Abstract
Background:
This was a meta-analysis of continuous positive airway pressure (CPAP) compliance. We compared telemonitor (TM) care with usual care and supervised PAP titration (SPT) in the sleep unit with home auto-adjusting pressure titration (HAPT) in patients with obstructive sleep apnea (OSA).
Methods:
We searched PubMed, Web of Science, Scopus, and Medline for appropriate randomized controlled trials (RCTs) that compared TM care with usual care for patients with OSA. Review Manager 5.3 was used for all comparisons and analyses.
Results:
Our meta-analysis included 19 studies involving a total of 2464 patients with OSA; CPAP compliance was significantly higher in the TM care group [mean difference (MD) 0.68 h, 95% confidence interval (CI) 0.48–0.89 h, I2 = 49%] compared with the usual care group. When we compared SPT and HAPT, two groups did not exhibit significantly different levels of CPAP compliance (MD −0.34 h, 95% CI −0.72–0.05 h, I2 = 91%). Subgroup analysis comparing the SPT with HAPT in CPAP compliance was grouped by follow-up time (⩾3 months or <3 months). Once again, there were no between-group differences in either long-term (MD = 0.56 h, 95% CI = 1.39–0.26 h, I2 = 91%), or short-term (MD = 0.34 h, 95% CI = 0.26–0.27 h, I2 = 14%) follow up.
Conclusions:
TM care was associated with significantly greater CPAP compliance compared with usual care. Also, HAPT was not inferior to SPT for CPAP compliance.
Keywords: CPAP compliance, obstructive sleep apnea, telemonitor
Introduction
Obstructive sleep apnea (OSA) is caused by a blockage or obstruction of the airway, and features a range of symptoms, including snoring, episodes of oxygen desaturation, and arousals from sleep. The prevalence of OSA increases with age1; among middle-aged people, it influences more than 20% of males and more than 8% of females.2 Health care resources related to the diagnosis and treatment of OSA are reportedly inadequate.3 OSA poses a range of risks, including hypertension, stroke, heart failure, etc.2,4,5 Some of these risks can be alleviated by continuous positive airway pressure (CPAP) treatment. Especially for patients with moderate and severe OSA, CPAP has been recommended as a first-line treatment.6
Compliance is important during CPAP treatment. Over the past two decades, several psychoeducational and technological interventions (e.g. group education sessions,7 intensive patient education and support protocol,8,9 and motivational enhancement programs10) have emerged with the common goal of increasing CPAP compliance. Most of these interventions have demonstrated only a modest impact on compliance. Moreover, intensive support protocols still required substantial time and resources to implement.
Current technological advances have facilitated telemonitor (TM) care in routine clinical practice.11,12 In addition, the devices that patients use can auto-adjust pressure titration at home without the supervision of sleep technicians/doctors.13,14 Few prior integrated studies or and meta-analyses have been used to guide clinical practice. We sought to carry out a comprehensive meta-analysis of previously published studies that examined supervised PAP titration (SPT) and home auto-adjusting pressure titration (HAPT), and follow-up procedures, including TM care or usual care, with regards to CPAP compliance.
Methods
Search strategy
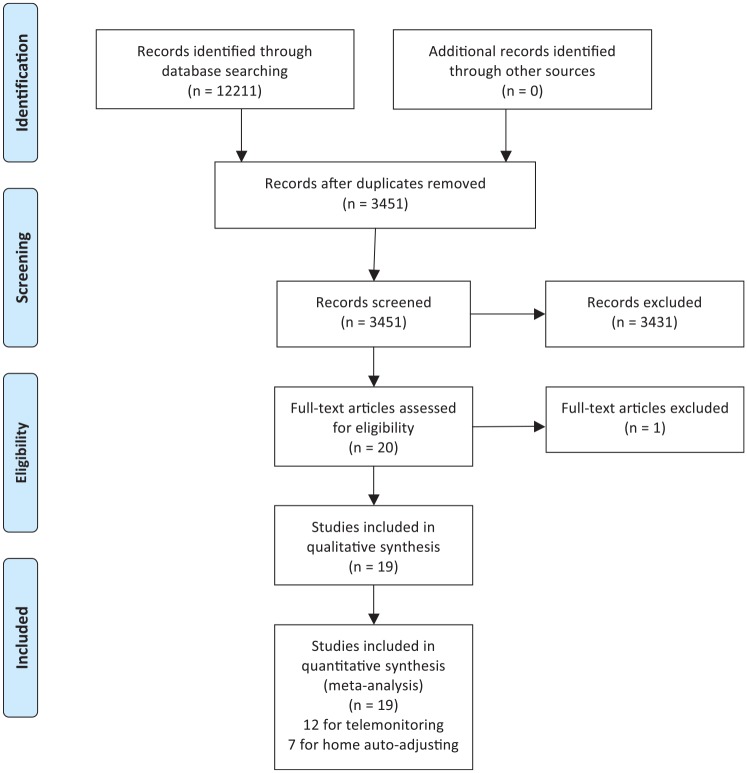
Two investigators independently searched articles from several databases (PubMed, Web of Science, Scopus, and Medline). The reference lists of eligible studies and relevant papers were also searched manually and reviewed. The search terms included ‘OSA’, ‘obstructive sleep apnea’, ‘OSAHS’, ‘obstructive sleep apnea and hypopnea syndrome’, ‘sleep apnea’, ‘compliance’, and ‘adherence’. In PubMed, we used (‘OSA’ or ‘OSAHS’ or ‘obstructive sleep apnea’ or ‘obstructive sleep apnea and hypopnea syndrome’ or ‘sleep apnea’) and (‘compliance’ or ‘adherence’). The final search date was 17 August 2019. The search terms and search strategies for two topics (topic 1: TM care versus usual care; topic 2: SPT versus HAPT) are shown in the supplementary data. We identified 3451 articles after removal of duplications. We excluded 3431 articles by reading the title and abstract. Finally, there were 19 included RCTs (13 studies for topic 1, and 6 studies for topic 2.11–29 (Figure 1)
Figure 1.
