Abstract
Objective
Worksite wellness programs (WWP) may positively impact employee health, medical expenditures, absenteeism and presenteeism. However, there has been little research to assess the benefits of WWP in small businesses. The purpose of this study is to prospectively evaluate changes in health, absenteeism and presenteeism for employees who participated in a WWP.
Methods
We conducted an observational, three-year cohort study of 5,766 employees from 314 businesses of differing sizes. We followed two cohorts of employees, who completed at least two annual health risk assessments (HRA) between May 2010 and December 2014. Changes from baseline to the first and second follow-up periods were assessed for chronic and non-chronic health conditions, absenteeism and presenteeism.
Results
Small business employees were more likely to participate in the WWP than were employees from large businesses. Changes in chronic and non-chronic health conditions varied by size of business, with small business employees showing improvements in stress, overall health, depression, smoking status, vegetable and fruit consumption, and physical activity, and in their perceptions of job health culture. In contrast, large business employees experienced improvements in stress, vegetable consumption, and alcohol use. No changes in absenteeism or presenteeism were observed.
Conclusions
Small businesses achieve higher employee participation rates and more health improvements when compared to employees from large employers. Findings suggest that small businesses may gain the most from a WWP.
INTRODUCTION
In 2013, 56.8 million U.S. workers, representing 48 percent of the workforce, were employed by small businesses, defined by the Small Business Administration as having fewer than 500 employees. The vast majority (98%) of these businesses had fewer than 100 employees (United States Census Bureau, 2016). While small businesses may benefit from worksite wellness programs WWPs (Newman et al., 2015), they often do not have them (Wilson et al., 1999; Tremblay et al., 2013; Taylor et al., 2016) and may lack the “know how” to implement them (McCoy et al., 2014). Furthermore, there is a dearth of research conducted on small businesses offering WWP, and the small body of relevant research has limited generalizability (Sorensen et al., 2005; Merrill et al., 2011; Merrill, 2013). Small business worksite wellness research has focused on a limited number of industries, few health outcomes, and for short periods of follow-up. Also, this research has not explored program impacts on the large segment of small enterprises that have fewer than 20 (17%) and between 21 and 99 (17%) employees (United States Census Bureau, 2016).
In 2010, Pinnacol Assurance was the first U.S. workers’ compensation (WC) insurer to offer WWP to policyholders. Pinnacol had established a 40-year history of providing occupational health and safety services to businesses (policyholders) in Colorado and hypothesized that worksite wellness services would provide an important and needed addition to those services. The need to offer these services to small employers was strategically important to the insurer because 94% of its businesses are classified as small businesses having fewer than 50 employees.
The purpose of this study is to describe the yearly change in health and work-related outcomes, absenteeism and presenteeism, for employees who participated in a WWP, comparing the impacts on large versus small employers. Instead of combining all small businesses into one category (<500 employees), we examined employees in four sub-categories: <50, 50–99, 100–499, and 500+, based on lines of evidence that organizational behavior varies among small enterprises based on size as well as other factors, some of which are related to size (Sinclair 2013).
Applying the diffusion of innovations theory (Rogers, 1962), we hypothesized that greater impacts would be achieved among employees of smaller-sized businesses than employees of larger businesses. This theory states that innovations spread via the process of communication through various channels to populations over time. Spread depends on factors such as the advantages of the innovation, interpersonal communication with peers, and the rate of adoption by early adopters. It also depends on the social structure that the innovation is diffusing through, such as the interconnectedness or ease with which ideas flow through social networks. In the context of small business, as a social unit, smaller businesses have smaller people networks where interaction takes place more frequently. Within this environment, encouragement to participate may be more meaningful and compelling. Further, access to other forms of health insurance is more limited in smaller businesses, possibly increasing the value of a wellness offering. Thus, increased participation in WWPs should result in greater change in health and work-related outcomes.
We hypothesized that a greater number of non-chronic health-related and work-related outcomes would improve significantly over time among employees of smaller sized businesses than among employees of larger sized businesses. However, given the latency between health behavior changes and measurable change in most of the chronic health conditions that behavior changes are thought to improve, we hypothesized that the incidence of chronic health conditions would not change among employees, regardless of business size.
METHODS
Background
The present study draws upon a cohort of Colorado employees who participated in a prospective longitudinal study. The details of the WWP intervention were described previously (Newman et al., 2015). In brief, participating businesses were encouraged to administer annual health risk assessments (HRAs) to their employees along with unlimited telephonic coaching, and access to educational resources. Participating businesses received organizational level feedback reports and action plans for improving their wellness programs. Employers with 50+ participating employees received company-specific annual recommendations for improving workers’ health. These included analyses of employee needs, ongoing feedback on participation and progress, educational content to distribute to employees, and advice on program enhancements. If employers had fewer than 50 employees, they were given an aggregated report based on their industry’s average health risk profile.
Study design and sample
We conducted an observational, prospective, three-year cohort study of employees from 314 businesses who completed at least two annual HRA anytime during the study period from May 1, 2010 to December 31, 2014. We assessed changes in outcomes from baseline (1st HRA) to 1st follow-up (2nd HRA) and from 1st follow-up to 2nd follow-up (3rd HRA) to determine if change occurred after one year and to determine if change was sustained after two years. Of the 16,926 employees who participated in the WWP by completing at least one HRA, 5,766 employees (34.1%) completed two HRAs and 2,261 (13.4%) competed three HRAs. We evaluated the effect of combining data from employees who completed two HRAs with those who took three HRAs via stratified models. The two cohorts’ results were similar, which indicated that the data could be acceptably combined.
