Anaphylaxis is a rare, but severe, potentially life-threatening allergic reaction, which most commonly presents with multi-system involvements, such as cutaneous, cardiovascular, respiratory, gastrointestinal and central nervous system signs and symptoms. It can hardly be recognized when occurring in the perioperative period due to the many influencing factors, for example, the cutaneous changes concealed by sterile drapes, inability to describe their symptoms when patients are sedated or anesthetized, and the application of anesthetics leading to sympathetic blockade which presents with blood pressure decrease. All of the above reasons make the identification and immediate treatment of perioperative anaphylaxis difficult and are partially attributable to high mortality.
The overall incidence rate of anaphylaxis during general anesthesia varies greatly worldwide, ranging from 1:20,000 to 1:381.[1,2] The mostly common cause of perioperative anaphylaxis is the use of the neuromuscular blocking agents (NMBAs), antibiotics, antiseptics (such as chlorhexidine), gelatin, latex, and others.[3]
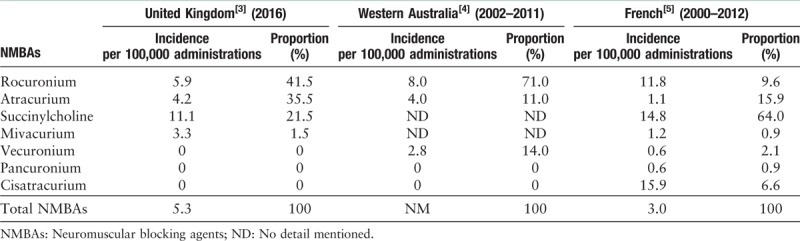
The use of NMBAs, a major cause of perioperative anaphylaxis, has already aroused the attention of anesthesiologists worldwide. Among the NMBAs used commonly in clinical practice, rocuronium is one of the most common culprits in the United Kingdom[3] and Western Australia,[4] while succinylcholine is responsible for over half of the cases of anaphylaxis caused by NMBAs in the France.[5] The big difference in the published incidences of anaphylaxis to NMBAs among studies is mainly due to the variations in local practice, official sales, NMBA exposure, and drug preferences. There have been few reported cases of anaphylaxis triggered by pancuronium or cisatracurium.[3,4] Analysis of recent data on anaphylaxis to NMBAs is shown in Table 1.
Table 1.
The incidences and proportions of anaphylactic reactions to different NMBAs in several epidemiologic surveys.
Several epidemiologic investigations show that antibiotics are common among the top three culprits of perioperative anaphylaxis and the proportion of anaphylactic episodes related to antibiotics significantly increases in recent years.[3,6–8] β-Lactam antibiotics have been identified as a common cause of perioperative anaphylaxis.[9] Immediate hypersensitivity reactions to β-lactam antibiotics may be because of reactivity to the β-lactam moiety or the side chain. Penicillin, amoxicillin, and cephalosporins, which share the β-lactam ring, have been reported as the leading antibiotic triggers for perioperative anaphylaxis.[6,10]
Anaphylaxis to chlorhexidine is an emerging concern. Routes of exposure to chlorhexidine can be divided into three categories: topical cutaneous (such as surgical skin preparation), mucous membrane (such as lubricant gels for urethral catheterization, and vaginal and rectal examination), and parenteral administration (such as a coated central venous catheter). However, it is an easily overlooked trigger due to the atypical presentation of chlorhexidine. It is reported that only 28% of allergies to chlorhexidine are suspected by anesthesiologists.[3] If this potential trigger (eg, coated central venous catheter) is not recognized as the source of the problem and removed, prolonged and intractable anaphylaxis may occur.
The clinical symptoms and signs of anaphylaxis during anesthesia do not vary from those of anaphylaxis in general. The classic clinical features of anaphylaxis are symptoms of the skin and mucous membranes, respiratory system, cardiovascular system, central nervous system, and gastrointestinal system.[11]
For anesthetized patients, the cardiovascular symptoms of anaphylaxis often comprise hypotension and tachycardia, which may rapidly progress into cardiovascular collapse if not recognized and treated in time. The respiratory symptoms, such as oxygen desaturation, difficult ventilation, bronchospasm, airway angioedema, are also common. The cutaneous symptoms, such as erythema, flushing, urticaria and/or angioedema, are common but easily ignored because these features are usually hidden by surgical drapes. Gastrointestinal symptoms (such as crampy abdominal pain, vomiting) and central nervous symptoms (for example, confusion, agitation, and loss of consciousness) can be observed only when patients are conscious in the perioperative period.[6,11,12]
Perioperative anaphylaxis is not always easy to recognize. It requires two elements. (a) Acute onset of anaphylactic reactions: the majority of perioperative anaphylaxis occur within minutes after exposure to triggers, which are often administered intravenously. However, some triggers (eg, latex, chlorhexidine, and the dye patent blue) administered via other routes (eg, skin and mucosa, urethra, peritoneum, or subcutaneous) may cause reactions after more than 15 min. (b) Typical symptoms occur in two or more systems: skin and mucous membranes, respiratory, cardiovascular, gastrointestinal, and central nervous systems.[11] Many anesthesiologists to diagnose anaphylaxis in time as they believe there should be cutaneous signs. However, cutaneous signs can be subtle or absent in up to 20% of reactions.
