Abstract
Background
The use of ultrasound for peripheral nerve blocks has proven extremely useful for improving the accuracy and efficacy of many regional anesthetic techniques. There remain a few nerve blocks which have lagged behind in employing the assistance of ultrasound consistently, one of which is the ankle block. This block is commonly utilized for either surgical anesthesia or post-operative analgesia for a variety of foot and ankle procedures. The objective of this study was to compare the accuracy of traditional anatomical landmark-guided technique with an ultrasound-guided approach for ankle block by assessing the spread of injectate along the posterior tibial nerve (PTN) in cadaver models.
Materials and Methods
Ten below-knee cadaver specimens were used for this study. Five were randomly chosen to undergo anatomical landmark-guided PTN blocks, and five were selected for ultrasound-guided PTN blocks. The anatomical landmark technique was performed by identifying the medial malleolus and Achilles tendon and inserting the needle (4 cm long, 21G Braun® Stimuplex) at the midpoint of the two structures, aiming toward the medial malleolus and advancing until bone was contacted. The ultrasound technique was performed with a linear probe identifying the medial malleolus and the PTN, with the needle subsequently advanced in-plane with a posterior to anterior trajectory until the tip was adjacent to the nerve. Each specimen was injected with 2 mL of acrylic dye. All the specimens were dissected following injection to determine which nerves had been successfully coated with dye.
Results
The PTN was successfully coated with dye in all five (100%) ultrasound-guided blocks. In the anatomical landmark group, two (40%) PTN were successfully coated with dye. Of the three unsuccessful attempts, two specimens were noted to have dye injected posterior to the PTN; dye was injected into the flexor digitorum longus tendon in one.
Conclusion
The base of evidence has dramatically increased in recent years in support of the use of ultrasound in regional anesthesia. This study substantiates the superiority of ultrasound guidance for ankle block by demonstrating a 100% success rate of delivering a simulated nerve block to the correct anatomic location.
Keywords: Posterior tibial block, Cadaver, Tibial nerve block, Nerve block, Ultrasound guided block
Introduction
Ankle blocks are a common form of perioperative anesthesia and postoperative analgesia due to the safety and effectiveness of the procedure [1, 2]. Most of the sensation of the plantar foot, as well as bony structures of the mid and forefoot, comes from the posterior tibial nerve, making a successful nerve block imperative. Differing methods of achieving a successful nerve block, whether through anatomical landmark-guided (ALG) or ultrasound-guided (USG), have been documented in medical literature [3–6]. ALG blocks have reported success rates towards 100%, according to various studies; however, there are also studies that have found the blocks less than adequate, with many anesthesiologists considering them inferior to USG blocks [2, 7, 8]. Anesthetic administration can differ in respect to landmarks used, ankle positioning, direction of needle insertion, as well as the amount of anesthetic in the syringe [4]. Some techniques rely on the Achilles tendon, medial malleolus, and the palpable posterior tibialis artery, which often can be absent in patients with severe vascular disease [2, 4].
The objective of this study was to compare the accuracy of the anatomical landmark-guided to ultrasound-guided posterior tibial nerve blocks. With ability to visualize anatomical structures, witness real-time visualization of needle, and spread of the local anesthetic through ultrasound, our primary hypothesis is that USG would increase the accuracy of a posterior tibial nerve block at the ankle joint compared to the traditional appreciation of anatomical surgical landmarks in cadaver models.
Methods
Ten fresh-frozen below-knee cadaver, without signs of musculoskeletal abnormalities, to avoid variety in anatomy, specimens were used for this study. Each cadaver was randomly assigned a number, one through ten. Five specimens were randomly chosen to undergo simulated landmark-guided posterior tibial nerve (PTN) blocks, and five were assigned to undergo ultrasound-guided PTN blocks. To simulate the PTN block, a single fellowship-trained anesthesiologist attempted to place a needle (4 cm long, 21G Braun® Stimuplex) into the posterior tibial nerve sheath or its surrounding compartment such that the PTN would be coated by the injected fluid. Upon needle placement, 2 mL of blue acrylic dye was injected. After completion of all injections, each specimen was immediately dissected by a fellowship-trained orthopedic surgeon and assessed for injection accuracy. Specimens in which the dye coated the PTN were considered successful (Fig. 1).
Fig. 1.

Ultrasound-guided injection with dye surrounding the posterior tibial nerve
Anatomical Landmark Technique
The anatomical landmark technique was performed by first palpating and identifying the medial malleolus and the Achilles tendon. The needle was inserted just posterior to the medial malleolus at the midpoint of the two structures. The needle was inserted at a trajectory of approximately 45° to the skin toward the medial malleolus, and advanced until bone was contacted. At this point, the dye was then injected.
