Abstract
Much of the world's prominent and burdensome chronic diseases, such as diabetes, Alzheimer's, and heart disease, are caused by impaired metabolism. By acting as both an efficient fuel and a powerful signalling molecule, the natural ketone body, d-β-hydroxybutyrate (βHB), may help circumvent the metabolic malfunctions that aggravate some diseases. Historically, dietary interventions that elevate βHB production by the liver, such as high-fat diets and partial starvation, have been used to treat chronic disease with varying degrees of success, owing to the potential downsides of such diets. The recent development of an ingestible βHB monoester provides a new tool to quickly and accurately raise blood ketone concentration, opening a myriad of potential health applications. The βHB monoester is a salt-free βHB precursor that yields only the biologically active d-isoform of the metabolite, the pharmacokinetics of which have been studied, as has safety for human consumption in athletes and healthy volunteers. This review describes fundamental concepts of endogenous and exogenous ketone body metabolism, the differences between the βHB monoester and other exogenous ketones and summarises the disease-specific biochemical and physiological rationales behind its clinical use in diabetes, neurodegenerative diseases, heart failure, sepsis related muscle atrophy, migraine, and epilepsy. We also address the limitations of using the βHB monoester as an adjunctive nutritional therapy and areas of uncertainty that could guide future research.
Keywords: ketone bodies, Ketone monoester, ketosis
Introduction
The human brain consumes between 100 and 120 grams of glucose daily. As 1.75 grams of muscle protein must be broken down to produce 1 gram of glucose, lean tissue mass would quickly atrophy in order to feed the glucose-deprived brain in early starvation [1], should no other adaptation take place. To decrease muscle atrophy, fuel the brain and allay rapid death in starvation, d-β-hydroxybutyrate and acetoacetate are produced from our plentiful fat stores in a process named, ketogenesis [2].
Physiological effects of ketone bodies
Having a higher H:C ratio than pyruvate (2 vs. 1.3), ketone bodies are more reduced, so can yield more free energy per mol of oxygen to fuel ATP production [3] and produce fewer reactive oxygen species (ROS) than glucose and fatty acids [4]. More than an efficient fuel, ketones regulate their own production by inhibiting lipolysis, spare glycogen and direct fuel oxidation in different tissues [5]. βHB acts as a signalling molecule in different tissues to co-ordinate a survival response during starvation; it increases histone acetylation, inducing the expression of genes that suppress oxidative stress [6], diminishes inflammation by blocking the NLRP3 inflammasome [7] and reduces sympathetic nervous system activity and total energy expenditure by inhibiting short-chain fatty acid signalling through GPR41 [8]. Finally, the βHB molecule is a histone modifier and directly regulates gene expression [9].
Production of ketone bodies
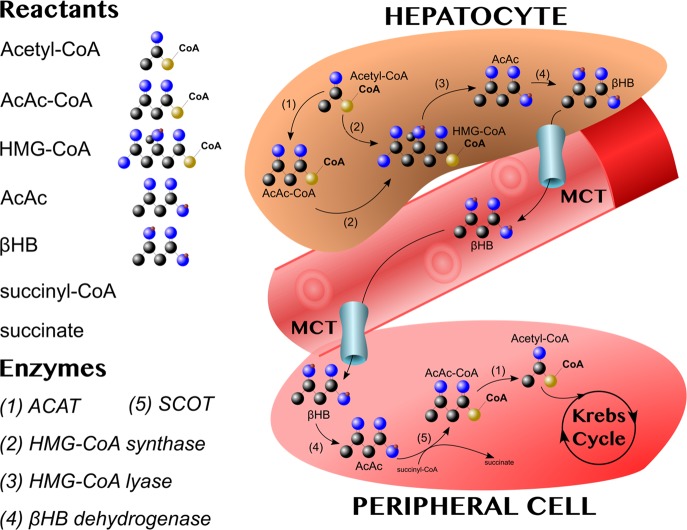
In fasting, the combination of low insulin with high cortisol and glucagon stimulates adipocytes to release non-esterified fatty acids into the bloodstream. Fatty acids are taken up by hepatocytes, which is where ketogenesis takes place [10]. Acetyl-coenzyme A acetyltransferases (ACAT) are ubiquitous enzymes that catalyse the formation of acetoacetyl-CoA (AcAc-CoA) from two molecules of acetyl-CoA, and vice versa (Figure 1). AcAc-CoA is converted to 3-hydroxymethylglutaryl-CoA (HMG-CoA) by HMG-CoA synthase. HMG-CoA lyase then cleaves HMG-CoA, releasing acetyl-CoA and the ketone body, acetoacetate (AcAc) [5]. From this point, AcAc can have one of three fates: enter the bloodstream through the monocarboxylate transporters (MCT) 1–4 [11], spontaneously decarboxylate into CO2 and acetone (both fat-soluble molecules that will diffuse out of hepatocytes and exit the body through ventilation), or be reduced by βHB dehydrogenase into βHB, which exits through the MCT [12].
Figure 1. In hepatocytes, acetyl-coenzyme A acetyltransferase (ACAT: 1) combines two acetyl-CoA molecules into acetoacetyl-CoA (AcAc-CoA).
