Barney et al. used biomaterials to uncover a role for fibronectin in preventing breast cancer cell escape from dormancy.
Abstract
Tumors can undergo long periods of dormancy, with cancer cells entering a largely quiescent, nonproliferative state before reactivation and outgrowth. To understand the role of the extracellular matrix (ECM) in regulating tumor dormancy, we created an in vitro cell culture system with carefully controlled ECM substrates to observe entrance into and exit from dormancy with live imaging. We saw that cell populations capable of surviving entrance into long-term dormancy were heterogeneous, containing quiescent, cell cycle–arrested, and actively proliferating cells. Cell populations capable of entering dormancy formed an organized, fibrillar fibronectin matrix via αvβ3 and α5β1 integrin adhesion, ROCK-generated tension, and TGFβ2 stimulation, and cancer cell outgrowth after dormancy required MMP-2–mediated fibronectin degradation. We propose this approach as a useful, in vitro method to study factors important in regulating dormancy, and we used it here to elucidate a role for fibronectin deposition and MMP activation.
INTRODUCTION
Even after apparently successful treatment, disseminated tumor cells (DTCs) can remain viable for many years, entering into a prolonged period of dormancy before eventual activation and outgrowth (1, 2). The presence of these disseminated, largely quiescent tumor cells in the bone marrow is a predictive marker of increased metastatic risk and poor prognosis (1, 2). It has long been hypothesized that DTCs must land in hospitable tissues to grow, and many cells that disseminate to secondary organs are incapable, at least initially, of colonizing and proliferating into an overt metastasis (3). However, it is debated whether the extracellular matrix (ECM) of the secondary tissue site, or any tumor cell–associated remodeling of the said ECM, is a primary determinant of the fate of DTCs.
Strong evidence is emerging to support that certain ECM proteins can promote cell dormancy, including thrombospondin-1 on the microvascular endothelium in breast cancer (4) and osteopontin within the bone marrow in leukemia (5). In related examples, collagen I fibrosis is required for outgrowth of a dormant breast cancer population (6, 7), and collagen I–mediated signaling through discoidin domain receptor tyrosine kinase 1 (DDR1) is required for reactivation of dormant breast cancer cells (8). Physical properties of the ECM have been implicated as well, in that stiff environments promote cell proliferation, while softer surfaces support quiescence (9). Recent work has demonstrated that changes in the expression of ECM proteins can facilitate cell survival and outgrowth. For instance, fibronectin is produced by the stroma to support survival of metastasizing lung cancer cells (10). Breast cancer cells have also been shown to trigger stromal periostin secretion (11) or produce their own tenascin C (12) to metastasize to the lung. Although not directly related to dormancy, these latter studies point to the importance of the generation of provisional matrices in first mediating survival and then outgrowth of disseminated cells.
Although entrance into dormancy and reactivation are continuous and dynamic processes, most dormancy studies use static, endpoint measurements in vivo. Because of the difficulty of live imaging in vivo and the prohibitive cost of high-resolution sampling in time, these studies inherently cannot simultaneously capture the spatial dynamics and heterogeneity of microenvironment components alongside the ability to visualize the proliferation or quiescence of an entire cell population. An endpoint measurement such as immunohistochemistry can identify colocalized Ki67-labeled cells with ECM (4, 13), which only correlates these ECM proteins with cell proliferation. A major limitation with these studies is that there is no way to determine whether an individual Ki67− cell will eventually proliferate. Intravital imaging has started to address this problem, but it cannot yet view cells deep in the animal (5, 14–16), and it is nearly impossible to search an organ for an individual or small group of dormant cells. Despite these limitations, key recent in vivo studies have linked dormant cell outgrowth to fibrosis (6), transmembrane 4 L six family member 1 (TM4SF1) (8), miR-138 (17), and most recently, laminin and smoking (14) in the lung. These efforts have required large pools of mice, particularly cost prohibitive for most laboratories. We sought to find an alternative strategy that would enable higher throughput screens across cell sources and ECMs to determine how a population of disseminated cells enters dormancy and eventually transitions to overt metastatic outgrowth.
We developed a cell culture system capable of inducible and reversible population-level dormancy, where we can track the dynamics of individual cells and cell clusters. Using live imaging, we reveal substantial heterogeneity across a dormant population of cells, simultaneously consisting of Ki67-positive, Ki67-negative, senescent, and actively proliferating cells. Across a diverse set of human breast cancer cell lines, those that could enter long periods of dormancy consistently produced and assembled a fibronectin matrix through α5β1 integrin–mediated adhesion and rho-associated kinase (ROCK)–mediated cell tension. The ability to proliferate after dormancy depended on the ability to degrade the fibronectin matrix with matrix metalloproteinase 2 (MMP-2). We demonstrated that the recipient ECM determined successful entry into and exit from dormancy, providing clues toward previously under-appreciated ECM-associated therapeutic targets to prevent reactivation of dormant cell populations.
RESULTS
In vitro model of dormancy reveals a heterogeneous population of cell cycle–arrested and proliferative cells
We combined our established system of defined ECM protein surfaces (18, 19) with serum deprivation to force cell populations into a dormant-like state (Fig. 1A). We define population level, or tumor dormancy [here referred to as “dormancy” (20)], as a cell population that is not increasing in number but remains viable for an extended time (at least 4 and up to 12+ weeks). The cell culture medium was serum and growth factor free but contained amino acids, vitamins, sugars, and salts. Continuous culture under this serum deprivation condition decreased both cell number and number of actively cycling cells (Ki67+) over the first 10 to 14 days, and we could rescue cell growth (both total number and Ki67+) by reintroducing serum (ZR-75-1 cells shown as typical example in Fig. 1A). This is indicative of a reversible, quiescent phenotype in some subpopulation of cells within the dormant culture.
Fig. 1. Serum withdrawal induces a reversible dormant phenotype in breast cancer cells.