Flow diagram for selection of appropriated articles.
Inclusion and exclusion
Inclusion criteria: randomized controlled trial (RCT) primary comparing TM care with usual care, and SPT to HAPT; primary outcome: CPAP compliance; published in English.
We excluded studies that were reviews, retrospective research, or case reports; and studies that did not report insufficient data [e.g. no reports of precise CPAP usage time or rates of CPAP compliant (>4 h) patients].
Data extracted
Two authors (Chongxiang Chen and Lanlan Pang) independently reviewed the identified abstracts and selected articles for full review. A third reviewer (Wei Liao) was brought in to address any discrepancies. For each selected publication, the following baseline and study characteristics were extracted: first author, publication year, country, participant characteristics, follow-up time, and baseline characteristics (Table 1). Interventions included in our studies comprised TM care, usual care, SPT, and HAPT. The definitions of TM care in all the included studies involved collecting data on CPAP treatment efficacy (CPAP compliance, air leaks) in real-time, and transmission of treatment data to clinical sleep center staff. The staff would then contact the patients, if necessary, to solve various problems. In the context of these studies, ‘usual care’ meant regular follow-up and face-to-face contact during the treatment period. ‘SPT’ meant that sleep doctors supervised PAP titration based on polysomnography (PSG) in these studies. ‘HAPT’ meant using autotitration pressure at home. All intervention group settings that were included in the studies are shown in Supplementary Tables 1 and 2. The risks of bias for the included studies are presented in Figures 2 and 3. The risk-of-bias analysis showed that all the studies were comparable (high-quality RCTs) and could be integrated. The efficacy outcome measure was CPAP compliance.
Table 1.
Characteristics of baseline patients.
| Study | Country | Jadad score | Intervention | CPAP compliance | Participating centers | Follow up | Patient number |
|---|---|---|---|---|---|---|---|
| Anttalainen16 | Finland | 1+1+0+1=3 | TM care versus Usual care | 6.4 ± 1.2 versus 6.1 ± 1.7 | 1 center | 12 months | 39 versus 49 |
| Fields17 | USA | 2+2+0+1=5 | TM care versus Usual care | 3.68 ± 0.63 versus 2.93 ± 0.61 | 2 centers | 3 months | 14 versus 20 |