Measures
An online, self-administered, English and Spanish Wellsource HRA provided by Trotter Wellness and certified by the National Committee for Quality Assurance, was offered to employees of participating businesses. In addition to health risk factors, the survey included a shortened version of the World Health Organization’s Health and Work Performance Questionnaire (HPQ) (Kessler et al., 2003) called the HPQ Select (Wang et al., 2003). The HRA data were transferred from the wellness vendor to the Integrated Benefits Institute for de-identification and delivery to the Center for Health, Work and Environment at the Colorado School of Public Health for analysis. A description of study outcomes can be viewed in the supplementary material. The Colorado Multiple Institutional Review Board determined the study to be exempt from human subjects research.
Outcomes
We examined various health risks such as body mass index (BMI), lifestyle behaviors, psychosocial factors, chronic health conditions and measures of self-reported work-outcomes, including absenteeism (sick time) and presenteeism (job performance rating). All non-chronic, chronic, absenteeism and presenteeism variables were coded to reflect best to worst status. The variables and operational definitions can be found in Supplemental Table 1.
Statistical analysis
We used regression analyses to test whether the outcomes changed significantly, comparing the prevalence of the health, absenteeism and presenteeism variables at baseline vs. 1st follow-up, and 1st follow-up vs. 2nd follow-up. The dependent variables were either continuous (e.g., BMI), binary (e.g., currently a smoker, yes or no), or ordered multinomial (e.g., number of alcoholic drinks). Thus, the regression models reflected the appropriate distribution for continuous (distribution=normal, link=identity), binary (distribution=binomial, link=logit), and multinomial (distribution=multinomial, link=clogit) variables. However, for the purposes of description, the variables were dichotomized to display the prevalence of all outcome variables at baseline, 1st follow-up and 2nd follow-up.
We ran a series of contrast tests to generate the mean difference and odds ratios, depending on the type of variable, between health, absenteeism and presenteeism measures at 1st follow-up vs. baseline and 2nd follow-up vs. 1st follow-up. For the continuous outcome (BMI), the coefficients were interpreted as the mean difference in BMI for 1st follow-up or 2nd follow-up minus baseline or 1st follow-up (e.g., BMI at 2nd HRA – BMI at 1st HRA), respectively. For this continuous model, if the mean difference comparing BMI at 1st follow-up vs. baseline and 2nd follow-up vs. 1st follow-up was greater than 0, respectively, BMI increased. For the binary outcomes, the odds ratios (OR) were interpreted as the odds of the outcome being present at 1st follow-up or 2nd follow-up compared to baseline or 1st follow-up (e.g., OR of 2nd HRA divided by OR of 1st HRA). For the multinomial outcomes, the odds ratios were interpreted as the odds of the outcome at 1st follow-up or 2nd follow-up being in a lower (i.e., worse) category than the odds of the outcome at baseline or 1st follow-up. For each of the binary and multinomial model outcomes, odds ratios comparing 1st follow-up vs. baseline and 2nd follow-up vs. 1st follow-up greater than 1.0 were viewed as negative changes in the health outcome.
The final regression models were adjusted for age and gender at baseline, whether the employee completed consecutive HRAs (>6 months - <1.5 years apart), and number of times the employee completed an HRA (2–5 times). For all analyses, the data were stratified by size of business at baseline. In addition, we assumed missing responses in the dataset were unrelated to the missing information and that data were missing at random. Thus, complete case analyses were conducted. All analyses were run in SAS version 9.4 using Proc Genmod.
RESULTS
Description of study sample