AcAc-CoA is combined with another acetyl-CoA by HMG-CoA synthase (2) to form 3-hydroxymethylglutaryl-CoA (HMG-CoA). HMG-CoA lyase (3) cleaves HMG-CoA, releasing acetyl-CoA and the ketone body, acetoacetate (AcAc). AcAc can then be reduced to βHB by βHB dehydrogenase (4). βHB, the main transport ketone, exits hepatocytes via monocarboxylate transporters (MCT) and travels through the circulation to peripheral tissues. Once there, βHB is oxidised back into AcAc by βHB dehydrogenase (4). In the rate-limiting step of ketolysis, succinyl-CoA-3-oxaloacid CoA transferase (SCOT) (5) converts AcAc and succinyl-CoA into AcAc-CoA and succinate. AcAc-CoA is then cleaved by ACAT (1) to yield two molecules of acetyl-CoA that can enter the Krebs cycle.
Oxidation of ketone bodies
At target tissues, βHB is oxidised into AcAc in the reverse reaction catalysed by βHB dehydrogenase. Next, in the rate-limiting step of ketolysis, succinyl-CoA-3-oxaloacid CoA transferase (SCOT) converts AcAc and succinyl-CoA into AcAc-CoA and succinate. AcAc-CoA is then cleaved by ACAT to yield two molecules of Acetyl-CoA that can enter the Krebs cycle. As an economic survival adaptation, hepatocytes do not express the rate-limiting enzyme, SCOT, and are thus incapable of metabolising the ketone bodies they produce [13]. Also, in contrast with the conversion of glucose to pyruvate through glycolysis, the metabolism of ketone bodies does not require the use of ATP [4]. The reactions involved in the production and oxidation of ketone bodies are illustrated in Figure 1.
Excretion of ketone bodies
Both AcAc and βHB are excreted by the kidneys and, notably, their reabsorption is increased in extended starvation. Importantly, although ketones are indeed acidic, acid-base disturbances in diabetic ketoacidosis are not caused by ketone body accumulation (in fact, their excretion is increased), but by volume contraction and changes in bicarbonate and electrolyte concentrations [14,15].
Regulation of the production and oxidation of ketone bodies
Ketogenesis occurs in response to metabolic demand for oxidative fuel when carbohydrate stores are low, a state communicated to adipocytes as a low insulin, high cortisol, high glucagon state. βHB also auto-regulates its own production by inhibiting lipolysis via PUMA-G nicotinic receptors on adipocytes [16] and decreasing free-fatty acid availability for ketogenesis. Within hepatocytes, ketogenic rates are fine-tuned, not only by fatty acid flux and concentrations of acetyl-CoA, but also by deacetylating mitochondrial 3-hydroxy-3-methylglutaryl CoA synthase 2, a rate-limiting enzyme in ketogenesis, via SIRT3 [17].
It is worth noticing that the conversion of AcAc into βHB, or vice versa, occurs in an NAD+/NADH-coupled near-equilibrium reaction and that the ratio of AcAc/βHB is proportional to the mitochondrial NAD+/NADH ratio. In other words, the activity of βHB dehydrogenase modulates the mitochondrial redox potential and ensures ketone bodies are terminally oxidised in proportion to the cellular ATP demand [18]. Furthermore, because the MCT are H+-coupled transporters, the NAD+/NADH ratio in the target tissues influences cellular uptake and oxidation proportionally to their energetic needs [11].
The βHB monoester compared with other ketogenic interventions
As previously described, the production of ketone bodies is a dynamic process with multiple inputs and regulatory points. Therefore, is not possible to accurately set blood βHB concentrations with the interventions that rely on endogenous ketosis. The advent of exogenous sources of ketone bodies, such as the salts and esters, has enabled the accurate manipulation of ketone body blood concentration and introduced an entirely new metabolic state: exogenous ketosis [19]. However, achieving a fasting-like concentration of blood βHB with ketone salts would require the consumption of many grams of salt. Additionally, most salts are racemic, with 50% the bioactive d-form of βHB and 50% the l-form of βHB [20], which is not normally found in blood. Using doses between 357 and 714 mg/kg, the βHB monoester allows the safe and accurate attainment of blood concentrations of βHB similar to those observed after several days of fasting, but within 30 min [21]. Moreover, it delivers only the d-form of βHB and is salt-free.
A notable ‘middle point' between endogenous and exogenous ketogenic interventions is the consumption of medium-chain triglycerides (MCTS) [22]. After ingestion, MCTS are rapidly taken up in the portal system and converted into ketone bodies in hepatocytes. Simply, they are an exogenous ketogenic precursor converted into ketones by normal endogenous means. While they indeed acutely raise βHB blood concentration, they do so moderately and do not permit the accurate titration of βHB concentration. One thing MCTS and exogenous ketones have in common is that their consumption may induce gastrointestinal discomfort. However, the frequency and severity of these symptoms are dose- and compound-specific [23]. Table 1 summarises the differences between available ketogenic interventions.