The grading system of anaphylaxis is important for guiding initial management and facilitating case reports and clinical research.[13] As the clinical manifestations of perioperative anaphylaxis show striking variations of severity ranging from mild to catastrophic, the severity-grading of anaphylactic reactions mainly depends on clinical signs and symptoms of patients. In the available literature, a number of grading systems with three, four, or five scales have been developed as ways of stratifying the severity of anaphylactic reactions. The most quoted grading system is developed by Ring and Messmer,[14] which includes the four grades: grade 1 (mild) is generalized cutaneous signs (erythema, urticaria with or without angioedema); grade 2 (moderate) is moderate multi-organ involvement with cutaneous signs, hypotension, and tachycardia, bronchial hyperreactivity (cough, ventilatory impairment); grade 3 (life-threatening) is severe life-threatening multi-organ involvement requiring specific treatments (circulatory collapse, tachycardia or bradycardia, cardiac arrhythmias, bronchospasm), but the cutaneous signs may be absent or occur only after the arterial blood pressure recovers; and grade 4 (arrest) is circulatory or respiratory arrest. The Scandinavian clinical practice guidelines on anaphylaxis add a fifth severity category, where grade 5 is death due to a lack of response to cardiopulmonary resuscitation.[12] The members of the Australian and New Zealand Anesthetic Allergy Group (ANZAAG) have proposed a new grading system of the Perioperative Anaphylaxis Grading System (PAGS).[13] It defines three grades of anaphylaxis: A, moderate; B, life-threatening and C, cardiac arrest with or without respiratory arrest. The grading system of PAGS removes grade 1 (mild) reactions as only the appearance of cutaneous symptoms in a stable patient should not prompt the use of epinephrine and the initiation of resuscitative treatments.
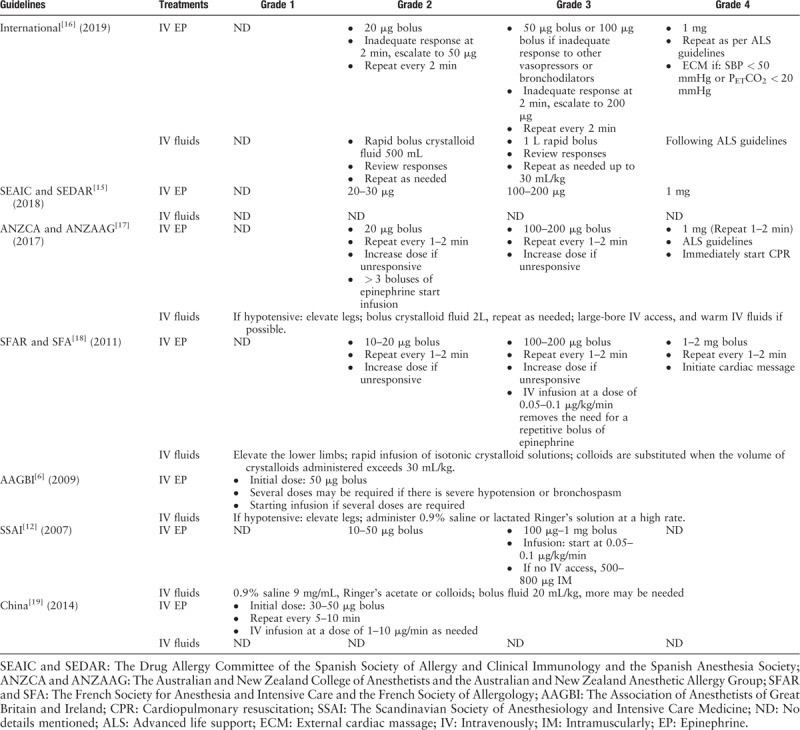
The cornerstones of treatments for perioperative anaphylaxis are intravenous epinephrine and fluid resuscitation. In managing perioperative anaphylaxis, there are actually no contraindications for the use of epinephrine. It must be emphasized that failure to inject epinephrine promptly is potentially associated with fatal outcomes. The available evidence that fatal anaphylaxis is significantly associated with delayed epinephrine administration and epinephrine is often under-used during anaphylaxis treatment.[11] However, potentially serious adverse effects by an overdose of epinephrine, such as ventricular arrhythmias, hypertensive crisis, and pulmonary edema, should not be ignored. Thus, it is best that epinephrine is intravenously tailored according to clinical severity. In addition, aggressive fluid resuscitation should immediately be initiated to treat the intravascular volume depletion. However, fluid administration is not always sufficient.[3] To date, several guidelines or consensus recommendations on the management of perioperative anaphylaxis about the intravenous epinephrine dose and fluids in adults are shown in Table 2.[6,12,15–19] In particular, in 2014, the Anesthesiology Branch of the Chinese Medical Association issued an expert consensus on the diagnosis and treatment of perioperative anaphylaxis, in which clinical symptoms, diagnosis, and treatments of perioperative anaphylaxis were described in detail, and a warning card of perioperative anaphylaxis was provided.[19] Recently, Zong and Hu[20] again reviewed the etiology, diagnosis, prevention, and treatment of perioperative anaphylaxis, in order to improve clinicians’ awareness of this life-threatening event and reduce the related morbidity and mortality.