Compared to employees at large businesses, a greater percentage of employees in small businesses were female, non-white, and had high school degree or less (see Table 1). Small business employees were more commonly employed in finance, construction/mining, and manufacturing industries and more commonly worked in executive, sales, administrative or laborer roles. Compared to employees from large businesses, employees from all other business sizes generally tended to display worse overall health at baseline (see Table 2). Small business employees rated their overall health as being worse than did employees in large enterprises, with seven percent of small company employees rating their health as fair or poor. A greater proportion of small business employees drank more than 8 alcoholic drinks per week (14.7% vs. 8.0%), smoked (13.0% vs. 3.3%), exercised for less than three days per week (39.2% vs. 31.1%), ate fewer fruits (81.6% vs. 67.7%) and vegetables (71.1% vs. 62.1%) and took sick time in the past month (15.6% vs.12.3%).
Table 1.
Characteristics of the study sample at baseline, stratified by size of business
| Small < 50 |
Small/Medium 50 – 99 |
Medium 100 – 499 |
Large 500 + |
|
|---|---|---|---|---|
| n = 842 |
n = 1093 |
n = 2151 |
n = 1680 |
|
| Variable | n (%) / M(SD) | n (%) / M(SD) | n (%) / M(SD) | n (%) / M(SD) |
| Gender | ||||
| Male | 473 (56.2) | 624 (57.1) | 1382 (64.3) | 1282 (76.3) |
| Female | 369 (43.8) | 469 (42.9) | 769 (35.8) | 398 (23.8) |
| Age | 41.9 (12.4) | 42.7 (12.6) | 42.8 (12.1) | 43.3 (10.9) |
| Race/ethnicity | ||||
| White | 694 (83.9) | 944 (87.4) | 1862 (87.5) | 1485 (89.9) |
| Black | 12 (1.5) | 12 (1.1) | 18 (0.9) | 4 (0.2) |
| Hispanic/Latino | 89 (10.8) | 93 (8.6) | 191 (8.9) | 125 (7.6) |
| Other | 32 (3.9) | 31 (2.9) | 57 (2.7) | 38 (2.3) |
| Education | ||||
| At least a 4-year college degree | 417 (49.5) | 536 (49.0) | 1019 (47.4) | 1121 (66.7) |
| Some college or 2-year degree | 270 (32.1) | 375 (34.3) | 694 (32.3) | 364 (21.7) |
| High school diploma or GED | 127 (15.1) | 127 (11.6) | 331 (15.4) | 123 (7.3) |
| Did not complete high school | 28 (3.3) | 55 (5.0) | 107 (4.9) | 72 (4.3) |
| Employment type | ||||
| Full-time | 755 (91.1) | 976 (92.2) | 1903 (90.6) | 1521 (93.3) |
| Part-time | 68 (8.2) | 79 (7.5) | 181 (8.6) | 99 (6.1) |
| Other | 6 (0.7) | 4 (0.4) | 16 (0.8) | 10 (0.6) |
| Pay scheme | ||||
| Salary | 501 (60.6) | 608 (57.9) | 1082 (52.2) | 908 (56.4) |
| Hourly | 326 (39.4) | 441 (42.0) | 991 (47.8) | 703 (43.6) |
| Industry | ||||
| Agriculture | 13 (1.5) | 4 (0.4) | - | - |
| Mining/Construction | 135 (16.0) | 41 (3.8) | 327 (15.2) | - |
| Manufacturing | 15 (1.8) | 122 (11.2) | 61 (2.8) | - |
| Transport/Communication/Electric/Gas/Sanitation | 40 (4.8) | 2 (0.2) | 64 (2.9) | - |
| Wholesale trade | 47 (5.6) | 34 (3.1) | 19 (0.9) | - |
| Retail trade | 1 (0.1) | 111 (10.2) | 230 (10.7) | 16 (0.9) |
| Finance | 237 (28.5) | 155 (14.2) | 116 (5.4) | - |
| Services | 317 (37.7) | 476 (43.6) | 1002 (46.6) | 1379 (82.1) |
| Public administration | 37 (4.4) | 148 (13.5) | 332 (15.4) | 285 (16.9) |
| Occupation | ||||
| Executive | 190 (22.9) | 200 (18.9) | 370 (17.8) | 143 (8.8) |
| Professional | 235 (28.4) | 305 (28.9) | 677 (32.5) | 954 (58.7) |
| Technical support | 17 (2.1) | 35 (3.3) | 62 (2.9) | 46 (2.8) |
| Sales | 76 (9.2) | 82 (7.8) | 121 (5.8) | 3 (0.2) |
| Clerical and administrative support | 160 (19.3) | 194 (18.4) | 354 (17.0) | 230 (14.2) |
| Service occupation | 67 (8.1) | 140 (13.3) | 256 (12.3) | 175 (10.8) |
| Precision production and crafts worker | 12 (1.5) | 12 (1.1) | 76 (3.7) | 8 (0.5) |
| Chemical/production operator | 1 (0.1) | 17 (1.6) | 8 (0.4) | 4 (0.3) |
| Laborer | 70 (8.5) | 69 (6.6) | 158 (7.6) | 61 (3.8) |
| Annual income (in dollars) | ||||
| <10,000 | 69 (8.2) | 95 (8.7) | 251 (11.7) | 166 (9.9) |
| 10,000 – 14,999 | 22 (2.6) | 28 (2.6) | 96 (4.5) | 46 (2.7) |
| 15,000 – 19,999 | 20 (2.4) | 24 (2.2) | 87 (4.0) | 61 (3.6) |
| 20,000 – 24,999 | 45 (5.3) | 84 (7.9) | 161 (7.5) | 105 (6.3) |
| 25,000 – 34,999 | 152 (18.1) | 220 (20.1) | 324 (15.1) | 198 (11.8) |
| 35,000 – 49,000 | 211 (25.1) | 249 (22.8) | 533 (24.8) | 548 (32.6) |
| 50,000 – 74,999 | 172 (20.4) | 228 (20.9) | 419 (19.5) | 393 (23.4) |
| 75,000 + | 151 (17.9) | 165 (15.1) | 280 (13.0) | 163 (9.70) |
Table 2.
Comparison of lifestyle and psychosocial health risks, absenteeism, presenteeism, and workers’ compensation claims of the study sample at baseline, stratified by size of business
| Small (< 50) |
Small/Medium (50 – 99) |
Small/Medium (50 – 99) |
Large (500 +)* |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 1st follow-up | 2nd follow-up | Baseline | 1st follow-up | 2nd follow-up | Baseline | 1st follow-up | 2nd follow-up | Baseline | 1st follow-up | 2nd follow-up | |
| n=842 | n=835 | n=361 | n=1093 | n=1000 | n=487 | n=2151 | n=2092 | n=984 | n=1680 | n=1839 | n=429 | |