Table 1. Endogenous and exogenous sources of the ketone bodies, d-β-hydroxybutyrate and acetoacetate, their ratios, the maximum blood βHB concentrations that can be reached, plus the insulin and glucose concentrations observed in their presence [1,19,22].
| Fasting | Ketogenic diet MCTS | Ketone salts | βHB monoester | |
|---|---|---|---|---|
| Ketone source | Liver | Liver | Salt form of βHB | (R)-3-hydroxybutyl (R)-3-hydroxybutyrate |
| βHB:AcAc | 5 : 1 | 3 : 1 | 3 : 1 | 5 : 1 |
| Blood βHB (mM) | 6–7 | 1–4 | 1–2 | 3–6 |
| Insulin | Low | Low | Normal | Normal |
| Blood glucose | Low | Low | Low-Normal | Low-Normal |
The metabolism of the βHB monoester
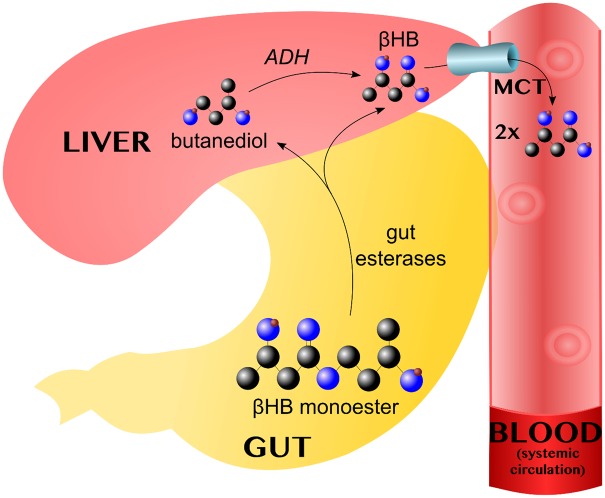
After ingestion, the βHB monoester bond is cleaved by esterases in the gut wall, yielding βHB and butanediol in equal amounts. Both are absorbed into the portal circulation and the latter is taken up by the liver, where it is converted into βHB by alcohol dehydrogenase (ADH). βHB leaves the hepatocytes via the MCT. Pharmacokinetic studies have shown that, in the fasted and resting states, the βHB monoester can induce ketoses for 3–4 h, with a peak at ∼1 h that is dose-dependent [21]. The metabolism of the βHB monoester is summarised in Figure 2.
Figure 2. The βHB monoester bond is cleaved by gut esterases, yielding βHB and butanediol, which enter the portal circulation.
In the liver, alcohol dehydrogenase (ADH) converts butanediol converted into βHB, which leaves via the monocarboxylate transporters (MCT). Each monoester molecule thus yields two βHB equivalents.
The potential applications of induced ketosis
To date, most of the studies involving the βHB monoester in humans have focused on exercise in athletes, but the rationale behind this approach is outside the scope of this review [24]. Although ketogenic diets and intermittent fasting strategies for metabolic health have regained popularity in the last few years [25], research on the mechanisms behind their benefits is scarce and/or difficult to interpret because the interventions result in many physiological changes and because of the inherent limitations of animal models and diet studies [26]. In this context, the βHB monoester offers the possibility of consistently, accurately, and singularly inducing high βHB blood concentrations in humans to allow the determination of results due to ketosis itself.
Arguably, the most exciting applications of the βHB monoester are therapeutic because many diseases are caused or exacerbated by energy deficits or abnormal metabolic regulation, thus inducing ketosis may be beneficial [4]. In the following section, we summarise the biochemical and physiological rationale behind the βHB monoester's use in specific diseases.
Refractory epilepsy
Ketogenic diets have been used as a treatment for epilepsy for centuries [27]. Although the benefits are clear [28], the diets are far from ideal because they have been associated with an increased risk of nephrolithiasis [29], stunted growth (due to the low insulin concentration) and poor compliance, the diets proving difficult for many patients and their parents [30].
There is still some debate on whether the mechanism for the ketogenic diet effect is due to the elevated ketone bodies themselves. Mouse studies have suggested that changes in fat metabolism and/or the composition of the microbiome may underly the benefits [31]. On the other hand, there is compelling evidence supporting the utilisation of ketone supplements in other neuro-excitability related illnesses, such as schizophrenia [32] and migraine [33] by modifying local neurotransmitter systems and reducing local inflammation. To our knowledge, there haven't been yet long-term studies using any form of exogenous ketones as an adjuvant treatment for refractory epilepsy.
Neurodegenerative diseases
Neurodegenerative diseases are multifactorial with complex underlying pathophysiological mechanisms. Not surprisingly, therefore, the standard monotherapeutic drug approach to conditions such as Alzheimer's and Parkinson's diseases has consistently failed to produce therapeutic or preventative treatments.
By addressing several of the key pathological mechanisms underlying neurodegenerative diseases simultaneously, ketogenic nutrition, including using a βHB monoester drink, could slow or halt the progression of conditions such as Alzheimer's and Parkinson's diseases. A more comprehensive and detailed review can be found elsewhere [34]; however, we will briefly, summarise some of the most relevant mechanisms here:
First, neurodegenerative diseases are marked by defects in mitochondrial metabolism, such as decreased ATP production, increase ROS production, complex IV dysfunction in Alzheimer's disease and complex I dysfunction in Parkinson's disease [35–38]. Ketones may improve mitochondrial metabolism via a number of mechanisms, including, but not limited to, improving the health of the mitochondrial pool by inducing mitochondrial turnover (inducing mitophagy and PGC-1α) in combination with reducing oxidative stress (decreasing ROS production and increasing antioxidant defences) and damage to mitochondrial DNA and proteins, as well as by simply serving as an alternative energy substrate where glucose metabolism is impaired [39–41].