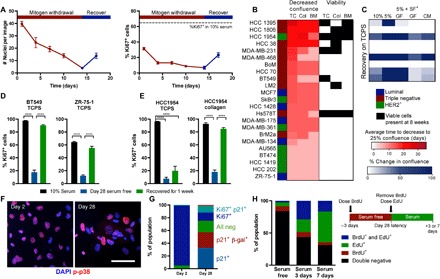
(A) ZR-75-1 breast cancer cell line number and proliferation (Ki67 staining) over time with serum withdrawal (red) and recovery in full serum (blue). (B) Survival of breast cell lines on TCPS (TC), collagen I coverslips (Col), or a mixture of ECM proteins inspired by those found in the bone marrow (BM)–functionalized coverslips. Average time to decrease confluence from 100 to 25% (scored by visual inspection by the same observer) is displayed on the left in red, and conditions where viable cells were detected at 8 weeks in culture are labeled on the right in black. (C) Best-performing cell lines were cultured on TCPS for 6 weeks and stimulated with varying media conditions (GF, growth factor cocktail; CM, conditioned medium from mesenchymal stem cells). SF, serum-free. Heat map shows increase in confluence over 7-day stimulation in blue. (D) Ki67 quantification of BT549 and ZR-75-1 plated on TCPS and (E) of HCC 1954 on TCPS or collagen. Black, 10% serum control; blue, day 28 serum-free culture; green, 7-day recovery. (F) Immunofluorescent staining for phospho-p38 (red; Thr180/Tyr182) and 4′,6-diamidino-2-phenylindole (DAPI) (blue) in HCC 1954 on collagen coverslips after 2 and 28 days of serum starvation (scale bar, 100 μm). (G) Population quantification of HCC 1954 via costaining of Ki67, p21, and senescence-associated β-galactosidase (β-gal). (H) BrdU- and EdU-labeling experiment schematic and results for HCC 1954 on collagen. Black, double negative; red, BrdU positive; green, EdU positive; blue, double BrdU and EdU positive. P < 0.05 was considered statistically significant. P < 0.05 is denoted with *P < 0.05, and ****P ≤ 0.0001.
We performed a screen on 23 human breast cancer cell lines to find those capable surviving 8 weeks of serum deprivation (Fig. 1B) and our ability to rescue growth after 7 days in serum or growth factor cocktails (Fig. 1C). Only eight cell lines had viable cells remaining after 8 weeks of serum starvation, and of those, only five cell lines could be restimulated to grow. For some of the poor-performing cell lines (e.g., ZR-75-1), we could boost their serum deprivation survival by increasing the cell density (fig. S1). We then asked whether the ECM proteins presented on the cell culture surface affected this reversible dormancy by performing the assay on tissue culture plastic, on a pure collagen 1 surface, or on a mixture of proteins reflective of those found in the bone marrow (a common site for clinical dormancy; Fig. 1B). These environments were made via covalently cross-linking proteins to a glass coverslip, with our previously published method (18). Largely, the ability of the serum deprivation stress to reduce cell culture confluency was independent of the ECM substrate, with few exceptions (most notably, MDA-MB-468, BT549, and MDA-MB-231). However, our ability to detect viable cells with a live-dead assay after a full 8 weeks of serum deprivation was highly substrate dependent for those cultures that did survive (Fig. 1B, right), with only the HCC 1954 and Hs578T cell lines having viable cells left on all ECMs.
From Fig. 1B, we chose to further investigate the HCC 1954, BT549, and ZR-75-1 cell lines, as these cell lines represent different clinical subtypes (HER2+, triple negative, and luminal, respectively), and they exhibited high, moderate, and low survival under serum starvation, respectively. Serum-free culture over 4 weeks induced population-level dormancy in these cell lines, defined by few Ki67+ cells (Fig. 1, D and E). When stimulated with serum, each cell population recovered their proliferation within a week. The HCC 1954 cell line only fully recovered the Ki67+ cell population on a collagen I–coated coverslip not on tissue culture polystyrene plates (TCPS) (Fig. 1E). To more deeply examine whether ECM was important in promoting survival in this assay, we screened serum-free survival of all three cell lines across several ECM proteins and protein combinations, varying amounts of those proteins, and different substrate stiffnesses. Of all these variables, we found that ECM protein identity, specifically collagen I, most notably promoted cell survival during serum starvation (fig. S2). For this reason, all subsequent experiments were performed using HCC 1954 on this substrate unless otherwise noted.
After 4 weeks of serum withdrawal, 10 to 20% of cells were still Ki67+, so we asked whether cells were actively proliferating, cell cycle arrested, or more homogeneously quiescent (Fig. 1, D and E). First, we observed that a subset of cells expressed active p38 after 28 days of serum deprivation (Fig. 1F), characteristic of a well-characterized dormancy program in vivo (21). Second, time-lapse imaging identified a small population of proliferating cells undergoing mitosis (movie S1). Third, we found that expression of p21 was significantly elevated in our dormant population, indicative of cell cycle arrest (fig. S3C). When we costained the population of cells after 2 and 28 days of serum deprivation for Ki67, p21, and senescence-associated β-galactosidase, we found that most cells were Ki67+ after 2 days, but there was a richly diverse set of cell cycle states across the population after 28 days (Fig. 1G). Most of the population was simultaneously p21+ and Ki67−, indicating that a large fraction of the surviving population was both cell cycle arrested and nonproliferative. However, cells remained that were negative for all markers, or were Ki67+, and we speculated that some of these cells were responsible for maintaining cell numbers after long periods of serum deprivation and possibly responsible for regrowth when serum was replenished in the “recovery” experiments.
To directly test whether individual cells could regain proliferation after dormancy, we sequentially labeled cells with 5-bromo-2′-deoxyuridine (BrdU) at day 25 of serum starvation, and 5-ethynyl-2′-deoxyuridine (EdU) immediately upon serum-stimulated recovery, and followed them for either three or seven additional days. We saw a large population of cells that did not incorporate BrdU during serum deprivation but did incorporate EdU during reactivation; that is, cells were quiescent during starvation but regained proliferation (Fig. 1H). When repeating this labeling experiment during sequential 72-hour periods of dormancy (i.e., label with BrdU during serum starvation and then label with EdU during a second period of serum starvation), we identified small populations (~7%) that were positive for either BrdU or EdU but not both (Fig. 1H, serum 3 days). Last, the very small percentage of double-positive cells decreased from days 3 to 7, reflective of the cells slowly cycling during serum deprivation, and continued proliferation after serum reintroduction.
This method of serum deprivation–mediated dormancy allowed us to create a population of quiescent (Ki67−) cells, stable for 4 to 8 weeks (fig. S3A). We wondered whether these cells were a result of selection for cells that were robustly “dormancy capable.” When we performed successive rounds of serum removal and recovery on a single culture, we observed no change in the number of surviving or regrowing cells compared to a naïve population (fig. S3B), suggesting that we recapitulated the heterogeneity of the original parental population upon regrowth.
Fibronectin secretion and organization is required for extended dormancy
We observed that many of the surviving cells had a spread, adherent phenotype, with some larger clusters of cells assembled into semi-adhered spheroids (movie S1). This suggested to us that surviving dormant retained both strong cell-matrix and cell-cell adhesions. Since our initial screen identified ECM protein identity as a key factor in serum-free cell survival, we hypothesized that the dormant cell cultures may secrete ECM proteins to support survival. We performed liquid chromatography–mass spectrometry (LC-MS) on HCC 1954 samples enriched for ECM proteins at days 2 and 28 of serum deprivation and again after 1 week of recovery in full serum (fig. S4, A and B). We were excited to find many collagens, glycoproteins, and proteoglycans that were not detectable at day 2, appeared at day 28, and subsequently disappeared when cell cultures were serum recovered (fig. S4, A and B), including fibronectin (isoform 6).