| Variable | % / M(SD) | % / M(SD) | % / M(SD) | % / M(SD) | % / M(SD) | % / M(SD) | % / M(SD) | % / M(SD) | % / M(SD) | % / M(SD) | % / M(SD) | % / M(SD) |
| Overall health rating | ||||||||||||
| Excellent, very good, good | 92.9% | 94.4% | 95.3% | 92.1% | 92.7% | 94.0% | 93.3% | 94.0% | 95.5% | 95.4% | 95.6% | 95.1% |
| Fair, poor | 7.1% | 5.6% | 4.7% | 7.9% | 7.3% | 6.0% | 6.7% | 6.0% | 4.5% | 4.7% | 4.4% | 4.9% |
| BMI | 26.7 (5.5) | 26.6 (5.5) | 27.7 (6.7) | 27.3 (5.8) | 27.2 (5.7) | 27.1 (5.5) | 27.3 (6.0) | 27.1 (5.9) | 26.8 (6.0) | 26.2 (5.3) | 26.6 (5.5) | 26.4 (5.6) |
| Smoking, currently (Ref no) | 13.0% | 10.1% | 7.8% | 10.5% | 9.4% | 6.6% | 10.6% | 9.4% | 5.1% | 3.3% | 4.1% | 3.0% |
| Alcohol drinks per week | ||||||||||||
| 0–7 | 85.3% | 88.0% | 88.4% | 85.8% | 90.5% | 88.3% | 90.2% | 91.9% | 92.5% | 92.0% | 92.5% | 93.2% |
| 8+ | 14.7% | 12.0% | 11.6% | 14.2% | 9.5% | 11.7% | 9.8% | 8.1% | 7.5% | 8.0% | 7.6% | 6.8% |
| Vegetable consumption, cups per day | ||||||||||||
| 2.5+ | 22.9% | 30.8% | 36.3% | 25.3% | 32.2% | 31.6% | 26.8% | 34.8% | 42.9% | 37.9% | 40.9% | 45.2% |
| <2.5 | 77.1% | 69.2% | 63.7% | 74.7% | 67.8% | 68.4% | 73.2% | 65.2% | 57.1% | 62.1% | 59.1% | 54.8% |
| Fruit consumption, cups per day | ||||||||||||
| 2.5+ | 18.4% | 24.2% | 27.2% | 21.9% | 27.3% | 28.5% | 22.9% | 30.4% | 36.4% | 33.3% | 35.1% | 39.9% |
| <2.5 | 81.6% | 75.8% | 72.9% | 78.1% | 72.7% | 71.5% | 77.1% | 69.6% | 63.6% | 66.7% | 64.9% | 60.1% |
| Physical activity days per week | ||||||||||||
| 3+ | 60.8% | 69.6% | 75.1% | 63.1% | 66.1% | 69.6% | 61.7% | 68.3% | 73.3% | 68.9% | 73.6% | 72.3% |
| <3 | 39.2% | 30.4% | 24.9% | 36.9% | 33.9% | 30.4% | 38.3% | 31.7% | 26.7% | 31.1% | 26.4% | 27.7% |
| Physical activity time per week | ||||||||||||
| >=2–3 hours, or run up to 6 to 10 miles | 53.9% | 65.2% | 67.9% | 58.4% | 62.3% | 66.5% | 55.4% | 62.3% | 69.5% | 64.8% | 67.7% | 66.0% |
| <=1 hour, or run up to 5 miles or less | 46.1% | 34.9% | 32.1% | 41.6% | 37.7% | 33.5% | 44.6% | 37.7% | 30.5% | 35.2% | 32.4% | 34.0% |
| Job health culture | ||||||||||||
| Excellent or good | 83.9% | 86.7% | 90.9% | 84.9% | 84.9% | 88.1% | 83.8% | 85.4% | 89.8% | 83.3% | 84.5% | 81.4% |
| Fair or poor | 16.2% | 13.3% | 9.1% | 15.1% | 15.1% | 11.9% | 16.2% | 14.6% | 10.2% | 16.7% | 15.6% | 18.7% |
| Stress at home | ||||||||||||
| Never or sometimes | 83.3% | 86.1% | 87.0% | 81.1% | 83.1% | 83.8% | 80.5% | 83.8% | 85.8% | 86.1% | 87.7% | 89.0% |
| Often or permanent or continual stress | 16.8% | 13.9% | 13.0% | 18.9% | 16.9% | 16.2% | 19.5% | 16.2% | 14.2% | 13.9% | 12.3% | 11.0% |
| Stress at work | ||||||||||||
| Never or sometimes | 69.1% | 70.4% | 71.7% | 70.1% | 69.7% | 69.2% | 69.1% | 69.6% | 73.7% | 68.8% | 69.9% | 67.1% |
| Often or permanent or continual stress | 30.9% | 29.6% | 28.3% | 29.9% | 30.3% | 30.8% | 30.9% | 30.5% | 26.3% | 31.2% | 30.1% | 32.9% |
| Stress over finances | ||||||||||||
| Little or none | 35.9% | 43.2% | 47.4% | 37.2% | 41.3% | 43.3% | 35.8% | 41.7% | 47.1% | 39.8% | 44.5% | 47.3% |
| Moderate or high or severe | 64.1% | 56.8% | 52.6% | 62.8% | 58.7% | 56.7% | 64.2% | 58.3% | 52.9% | 60.2% | 55.5% | 52.7% |
| Absenteeism, at least 1 hour of sick time taken in the past 4 weeks (Ref none) | 15.6% | 12.6% | 11.9% | 14.0% | 16.5% | 13.6% | 14.2% | 13.3% | 11.8% | 12.3% | 12.2% | 11.0% |
| Presenteeism, 1–10 rating best to worst | ||||||||||||
| 0 - Best performance | 20.0% | 19.6% | 21.1% | 19.7% | 18.9% | 17.9% | 20.1% | 19.9% | 20.0% | 21.6% | 22.5% | 19.5% |
| 1+ - Anything less than the best | 80.1% | 80.4% | 78.9% | 80.3% | 81.1% | 82.1% | 80.0% | 80.1% | 80.0% | 78.5% | 77.5% | 80.5% |
Note. Health, absenteeism and presenteeism outcome variables were dichotomized only for descriptive purposes. The final multivariable regression models analyzed the variables in their original form.
One company moved from a medium to a large company from baseline to 1st follow-up, which resulted in a larger sample size at 1st follow-up.
Participation and Retention
At the business level, we observed an inverse relationship between average employee participation rates at each HRA and business size (see Figure 1). At the employee level, employees in large businesses were less likely to continue to complete HRAs at the 2nd follow-up (see sample sizes in Tables 2).
Figure 1:
Business level employee participation rates by HRA and business size (number of employees).