Ultrasound-Guided Technique
The ultrasound-guided technique was performed using a linear probe. The medial malleolus was first identified, and the probe was subsequently repositioned until the PTN was identified. The needle was then advanced in-plane with a posterior to anterior trajectory until the tip of the needle was visibly adjacent to the nerve. At this point, 2 mL of blue acrylic dye was injected surrounding the nerve.
Results
Of the ten cadaver specimens used, four were male and six were female. Eight specimens were left-sided, and two were right-sided. The average age of the specimens was 66.2 years.
All five (100%) ultrasound-guided injections were successfully performed, with dye observed to be coating the posterior tibial nerve. Of the landmark-guided injections, two of five (40%) were successfully injected to coat the posterior tibial nerve (Fig. 2). One specimen was noted to have dye injected into the flexor digitorum longus (FDL) tendon sheath. In two specimens, the injections were done posteriorly to the tibial nerve, with dye noted to be posterior to the ankle joint. No specimens were noted to have any structural insult or injury from the procedure. No instances of injection into any vascular structure occurred (Table 1).
Fig. 2.
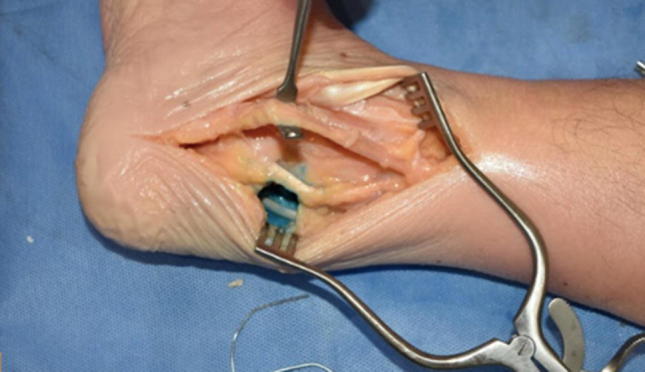
Landmark-guided injection with dye posterior to the posterior tibial nerve
Table 1.
Successful and unsuccessful attempts at ultrasound- and landmark-guided injections by specimen number
| Cadaver no. | Technique | Successful | Notes |
|---|---|---|---|
| 1 | Ultrasound | Yes | |
| 2 | Landmark | No | Injected into FDL tendon sheath |
| 3 | Landmark | No | Injected posteriorly |
| 4 | Ultrasound | Yes | |
| 5 | Landmark | Yes | |
| 6 | Landmark | No | Injected posteriorly |
| 7 | Ultrasound | Yes | |
| 8 | Landmark | Yes | |
| 9 | Ultrasound | Yes | |
| 10 | Ultrasound | Yes |
Discussion
Nerve blocks are a widely used form of pre and post-operative analgesia. This form of regional anesthesia can provide a safer perioperative experience, improve pain control, and reduce opioid consumption after surgery [9]. Patients can also avoid complications that are associated with high opioid dose or general anesthesia. This is particularly advantageous in more susceptible patient populations. This includes patients with a history of cardiopulmonary disease, decreased cognition, dementia, or history of narcotic dependence [10]. It is important to understand the safest form of nerve block delivery to take advantage of these benefits while minimizing possible harm from the procedure. This study showed ultrasound guidance can enhance the accuracy of posterior tibial nerve blocks (100% success rate in five specimens) in a cadaveric model. Although the sample size is limited by the nature of the study, this still demonstrates a more consistent model of nerve block delivered compared to the traditional landmark method (40% success rate in five specimens).
There are several risks associated with using nerve blocks as a form of analgesia after foot and ankle surgery. To minimize these risks, it is important to have a consistent system for delivering blocks. Following PTN block placement, patients can often have problems with their balance and gait [11]. Nerve blocks can also make it difficult for physicians to complete an accurate physical exam. This can mask compartment syndrome in the effected extremity, which although rare, can be devastating if not identified and treated with fasciotomy early. Unfortunately, nerve blocks can mask many of the common symptoms on post-operative exam. One of the more feared complications of nerve blocks is peripheral nerve injury (PNI). In a study of 1014 patients Anderson noted that 5% of patients had postoperative neuropathic symptoms and 0.7% of patients had symptoms at 12 months’ follow-up [12]. This typically occurs when there is direct damage to the nerve leading to traction on the nerve, stretching, or complete transection [9]. These injuries can be long lasting and cause chronic pain. SS Liu, in his systematic review, reported a level 1b evidence to make a grade A recommendation for ultrasound guidance to attain a modest improvement in peripheral nerve block with respect to their onset and quality, particularly in the lower extremity block [13]. Similarly, an analysis of the literature performed by Salinas FV supported the using of USG to decrease block performance time, the block’s onset time, and to achieve increased rate of complete sensory block along with enhanced analgesic efficacy [14]. The use of USG guidance for nerve blocks improves on the anatomic landmark technique in three primary ways: direct visualization of anatomy, avoidance of nearby vasculature, and improved allocation of anesthetic solutions [15]. Hence, the use of ultrasound for tibial nerve blocks can help to minimize peripheral nerve injuries by achieving appropriated block placement while still providing the benefits of PTN blocks to post-operative and pre-operative patients.
