To the Editor: Acute generalized exanthematous pustulosis (AGEP) is a rare clinical reaction mainly induced by drugs, characterized by an acute onset of generalized, non-follicular sterile pustules on erythematous skin with fever and increased neutrophil count, which is usually accompanied by a relatively favorable prognosis.[1] Hereby, we present a special case of AGEP complicated with pemphigus foliaceus (PF).
A 46-year old woman presented with multiple pustules on her four limbs during her treatment of PF for three days. PF was diagnosed by skin biopsy three weeks earlier. Small blisters first formed all over her trunk, ruptured quickly and left crusts with underlying erosions. Both direct immunofluorescence of complement C3 and immunoblotting against Dsg1 are positive. Dsg3 was negative. After a 20-day treatment of prednisone gradually added to 120 mg daily from 60 mg, she was slowly improved. Mycophenolate mofetil 500 mg twice daily was added for further disease control, but on the second day, she developed several pustules on the folds of both wrists. Pustules gradually evolved on her four limbs up to elbows and knees, then coalesced into lakes of pus. Pruritus was mild. Skin examination revealed numerous 1–2 mm superficial, non-follicular pustules on the background of erythematous rash with the Nikolsky sign (Figure 1A and 1B). The laboratory results were normal. The skin biopsy on the pustule showed dense infiltration of neutrophils and subcorneal blisters with neutrophils and acantholytic cells (Figure 1D and 1E). Direct immunofluorescence of C3 was positive.
Figure 1.
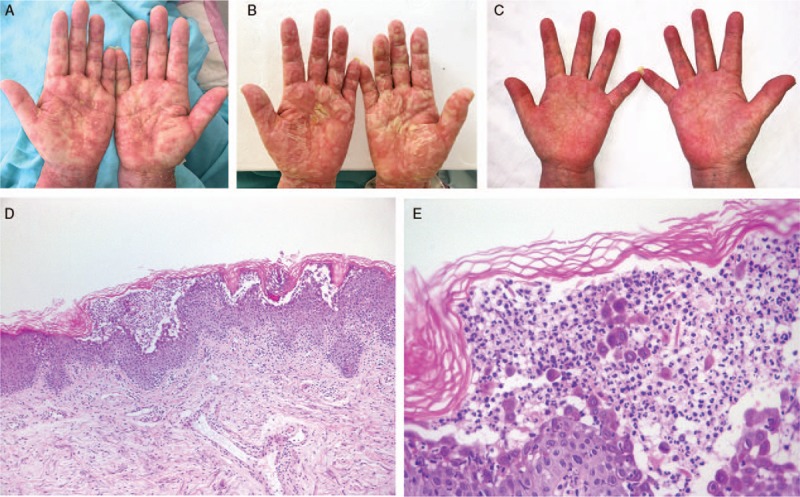
Clinical manifestation of the patient showed extensive, non-follicular sterile pustules on the erythematous base (A), which coalesced into lakes of pus in a few days (B) and resolved quickly after discontinuation of mycophenolate mofetil (C); Skin biopsy revealed not only with neutrophils but also acantholytic cells subcorneal blisters (D, E, Hematoxylin-eosin staining). Mild spongiosis could be seen in the epidermis, and the neutrophils infiltrated both dermis and epidermis (D, original magnification ×100; E, original magnification ×400).
The clinical diagnosis of AGEP was made. Mycophenolate mofetil was stopped immediately while 120 mg prednisone daily was remained. A fever around 38.2°C occurred on the fourth day, which was quickly brought down by a pill of Tylenol. The lesion resolved gradually in a week (Figure 1C).
Mycophenolate mofetil is widely used in autoimmune diseases to inhibiting inosine monophosphate dehydrogenase reversibly with rare drug eruption reported.[2] Although AGEP is associated with azathioprine,[3] another immunosuppressant, this case was induced by mycophenolate mofetil. The rash of AGEP typically tends to appear on the trunk, but sometimes started from extremeties.[4] The former lesions of PF with crusts and excoriation all over her trunk may also be a reason of this rare distribution, and the high-dose of steroid can also explain limited expansion of rash, delayed fever and normal neutrophil count. Pustules in this case can be confused with many other skin eruptions, such as subcorneal pustular dermatitis and pustular psoriasis including palmoplantar pustulosis and acrodermatitis continua. The result of negative IgA in direct immunofluorescence and negative antibodies against Dsg1 in immunoblotting was in the opposition of subcorneal pustular dermatosis. No parakeratosis can be seen in biopsy, thus pustular psoriasis can be excluded. According to AGEP validation score of the EuroSCAR study group, the patient got least eight score with typical lesions, fever and histological findings, which also indicated the diagnosis of AGEP.[5]
Drug eruption including AGEP rarely attributes to immunosuppressant, especially with such a high dose of steroid. Immune dysfunction induced by PF may explain the occurrence of AGEP in this case, and the complication presented a special histological feature of acantholytic cells in subcorneal pustules, which matched the positive Nikolsky sign. Patch test is helpful to confirm the drug sensitivity, [1] but we could not conduct it with lesions of PF on the patient's trunk.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient provided her consent for the images and other clinical information to be reported in the journal. The patient understands that her names and initials will not be published and efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Footnotes
How to cite this article: Chen X, Yang YM, Li B, Li XQ, Zhou C, Jin J, Cai L, Zhang JZ, Mu ZL. Acute generalized exanthematous pustulosis induced by Mycophenolate Mofetil: A case complicated with pemphigus foliaceus. Chin Med J 2020;133:629–630. doi: 10.1097/CM9.0000000000000671
The authors have no conflict of interest to declare.
References
- 1.Szatkowski J, Schwartz RA. Acute generalized exanthematous pustulosis (AGEP): a review and update. J Am Acad Dermatol 2015; 73:843–848. doi: 10.1016/j.jaad.2017.03.002. [DOI] [PubMed] [Google Scholar]
- 2.Georgesen C, Lieber S, Lee H. A generalized fixed drug eruption associated with mycophenolate. JAAD Case Rep 2017; 3:98–99. doi: 10.1016/j.jdcr.2016.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Elston GE, Johnston GA, Mortimer NJ, Harman KE. Acute generalized exanthematous pustulosis associated with azathioprine hypersensitivity. Clin Exp Dermatol 2007; 32:52–53. doi: 10.1111/j.1365-2230.2006.02257.x. [DOI] [PubMed] [Google Scholar]
- 4.Liccioli G, Marrani E, Giani T, Simonini G, Barni S, Mori F. The First Pediatric Case of Acute Generalized Exanthematous Pustulosis Caused by Hydroxychloroquine. Pharmacology 2019; 104:57–59. doi: 10.1159/000500406. [DOI] [PubMed] [Google Scholar]
- 5.Ardern-Jones MR, Mockenhaupt M. Making a diagnosis in severe cutaneous drug hypersensitivity reactions. Curr Opin Allergy Clin Immunol 2019; 19:283–293. doi: 10.1097/ACI.0000000000000546. [DOI] [PubMed] [Google Scholar]