| Fox18 | Canada | 2+1+0+1=4 | TM care versus Usual care | 5.35 ± 1.33 versus 3.45 ± 1.77 | 1 center | 3 months | 28 versus 26 |
| Frasnelli19 | Switzerland | 1+1+0+0=2 | TM care versus Usual care | 5.3 ± 1.8 versus 4.43 ± 2.78 | 1 center | 1 month | 113 versus 110 |
| Hoet20 | Belgium | 1+1+0+1=3 | TM care versus Usual care | 5.7 ± 1.6 versus 4.2 ± 1.9 | 1 center | 3 months | 17 versus 20 |
| Hwang21 | USA | 2+1+0+1=4 | TM care versus Usual care | 4.67 ± 2.27 versus 3.8 ± 2.5 | 1 center | 3 months | 263 versus 129 |
| Isetta22 | Spain | 2+2+0+1=5 | TM care versus Usual care | 4.4 ± 2 versus 4.2 ± 2 versus | 8 centers | 6 months | 64 versus 64 |
| Munafo25 | USA | 1+1+0+1=3 | TM care versus Usual care | 5.1 ± 1.9 versus 4.7 ± 2.1 | 1 center | 3 months | 58 versus 64 |
| Stepnowsky11 | USA | 2+2+0+1=5 | TM care versus Usual care | 4.1 ± 1.8 versus 2.8 ± 2.2 | 1 center | 1 month | 20 versus 20 |
| Sparrow28 | USA | 2+1+0+1=4 | TM care versus Usual care | / | 2 centers | 12 months | 112 versus 122 |
| Taylor29 | USA | 2+1+0+1=4 | TM care versus Usual care | 4.29 ± 2.15 versus 4.22 ± 2.05 | 1 center | 1 month | 56 versus 58 |
| Turino12 | Spain | 1+1+0+0=2 | TM care versus Usual care | 5.1 ± 2.1 versus 4.9 ± 2.2 | 1 center | 3 months | 52 versus 48 |
| Antic15 | Australia | 1+1+0+1=3 | Supervised versus Home auto-adjustment | 4.56 ± 0.3 versus 4.11 ± 0.28 | 3 centers | 3 months | 95 versus 100 |
| Berry13 | USA | 1+1+0+1=3 | Supervised versus Home auto-adjustment | 5.25 ± 0.38 versus 5.20 ± 0.28 | 1 center | 1.5 months | 39 versus 40 |
| Kim23 | USA | 1+1+0+1=3 | Supervised versus Home auto-adjustment | 3.65 ± 2.4 versus 4.68 ± 2.1 | Multicenter | 3 months | 61 versus 74 |
| Kuna14 | USA | 1+1+0+1=3 | Supervised versus Home auto-adjustment | 2.92 ± 2.32 versus 3.49 ± 2.45 | 1 center | 3 months | 110 versus 113 |
| Mulgrew24 | Canada | 2+2+0+1=5 | Supervised versus Home auto-adjustment | 5.17 ± 2.1 versus 6.07 ± 1.55 | 1 center | 3 months | 30 versus 31 |
| Rosen26 | USA | 1+1+0+1=3 | Supervised versus Home auto-adjustment | 3.7 ± 2.4 versus 4.7 ± 2.1 | 1 center | 3 months | 61 versus 74 |
| Skomro27 | Canada | 1+1+0+1=3 | Supervised versus Home auto-adjustment | 5.56 ± 2.0 versus 5.96 ± 1.4 | 1 center | 1 month | 37 versus 33 |
CPAP, continuous positive airway pressure; TM, telemonitor.
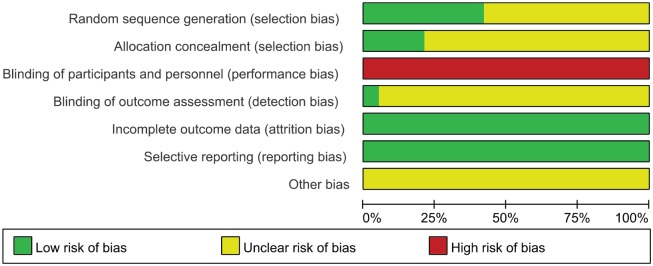
Figure 2.
Risk of bias graph.
Figure 3.
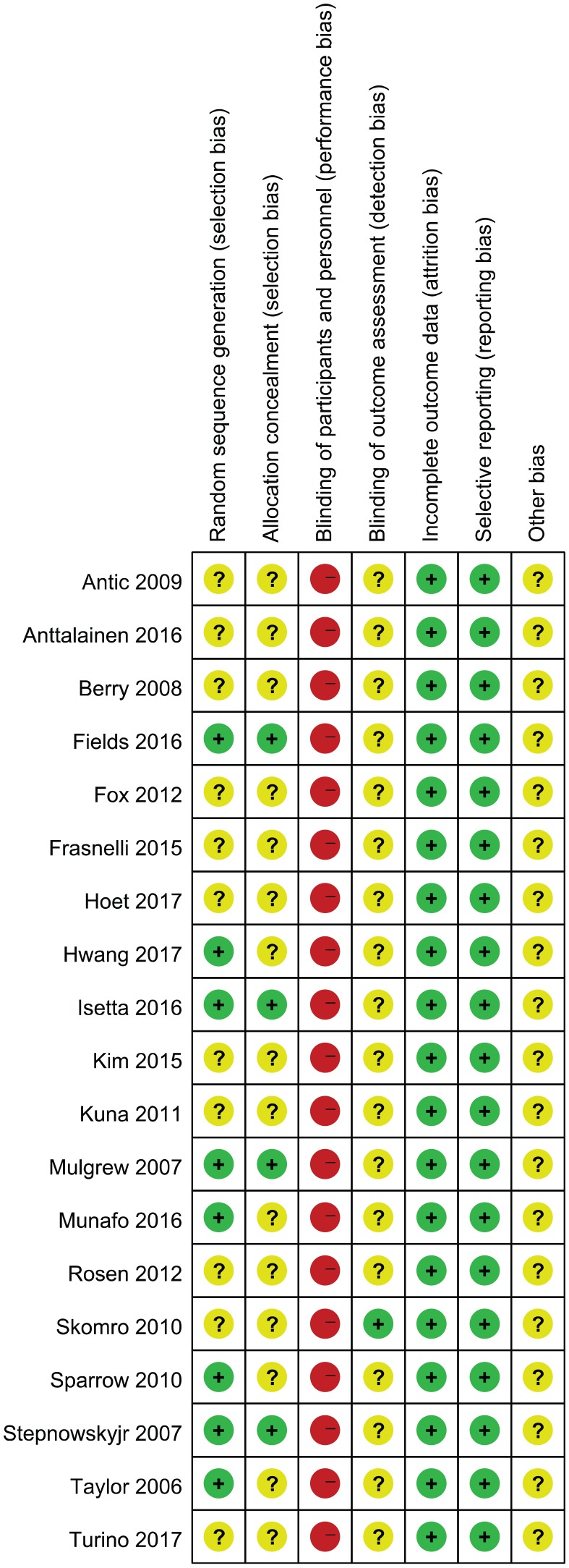
Risk of bias summary.