The traditional anatomical landmark technique, used to deliver ankle blocks, has a higher rate of inaccurate nerve blocks leading to increased incidence of insufficient anesthetic relief. This can ultimately lead to increased patient discomfort post-operatively [12]. Without adequate pain relief, patients can experience longer rehabilitation times, higher costs, and an increase in adverse patient outcomes [16]. Munirama and Mcleod asserted that ultrasound localization during nerve block reduces patient reported procedural pain [17]. They also found that it decreases the amount of anesthetic needed and accidental vascular puncture. The USG-guided block is a longer procedure that involves more needle redirections, but ultimately has a higher rate of complete block compared to the anatomical landmark technique [2]. Our study further demonstrated that USG technique can be more effective in delivering a simulated nerve block in the desired anatomic location.
There have been several studies that show the clinical advantages of using USG when placing a nerve block [2, 6, 9, 17, 18]. This technique has been shown to reduce patient complications and provide adequate pain relief while reducing the need for heavy narcotics [3]. After comparing the results of the USG and ALG techniques in each specimen we believe that the high success rate of USG is from the higher accuracy of PTN nerve block placement.
There are multiple limitations to this study that should be considered. The study is a cadaver study, so it is uncertain if these results can be considered directly applicable to clinical practice. However, it is common practice to use a cadaveric specimen to replicate and assess the benefits of a procedural technique such as nerve block delivery. To our knowledge, an analysis of PTN block placement has not been carried out in a cadaver model. The cadaveric study can accurately identify which structures were injected with the dye that simulated a block, which is not possible in an in vivo setting. Although we could identify the anatomic structures that were stained with the acrylic dye, it does not guarantee that a patient would have had adequate pain relief with either technique. The study is also limited by the small sample size of ten specimens. This may not give an accurate representation of a larger patient population. Also, results of ultrasound-guided injections cannot be generalized for it depends on the user and his/her experience.
Conclusions
Peripheral nerve blocks are a useful tool for pain control following ankle surgery. This study demonstrates that the use of ultrasound guidance can increase the accuracy of nerve block placement in cadaver models. It can be concluded that the increased anatomical accuracy of PTN blocks with the use of ultrasound guidance can help provide complete anesthetic relief and avoid complications from damaging nearby structures in the medial malleolar space.
Compliance with Ethical Standards
Conflict of Interest
No author holds any financial interest in this manuscript.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Ashish Shah, Email: ashishshah@uabmc.edu.
Sara Morris, Email: semorris@uabmc.edu.
Bradley Alexander, Email: Bradley.alexander@bcm.edu.
Haley McKissack, Email: hmckissack@uabmc.edu.
James Rush Jones, Email: rjones2@uab.edu.
Chandler Tedder, Email: ect1621@jagmail.southalabama.edu.
Aaradhana J. Jha, Email: aaradhana.jha@gmail.com
Rasesh Desai, Email: dr_rasesh@yahoo.com.