Second, neurodegenerative diseases almost universally feature neuroinflammation. By inhibiting pathologic microglial activation [42] and key regulators in inflammation pathways, such as the NLRP3 inflammasome [7], a βHB monoester could also protect against neuroinflammation.
Third, ketones can protect against the toxicity of neurotoxins, such as Aβ oligomers and MPP+ in models of Alzheimer's and Parkinson's, respectively [43].
It is unlikely that a single intervention (either drug, diet or ketone supplement) can alone salvage or repair a severely diseased brain. However, by combining interventions, along with other lifestyle changes (sleep, exercise, stress reduction, etc.), it may be possible to develop a multifaceted approach to effectively treat these debilitating diseases. A study involving a monthly intervention of the βHB monoester in people living with Parkinson's disease is currently in progress [44].
Heart failure
Today, cardiovascular disease is the most frequent cause of death [45]. Ketone oxidation improved hydraulic efficiency and ATP production in the working rat heart [3] and ketone body oxidation is increased in heart failure [46]; however, patients with heart failure rarely have a high enough βHB blood concentration to properly fuel their cardiac demands. A recent study in heart failure patients reported an acute 40% improvement in cardiac output and 8% improvement of left ventricular ejection fraction after infusion of βHB salts [47], yet salt consumption causes fluid retention and current therapeutic guidelines recommend a daily salt intake of less than 2 grams [48]. Consequently, a salt-based ketogenic supplement would be an unfeasible treatment for chronic heart failure. It is also worth mentioning that most current treatments for chronic heart failure are aimed at slowing its progression. Inotropic drugs, such as digoxin or levosimendan, are only prescribed in late stages of the disease or during acute exacerbations, respectively [48]. Therefore, any intervention that ameliorates a diminished cardiac output and can be consumed chronically could be highly desirable.
Diabetes
In recent years, ketogenic diets have yielded positive results, to the point of reversing type 2 diabetes in 54% of patients in one 2-year study [49]. However, it is unclear if the benefit arose from a reduced glucose load or a ketone specific mechanism. It is an undisputed fact that, regardless of the animal model and regardless of the ketogenic intervention, acute ketosis lowers blood glucose within a few minutes [20,50,51]. There is evidence suggesting ketosis acutely reduces the glycaemic response to a glucose challenge [52], and improves insulin secretion [50] however, ketone infusions lower blood glucose concentration even in the absence of insulin [53] and there is current research looking into the effect of acute ketosis substrate availability for gluconeogenesis [54]. On the other hand, diabetes treatment involves many non-glucose related goals [55] and dyslipidaemia is one of the hallmarks of this disease. Additionally, most diabetes patients die from cardiovascular-related complications [56]. Therefore, the already described effects in cardiac output, and the added fact that acute ketosis also reduces free fatty acids [16,20], could prove beneficial for these patients. A study involving a monthly intervention with the βHB monoester in people living with type 2 diabetes is in progress [57].
Sepsis related muscle atrophy
Arguably, ketone metabolism evolved to prevent muscle atrophy during prolonged catabolism [58] and the idea that inducing sustained ketosis in sepsis patients could ameliorate it has been around for at least three decades [59]. Sepsis is a hypercatabolic state usually worsened by undernutrition [60], and characterised by severe systemic inflammation [61]. On the other hand, ketone bodies themselves are a source of calories [62], βHB inhibits lipolysis via the PUMA-G receptor [16], reduces total energy expenditure by inhibiting short-chain fatty acid signalling through GPR41 [8] and most importantly, diminishes inflammation by blocking the NLRP3 inflammasome [7]. Enticing the idea of a similar outcome in sepsis patients, research on another hypercatabolic state: exercise [63], suggest ketone oxidation preserves glycogen, branched-chained amino acids, and total muscle mass [64]. Additionally, hyperglycaemia, is one of the most prominent hallmarks of sepsis [61] and is associated with mortality. By the same mechanisms already described, inducing ketosis could also help improve glucose control in sepsis patients. Despite this, the lack of safe exogenous precursors and significant gaps in our knowledge about its safety in this population have prevented further research. To our knowledge, the only study that has directly looked into it, involved a four-hour ketone salt infusion and showed improvements in glucose and fat metabolism but, understandably, was not long enough to show protein catabolism benefits [65]. Having the most thoroughly studied safety profile so far ketone supplement so far, the βHB monoester offers an opportunity to advance research on novel nutritional strategies for this critical condition.
Conclusion
The βHB monoester is a promising treatment for of numerous diseases. However, more research is needed to describe its safety for specific patient populations, to assess the magnitude of its clinical benefits, and to increase our understanding about the underlying mechanisms behind its therapeutic effects. Additionally, allowing the quick and accurate manipulation of βHB concentration in the blood, it is a useful tool for ketone metabolism research.
Perspectives
Since most pathologies are induced or aggravated by energy deficits or abnormal metabolic regulation, the induction of ketosis may be broadly beneficial. However, safety and accurately increasing blood βHB concentration is difficult with most ketogenic interventions, the exception being the βHB monoester.
Importance: Yielding only the d-isoform of βHB and being salt-free, the βHB monoester is a promising ketotherapeutic. Additionally, its pharmacological profile has been thoroughly studied.