Table 2.
Summary of immediate management of perioperative anaphylaxis in adults in different guidelines or consensus recommendations.
In conclusion, perioperative anaphylaxis is often a life-threatening clinical condition involving multiple organ systems, with the severity ranging from mild to catastrophic. As the incidence of perioperative anaphylaxis is relatively low and clinical features are most changeful, it is difficult for anesthesiologists to accurately recognize and properly respond within a short time, which may significantly reduce the mortality rate. Therefore, both the mastery of clinical features of perioperative anaphylaxis and immediate initiation of effective management are very important for successful treatment.
Conflicts of interest
None.
Footnotes
How to cite this article: Zou Y, Shao LJ, Xue FS. Perioperative anaphylaxis: a potential hazard to the safety of surgical patients. Chin Med J 2020;133:609–612. doi: 10.1097/CM9.0000000000000659
References
- 1.Berroa F, Lafuente A, Javaloyes G, Cabrera-Freitag P, de la Borbolla JM, Moncada R, et al. The incidence of perioperative hypersensitivity reactions: a single-center, prospective, cohort study. Anesth Analg 2015; 121:117–123. doi: 10.1213/ANE.0000000000000776. [DOI] [PubMed] [Google Scholar]
- 2.Fisher MM, Baldo BA. The incidence and clinical features of anaphylactic reactions during anesthesia in Australia. Ann Fr Anesth Reanim 1993; 12:97–104. doi: 10.1016/s0750-7658(05)81016-0. [DOI] [PubMed] [Google Scholar]
- 3.Harper NJN, Cook TM, Garcez T, Farmer L, Floss K, Marinho S, et al. Anaesthesia, surgery, and life-threatening allergic reactions: epidemiology and clinical features of perioperative anaphylaxis in the 6th National Audit Project (NAP6). Br J Anaesth 2018; 121:159–171. doi: 10.1016/j.bja.2018.04.014. [DOI] [PubMed] [Google Scholar]
- 4.Sadleir PH, Clarke RC, Bunning DL, Platt PR. Anaphylaxis to neuromuscular blocking drugs: incidence and cross-reactivity in Western Australia from 2002 to 2011. Br J Anaesthesia 2013; 110:981–987. doi: 10.1093/bja/aes506. [DOI] [PubMed] [Google Scholar]
- 5.Petitpain N, Argoullon L, Masmoudi K, Fedrizzi S, Cottin J, Latarche C, et al. Neuromuscular blocking agents induced anaphylaxis: results and trends of a French pharmacovigilance survey from 2000 to 2012. Allergy 2018; 73:2224–2233. doi: 10.1111/all.13456. [DOI] [PubMed] [Google Scholar]
- 6.Harper NJ, Dixon T, Dugue P, Edgar DM, Fay A, Gooi HC, et al. Suspected anaphylactic reactions associated with anaesthesia. Anaesthesia 2009; 64:199–211. doi: 10.1111/j.1365-2044.2008.05733.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Krishna MT, York M, Chin T, Gnanakumaran G, Heslegrave J, Derbridge C, et al. Multi-centre retrospective analysis of anaphylaxis during general anaesthesia in the United Kingdom: aetiology and diagnostic performance of acute serum tryptase. Clin Exp Immunol 2014; 178:399–404. doi: 10.1111/cei.12424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mertes PM, Alla F, Trechot P, Auroy Y, Jougla E. Anaphylaxis during anesthesia in France: an 8-year national survey. J Allergy Clin Immunol 2011; 128:366–373. doi: 10.1016/j.jaci.2011.03.003. [DOI] [PubMed] [Google Scholar]