Risk-of-bias assessment
Trial risk-of-bias was assessed according to the recommendations of the Cochrane Handbook of Systematic Reviews of Interventions, in the following domains: selection bias (random sequence generation and allocation concealment), performance bias (blinding of participants and personnel), detection bias (blinding of outcome assess-ment), attrition bias (incomplete outcome data), and reporting bias (selective outcome reporting) (http://handbook.cochrane.org). The Jadad scale was used to calculate the quality of every enrolled study. In the review of randomization, every study that contained the exact randomized method, we scored as ‘low risk’; however, when the study did not report the exact randomized method, but indicated that the studies were carried out under randomized, controlled designs, we scored them as ‘unclear’, which was similar to other scoring in allocation of randomization, blind method, incomplete outcome data, selective reporting. Other bias sometimes contains unknown risk, so we think we should score all the other bias in every article as ‘unclear’.
Statistic analysis
We pooled data and used mean deviation (MD), with 95% confidence interval (CI) for continuous outcomes: CPAP compliance, Epworth Sleepiness Scale (ESS) change, and changes in the Functional Outcomes of Sleep Questionnaire (FOSQ). We used odds ratios (OR), with 95% CI for the dichotomous outcome: the rate of CPAP compliant (>4 h) patients. We used a fixed-effect model if there was no considerable heterogenous factors among the various studies. We used a random-effects model if the I2 statistic was above 50% and Cochran’s Q statistic had a p value ⩽ 0.1. Funnel plots were used to screen for potential publication bias. All statistical analyses were carried out with Review Manager 5.3 (The Cochrane Collaboration)
Results
The studies included in our meta-analysis were all RCTs, published from 2006 to 2018. The studies were conducted in the USA,11,13,14,17,21,23,25,26,28,29 Spain,12,22 Australia,15 Canada,18,24,27 Belgium,20 Switzerland,19 and Finland.16 Table 1 presents the basic characteristics of included trials and participants’ demographic data. Three trials were multicenter studies,15,17,22,23,28 and the Jadad Scales of all included studies ranged from 2 to 5.
In total, there were 19 RCTs with 2464 patients. These studies addressed OSA treatment and management, and explored which methods could contribute improved CPAP compliance. Article quality evaluation results are presented in Figures 2 and 3.
Telemonitor care versus usual care
CPAP compliance
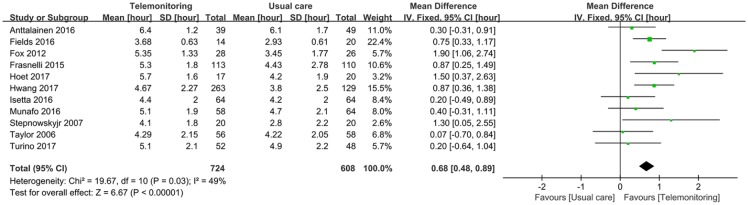
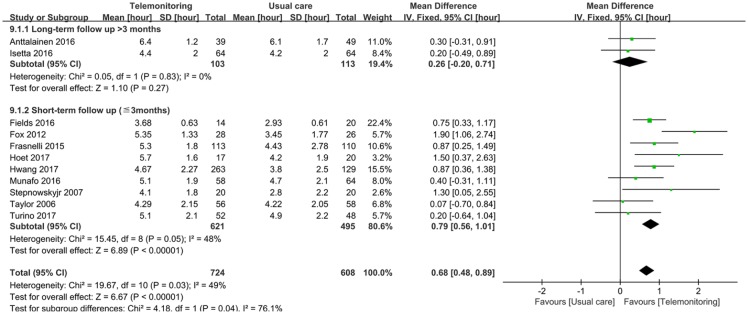
When we compared TM care with usual care, our study indicated that telemonitoring follow up could significantly increase CPAP compliance. Our study included 11 studies with a total of 1332 patients11,12,16–22,25,29; the results showed that the compliance outcome of the TM care group was significantly higher than the usual care group (MD 0.68 h, 95% CI 0.48–0.89 h). Heterogeneity testing revealed I2 = 49%, indicating low heterogeneity (Figure 4). We then analyzed CPAP compliance grouped by follow-up time (>3 months or less). The results showed that TM care group compliance was significantly higher than that in the usual care group (MD 0.79 h, 95% CI 0.56–1.01 h, I2 = 48%) for short-term follow up; however, long-term results were not significantly different (MD 0.26 h, 95% CI −0.20–0.71 h, I2 = 0%; Figure 5).
Figure 4.
CPAP compliance (hours of daily use) comparing TM care with usual care in OSA patients.
CPAP, continuous positive airway pressure; OSA, obstructive sleep apnea; TM, telemonitor.
Figure 5.