Current thinking: The safety and tolerability of consuming the βHB monoester, three times per day for one month, has been demonstrated in healthy volunteers [66]; however, further disease-specific safety and tolerability studies are warranted. Safety and efficacy studies in type 2 diabetes mellitus [57] and Parkinson's disease [44] patients are in progress.
Future directions: As discussed, among the most exciting clinical applications of the βHB monoester are chronic diseases. However, due to its half-life, these applications would require patients to consume drinks frequently in order to sustain a fasting-like blood βHB concentration for a prolonged time. Additionally, the current price of chronically sustaining exogenous ketosis with the βHB monoester would impose an enormous financial burden for most patients and health systems. More research is needed to assess disease-specific cost-benefit ratios. Finally, despite the good tolerability reported in some studies, the bitter taste may impair adherence, particularly in children, the elderly and the critically ill.
Acknowledgements
The authors thank Vicky Ball for her diligent support. Dr Adrian Soto Mota thanks the Consejo Nacional de Ciencia y Tecnología (CONACYT, Mexico) and the Fundación para la Salud y Educación Dr Salvador Zubirán (FUNSAED, Mexico) for their financial support.
Abbreviations
- AcAc
Acetoacetate
- AcAc-CoA
Acetoacetyl-CoA
- ACAT
Acetyl-coenzyme A acetyltransferases
- ADH
alcohol dehydrogenase
- ATP
Adenosine triphosphate
- MCT
Monocarboxylate transporters
- MCTS
Medium chain triglycerides
- NAD
Nicotinamide adenine dinucleotide
- NADH
Nicotinamide adenine dinucleotide + hydrogen (H)
- ROS
Reactive oxygen species
- SCOT
Succinyl-CoA-3-oxaloacid CoA transferase
- βHB
d-β-hydroxybutyrate
Author Contribution
All authors contributed significantly to the elaboration of this review.
Open Access
Open access for this article was enabled by the participation of University of Oxford in an all-inclusive Read & Publish pilot with Portland Press and the Biochemical Society under a transformative agreement with JISC.
Competing Interests
The intellectual property covering the uses of ketone bodies and ketone esters are owned by BTG Plc, Oxford University Innovation Ltd and the US National Institutes of Health. Professor Kieran Clarke, as an inventor, will receive a share of the royalties under the terms prescribed by each institution. Professor Clarke is a director of TdeltaS Ltd, a company spun out of the University of Oxford to develop products based on the science of ketone bodies in human nutrition. The other authors declare that they have no competing financial interests or personal relationships that could have influenced the work reported in this paper.
References
- 1.Cahill G.F. (2006) Fuel metabolism in starvation. Annu. Rev. Nutr. 26, 1–22 10.1146/annurev.nutr.26.061505.111258 [DOI] [PubMed] [Google Scholar]
- 2.Balasse E.O. (1979) Kinetics of ketone body metabolism in fasting humans. Metab. Clin. Exp. 28, 41–50 10.1016/0026-0495(79)90166-5 [DOI] [PubMed] [Google Scholar]
- 3.Sato K., Kashiwaya Y., Keon C.A., Tsuchiya N., King M.T., Radda G.K. et al. (1995) Insulin, ketone bodies, and mitochondrial energy transduction. FASEB J. 9, 651–658 10.1096/fasebj.9.8.7768357 [DOI] [PubMed] [Google Scholar]
- 4.Veech R.L. (2004) The therapeutic implications of ketone bodies: the effects of ketone bodies in pathological conditions: ketosis, ketogenic diet, redox states, insulin resistance, and mitochondrial metabolism. Prostaglandins Leukot. Essent. Fatty Acids 70, 309–319 10.1016/j.plefa.2003.09.007 [DOI] [PubMed] [Google Scholar]
- 5.Newman J.C. and Verdin E. (2014) β-hydroxybutyrate: much more than a metabolite. Diabetes Res. Clin. Pract. 106, 173–181 10.1016/j.diabres.2014.08.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shimazu T., Hirschey M.D., Newman J., He W., Shirakawa K., Le Moan N. et al. (2013) Suppression of oxidative stress by β-hydroxybutyrate, an endogenous histone deacetylase inhibitor. Science 339, 211–214 10.1126/science.1227166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Youm Y.H., Nguyen K.Y., Grant R.W., Goldberg E.L., Bodogai M., Kim D. et al. (2015) The ketone metabolite β-hydroxybutyrate blocks NLRP3 inflammasome-mediated inflammatory disease. Nat. Med. 21, 263–269 10.1038/nm.3804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kimura I., Inoue D., Maeda T., Hara T., Ichimura A., Miyauchi S. et al. (2011) Short-chain fatty acids and ketones directly regulate sympathetic nervous system via G protein-coupled receptor 41 (GPR41). Proc. Natl Acad. Sci. U.S.A. 108, 8030–8035 10.1073/pnas.1016088108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xie Z., Zhang D., Chung D., Tang Z., Huang H., Dai L. et al. (2016) Metabolic regulation of gene expression by histone lysine β-hydroxybutyrylation. Mol. Cell 62, 194–206 10.1016/j.molcel.2016.03.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cahill G.F., Herrera M.G., Morgan A.P., Soeldner J.S., Steinke J., Levy P.L. et al. (1966) Hormone-fuel interrelationships during fasting. J. Clin. Invest. 45, 1751–1769 10.1172/JCI105481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Halestrap A.P. (2013) The SLC16 gene family—Structure, role and regulation in health and disease. Mol. Aspects Med. 34, 337–349 10.1016/j.mam.2012.05.003 [DOI] [PubMed] [Google Scholar]