We were particularly interested in ECM proteins with known, strong roles in integrin-mediated adhesion, such as fibronectin, laminins, collagens, vitronectin, and osteopontin. Many of these were detected at day 28 of serum-free culture by LC-MS, and some of them were no longer detectable after recovery in serum (fig. S4B). When we looked more closely at these proteins via immunofluorescence, we saw that laminins (identified with a pan-laminin antibody), vitronectin, and osteopontin were all detected at increased levels during the dormant HCC 1954 culture, but all appeared intracellular by visual inspection (Fig. 2A). Serum-starved cells can uptake ECM to promote survival (22), potentially explaining the intracellular distribution of these proteins we observed. Fibronectin was deposited at high amounts at the day 28 time point (Fig. 2A), and we observed this fibronectin secretion phenotype consistently across all three cell lines we tested (fig. S5A). In particular, the HCC 1954 cells organized a dense fibronectin matrix over 28 days of dormancy, on both TCPS and collagen surfaces (fig. S5B). They did not assemble fibronectin during 28 days of culture in serum-containing medium on any ECM, demonstrating that this secretion happens as a result of serum starvation, not normal growth culture.
Fig. 2. Dormant cells up-regulate extracellular fibronectin specifically during serum withdrawal.
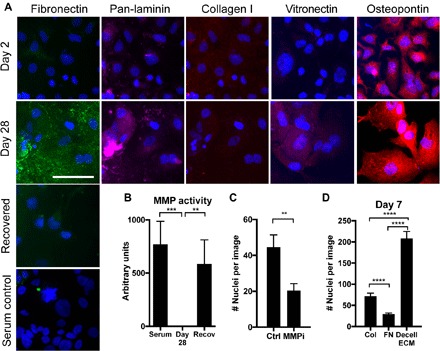
(A) Top, immunofluorescence for matrix proteins and DAPI in HCC 1954 on collagen in serum-free medium for 2 and 28 days. Bottom, immunofluorescence and for fibronectin in HCC 1954s grown for 28 days or serum-starved for 28 days and recovered in situ for 1 week (blue, DAPI; green, fibronectin; pink, laminin; red, collagen I, vitronectin, or osteopontin, as labeled). Scale bar, 100 μm. (B) Total MMP activity of HCC 1954 cells on collagen coverslips (C) Number of nuclei resulting from reactivation of dormant cells treated with a pan MMP inhibitor for 7 days (MMPi; GM6001, 25 μM) or control (serum-containing media, no inhibitor). (D) HCC 1954 day 7 survival on collagen, fibronectin (FN), or HCC 1954 day 28 decellularized ECM (decell ECM) coverslips.
When the cells were cultured in serum-free conditions and then these same cells were recovered in situ with complete serum for 7 days, the fibronectin matrix was locally degraded where we saw high densities of cells (Fig. 2A and fig. S6A). We hypothesized that cells were activating MMPs to degrade the fibronectin. Total MMP activity was measured with a fluorometric assay, and MMP activity was high in cells under normal growth conditions but undetectable in the dormant cell cultures (Fig. 2B). MMP activity was recovered with 1 week of recovery culture in serum, suggesting that MMPs were involved in the fibronectin degradation during reactivation. Specifically, zymography revealed that cathepsins S and V and MMPs 2 and 9 were low, but detectable, in normal growth conditions. These decrease during the serum-free culture (with the exception of MMP-2), and cathepsin V and MMPs 2 and 9 were highly activated during growth recovery (fig. S6, B and C). Last, when the cells were cultured with a pan-MMP inhibitor (GM6001; 25 μM) during serum-stimulated recovery, HCC 1954 regrowth was reduced during serum recovery (Fig. 2C), suggesting that MMP activation and fibronectin degradation are beneficial for regrowth after dormancy. Inhibition of cathepsin activity with E64 (5 μM) did not inhibit reactivation and outgrowth, suggesting that outgrowth is MMP, but not cathepsin, dependent (fig S6D).
To test whether the presence of a fibronectin-rich ECM directly supports long-term cell survival during serum deprivation, we allowed the dormant HCC 1954 cultures to assemble the insoluble fibronectin matrices over the 28 days of serum deprivation, and then, we decellularized these samples and reseeded new, naïve cell cultures onto them. When these cells were subjected to the long-term serum deprivation on these decellularized, fibronectin-rich matrices, we found that HCC 1954 and multiple other cell lines had visibly improved survival compared to the collagen surfaces across several cell lines (Fig. 2D and fig. S5C). This suggests that fibronectin promotes dormant cell survival during the serum starvation. However, some cell lines (AU565 and HCC 1419) showed no ability to survive serum deprivation in the original screen and also did not show improved survival with a decellularized ECM (fig. S4C); thus, fibronectin is not sufficient to support entrance into dormancy by itself. We also surmised that the structure of fibronectin is important in this assay because when we covalently coupled monomeric fibronectin to a coverslip, cells did not survive well (Fig. 2D). Monomeric fibronectin did not support survival as well as collagen (Fig. 2D and fig. S5D).
Dormant cells assemble fibronectin via cancer cell–secreted TGFβ
Because matrix assembly is classically stimulated by transforming growth factor–β (TGFβ) signaling, we explored whether TGFβ signaling affected the survival of dormant cells. When we provided cell cultures with exogenous TGFβ1 (1 ng/ml) or TGFβ2 (2 ng/ml) at every regular medium change, we saw no effect on cell survival at day 7 (Fig. 3A). Similarly, inhibition of TGFβ receptor signaling with LY-364947, a selective and adenosine 5′-triphosphate–competitive inhibitor of TGFβRI, did not affect day 7 survival (Fig. 3A). When the dormant cell cultures were exposed to the inhibitor over 28 days, however, cell survival was significantly decreased, and we observed a marked decrease in the fibronectin matrix (Fig. 3, B and C). Continuous treatment of the cultures with exogenous TGFβ1 or TGFβ2 for the entire 28-day serum deprivation culture either increased or maintained survival, respectively (Fig. 3, B and C). Analysis of the culture supernatant demonstrated that HCC 1954 express undetectable levels of TGFβ1 and TGFβ3 (Fig. 3D) but high levels of TGFβ2 at day 28 of serum-free culture, suggesting that serum starvation stimulates TGFβ2 secretion, which initiates fibronectin matrix remodeling and the survival of dormant cultures.