Subgroup analysis of CPAP compliance (hours of daily use) comparing TM care with usual care in OSA patients grouped by follow-up time.
CPAP, continuous positive airway pressure; OSA, obstructive sleep apnea; TM, telemonitor.
Additionally, we compared the rate of CPAP compliant (>4 h) patients between the TM care and usual care groups. Here, TM care had a significantly higher rate of CPAP compliant patients than usual care (OR 1.81, 95% CI 1.33–2.46). Heterogeneity testing revealed I2 = 0%, indicating low heterogeneity (Supplementary Figure 1).
ESS change
To compare TM care with usual care in terms of change in ESS, our study included six studies with a total of 726 patients11,16–18,21,25; the results did not show a significant between-group difference (MD 0.12, 95% CI −0.65 to 0.89). Heterogeneity testing revealed I2 = 0%, indicating low heterogeneity (Supplementary Figure 2).
FOSQ change
To compare TM care with usual care for change in FOSQ, we included three studies with a total of 462 patients11,17,21; the results demonstrated a significantly greater change in FOSQ for the TM group (MD 2.05, 95% CI 0.65–3.46). Hetero-geneity testing revealed I2 = 0%, indicating low heterogeneity (Supplementary Figure 3).
Supervised PAP titration versus home autoadjusting pressure titration
CPAP compliance
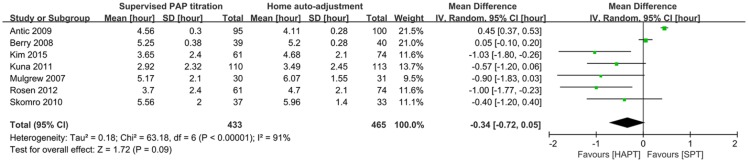
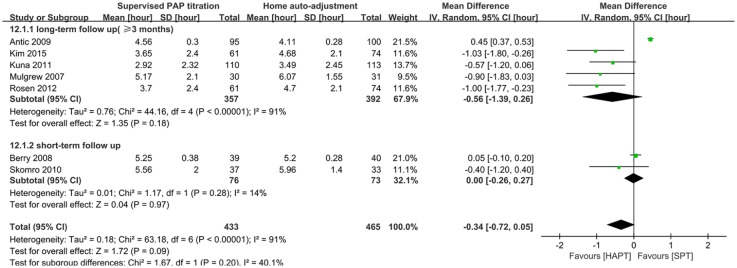
We compared CPAP compliance in patients who underwent SPT or HAPT. Our search strategy revealed seven studies with a total of 898 patients13–15,23,24,26,27; the two groups did not exhibit any significant differences in CPAP compliance (MD −0.34 h, 95% CI −0.72–0.05 h). Hetero-geneity testing showed that I2 = 91%, indicating high heterogeneity (Figure 6). Subgroup analysis of the included studies, grouped by follow-up time (⩾3 months or <3 months) also demonstrated that two groups were not significantly different in long-term follow up (MD −0.56 h, 95% CI −1.39–0.26 h, I2 = 91%), or short-term follow up (MD 0.00 h, 95% CI −0.26–0.27 h, I2 = 14%; Figure 7).
Figure 6.
CPAP compliance (hours of daily use) comparing supervised PAP titration with home auto-adjusting pressure titration in OSA patients.
CPAP, continuous positive airway pressure; OSA, obstructive sleep apnea; PAP, positive airway pressure.
Figure 7.
Subgroup analysis of CPAP compliance (hours of daily use) divided by follow-up time comparing supervised PAP titration with home auto-adjusting pressure titration in OSA patients.
CPAP, continuous positive airway pressure; OSA, obstructive sleep apnea; PAP, positive airway pressure.
In addition, we compared rates of CPAP compliant (>4 h) patients between patients who received SPT and those who received HAPT. The results showed no significant between-group difference in the rate of CPAP compliant patients (OR 0.72, 95% CI 0.48–1.08). Heterogeneity testing revealed I2 = 0%, indicating low heterogeneity (Supplementary Figure 4).
ESS change
Comparing the SPT and HAPT groups for change of ESS, we identified five studies with a total of 635 patients.13–15,24,26 The two groups were not significantly different (MD −0.21, 95% CI −0.68 to 0.26). Heterogeneity testing showed that I2 = 68%, indicating high heterogeneity (Supplementary Figure 5).
FOSQ change
For comparing SPT with HAPT in the change of FOSQ, we included four studies with a total of 592 patients.13–15,26 The results indicated there was a significantly greater change in FOSQ among patients who underwent SPT (MD 0.22, 95% CI 0.07–0.38). Heterogeneity testing revealed I2 = 0%, indicating low heterogeneity (Supplementary Figure 6).
We analyzed potential publication bias of treatment and management methods used for treating patients with OSA. Our results revealed a funnel plot, and the results showed no significant differences (Supplementary Figure 7).
Discussion
Tools for diagnosing and making individualized treatment decisions are needed by practitioners who manage patients with OSA. As the first-line recommended treatment, compliance with CPAP is crucial to improving quality of life and cardiovascular outcomes30; however, the predictors of therapy adherence remain unknown. Consequently, we must enhance CPAP compliance through intervention methods.