Trends in non-chronic health outcomes over time
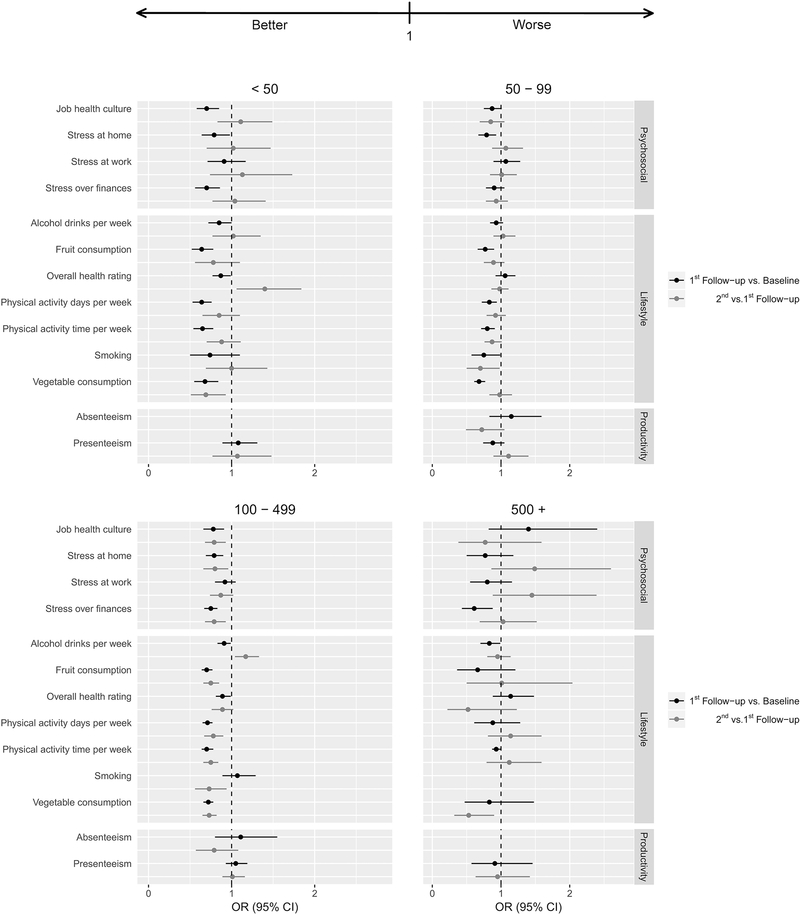
The stratified multivariate regression models demonstrated that change in the non-chronic health-outcomes varied by size of business during the three-year study period (see Table 2 and Figure 2). This supports our first hypothesis.
Figure 2:
Odds ratios and 95% confidence intervals explaining the change in health and productivity outcomes between 1st follow-up and baseline and 2nd and 1st follow-up, stratified by size of business. Note. HRA responses are adjusted for age, gender, number of times employees took an HRA and whether the employee took consecutive HRAs. If information is missing, it is due to a model not converging.
Small businesses (<50)
Employees in small business exhibited significant improvement in eight non-chronic health outcomes from baseline to 1st follow-up, and in two health conditions from the 1st to the 2nd follow-up. For example, the proportion of small business employees reporting excellent or good job health culture increased from 83.9% at baseline to 86.7% and 90.9% at 1st and 2nd follow-up, respectively. This change was statistically significant from baseline to 1st follow-up as the odds of an employee being in a worse job health culture category during the 1st follow-up was 0.70 times the odds of an employee being in a worse job health culture category at baseline (OR = 0.70, 95% CI = 0.58–0.85).
Small/medium businesses (50–99)
Employees in small/medium businesses exhibited significant improvement in five non-chronic health-outcomes from baseline to 1st follow-up, while no health conditions significantly improved from the 1st to the 2nd follow-up. For example, the proportion of small/medium business employees reporting little or no stress at home increased from 81.1% at baseline to 83.1% and 83.8% at 1st and 2nd follow-up, respectively. This change was statistically significant from baseline to 1st follow-up but not from 1st follow-up to 2nd follow-up. The odds of an employee reporting worse stress at home at the time of their 1st follow-up was 0.79 the odds of an employee reporting worse stress at home at baseline (OR =0.79, 95% CI = 0.67–0.93). There was change in the odds of an employee reporting worse stress at home between 1st and 2nd follow-up (OR =1.07, 95% CI = 0.87–1.32). While not significant, BMI was on average 0.15 lower at the 1st follow-up compared to baseline (95% CI = −0.42 – 0.12) and 0.04 lower at the 2nd follow-up compared to 1st follow-up (95% CI = −0.39 – 0.31).
Medium-sized businesses (100–499)
Employees in medium businesses exhibited the most number of improvements in non-chronic health outcomes. Nine outcomes improved significantly from baseline to 1st follow-up, seven of them continued to improve from the 1st to 2nd follow-up. Smoking only improved from 1st to 2nd follow-up (OR =0.73, 95% CI = 0.56–0.94). The proportion of medium business employees reporting smoking went from 10.6% at baseline to 9.4% and 5.1% at 1st and 2nd follow-up, respectively. While not statistically significant, BMI was on average 0.10 lower at the 1st follow-up compared to baseline (95% CI = −0.25 – 0.05) and 0.10 lower at the 2nd follow-up compared to 1st follow-up (95% CI = −0.33 – 0.15).
Large-sized businesses (500+)
Employees in large businesses did not exhibit significant improvement in most of the non-chronic health outcomes. The proportion of large business employees reporting moderate, high or severe stress over finances fell from 60.2% at baseline to 55.5% and 52.7% at 1st to 2nd follow-up, respectively. This change was statistically significant from the baseline to 1st follow-up (OR = 0.61, 95% CI = 0.43–0.88). While not significant, BMI was on average 0.05 higher at the 1st follow-up compared to baseline (95% CI = −0.47 – 0.57) and 0.24 lower at the 2nd follow-up compared to 1st follow-up (95% CI = −0.64 – 0.5).
Trends in chronic health conditions
At baseline, regardless of business size, the most commonly reported chronic health condition was depression. Interestingly, it was the only chronic health condition that improved significantly over time. For example, among small business employees, the proportion of employees reporting depression fell from 20% at baseline to 17% and 15% at 1st and 2nd follow-up, respectively (see Table 3). This was significant from baseline to 1st follow-up as the odds of an employee having depression during 1st follow-up was 0.71 times the odds of an employee having depression at baseline (OR = 0.71, 95% CI = 0.55–0.92).
Table 3.