Fig. 3. TGFβ2 stimulates fibronectin matrix production that mediates survival during mitogen withdrawal.
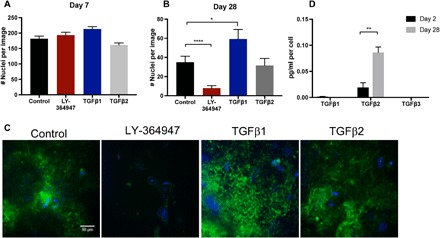
(A and B) Survival of HCC1954 under control, TGFβ receptor inhibition (LY-364947, 5 μM), and TGFβ1 (1 ng/ml) or TGFβ2 (2 ng/ml) stimulation over (A) 7 days or (B) 28 days. (C) Immunofluorescence for fibronectin (green) and DAPI (blue) at day 28. (D) Expression of secreted TGFβ1, TGFβ2, or TGFβ3 in serum-starved cultures at 2 and 28 days in culture. P < 0.05 is denoted with *, P ≤ 0.01 with ** and P ≤ 0.0001 with ****.
Fibronectin is assembled via α5β1 integrin–mediated tension and mediates survival via adhesion through αvβ3 and α5β1 integrins
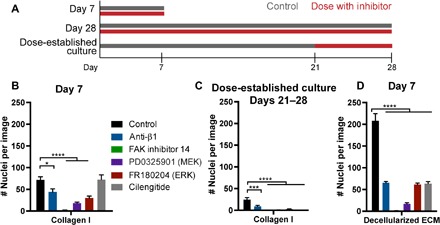
Fibronectin assembly occurs via adhesion through α5β1 integrin and downstream RhoA activation, which then activates rho kinase (ROCK), generating tension to expose cryptic self-assembly sites in fibronectin, inducing polymerization (23–26). The αvβ3 and α5β1 integrin heterodimers bind to fibronectin with high affinity, and we observed that these subunits were transcriptionally up-regulated in our fibronectin-producing dormant cells (fig. S7). We tested whether this pathway of fibronectin assembly was important for dormancy phenotype by inhibiting ROCK (Y-27632). We administered Y-27632 to cell cultures during serum deprivation during the first 7 days (entrance into dormancy), or continuously over all 28 days (long-term dormant survival), or lastly, we allowed the dormant cells to build up a fibronectin matrix for the first 21 days of dormancy and added the inhibitors during days 21 to 28 (Fig. 4A).
Fig. 4. Dormancy-associated fibronectin is assembled via α5β1 integrin and ROCK to mediate survival.
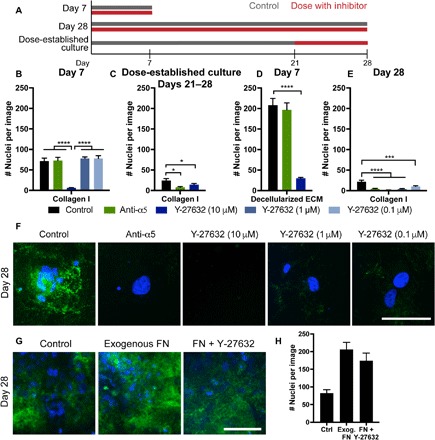
(A) Experimental timeline of inhibitor dosing. Day 7 experiments were dosed continually through a day 7 endpoint; day 28 experiments were dosed continually through a day 28 endpoint; separate cultures were established for 21 days, where inhibitor dosing was initiated for an additional 7 days (“dose-established culture”). (B) Day 7 survival of HCC 1954 on collagen with inhibitors dosed at seeding and every medium change. (C) Survival of cells with inhibitors, dosed after establishment of dormant culture for 21 days and then subsequent dosing at every medium change through days 21 to 28. (D) Day 7 survival of HCC 1954 on decellularized matrix with inhibitors dosed at every medium change. (E) Day 28 survival of cells with inhibitors dosed at seeding and every medium change throughout the entirety of the experiment. Green, α5 integrin function affecting antibody; blue, Y-27632 (ROCK inhibitor at various concentrations). (F) Immunofluorescence for fibronectin (green) and DAPI (blue) at day 28 on collagen with inhibitors dosed for the entire 28-day time period. Scale bar, 100 μm. (G) Immunofluorescence for fibronectin (green) and DAPI (blue) at day 28 on collagen with exogenous fibronectin (10 μg/ml) or fibronectin with Y-27632 (1 μM). (H) Day 28 survival of cells under control, exogenous fibronectin, or fibronectin with Y-27632. P < 0.05 is denoted with *, P ≤ 0.001 with *** and P ≤ 0.0001 with ****.
The maximum dose of Y-27632 (10 μM) inhibited survival of cells over the first 7 days of serum-free culture on collagen-coated coverslips (Fig. 4B, dark blue bars). This maximum dose also inhibited cell survival when we administered the inhibitor after cells were allowed to preestablish the fibronectin matrix (Fig. 4, B and C) and when we seeded cells onto a decellularized ECM (Fig. 4D). However, 10- and 100-fold lower doses of Y-27632 did not affect survival during the first 7 days but prevented survival of cells when administered over the full 28 days of serum deprivation (Fig. 4E). When we supplemented the culture with soluble fibronectin (10 μg/ml) to potentially jump-start the matrix, this promoted survival over the 28 days of serum-free culture, even in the presence of Y-27632 (Fig. 4, G and H). This suggests that cells use ROCK to secrete and assemble fibronectin to survive serum deprivation culture. Maximum doses of ROCK inhibitor prevented cell survival in all cases, but these lower doses allowed us to observe the more specific role of ROCK in fibronectin assembly and long-term survival.
Inhibiting α5 integrin did not affect survival on collagen over the first 7 days (Fig. 4B, green bar), but it reduced cell survival when dosed after establishment of the fibronectin matrix (from days 21 to 28, Fig. 4C). When we seeded cells onto a decellularized matrix while inhibiting α5 integrin, we saw no change in survival over the first 7 days (Fig. 4D). Last, inhibiting α5 integrin function during the entire 28-day duration of the experiment inhibited cell survival under serum deprivation (Fig. 4E). We also saw an absence of fibronectin staining at day 28 in all these inhibitor conditions (Fig. 4F). Collectively, these results suggest that cells require α5 integrin to create the organized fibronectin matrices during serum deprivation.