Our results provide a comprehensive strategy for improving the management and treatment of patients with OSA. Our results indicate that the TM care group had significantly better CPAP compliance compared with the usual care group. Effective follow up should be considered first in patients with OSA who are treated with CPAP. A study conducted by Mendelson and colleagues showed that TM did not improve blood pressure to reduce the occurrence of cardiovascular events.31 From our point of view, why blood pressure was used as an outcome is unclear. Further, the follow-up time in their study was too short to detect differences in blood pressure changes.
Moreover, in our study, HAPT was non-inferior to SPT in terms of CPAP compliance. Traditionally, when a patient is diagnosed with OSA, they returns to the sleep unit for additional polysomnography to determine the therapeutic CPAP level. Nowadays, home diagnosis and auto-adjusting pressure titration are alternative treatment methods. However, for the purposes of diagnosis, the accuracy of these technologies remains insufficient.32 For pressure-titration, some studies have shown that HAPT produces effects similar to SPT.33–35 Nowadays, auto-adjusting pressure titration is becoming popular in OSA patients, and we believe that simplified OSA diagnosis and treatment methods are more important for patients in rural or remote areas.
In 1997, Weaver and colleagues developed the FOSQ,36 a self-administered tool that quantifies the effects of daytime sleepiness on activities of everyday living.37 In 2009, Chasens and colleagues designed a short and easier-to-use version of the FOSQ based on the original.38 In our study, the change of FOSQ in the TM care group was significantly greater than that detected in the usual care group. Further, the scores increased more in the SPT group than in the HAPT group, which meant that TM care and SPT had better treatment efficacy than the comparators.
The limitations of our study were as follows. First of all, the primary outcome in our study was CPAP compliance, but the follow-up time was different for each included study, leading to high heterogeneity in the results. To address this, in subgroup analysis, we used 3 months as a cut-off to calculate long- and short-term compliance. In addition, although the TM care group had the same definition in every study, which were real-time feedback on compliance and problem solving, most of the included studies used telephone or E-mail to follow-up, but some also used specific advanced devices. Although TM care is more useful in CPAP compliance than usual care, the application of advanced devices depends largely on individual income, and thus is not useful for most patients of lower socioeconomic status. Lastly, HAPT is not a pathway suitable for all patients suffering from OSA. It is limited to cases of apnea hypopnea index (AHI) >30; no obesity hypopnea syndrome (OHS); no central sleep apnea (CSA), cardiac/pulmonary comorbidities; the patient must be able to manage APAP alone for the first night; and not live too far from their nearest treatment center. The guidelines also recommended that APAP should be utilized in OSA patients with no significant comorbidities.39 This study presents a comprehensive clinical pathway for improving CPAP compliance; however, we still have a long way to go.39
Conclusion
To improve CPAP compliance, using TM care is more useful than usual care. In addition, HAPT showed non-inferior efficacy in CPAP compliance than SPT in the sleep unit. Clinicians should consider the use of more effective methods for improving CPAP compliance in patients with OSA.
Supplemental Material
Supplemental material, Supplementary_Data for Telemonitor care helps CPAP compliance in patients with obstructive sleep apnea: a systemic review and meta-analysis of randomized controlled trials by Chongxiang Chen, Jiaojiao Wang, Lanlan Pang, Yanyan Wang, Gang Ma and Wei Liao in Therapeutic Advances in Chronic Disease
Acknowledgments
Authors Chongxiang Chen, Jiaojiao Wang, and Lanlan Pang contributed equally to this work.
We acknowledge all the authors of the contributing studies.
Footnotes
Author contributions: Chongxiang Chen designed the study. Chongxiang Chen designed the search strategy and performed the search. Chongxiang Chen and Lanlan Pang performed abstract screening, full text screening, data extraction, and risk of bias assessment. All the authors drafted the manuscript. Jiaojiao Wang, and Gang Ma helped in the revision process. All authors revised the manuscript, as well as reading and approving the final manuscript.
Funding: The author(s) received no financial support for the research, authorship, and publication of this article.
Conflict of interest statement: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics approval and consent to participate: Not applicable.
Consent for publication: All authors have agreed to the publication of this manuscript.
Availability of data and materials: The datasets used and/or analyzed in the current study are available from the corresponding author upon request.
Data availability: All data generated or analyzed during this study are included in this published article.
ORCID iD: Chongxiang Chen  https://orcid.org/0000-0002-2079-881X
https://orcid.org/0000-0002-2079-881X
Supplemental material: Supplemental material for this article is available online.
Contributor Information
Chongxiang Chen, Guangzhou Institute of Respiratory Diseases, the First Affiliated Hospital of Guangzhou Medical University, State Key Laboratory of Respiratory Disease, Guangzhou, China; Department of Intensive Care Unit, Sun Yat-sen University Cancer Center, State Key Laboratory of Oncology in South China, Collaborative Innovation Center for Cancer Medicine, Guangzhou, China.
Jiaojiao Wang, Department of Tuberculosis, Fuzhou Pulmonary Hospital of Fujian, Fuzhou, Fujian Province, China.