- 9.Scolaro RJ, Crilly HM, Maycock EJ, McAleer PT, Nicholls KA, Rose MA, The R. Australian and New Zealand anaesthetic allergy group perioperative anaphylaxis investigation guidelines. Anaesth Intensive Care 2017; 45:543–555. doi: 10.1177/0310057X1704500504. [DOI] [PubMed] [Google Scholar]
- 10.Kuhlen JL, Jr, Camargo CA, Jr, Balekian DS, Blumenthal KG, Guyer A, Morris T, et al. Antibiotics are the most commonly identified cause of perioperative hypersensitivity reactions. J Allergy Clin Immunol Pract 2016; 4:697–704. doi: 10.1016/j.jaip.2016.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Simons FE, Ardusso LR, Bilo MB, El-Gamal YM, Ledford DK, Ring J, et al. World allergy organization guidelines for the assessment and management of anaphylaxis. World Allergy Organ J 2011; 4:13–37. doi: 10.1097/WOX.0b013e318211496c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kroigaard M, Garvey LH, Gillberg L, Johansson SG, Mosbech H, Florvaag E, et al. Scandinavian Clinical Practice Guidelines on the diagnosis, management and follow-up of anaphylaxis during anaesthesia. Acta Anaesthesiol Scand 2007; 51:655–670. doi: 10.1111/j.1399-6576.2007.01313.x. [DOI] [PubMed] [Google Scholar]
- 13.Rose MA, Green SL, Crilly HM, Kolawole H. Perioperative anaphylaxis grading system:’making the grade’. Br J Anaesth 2016; 117:551–553. doi: 10.1093/bja/aew251. [DOI] [PubMed] [Google Scholar]
- 14.Ring J, Messmer K. Incidence and severity of anaphylactoid reactions to colloid volume substitutes. Lancet 1977; 1:466–469. doi: 10.1016/s0140-6736(77)91953-5. [DOI] [PubMed] [Google Scholar]
- 15.Laguna JJ, Archilla J, Dona I, Corominas M, Gastaminza G, Mayorga C, et al. Practical guidelines for perioperative hypersensitivity reactions. J Investig Allergol Clin Immunol 2018; 28:216–232. doi: 10.18176/jiaci.0236. [DOI] [PubMed] [Google Scholar]
- 16.Garvey LH, Dewachter P, Hepner DL, Mertes PM, Voltolini S, Clarke R, et al. Management of suspected immediate perioperative allergic reactions: an international overview and consensus recommendations. Br J Anaesth 2019; 123:e50–e64. doi: 10.1016/j.bja.2019.04.044. [DOI] [PubMed] [Google Scholar]
- 17.Kolawole H, Marshall SD, Crilly H, Kerridge R, Roessler P. Australian and New Zealand anaesthetic allergy group/Australian and New Zealand College of Anaesthetists Perioperative Anaphylaxis Management guidelines. Anaesth Intensive Care 2017; 45:151–158. doi: 10.1177/0310057X1704500204. [DOI] [PubMed] [Google Scholar]
- 18.Mertes PM, Malinovsky JM, Jouffroy L, Aberer W, Terreehorst I, Brockow K, Demoly P. Reducing the risk of anaphylaxis during anesthesia: 2011 updated guidelines for clinical practice. J Investig Allergol Clin Immunol 2011; 21:442–453. [PubMed] [Google Scholar]
- 19.Wang JK, Ye TH, Wu XM, Zhao J, Xue ZG. Liu J, Deng XM. Consensus recommendations for diagnosis and management of perioperative anaphylaxis [in Chinese]. China Anesthesiology: Guidelines and Consensus Recommendations. Beijing:People's Medical Publishing House; 2014. 234–236. [Google Scholar]
- 20.Zong Y, Hu L G. Overview of perioperative anaphylaxis (in Chinese). Int J Anesth Resus 2018; 39:989–992. doi: 10.3760/cma.j.issn.1673-4378.2018.10.017. [Google Scholar]