When β1 integrin, which dimerizes with many alpha subunits (including α5), was similarly blocked, there was minimal ability for cells to survive during serum starvation, regardless of when we applied the treatment [including seeding cells onto decellularized matrices (Fig. 5, B to D)]. This demonstrates that β1 integrin was driving adhesion to both the collagen and fibronectin matrices. To more specifically target adhesion to fibronectin, we used cilengitide, a cyclic RGD drug that reduces fibronectin binding primarily via αvβ3 and αvβ5 integrins (27). Cilengitide treatment did not affect the number of cells adhered to the collagen coverslip (Fig. 5B), but it was highly effective at disrupting survival when the dormant cells had assembled a fibronectin matrix (Fig. 5C) and when cells were seeded onto decellularized matrices containing dense fibronectin (Fig. 5D). Although there is some evidence that αvβ3 integrin can bind to denatured collagen (28), in our cells, cilengitide appeared to reduce adhesion to fibronectin but not to collagen-coupled coverslips.
Fig. 5. Survival is mediated via adhesion-FAK-ERK signaling.
(A) Experimental timeline of inhibitor dosing. Day 7 experiments were dosed continually through a day 7 endpoint; day 28 experiments were dosed continually through a day 28 endpoint; separate cultures were established for 21 days, where inhibitor dosing was initiated for an additional 7 days (dose-established culture). (B) HCC 1954 survival at day 7 on collagen coverslips with selected inhibitors dosed for the duration of the experiment. (C) Survival of HCC 1954 cells after establishment of dormant culture for 21 days and then subsequent dosing with inhibitors through days 21 to 28. (D) HCC 1954 survival at day 7 with inhibitors when seeded onto HCC 1954 decellularized ECM. Black, control; blue, anti-β1 (MAB17781; 1 μg/ml); green, FAK inhibitor 14 (10 μM); purple, PD0325901 (MEK inhibitor, 10 μM); red, FR180204 (ERK inhibitor, 20 μM); gray, cilengitide (100 μM). P < 0.05 is denoted with *, P ≤ 0.001 with *** and P ≤ 0.0001 with ****.
We performed a small screen of tyrosine kinases to identify pathways activated during adhesion to the decellularized fibronectin matrices. Across this screen, only extracellular signal–regulated kinase (ERK) was highly phosphorylated in both the dormant cell cultures and during adhesion to the decellularized ECMs (fig. S8, A to E). Pharmacological inhibitors to focal adhesion kinase (FAK), mitogen-activated protein kinase (MAPK) kinase (MEK), and ERK all decreased cell survival over the first 7 days of serum starvation on both the collagen- and fibronectin-coupled coverslips and decellularized ECMs (Fig. 5, B to D). This supports a hypothesis that cells are activating a survival pathway driven by αvβ3 integrin–mediated adhesion to the assembled fibronectin matrix, downstream of ERK pathway activation during this serum starvation–induced dormancy in culture.
DISCUSSION
Applied cellular stresses, such as serum deprivation, application of drug, or hypoxia, have been used to select for cell populations primed for migration and metastasis (29–33). By combining this approach with engineered materials, we selected for human breast cancer cells that can enter and survive dormancy based on their ability to secrete and organize ECM, a phenotype likely missed using traditional culture platforms or genetic profiling alone (34). Our data support the idea that dense fibronectin matrices facilitate long-term survival of cancer cells during serum deprivation–induced dormancy. Inhibiting α5β1, ROCK, or TGFβ receptor signaling prohibited fibronectin assembly, eliminating a large population of the surviving dormant cells. We suggest a role for α5β1 in this process, as adhesion to fibronectin through α5β1 integrin is associated with mature focal adhesions (23) to support intracellular tension necessary for matrix assembly, while adhesion through αvβ3 does so weakly (35). Reactivation and outgrowth of the cancer cells after the dormancy period could be inhibited by blocking their ability to degrade the fibronectin matrix via MMPs. Although they target different aspects of fibronectin matrix dynamics, both approaches could be promising mechanisms to eliminate dormant cell populations.
Other in vitro models have been used to study spontaneous dormancy (36, 37), using far shorter culture times than our method here. Other approaches have used cell lines preselected with distinct proliferative or dormant potentials (e.g., the 4T1 and D2 series) (7, 17, 38–41). Our study is unique in that a proliferative, heterogeneous cell population can be induced to become dormant via serum deprivation stress, and the dormancy-competent cells can be subsequently reactivated. This approach is analogous to that used in the drug resistance studies, where resistant cells are selected via prolonged drug-induced stress (42, 43). As one validation of our approach, the HCC 1954 cell line capable of showing this dormancy phenotype was also identified by Massagué and colleagues as one of two cell lines capable of generating dormancy-competent cells in vivo (13).
It has been proposed that dormant micrometastases are a mixture of arrested, quiescent, and slow-cycling cells (44). This has not been completely clarified since these studies were endpoint analyses, relying on defining dormant cells by fixed staining for lack of proliferation (Ki67−), DNA synthesis (EdU incorporation), or cell cycle stalling (p27+) (4, 21, 38). These studies report that 70 to 80% of Ki67− or p27+ are dormant in vivo (4, 21); however, in our culture system, the remaining 20 to 30% of Ki67+ cells could be cell cycle arrested (p21+) or proliferative (Fig. 1G). By imaging live cells during the dormant culture, we revealed the presence of persisting cycling, quiescent, and arrested cells, a population-wide phenotype reminiscent of tumor dormancy.
We were initially surprised that our data appeared to contradict that of Aguirre-Ghiso, who has very thoroughly characterized an α5β1 integrin/epidermal growth factor receptor/uPAR/fibronectin mechanism, mediating proliferation through ERK not p38 (45, 46). His laboratory showed that fibronectin fibrils block the p38 activity characteristic of quiescent cells, which results in sustained ERK signaling and proliferation (45, 47, 48). Our data showed that dormant cells simultaneously suppressed p38 and activated ERK (fig. S6, A and B). However, when looking closer, immunofluorescence revealed that high phospho-ERK was ubiquitous (fig. S6E), but phospho-p38 was heterogeneous (Fig. 1F). This suggests that this subpopulation of dormant cells may be activating the same stress signaling pathway described by the Aguirre-Ghiso laboratory (47). In fibroblasts, serum withdrawal induces a reversible quiescence, wherein cells initially have decreased ERK activity that is eventually regained and sustained (49). This report is consistent with the high phospho-ERK we report at long dormancy times in cancer cells (fig. S6A). Induction of stromal cell senescence is associated with acute activation of p38 and interleukin-6 release after genotoxic stress in lymphoma (50). Therefore, it is possible that the heterogeneous population of p38-high and p38-low cells is associated with senescent and quiescent cells, respectively, allowing for a population-level dormancy in response to serum deprivation stress.