- 12.Puchalska P. and Crawford P.A. (2017) Multi-dimensional roles of ketone bodies in fuel metabolism, signaling, and therapeutics. Cell Metab. 25, 262–284 10.1016/j.cmet.2016.12.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Orii K.E., Fukao T., Song X.-Q., Mitchell G.A. and Kondo N. (2008) Liver-specific silencing of the human gene encoding succinyl-CoA: 3-ketoacid CoA transferase. Tohoku J. Exp. Med. 215, 227–236 10.1620/tjem.215.227 [DOI] [PubMed] [Google Scholar]
- 14.Balasse E.O. and Féry F. (1989) Ketone body production and disposal: effects of fasting, diabetes, and exercise. Diabetes Metab. Rev. 5, 247–270 10.1002/dmr.5610050304 [DOI] [PubMed] [Google Scholar]
- 15.Green A. and Bishop R.E. (2019) Ketoacidosis—Where do the protons come from? Trends Biochem. Sci. 44, 484–489 10.1016/j.tibs.2019.01.005 [DOI] [PubMed] [Google Scholar]
- 16.Taggart A.K.P.P., Kero J., Gan X., Cai T.-Q.Q., Cheng K., Ippolito M. et al. (2005) (D)-β-hydroxybutyrate inhibits adipocyte lipolysis via the nicotinic acid receptor PUMA-G. J. Biol. Chem. 280, 26649–26652 10.1074/jbc.C500213200 [DOI] [PubMed] [Google Scholar]
- 17.Shimazu T., Hirschey M.D., Hua L., Dittenhafer-Reed K.E., Schwer B., Lombard D.B. et al. (2010) SIRT3 deacetylates mitochondrial 3-hydroxy-3-methylglutaryl CoA synthase 2 and regulates ketone body production. Cell Metab. 12, 654–661 10.1016/j.cmet.2010.11.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Krebs H.A., Wallace P.G., Hems R. and Freedland R.A. (1969) Rates of ketone-body formation in the perfused rat liver. Biochem. J. 112, 595–600 10.1042/bj1120595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Newport M.T., VanItallie T.B., Kashiwaya Y., King M.T. and Veech R.L. (2015) A new way to produce hyperketonemia: use of ketone ester in a case of Alzheimer's disease. Alzheimer's Dement. 11, 99–103 10.1016/j.jalz.2014.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stubbs B.J., Cox P.J., Evans R.D., Santer P., Miller J.J., Faull O.K. et al. (2017) On the metabolism of exogenous ketones in humans. Front. Physiol. 8, 848 10.3389/fphys.2017.00848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Clarke K., Tchabanenko K., Pawlosky R., Carter E., Todd King M., Musa-Veloso K. et al. (2012) Kinetics, safety and tolerability of (R)-3-hydroxybutyl (R)-3-hydroxybutyrate in healthy adult subjects. Regul. Toxicol. Pharmacol. 63, 401–408 10.1016/j.yrtph.2012.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kesl S.L., Poff A.M., Ward N.P., Fiorelli T.N., Ari C., Van Putten A.J. et al. (2016) Effects of exogenous ketone supplementation on blood ketone, glucose, triglyceride, and lipoprotein levels in sprague–Dawley rats. Nutr. Metab. (Lond) 13, 1–15 10.1186/s12986-016-0061-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stubbs B.J., Cox P.J., Kirk T., Evans R.D. and Clarke K. (2019) Gastrointestinal effects of exogenous ketone drinks are infrequent, mild and vary according to ketone compound and dose. Int. J. Sport Nutr. Exerc. Metab. 29, 596–603 10.1123/ijsnem.2019-0014 [DOI] [PubMed] [Google Scholar]
- 24.Dearlove D.J., Faull O.K. and Clarke K. (2019) Context is key: exogenous ketosis and athletic performance. Curr. Opin. Physiol. 10, 81–89 10.1016/j.cophys.2019.04.010 [DOI] [Google Scholar]
- 25.Abbasi J. (2018) Interest in the ketogenic diet grows forweight loss and type 2 diabetes. JAMA 319, 215–217 10.1001/jama.2017.20639 [DOI] [PubMed] [Google Scholar]
- 26.Joshi S., Ostfeld R.J. and McMacken M. (2019) The ketogenic diet for obesity and diabetes—Enthusiasm outpaces evidence. JAMA Intern. Med. 179, 1163–1164 10.1001/jamainternmed.2019.2633 [DOI] [PubMed] [Google Scholar]
- 27.Gano L.B., Patel M. and Rho J.M. (2014) Ketogenic diets, mitochondria, and neurological diseases. J. Lipid Res. 55, 2211–2228 10.1194/jlr.R048975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Martin-Mcgill K.J., Jackson C.F., Bresnahan R., Levy R.G. and Cooper P.N. (2018) Ketogenic diets for drug-resistant epilepsy. Cochrane Database Syst. Rev. 11, CD001903 10.1002/14651858.CD001903.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kielb S., Koo H.P., Bloom D.A. and Faerber G.J. (2000) Nephrolithiasis associated with the ketogenic diet. J. Urol. 164, 464–466 10.1016/S0022-5347(05)67400-9 [DOI] [PubMed] [Google Scholar]
