.M. Explanation for the electrocardiogram in subendocardial ischemia of the anterior wall of the left ventricle. J Electrocardiol. 2009;42:248–249. doi: 10.1016/j.jelectrocard.2009.01.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Transthoracic echocardiography: Apical 4-chamber view focused on left ventricle showing moderate reduction of left ventricular ejection fraction due to mid septum and apical segmental akinesia.