We found that the assembly of fibronectin coincided with entrance into a dormant phenotype, and this fibronectin assembly was dependent on TGFβ. Similarly, in cancer-associated fibroblasts, TGFβ is required to create a desmoplastic ECM (51), and oncofetal splice variants of fibronectin are stimulated by TGFβ in glioblastoma (52). We observed that cells required ROCK activation to assemble this fibronectin matrix, and other work has shown that there may be a feedback loop between tension-mediated TGFβ release and matrix assembly (53). Cells responding to TGFβ are less proliferative but more invasive and drug resistant (54). Further, there are other reports of a TGFβ2 regulating the dormancy of tumor cells (21, 55). The well-characterized senescence-associated secretory phenotype is associated with a secretome that includes TGFβ (56). This suggests that the senescent subpopulation we observed in our cultures (Fig. 1G) may be contributing to TGFβ release and subsequent fibronectin deposition. TGFβ is a promising target in many cancer clinical trials, and we suggest here a role for an anti-TGFβ therapy to prevent survival of dormant disseminated cells (57).
Our data suggest that TGFβ-mediated secretion of fibronectin allows cells to maintain a dormant state, agreeing with a recent demonstration that the optimal anti-TGFβ treatment for metastasis was during the pre-metastatic stage (58). We also saw that inhibiting TGFβ significantly and substantially reduced the number of surviving cells during our dormancy assay (Fig. 3B); however, this could be clinically challenging because metastatic cells can disseminate extremely early during disease progression (59). In our work, fibronectin disassembly occurred during the transition to outgrowth, and preventing MMP-mediated degradation of fibronectin may provide a better strategy to maintain dormancy and prevent reactivation. Together, this suggests that the dynamic control of fibronectin secretion/assembly and degradation may be a prerequisite for metastasis via promoting survival and subsequent outgrowth of dormant disseminated cells. Fibronectin expression, assembly, and degradation have all been featured as critical components of drug resistance and metastasis: MAPK and BRAF inhibitors can promote fibronectin production to promote drug resistance (60, 61); serum starvation induces ECM secretion (62); and hypoxia stimulates matrix remodeling and ensuing drug resistance (63). Fibronectin, specifically, prevents serum deprivation–induced apoptosis via MEK1 and ERK activation (64), promotes proliferation (65), and permits survival of growth-arrested cells through α5β1 integrin (66, 67), all in agreement with our findings.
We uncovered a mechanism by which dynamic fibronectin assembly and disassembly regulate breast cancer cell dormancy, which could be targeted to eliminate dormant cells or prevent their reactivation. Treatment regimens for eliminating dormant cells are difficult due to the stochastic nature of reactivation and the extremely long time before relapse (68); however, several treatment regimens have been proposed (68–71). One camp argues that since these dormant cells are difficult to find and treat, they could be reactivated and sensitized to chemotherapy. This approach obviously comes with risk, as a patient would have awakened dormant cells that could be drug resistant. Another camp promotes a regimen that would keep cells in a dormant state, but this could be costly, lengthy, and unnecessary if a patient does not have micrometastases. A more exciting possibility is the recent revelation that dormant cells may in fact be sensitized to chemotherapy in an ECM-dependent manner (5, 72). This agrees with our suggestion that targeting survival signaling from cell-ECM adhesion could be a valuable treatment option. There is promising preclinical evidence of efficacy of cilengitide as an antimetastatic drug (73–75), and cotargeting dormant cells with cilengitide and chemotherapy may prevent metastatic outgrowth by eliminating dormant cells at the minimal residual disease stage.
METHODS
Breast cancer cell culture
All cells were cultured at 37°C and with 5% CO2, unless otherwise noted. All cell culture supplies were purchased from Thermo Fisher Scientific (Waltham, MA). AU565, BT474, HCC 1395, HCC 1419, HCC 1428, HCC 1806, HCC 1954, HCC 202, HCC 38, HCC 70, and ZR-75-1 were cultured in RPMI supplemented with 10% fetal bovine serum (FBS) and 1% penicillin/streptomycin (P/S). BT549, Hs578T, MCF7, MDA-MB-231, MDA-MB-468, MDA-MB-231 BoM (bone tropic), MDA-MB-231 BrM2a (brain tropic), MDA-MB-231 LM2 (lung tropic), and SkBr3 were cultured in Dulbecco’s modified Eagle’s medium with 10% FBS and 1% P/S. MDA-MB-175 was cultured in Leibovitz’s L-15 medium with 10% FBS and 1% P/S without supplemental CO2, and MDA-MB-134 and MDA-MB-361 were cultured in Leibovitz’s L-15 medium with 20% FBS and 1% P/S without supplemental CO2. Tropic variants were a gift from J. Massagué (76–78); MDA-MB-231 was provided by S. Smith-Schneider; BT549, MCF7, and SkBr3 were provided by S. Hughes; and all others were provided by M. Niepel.
Biomaterial preparation
Glass coverslips (5, 15, and 18 mm) and poly(ethylene glycol) (PEG)–phosphorylcholine hydrogels were prepared as previously described (18, 19). Briefly, coverslips (Thermo Fisher Scientific) were ultraviolet (UV)-ozone treated and silanized through vapor phase deposition of 3-aminopropyltriethoxysilane (Sigma-Aldrich) at 90°C for a minimum of 18 hours. The coverslips were rinsed sequentially in toluene (Thermo Fisher Scientific), 95% ethanol (Pharmco-Aaper, Brookfield, CT), and water and dried at 90°C for 1 hour. They were then functionalized with 10 g/liter N,N′-disuccinimidyl carbonate (Sigma-Aldrich) and 5% (v/v) diisopropylethylamine (Sigma-Aldrich) in acetone (Thermo Fisher Scientific) at room temperature for 2 hours. Coverslips were rinsed three times in acetone and air-dried. ECM proteins (collagen I and natural mouse laminin were purchased from Life Technologies; human plasma fibronectin from Millipore; human collagen IV from Sigma-Aldrich; recombinant human tenascin C, osteopontin, thrombospondin-1, and vitronectin from R&D Systems; and laminin 511 and laminin 521 from BioLamina) were covalently bound to the glass surface by incubation at room temperature for 3 hours and then with methacrylate-PEG-amine [MA(PEG)] (10 mg/cm2) (Thermo Fisher Scientific) for 2 hours to block nonspecific protein adsorption, rinsed three times in phosphate-buffered saline (PBS), and UV-sterilized before cell seeding. Functionalized coverslips were placed into tissue culture plates that were coated with polyHEMA (100 μg/cm2) to block nonspecific cell adhesion.