- 30.Groleau V., Schall J.I., Stallings V.A. and Bergqvist C.A. (2014) Long-term impact of the ketogenic diet on growth and resting energy expenditure in children with intractable epilepsy. Dev. Med. Child Neurol. 56, 898–904 10.1111/dmcn.12462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.D'Andrea Meira I., Romão T.T., Pires do Prado H.J., Krüger L.T., Pires M.E.P. and da Conceição P.O. (2019) Ketogenic diet and epilepsy: what we know so far. Front. Neurosci. 13, 5 10.3389/fnins.2019.00005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kovács Z., D'Agostino D.P., Diamond D., Kindy M.S., Rogers C. and Ari C. (2019) Therapeutic potential of exogenous ketone supplement induced ketosis in the treatment of psychiatric disorders: review of current literature. Front. Psychiatry 10, 363 10.3389/fpsyt.2019.00363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gross E.C., Lisicki M., Fischer D., Sándor P.S. and Schoenen J. (2019) The metabolic face of migraine—from pathophysiology to treatment. Nat. Rev. Neurol. 15, 627–643 10.1038/s41582-019-0255-4 [DOI] [PubMed] [Google Scholar]
- 34.Norwitz N.G., Hu M.T. and Clarke K. (2019) The mechanisms by which the ketone body d-β-hydroxybutyrate may improve the multiple cellular pathologies of Parkinson's disease. Front. Nutr. 6, 63 10.3389/fnut.2019.00063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhang C., Rissman R.A. and Feng J. (2015) Characterization of ATP alternations in an Alzheimer's disease transgenic mouse model. J. Alzheimer's Dis. 44, 375–378 10.3233/JAD-141890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Greenamyre J.T., Sherer T.B., Betarbet R. and Panov A V. (2001) Complex I and Parkinson's disease. IUBMB Life 52, 135–141 10.1080/15216540152845939 [DOI] [PubMed] [Google Scholar]
- 37.Mosconi L., de Leon M., Murray J E.L., Lu J., Javier E. et al. (2011) Reduced mitochondria cytochrome oxidase activity in adult children of mothers with Alzheimer's disease. J. Alzheimer's Dis. 27, 483–490 10.3233/JAD-2011-110866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kim G.H., Kim J.E., Rhie S.J. and Yoon S. (2015) The role of oxidative stress in neurodegenerative diseases. Exp. Neurobiol. 24, 325 10.5607/en.2015.24.4.325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fortier M., Castellano C.-A., Croteau E., Langlois F., Bocti C., St-Pierre V. et al. (2019) A ketogenic drink improves brain energy and some measures of cognition in mild cognitive impairment. Alzheimer's Dement. 15, 625–634 10.1016/j.jalz.2018.12.017 [DOI] [PubMed] [Google Scholar]
- 40.Srivastava S., Baxa U., Niu G., Chen X. and Veech R.L. (2013) A ketogenic diet increases brown adipose tissue mitochondrial proteins and UCP1 levels in mice. IUBMB Life 65, 58–66 10.1002/iub.1102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kashiwaya Y., Pawlosky R., Markis W., King M.T., Bergman C., Srivastava S. et al. (2010) A ketone ester diet increases brain malonyl-CoA and uncoupling proteins 4 and 5 while decreasing food intake in the normal wistar rat. J. Biol. Chem. 285, 25950–25956 10.1074/jbc.M110.138198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Xu X., Zhang Q., Tu J. and Ren Z. (2011) d-β-hydroxybutyrate inhibits microglial activation in a cell activation model in vitro. J. Med. Coll. PLA 26, 117–127 10.1016/S1000-1948(11)60042-7 [DOI] [Google Scholar]
- 43.Kashiwaya Y., Takeshima T., Mori N., Nakashima K., Clarke K. and Veech R.L. (2000) d-β-hydroxybutyrate protects neurons in models of Alzheimer's and Parkinson's disease. Proc. Natl Acad. Sci. U.S.A. 97, 5440–5444 10.1073/pnas.97.10.5440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.ISRCTN - ISRCTN64294760: Can a ketone drink reduce the severity of symptoms of Parkinson's disease? [Internet]. Available from: https://www.isrctn.com/ISRCTN64294760?q=&filters=conditionCategory:Nervous System Diseases,ageRange:Mixed&sort=&offset=2&totalResults=17&page=1&pageSize=10&searchType = basic-search
- 45.Miranda J.J., Barrientos-Gutiérrez T., Corvalan C., Hyder A.A., Lazo-Porras M., Oni T. et al. (2019) Understanding the rise of cardiometabolic diseases in low- and middle-income countries. Nat. Med. 25, 1667–1679 10.1038/s41591-019-0644-7 [DOI] [PubMed] [Google Scholar]