Lanlan Pang, Zhongshan School of Medicine, Sun Yat-sen University, Guangzhou, Guangdong Province, China.
Yanyan Wang, Zhongshan School of Medicine, Sun Yat-sen University, Guangzhou, Guangdong Province, China.
Gang Ma, Department of Intensive Care Unit, Sun Yat-sen University Cancer Center, State Key Laboratory of Oncology in South China, Collaborative Innovation Center for Cancer Medicine, Guangzhou 510060, China.
Wei Liao, Department of Intensive Care Unit, Sun Yat-sen University Cancer Center, State Key Laboratory of Oncology in South China, Collaborative Innovation Center for Cancer Medicine, Dongfeng East Road 651, Guangzhou, 510060, China.
References
- 1. Peppard PE, Young T, Barnet JH, et al. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 2013; 177: 1006–1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Young T, Palta M, Dempsey J, et al. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 1993; 328: 1230–1235. [DOI] [PubMed] [Google Scholar]
- 3. Rotenberg B, George C, Sullivan K, et al. Wait times for sleep apnea care in Ontario: a multidisciplinary assessment. Can Respir J 2010; 17: 170–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Yaggi HK, Concato J, Kernan WN, et al. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med 2005; 353: 2034–2041. [DOI] [PubMed] [Google Scholar]
- 5. Peppard PE, Young T, Palta M, et al. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med 2000; 342: 1378–1384. [DOI] [PubMed] [Google Scholar]
- 6. Patil SP, Ayappa IA, Caples SM, et al. Treatment of adult obstructive sleep apnea with positive airway pressure: an American academy of sleep medicine systematic review, meta-analysis, and GRADE assessment. J Clin Sleep Med 2019; 15: 301–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Likar LL, Panciera TM, Erickson AD, et al. Group education sessions and compliance with nasal CPAP therapy. Chest 1997; 111: 1273–1277. [DOI] [PubMed] [Google Scholar]
- 8. Hoy CJ, Vennelle M, Kingshott RN, et al. Can intensive support improve continuous positive airway pressure use in patients with the sleep apnea/hypopnea syndrome? Am J Respir Crit Care Med 1999; 159: 1096–1100. [DOI] [PubMed] [Google Scholar]
- 9. Hui DS, Chan JK, Choy DK, et al. Effects of augmented continuous positive airway pressure education and support on compliance and outcome in a Chinese population. Chest 2000; 117: 1410–1416. [DOI] [PubMed] [Google Scholar]
- 10. Bakker JP, Wang R, Weng J, et al. Motivational enhancement for increasing adherence to CPAP: a randomized controlled trial. Chest 2016; 150: 337–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Stepnowsky CJ, Palau JJ, Marler MR, et al. Pilot randomized trial of the effect of wireless telemonitoring on compliance and treatment efficacy in obstructive sleep apnea. J Med Internet Res 2007; 9: e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Turino C, de Batlle J, Woehrle H, et al. Management of continuous positive airway pressure treatment compliance using telemonitoring in obstructive sleep apnoea. Eur Respir J 2017; 49: pii: 1601128. [DOI] [PubMed] [Google Scholar]
- 13. Berry RB, Hill G, Thompson L, et al. Portable monitoring and autotitration versus polysomnography for the diagnosis and treatment of sleep apnea. Sleep 2008; 31: 1423–1431. [PMC free article] [PubMed] [Google Scholar]
- 14. Kuna ST, Gurubhagavatula I, Maislin G, et al. Noninferiority of functional outcome in ambulatory management of obstructive sleep apnea. Am J Respir Crit Care Med 2011; 183: 1238–1244. [DOI] [PubMed] [Google Scholar]
- 15. Antic NA, Buchan C, Esterman A, et al. A randomized controlled trial of nurse-led care for symptomatic moderate-severe obstructive sleep apnea. Am J Respir Crit Care Med 2009; 179: 501–508. [DOI] [PubMed] [Google Scholar]
- 16. Anttalainen U, Melkko S, Hakko S, et al. Telemonitoring of CPAP therapy may save nursing time. Sleep Breath 2016; 20: 1209–1215. [DOI] [PubMed] [Google Scholar]
- 17. Fields BG, Behari PP, McCloskey S, et al. Remote ambulatory management of veterans with obstructive sleep apnea. Sleep 2016; 39: 501–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Fox N, Hirsch-Allen AJ, Goodfellow E, et al. The impact of a telemedicine monitoring system on positive airway pressure adherence in patients with obstructive sleep apnea: a randomized controlled trial. Sleep 2012; 35: 477–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Frasnelli M, Baty F, Niedermann J, et al. Effect of telemetric monitoring in the first 30 days of continuous positive airway pressure adaptation for obstructive sleep apnoea syndrome - a controlled pilot study. J Telemed Telecare 2016; 22: 209–214. [DOI] [PubMed] [Google Scholar]
- 20. Hoet F, Libert W, Sanida C, et al. Telemonitoring in continuous positive airway pressure-treated patients improves delay to first intervention and early compliance: a randomized trial. Sleep Med 2017; 39: 77–83. [DOI] [PubMed] [Google Scholar]