For experiments on TCPS, TCPS wells were coated with serum-containing medium at 37°C for at least 1 hour before cell seeding to facilitate cell adhesion. ECM proteins were used at 2 μg/cm2 unless otherwise noted. The Human Protein Atlas (79) was used to determine the composition of integrin-binding ECM proteins in human bone marrow, which primarily includes collagens, fibronectin, and laminins (80). We created a minimalist representation of bone marrow ECM that contains proteins known to bind to cancer cells (18), composed of 50% collagen I, 15% laminin 521, 12% fibronectin, 8% tenascin C, 8% osteopontin, 5% laminin 511, and 2% vitronectin by weight. Collagen I and natural mouse laminin were purchased from Thermo Fisher Scientific (Carlsbad, CA); human plasma fibronectin from Millipore (Billerica, MA); human collagen IV from Sigma-Aldrich (St. Louis, MO); recombinant human tenascin C, osteopontin, thrombospondin-1, and vitronectin from R&D Systems (Minneapolis, MN); and laminin 511 and laminin 521 from BioLamina (Matawan, NJ).
Establishment of dormant cell cultures
Breast cancer cells were seeded onto biomaterials in serum-free medium using the specified culture medium for each cell line. For 7-day experiments on different ECM proteins, protein concentrations, and hydrogels in Fig. 1A and fig. S1, cells were seeded at 11,000 cells/cm2. For all other experiments, cells were seeded at 47,000 cells/cm2 to extend the possible duration. Serum-free medium was changed every 2 to 3 days for the duration of the experiment. At specified time points, cells were changed to serum-containing medium to grow a recovered population. Recovery was assessed after 7 days of growth.
In cases where pharmacological inhibitors were used, inhibitor was replenished with every regular medium change. Concentrations of inhibitors and antibodies were chosen empirically to not affect initial seeding density. Where noted, inhibitors or antibodies were included in the serum-free or serum-containing medium at the following concentrations: E64 (Tocris; 5 μM), ERK inhibitor FR180204 (Sigma-Aldrich; 20 μM), FAK inhibitor 14 (Sigma-Aldrich; 10 μM), soluble fibronectin (Millipore; 10 μg/ml), anti-α5 AF1864 (R&D Systems; 1 μg/ml), cilengitide (Apex Biotechnology; 100 μM), anti-β1 MAB17781 (R&D Systems; 1 μg/ml), MEK inhibitor PD0325901 (Sigma-Aldrich; 10 μM), pan-MMP inhibitor GM6001 (Millipore; 25 μM), ROCK inhibitor Y-27632, (Millipore; 0.1, 1, and 10 μM), pan-TGFβ AB-100-NA (R&D Systems; 20 μg/ml), anti-TGFBR1, LY-364947 (Sigma-Aldrich; 5 μM).
Where noted in specific experiments, medium was supplemented with EGF (R&D Systems, Minneapolis, MN; 1 ng/ml), fibroblast growth factor 1 (FGF1; R&D Systems; 100 ng/ml), insulin-like growth factor 1 (R&D Systems; 100 ng/ml), hepatocyte growth factor (R&D Systems; 100 ng/ml), TGFβ1 (Sigma-Aldrich, St. Louis, MO; 1 ng/ml), SDF1α ( stromal cell-derived factor 1 α) (R&D Systems; 100 ng/ml), or conditioned medium collected from mesenchymal stem cells to stimulate reactivation and growth. Where noted, medium was supplemented with a growth factor cocktail for recovery EGF (R&D Systems; 100 ng/ml), FGF1 (R&D Systems; 100 ng/ml), and TGFβ1 (R&D Systems; 100 ng/ml). In addition, TGFβ2 (Sigma-Aldrich; 2 ng/ml) or TGFβ1 (Sigma-Aldrich; 1 ng/ml) was supplemented in serum-free medium.
Characterization and viability of dormant cell cultures
Viability was assessed after 8 weeks of culture by staining with 4 μM ethidium homodimer-1 and 2 μM calcein AM (Thermo Fisher Scientific). Any condition where at least one viable cell was identified was considered positive for the presence of viable cells. Proliferation was assessed with immunofluorescence for Ki67, G1/S arrest by immunofluorescence for p21, and senescence by senescence-associated β-galactosidase staining (Sigma-Aldrich). Immunofluorescence was performed according to standard protocols, and imaging was performed using a Zeiss Axio Observer Z1 with color and monochrome cameras or a Zeiss Spinning Disc Cell Observer SD (Zeiss, Oberkochen, Germany). The following primary antibodies were used for immunofluorescence: BrdU (ab8039, Abcam; 2 μg/ml), collagen I (ab6308, Abcam; 1:200), EdU (Click-iT EdU, Life Technologies; per the manufacturer’s protocol), phosphor Thr202/Tyr204 ERK (no. 4370, Cell Signaling; 1:200), fibronectin (no. 563100, BD Biosciences; 1:200), Ki67 (ab16667, Abcam; 1:200), pan-laminin (ab11575, Abcam; 1:100), osteopontin (ab8448, Abcam; 1:1000), phosphor Thr180/Tyr182 p38 (no. 4511, Cell Signaling; 1:800), p21 (ab7093, Abcam; 1:100), vitronectin (ab13413, Abcam; 1 μg/ml).
BrdU and EdU incorporation and staining
BrdU (10 μM; Thermo Fisher Scientific) was dosed for 3 days in serum-free medium for 72 hours before the day 28 endpoint. At day 28, the BrdU-containing medium was removed; cells were washed once in serum-free medium and then stimulated with serum-containing or serum-free medium containing 10 μM EdU (Thermo Fisher Scientific). Cells were fixed after an additional 72 hours or 7 days of culture, with regular medium changes. Cells were permeabilized in TBS-T (tris-buffered saline plus triton-X 100), and DNA was denatured with 1 M HCl (10 min, on ice), 2 M HCL (10 min, room temperature), and phosphate-citric acid buffer (10 min, room temperature). Then, staining for EdU was performed according to the manufacturer’s protocol (Life Technologies), and subsequently, BrdU staining was performed using antibody labeling (Abcam, ab8039; 2 μg/ml).
Decellularized ECMs
Decellularized ECMs were generated from dormant HCC 1954 cell cultures (originally seeded on collagen I–functionalized glass coverslips at 47,000 cells/cm2 in serum-free culture for 28 days) according to a published protocol (81). Briefly, cells were extracted with warm PBS containing 0.5% Triton X-100 (Thermo Fisher Scientific) and 20 mM NH4OH (Thermo Fisher Scientific), added dropwise, and incubated at 37°C for 10 min. Twice the volume, PBS was then added, matrices stored at 4°C overnight, and washed carefully with PBS three times. Decellularized ECMs were created and stored hydrated at 4°C for up to 1 month before use. Decellularized ECMs were transferred to new well plates and rinsed once each in PBS and serum-free medium before use.
Statistical analysis
Statistical analysis was performed using Prism v6.0b. Data are reported as means ± SE. Statistical significance was evaluated using a one-way analysis of variance, followed by a Tukey’s posttest for pairwise comparisons. For Kaplan-Meier survival analysis, significance was determined using a log-rank (Mantel-Cox) test. P < 0.05 is denoted with *, P ≤ 0.01 with **, P ≤ 0.001 with ***, P and ≤ 0.0001 with ****; P ≥ 0.05 is considered not significant (“ns”).