Comparison of chronic health conditions of the study sample by HRA response, stratified by size of business
| Baseline |
1st Follow-up |
Adjusted odds ratio comparing 1st follow-up vs. baseline |
2nd- Follow-up |
Adjusted odds ratio comparing 2nd follow-up vs. 1st follow-up |
|||
|---|---|---|---|---|---|---|---|
| Variable | % | % | OR | 95% CI | % | OR | 95% CI |
| Small < 50 | |||||||
| Depression | 20.0% | 16.7% | 0.71 | (0.55, 0.92) | 15.0% | 1.00 | (0.50, 2.02) |
| Diabetes | 4.2% | 4.7% | - | 4.7% | - | ||
| Cholesterol | 16.3% | 14.9% | 1.14 | (0.70, 1.84) | 13.8% | 0.81 | (0.60, 1.11) |
| Blood pressure | 15.0% | 15.2% | 0.87 | (0.70, 1.07) | 15.4% | 1.06 | (0.74, 1.54) |
| Small/Medium 50 – 99 | |||||||
| Depression | 23.5% | 21.8% | 0.91 | (0.73, 1.14) | 19.2% | 0.80 | (0.57, 1.11) |
| Diabetes | 4.2% | 4.2% | - | 4.1% | - | ||
| Cholesterol | 19.3% | 20.4% | 1.10 | (0.88, 1.37) | 24.6% | 1.07 | (0.86, 1.33) |
| Blood pressure | 15.6% | 15.6% | 0.99 | (0.79, 1.23) | 18.4% | 1.11 | (0.88, 1.41) |
| Medium 100 – 499 | |||||||
| Depression | 20.9% | 19.2% | 0.77 | (0.61, 0.98) | 18.6% | 0.94 | (0.74, 1.20) |
| Diabetes | 3.9% | 3.9% | 0.91 | (0.78, 1.06) | 4.1% | 1.08 | (0.85, 1.38) |
| Cholesterol | 17.0% | 15.9% | 0.89 | (0.74, 1.06) | 17.0% | 0.85 | (0.65, 1.09) |
| Blood pressure | 16.0% | 15.8% | 0.96 | (0.82, 1.12) | 15.6% | 0.86 | (0.74, 1.00) |
| Large 500+ | |||||||
| Depression | 16.8% | 14.4% | - | 11.1% | - | ||
| Diabetes | 2.6% | 2.8% | - | 3.7% | - | ||
| Cholesterol | 19.5% | 16.3% | - | 13.8% | - | ||
| Blood pressure | 12.9% | 12.8% | - | 11.3% | - | ||
Note. Odds ratios comparing HRA responses are adjusted for age, gender, number of times employees took an HRA and whether the employee took consecutive HRAs
- Model did not converge due to sample size limitations
Trends in absenteeism and presenteeism
Among employees in all sizes of business, we observed no significant change in absenteeism or presenteeism between baseline and 1st follow-up and from 1st follow-up to 2nd follow-up.
DISCUSSION
In a 3-year prospective, study of more than 300 employers, we demonstrate potential benefits of worksite wellness programs for organizations of all sizes. Most notably, small businesses saw the greatest levels of employee participation and improvements in health risk reduction and perceived job health culture. Although there were significant indications of improved health risk behaviors, we did not observe much progress in health outcomes or improvements in either absenteeism nor presenteeism in the participating businesses. This may be due to a relatively short follow-up timeframe. These findings are encouraging from the standpoint of small enterprises that may be considering the merits of having a WWP to promote health behavior change. They also highlight the novel, but potentially important role that WC insurers can play in helping small employers adopt and implement programs aimed at improving worker health and well-being.
Unlike prior research (Soler et al., 2010), employees from large businesses in our study did not exhibit many changes in health. Baseline descriptive and health information demonstrate that the employees from businesses with over and under 500 employees are somewhat different both demographically and in terms of their initial health status. This has two important implications. First, the WWP offered by the WC insurer may have attracted different types of employees depending on business size. It is possible that the employees from large employers had been previously engaged in other WWPs, had previously offered HRAs to employees, and possibly had already achieved positive health changes. If this is the case, then the static health findings in the present study are still encouraging, in that their stability could be interpreted as positive health maintenance. Conversely, for employees of small businesses that participated, this program may have been their first opportunity to participate in a WWP. Anecdotally, we noted that most of the small businesses that enrolled had not had access to a WWP previously. At the time of enrollment, we had to create materials to explain what a WWP and HRA were. Thus, it is likely that these businesses, and the employees, did not have access to these services previously, and that the WWP helped jumpstart their efforts. Future research should seek to understand why employee engagement and health behavior change differs depending on business size during an WWP like this.
Very few studies have evaluated WWPs among small businesses, and none compared their results by different small business definitions. In a review of six small business health promotion programs that were evaluated using group- or cluster-randomized-designs, Harris et al. (2014) reported that all but one of the studies found a significant change in eating, physical activity, or body weight. Of these six studies, one study investigated businesses with 49–1700 employees (Biener et al., 1999), another with 50–350 employees (Beresford et al., 2010), but all others did not report the size of business (French et al., 2010; Lemon et al., 2010; Meenan et al., 2010; Siegel et al., 2010). Sorensen et al.’s (2005) randomized control trial study demonstrated changes in healthy food consumption and physical activity at follow-up among twenty-six small manufacturing businesses with 50–150 employees. Merrill et al.’s separate non-control group longitudinal studies with five small businesses and one medium business, all with fewer than 1000 employees, found positive change at follow-up in exercise, healthy food consumption, sleep, life/job satisfaction, and overall health perceptions (Merrill, 2013) as well as blood pressure, flexibility, and obesity/body weight (men only) (Merrill et al., 2011).