- 21. Hwang D, Chang JW, Benjafield AV, et al. Effect of telemedicine education and telemonitoring on continuous positive airway pressure adherence. The tele-OSA randomized trial. Am J Respir Crit Care Med 2018; 197: 117–126. [DOI] [PubMed] [Google Scholar]
- 22. Isetta V, Negrin MA, Monasterio C, et al. A bayesian cost-effectiveness analysis of a telemedicine-based strategy for the management of sleep apnoea: a multicentre randomised controlled trial. Thorax 2015; 70: 1054–1061. [DOI] [PubMed] [Google Scholar]
- 23. Kim RD, Kapur VK, Redline-Bruch J, et al. An economic evaluation of home versus laboratory-based diagnosis of obstructive sleep apnea. Sleep 2015; 38: 1027–1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Mulgrew AT, Fox N, Ayas NT, et al. Diagnosis and initial management of obstructive sleep apnea without polysomnography: a randomized validation study. Ann Intern Med 2007; 146: 157–166. [DOI] [PubMed] [Google Scholar]
- 25. Munafo D, Hevener W, Crocker M, et al. A telehealth program for CPAP adherence reduces labor and yields similar adherence and efficacy when compared to standard of care. Sleep Breath 2016; 20: 777–785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Rosen CL, Auckley D, Benca R, et al. A multisite randomized trial of portable sleep studies and positive airway pressure autotitration versus laboratory-based polysomnography for the diagnosis and treatment of obstructive sleep apnea: the HomePAP study. Sleep 2012; 35: 757–767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Skomro RP, Gjevre J, Reid J, et al. Outcomes of home-based diagnosis and treatment of obstructive sleep apnea. Chest 2010; 138: 257–263. [DOI] [PubMed] [Google Scholar]
- 28. Sparrow D, Aloia M, Demolles DA, et al. A telemedicine intervention to improve adherence to continuous positive airway pressure: a randomised controlled trial. Thorax 2010; 65: 1061–1066. [DOI] [PubMed] [Google Scholar]
- 29. Taylor Y, Eliasson A, Andrada T, et al. The role of telemedicine in CPAP compliance for patients with obstructive sleep apnea syndrome. Sleep Breath 2006; 10: 132–138. [DOI] [PubMed] [Google Scholar]
- 30. Barbe F, Duran-Cantolla J, Sanchez-de-la-Torre M, et al. Effect of continuous positive airway pressure on the incidence of hypertension and cardiovascular events in nonsleepy patients with obstructive sleep apnea: a randomized controlled trial. JAMA 2012; 307: 2161–2168. [DOI] [PubMed] [Google Scholar]
- 31. Mendelson M, Vivodtzev I, Tamisier R, et al. CPAP treatment supported by telemedicine does not improve blood pressure in high cardiovascular risk OSA patients: a randomized, controlled trial. Sleep 2014; 37: 1863–1870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Schechter MS, Section on Pediatric Pulmonology and Subcommittee on Obstructive Sleep Apnea Syndrome. Technical report: diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics 2002; 109: e69. [DOI] [PubMed] [Google Scholar]
- 33. West SD, Jones DR, Stradling JR. Comparison of three ways to determine and deliver pressure during nasal CPAP therapy for obstructive sleep apnoea. Thorax 2006; 61: 226–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Stradling JR, Barbour C, Pitson DJ, et al. Automatic nasal continuous positive airway pressure titration in the laboratory: patient outcomes. Thorax 1997; 52: 72–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Berry RB, Parish JM, Hartse KM. The use of auto-titrating continuous positive airway pressure for treatment of adult obstructive sleep apnea. An American academy of sleep medicine review. Sleep 2002; 25: 148–173. [PubMed] [Google Scholar]
- 36. Weaver TE, Laizner AM, Evans LK, et al. An instrument to measure functional status outcomes for disorders of excessive sleepiness. Sleep 1997; 20: 835–843. [PubMed] [Google Scholar]
- 37. Rey de Castro J, Rosales-Mayor E, Weaver TE. Reliability and validity of the functional outcomes of sleep questionnaire - Spanish short version (FOSQ-10SV) in Peruvian patients with obstructive sleep apnea. J Clin Sleep Med 2018; 14: 615–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Chasens ER, Ratcliffe SJ, Weaver TE. Development of the FOSQ-10: a short version of the functional outcomes of sleep questionnaire. Sleep 2009; 32: 915–919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Patil SP, Ayappa IA, Caples SM, et al. Treatment of adult obstructive sleep apnea with positive airway pressure: an american academy of sleep medicine clinical practice guideline. J Clin Sleep Med 2019; 15: 335–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplementary_Data for Telemonitor care helps CPAP compliance in patients with obstructive sleep apnea: a systemic review and meta-analysis of randomized controlled trials by Chongxiang Chen, Jiaojiao Wang, Lanlan Pang, Yanyan Wang, Gang Ma and Wei Liao in Therapeutic Advances in Chronic Disease