References
- 1.Tryba M. Ankle block: a safe and simple technique for foot surgery. Current Opinion in Anesthesiology. 1997 doi: 10.1097/00001503-199710000-00016. [DOI] [Google Scholar]
- 2.Redborg KE, Antonakakis JG, Beach ML, Chinn CD, Sites BD. Ultrasound improves the success rate of a tibial nerve block at the ankle. Regional Anesthesia and Pain Medicine. 2009;34(3):256–260. doi: 10.1097/AAP.0b013e3181a343a2. [DOI] [PubMed] [Google Scholar]
- 3.Falyar CR. Ultrasound-guided ankle blocks: a review of current practices. AANA Journal. 2015;83:357–364. [PubMed] [Google Scholar]
- 4.Wassef MR. Posterior tibial nerve block: a new approach using the bony landmark of the sustentaculum tali. Anaesthesia. 1991 doi: 10.1111/j.1365-2044.1991.tb09597.x. [DOI] [PubMed] [Google Scholar]
- 5.Soares LG, Brull R, Chan VW. Teaching an old block a new trick: ultrasound-guided posterior tibial nerve block. Acta Anaesthesiologica Scandinavica. 2008 doi: 10.1111/j.1399-6576.2007.01515.x. [DOI] [PubMed] [Google Scholar]
- 6.Rudkin GE, Rudkin AK, Dracopoulos GC. Ankle block success rate: a prospective analysis of 1000 patients. Canadian Journal of Anesthesia. 2005 doi: 10.1007/BF03027734. [DOI] [PubMed] [Google Scholar]
- 7.Rudkin GE, Micallef TA. Impediments of the use of ankle block in Australia. Anaesthesia and Intensive Care. 2004;32:368–371. doi: 10.1177/0310057X0403200311. [DOI] [PubMed] [Google Scholar]
- 8.Chin KJ, Wong NWY, MacFarlane AJR, Chan VWS. Ultrasound-guided versus anatomic landmark-guided ankle blocks: a 6-year retrospective review. Regional Anesthesia and Pain Medicine. 2011;36(6):611–618. doi: 10.1097/AAP.0b013e31822b1291. [DOI] [PubMed] [Google Scholar]
- 9.Helander EM, Kaye AJ, Eng MR, Kaye AD, et al. Regional nerve blocks—best practice strategies for reduction in complications and comprehensive review. Current Pain and Headache Reports. 2019 doi: 10.1007/s11916-019-0782-0. [DOI] [PubMed] [Google Scholar]
- 10.Tuncer B. Peripheral nerve blocks in foot and ankle surgery. Türk Ortopedi Ve Travmatoloji Birliği Derneği Dergisi. 2013;12(2):83–87. doi: 10.5606/totbid.dergisi.2013.11. [DOI] [Google Scholar]
- 11.Xing JG, Abdallah FW, Brull R, Oldfield S, Dold A, Murnaghan ML, et al. Preoperative femoral nerve block for hip arthroscopy. The American Journal of Sports Medicine. 2015;43(11):2680–2687. doi: 10.1177/036354651560246. [DOI] [PubMed] [Google Scholar]
- 12.Anderson JG, Bohay DR, Maskill JD, Gadkari KP, Hearty TM, Braaksma W, et al. Complications after popliteal block for foot and ankle surgery. Foot and Ankle International. 2015;36(10):1138–1143. doi: 10.1177/1071100715589741. [DOI] [PubMed] [Google Scholar]
- 13.Liu SS, Ngeow J, John RS. Evidence basis for ultrasound-guided block characteristics. Regional Anesthesia and Pain Medicine. 2010 doi: 10.1097/aap.0b013e3181d266f0. [DOI] [PubMed] [Google Scholar]
- 14.Salinas FV. Evidence basis for ultrasound guidance for lower-extremity peripheral nerve block. Regional Anesthesia and Pain Medicine. 2016;41(2):261–274. doi: 10.1097/aap.0000000000000336. [DOI] [PubMed] [Google Scholar]
- 15.Amini R, Kartchner J, Nagdev A. 2092251 ultrasound guided nerve blocks in emergency medicine practice. Ultrasound in Medicine and Biology. 2015 doi: 10.1016/j.ultrasmedbio.2014.12.655. [DOI] [PubMed] [Google Scholar]
- 16.Hunt KJ, Higgins TF, Carlston CV, Swenson JR, McEachern EJ, Beals TC, et al. Continuous peripheral nerve blockade as postoperative analgesia for open treatment of calcaneal fractures. Journal of Orthopaedic Trauma. 2010;24(3):148–155. doi: 10.1097/bot.0b013e3181bfc9f7. [DOI] [PubMed] [Google Scholar]
- 17.Munirama S, Mcleod G. A systematic review and meta-analysis of ultrasound versus electrical stimulation for peripheral nerve location and blockade. Anaesthesia. 2015;70(9):1084–1091. doi: 10.1111/anae.13098. [DOI] [PubMed] [Google Scholar]
- 18.Su M, Huang P, Tseng K, Shen YC, Chen PN, Cheng KI. Pretreatment of ankle nerve block provides better postoperative analgesia than peri-incisional local anesthetic infiltration in hallux valgus correction surgery. The Kaohsiung Journal of Medical Sciences. 2019;35(3):168–174. doi: 10.1002/kjm2.12029. [DOI] [PMC free article] [PubMed] [Google Scholar]