The positive effect of WWPs on health risk behaviors among smaller business employees in the present study may be due to higher employee participation rates compared to large business. This finding may be because knowledge of, and motivation for, WWPs within small businesses may be transmitted faster due to the fewer number of people within their network (Rogers, 1962). While Hall et al. (2014) found employee engagement is a common barrier to WPP effectiveness regardless of business size, our findings suggest that employee engagement may be less of a problem in small businesses given the right program support and an organizational culture that encourages participation.
Although our study ran for three-year period, this may still be a relatively short follow-up time in which to observe significant changes in incidence of chronic health conditions. However, given the significant change in many of the non-chronic health-outcomes, we would expect to see eventual changes in these chronic health outcomes. For example, Pronk et al. (2010) found employees who had optimal lifestyles (physical activity, alcohol, smoking, fruit and vegetable consumption) had a lower two-year risk of chronic health outcome development. Future research should take into account the expected biological latency between a change in health behavior (e.g. diet) and health outcome (improvement in diabetes.)
Based on our past research (Jinnett et al., 2017), we had hypothesized that we would observe improvements in work-related outcomes, although we note that the literature shows mixed evidence for the impact of WWP on absenteeism and presenteeism at work. Much of the previous research has focused on absenteeism, and two reviews of the literature found mixed evidence of whether absenteeism declines during WWPs (Parks and Steelman, 2008; Soler et al., 2010). Subsequent studies, also found little or no relationship (Meenan et al., 2010; Christensen et al., 2013; Hafner et al., 2015). In terms of presenteeism, one study did observe change after their intervention (Christensen et al., 2013), but another did not (Meenan et al., 2010). It is possible that, if our cohort were to be followed beyond three years, work-related outcome gains may eventually be observed. We did observe health risk reduction, and prior studies have linked health behavior changes to absenteeism and presenteeism improvements (Goetzel et al., 2009; VanWormer et al., 2015). Future health and work-related outcomes research is needed to better understand the mechanisms and time lag that should be expected.
Limitations
This longitudinal cohort study design captured data on participating employees and did not afford us the opportunity to survey non-participants. Thus, our ability to demonstrate that the WWP caused the observed changes in health in the present study is limited. However, we were able to compare the changes we observed in our sample to the United States population expected change without a program in an earlier study with our preliminary sample of 121 businesses (Goetzel et al., 2014). A related limitation is that the employers and employees in the program may represent a population that may be more motivated to engage in behavior change. However, our sample was not as healthy as the general Colorado population (Newman et al., 2015). Additionally, we were unable to account for correlation at both the employee and employer level since our sample size, however large, was not able to estimate the more complex, and more realistic, variance structure. When trying to cluster employees within employers the majority of models failed to converge. This is thought to be attributed to a combination of the large number of employers (N=168) and the fact that 46% of these businesses had less than 50 employees, with even fewer responding to the survey. Finally, our analytical strategy may be limited by the self-report nature of the health questions as well as an inability to control for potential unmeasured environmental factors associated with employers.
An additional limitation is that changes in the WWP contributed to a decline in participation between the 1st follow up and the 2nd follow up. The WWP was initially offered as a five-year health improvement program. However, before the end of the 3rd year, Pinnacol Assurance announced that the study would be terminated one year early due to the compelling results, with a new program to be rolled out within a year. Because the largest initial enrollment came during the 2nd year of the program, the majority of 2nd follow up would have occurred during the 4th year of the study. Participants were thus aware that there would be a new program coming shortly and may have opted not to engage in the activities entailed for their second follow up year. Pinnacol Assurance did not actively encourage or discourage participation; in the past, renewal was actively encouraged. These programmatic changes were applied to all of the businesses that participated in our study, thus mitigating any risk of differential access to the intervention.
Conclusions
Our findings suggest that there is an important need and opportunity to engage small businesses in health promotion. The addition of worksite wellness services to existing WC insurer safety services represents an effort to integrate more comprehensive workplace health, as well as safety, practices and programs, consistent with the precepts of Total Worker Health® (Schill and Chosewood, 2013). Our study results suggest that such efforts were successful in fostering job health culture as well as worker engagement and health behavior change among small businesses.
Supplementary Material
Acknowledgments
Funding: This study was funded by Pinnacol Assurance. It was also supported in part by Cooperative Agreement 1 U19 OH 011227, funded by the Centers for Disease Control and Prevention. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention or the Department of Health and Human Services.