- 46.Aubert G., Martin O.J., Horton J.L., Lai L., Vega R.B., Leone T.C. et al. (2016) The failing heart relies on ketone bodies as a fuel. Circulation 133, 698–705 10.1161/CIRCULATIONAHA.115.017355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nielsen R., Møller N., Gormsen L.C., Tolbod L.P., Hansson N.H., Sorensen J. et al. (2019) Cardiovascular effects of treatment with the ketone body 3-hydroxybutyrate in chronic heart failure patients. Circulation 139, 2129–2141 10.1161/CIRCULATIONAHA.118.036459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.McMurray J.J.V., Adamopoulos S., Anker S.D., Auricchio A., Böhm M., Dickstein K. et al. (2012) ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The task force for the diagnosis and treatment of acute and chronic heart failure 2012 of the european society of cardiology. developed in collaboration with the heart failure association (HFA) of the ESC. Eur. Heart J. 33, 1787–1847 10.1093/eurheartj/ehs104 [DOI] [PubMed] [Google Scholar]
- 49.Lim E.L., Hollingsworth K.G., Aribisala B.S., Chen M.J., Mathers J.C. and Taylor R. (2011) Reversal of type 2 diabetes: Normalisation of beta cell function in association with decreased pancreas and liver triacylglycerol. Diabetologia 54, 2506–2514 10.1007/s00125-011-2204-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Muller M.J., Paschen U. and Seitz H.J. (1984) Effect of ketone bodies on glucose production and utilization in the miniature pig. J. Clin. Invest. 74, 249–261 10.1172/JCI111408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ari C., Murdun C., Koutnik A.P., Goldhagen C.R., Rogers C., Park C. et al. (2019) Exogenous ketones lower blood glucose level in rested and exercised rodent models. Nutrients 11, E2330 10.3390/nu11102330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Myette-Côté É., Caldwell H.G., Ainslie P.N., Clarke K. and Little J.P. (2019) A ketone monoester drink reduces the glycemic response to an oral glucose challenge in individuals with obesity: a randomized trial. Am. J. Clin. Nutr. 110, 1491–1501 10.1093/ajcn/nqz232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sherwin R.S., Hendler R.G. and Felig P. (1976) Effect of diabetes mellitus and insulin on the turnover and metabolic response to ketones in man. Diabetes 25, 776–784 10.2337/diab.25.9.776 [DOI] [PubMed] [Google Scholar]
- 54.ISRCTN - ISRCTN16169021: The mechanism whereby an exogenous ketone drink lowers blood glucose [Internet]. Available from: http://www.isrctn.com/ISRCTN16169021?q=&filters=conditionCategory:Not Applicable&sort=&offset=5&totalResults=917&page=1&pageSize=10&searchType = basic-search
- 55.Matthew C. Riddle (2019) Introduction: standards of medical care in diabetes—2019. Diabetes Care 42, S1–S2 10.2337/dc19-Sint01 [DOI] [PubMed] [Google Scholar]
- 56.Wright A.K., Kontopantelis E., Emsley R., Buchan I., Sattar N., Rutter M.K. et al. (2017) Life expectancy and cause-specific mortality in type 2 diabetes: a population-based cohort study quantifying relationships in ethnic subgroups. Diabetes Care 40, 338–345 10.2337/dc16-1616 [DOI] [PubMed] [Google Scholar]
- 57.ISRCTN - ISRCTN12401551: Safety of twenty-eight-day consumption of ΔG® in healthy adults and type 2 diabetes patients [Internet]. Available from: http://www.isrctn.com/ISRCTN12401551
- 58.Evans M., Cogan K.E. and Egan B. (2017) Metabolism of ketone bodies during exercise and training: physiological basis for exogenous supplementation. J. Physiol. 595, 2857–2871 10.1113/JP273185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rich A.J. (1990) Ketone bodies as substrates. Proc. Nutr. Soc. 49, 361–373 10.1079/PNS19900042 [DOI] [PubMed] [Google Scholar]
- 60.Alverdy J.C. (2018) Hypermetabolism and nutritional support in sepsis. Surg. Infect. (Larchmt) 19, 163–167 10.1089/sur.2017.313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Cecconi M., Evans L., Levy M. and Rhodes A. (2018) Sepsis and septic shock. Lancet 392, 75–87 10.1016/S0140-6736(18)30696-2 [DOI] [PubMed] [Google Scholar]
- 62.Frayn K.N. (1983) Calculation of substrate oxidation rates in vivo from gaseous exchange. J. Appl. Physiol. Respir. Environ. Exerc. Physiol. 55, 628–634 10.1152/jappl.1983.55.2.628 [DOI] [PubMed] [Google Scholar]
- 63.Cox P.J. and Clarke K. (2014) Acute nutritional ketosis: implications for exercise performance and metabolism. Extrem. Physiol. Med. 3, 17 10.1186/2046-7648-3-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Cox P.J., Kirk T., Ashmore T., Willerton K., Evans R., Smith A. et al. (2016) Nutritional ketosis alters fuel preference and thereby endurance performance in athletes. Cell Metab. 24, 256–268 10.1016/j.cmet.2016.07.010 [DOI] [PubMed] [Google Scholar]
- 65.Beylot M., Chassard D., Chambrier C., Guiraud M., Odeon M., Beaufrere B. et al. (1994) Metabolic effects of a d-β-hydroxybutyrate infusion in septic patients. Crit. Care Med. 22, 1091–1098 10.1097/00003246-199407000-00007 [DOI] [PubMed] [Google Scholar]
- 66.Soto-Mota A., Vansant H., Evans R.D. and Clarke K. (2019) Safety and tolerability of sustained exogenous ketosis using ketone monoester drinks for 28 days in healthy adults. Regul. Toxicol. Pharmacol. 109, 104506 10.1016/j.yrtph.2019.104506 [DOI] [PubMed] [Google Scholar]