References
- Beresford SA, Bishop SK, Brunner NL, Duncan GE, McGregor BA, McLerran DF, West B, Thompson B. (2010) Environmental assessment at worksites after a multilevel intervention to promote activity and changes in eating: the PACE project. J Occup Environ Med; 52 Suppl 1: S22–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biener L, Glanz K, McLerran DF, Sorensen G, Thompson B, Basen-Engquist K, Linnan LA, Varnes J. (1999) Impact of the working well trial on the worksite smoking and nutrition environment. Health Educ. Behav; 26: 478–94. [DOI] [PubMed] [Google Scholar]
- Christensen JR, Overgaard K, Hansen K, Søgaard K, Holtermann A. (2013) Effects on Presenteeism and Absenteeism From a 1-Year Workplace Randomized Controlled Trial Among Health Care Workers. J Occup Environ Med; 55: 1186–90. [DOI] [PubMed] [Google Scholar]
- French SA, Harnack LJ, Hannan PJ, Mitchell NR, Gerlach AF, Toomey TL. (2010) Worksite environment intervention to prevent obesity among metropolitan transit workers. Prev Med; 50: 180–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goetzel RZ, Carls GS, Wang S, Kelly E, Mauceri E, Columbus D, Cavuoti A. (2009) The relationship between modifiable health risk factors and medical expenditures, absenteeism, short-term disability, and presenteeism among employees at Novartis. J Occup Environ Med; 51: 487–99. [DOI] [PubMed] [Google Scholar]
- Goetzel RZ, Tabrizi M, Henke RM, Benevent R, Brockbank CavS, Stinson K, Trotter M, Newman LS. (2014) Estimating the Return on Investment From a Health Risk Management Program Offered to Small Colorado-Based Employers. J Occup Environ Med; 56: 554–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hafner M, van Stolk C, Saunders C, Krapels J, Baruch B. (2015) Health, wellbeing and productivity in the workplace: A Britain’s healthiest company summary report. Book Health, wellbeing and productivity in the workplace: A Britain’s healthiest company summary report, City: RAND Corporation. [Google Scholar]
- Hall ME, Bergman RJ, Nivens S. (2014) Worksite health promotion program participation: A study to examine the determinants of participation. Health Promo Pract; 15: 768–76. [DOI] [PubMed] [Google Scholar]
- Harris JR, Hannon PA, Beresford SAA, Linnan LA, McLellan DL. (2014) Health promotion in smaller workplaces in the United States. Annual Review Public Health; 35: 327–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jinnett K, Schwatka N, Tenney L, Brockbank CV, Newman LS. (2017) Chronic conditions, workplace safety, and job demands contribute to absenteeism and job performance. Health Aff (Millwood); 36: 237–44. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Barber C, Beck A, Berglund P, Cleary PD, McKenas D, Pronk N, Simon G, Stang P, Ustun TB, et al. (2003) The World Health Organization Health and Work Performance Questionnaire (HPQ). J Occup Environ Med; 45: 156–74. [DOI] [PubMed] [Google Scholar]
- Lemon SC, Zapka J, Li W, Estabrook B, Rosal M, Magner R, Andersen V, Borg A, Hale J. (2010) Step ahead a worksite obesity prevention trial among hospital employees. Am J Prev Med; 38: 27–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCoy K, Stinson K, Scott K, Tenney L, Newman LS. (2014) Health promotion in small business: A systematic review of factors influencing adoption and effectiveness of worksite wellness programs. Journal of Occupational and Environmental Medicine; 56: 579–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meenan RT, Vogt TM, Williams AE, Stevens VJ, Albright CL, Nigg C. (2010) Economic evaluation of a worksite obesity prevention and intervention trial among hotel workers in Hawaii . J Occup Environ Med; 52 Suppl 1: S8–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merrill R, Steven GA, Tonya PV, Howe G, David RA, R WW. (2011) The Impact of Worksite Wellness in a Small Business Setting. J Occup Environ Med; 53: 127–31. [DOI] [PubMed] [Google Scholar]
- Merrill RM. (2013) A small business worksite wellness model for improving health behaviors. Journal of Occupational and Environmental Medicine; 55: 895–900. [DOI] [PubMed] [Google Scholar]
- Newman LS, Stinson KE, Metcalf D, Fang H, Brockbank CV, Jinnett K, Reynolds S, Trotter M, Witter R, Tenny L, et al. (2015) Implementation of a worksite wellness program targeting small businesses: The Pinnacol Assurance Health Risk Management Study. Journal of Occupational and Environmental Medicine; 57: 14–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parks KM, Steelman LA. (2008) Organizational wellness programs: A meta-analysis. J Occup Health Psych; 13: 58–68. [DOI] [PubMed] [Google Scholar]
- Pronk NP, Lowry M, Kottke TE, Austin E, Gallagher J, Katz A. (2010) The Association Between Optimal Lifestyle Adherence and Short-Term Incidence of Chronic Conditions among Employees. Popul Health Manag; 13: 289–95. [DOI] [PubMed] [Google Scholar]
- Rogers EM. (1962) Diffusion of innovations. New York,: Free Press of Glencoe. [Google Scholar]
- Schill AL, Chosewood LC. (2013) The NIOSH Total Worker Health™ Program . Journal of Occupational and Environmental Medicine; 55: S8–S11. [DOI] [PubMed] [Google Scholar]
- Siegel JM, Prelop ML, Erausquin JT, Skim SA. (2010) A worksite obesity intervention: Results from a group-randomized trial. Am. J. Public Health; 100: 327–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soler RE, Leeks KD, Razi S, Hopkins DP, Griffith M, Aten A, Chattopadhyay SK, Smith SC, Habarta N, Goetzel RZ, et al. (2010) A systematic review of selected interventions for worksite health promotion. The assessment of health risks with feedback. Am J Prev Med; 38: S237–62. [DOI] [PubMed] [Google Scholar]
- Sorensen G, Barbeau E, Stoddard A, Hunt M, Kaphingst K, Wallace L. (2005) Promoting behavior change among working-class, multiethnic workers: Results of the Healthy Directions—Small Business Study. American Journal of Public Health; 95: 1389–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor AW, Pilkington R, Montgomerie A, Feist H. (2016) The role of business size in assessing the uptake of health promoting workplace initiatives in Australia. BMC Public Health; 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tremblay PA, Nobrega S, Davis L, Erck E, Punnett L. (2013) Healthy Workplaces? A Survey of Massachusetts Employers. Am J Health Promot; 27: 390–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Census Bureau. (2016) Statistics of U.S. Businesses Main. Book Statistics of U.S. Businesses Main, City
- VanWormer JJ, Boucher JL, Sidebottom AC. (2015) Two-year impact of lifestyle changes on workplace productivity loss in the Heart of New Ulm Project. Occup Environ Med; 72: 460–2. [DOI] [PubMed] [Google Scholar]
- Wang PS, Beck A, Berglund P, Leutzinger JA, Pronk N, Richling D, Schenk TW, Simon G, Stang P, Ustun TB, et al. (2003) Chronic Medical Conditions and Work Performance in the Health and Work Performance Questionnaire Calibration Surveys. J Occup Environ Med; 45: 1303–11. [DOI] [PubMed] [Google Scholar]
- Wilson MG, DeJoy DM, Jorgensen CM, Crump CJ. (1999) Health Promotion Programs in Small Results of a National SurveyWorksites:. Am J Health Promot; 13: 358–65. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.