Supplementary Material
Acknowledgments
We thank L. Jansen, D. J. Jerry, and M. Niepel for helpful discussions and L. Jansen for providing a MATLAB code for quantification of cell number and the human bone marrow ECM analysis. We thank J. Massagué, S. Hughes, S. Smith-Schneider, and M. Niepel for providing cell lines and E. Cukierman and S. Polio for assistance with the decellularization protocol. Mass spectral data were acquired at the University of Massachusetts Mass Spectrometry Core Facility, and we thank S. Eyles for assistance with sample preparation and data acquisition. Funding: This work was funded by an NSF-NCI award DMR-1234852 to S.R.P. and a grant from the NIH (1DP2CA186573-01). S.R.P. is a Pew Biomedical Scholar supported by the Pew Charitable Trusts and was supported by a Barry and Afsaneh Siadat faculty award. L.E.B. was partially supported by National Research Service Award T32 GM008515 from the National Institutes of Health. A.D.S. was supported by a National Science Foundation Graduate Research Fellowship (1451512). A.N.P. was supported by the Cell and Tissue Engineering NIH Biotechnology Training Grant (T32-GM008433), and M.O.P. was supported by a donation from the Giglio Family to the Wallace H. Coulter Department of Biomedical Engineering. A.M.M. was supported by NCI R01 CA168464 and 203439. Author contributions: L.E.B. and S.R.P. conceived the project and wrote the manuscript. L.E.B., M.O.P., A.M.M., and S.R.P. designed research. L.E.B., C.L.H., A.D.S., A.N.P., C.S., and S.G. performed experiments. All authors discussed the results and revised the manuscript. Competing interests: The authors declare that they have no competing interests. Data and materials availability: All data needed to evaluate the conclusions in the paper are present in the paper and/or the Supplementary Materials. Additional data related to this paper may be requested from the authors.
SUPPLEMENTARY MATERIALS
Supplementary material for this article is available at http://advances.sciencemag.org/cgi/content/full/6/11/eaaz4157/DC1
Supplemental Methods
Fig. S1. Heat map of percent decrease in confluence and viability for bottom performing cell lines.
Fig. S2. Survival is maximized on collagen I coverslips.
Fig. S3. Serum-starved cells are cell cycle arrested and nonproliferative.
Fig. S4. Proteomic of ECM produced by HCC 1954 during serum starvation and recovery.
Fig. S5. Dormant cells organize fibronectin.
Fig. S6. Fibronectin is locally degraded during reactivation via MMPs.
Fig. S7. Integrin expression of dormant cells determined by quantitative polymerase chain reaction.
Fig. S8. ERK mediates survival in other cell lines.
Table S1. Inhibitors and activators used in experiments.
Table S2. Antibodies used for immunofluorescence.
Table S3. Integrin and CDKN primers.
Movie S1. Rare cells divide after 4 weeks of serum-free culture.
REFERENCES AND NOTES
- 1.Braun S., Pantel K., Müller P., Janni W., Hepp F., Kentenich C. R., Gastroph S., Wischnik A., Dimpfl T., Kindermann G., Riethmuller G., Schlimok G., Cytokeratin-positive cells in the bone marrow and survival of patients with stage I, II, or III breast cancer. N. Engl. J. Med. 342, 525–533 (2000). [DOI] [PubMed] [Google Scholar]
- 2.Braun S., Vogl F. D., Naume B., Janni W., Osborne M. P., Coombes R. C., Schlimok G., Diel I. J., Gerber B., Gebauer G., Pierga J. Y., Marth C., Oruzio D., Wiedswang G., Solomayer E. F., Kundt G., Strobl B., Fehm T., Wong G. Y., Bliss J., Vincent-Salomon A., Pantel K., A pooled analysis of bone marrow micrometastasis in breast cancer. N. Engl. J. Med. 353, 793–802 (2005). [DOI] [PubMed] [Google Scholar]
- 3.Luzzi K. J., MacDonald I. C., Schmidt E. E., Kerkvliet N., Morris V. L., Chambers A. F., Groom A. C., Multistep nature of metastatic inefficiency. Am. J. Pathol. 153, 865–873 (1998). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ghajar C. M., Peinado H., Mori H., Matei I. R., Evason K. J., Brazier H., Almeida D., Koller A., Hajjar K. A., Stainier D. Y., Chen E. I., Lyden D., Bissell M. J., The perivascular niche regulates breast tumour dormancy. Nat. Cell Biol. 15, 807–817 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boyerinas B., Zafrir M., Yesilkanal A. E., Price T. T., Hyjek E. M., Sipkins D. A., Adhesion to osteopontin in the bone marrow niche regulates lymphoblastic leukemia cell dormancy. Blood 121, 4821–4831 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barkan D., El Touny L. H., Michalowski A. M., Smith J. A., Chu I., Davis A. S., Webster J. D., Hoover S., Simpson R. M., Gauldie J., Green J. E., Metastatic growth from dormant cells induced by a col-I-enriched fibrotic environment. Cancer Res. 70, 5706–5716 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barkan D., Kleinman H., Simmons J. L., Asmussen H., Kamaraju A. K., Hoenorhoff M. J., Liu Z. Y., Costes S. V., Cho E. H., Lockett S., Khanna C., Chambers A. F., Green J. E., Inhibition of metastatic outgrowth from single dormant tumor cells by targeting the cytoskeleton. Cancer Res. 68, 6241–6250 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gao H., Chakraborty G., Zhang Z., Akalay I., Gadiya M., Gao Y., Sinha S., Hu J., Jiang C., Akram M., Brogi E., Leitinger B., Giancotti F. G., Multi-organ site metastatic reactivation mediated by non-canonical discoidin domain receptor 1 signaling. Cell 166, 47–62 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schrader J., Gordon-Walker T. T., Aucott R. L., van Deemter M., Quaas A., Walsh S., Benten D., Forbes S. J., Wells R. G., Iredale J. P., Matrix stiffness modulates proliferation, chemotherapeutic response, and dormancy in hepatocellular carcinoma cells. Hepatology 53, 1192–1205 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kaplan R. N., Riba R. D., Zacharoulis S., Bramley A. H., Vincent L., Costa C., MacDonald D. D., Jin D. K., Shido K., Kerns S. A., Zhu Z., Hicklin D., Wu Y., Port J. L., Altorki N., Port E. R., Ruggero D., Shmelkov S. V., Jensen K. K., Rafii S., Lyden D., VEGFR1-positive haematopoietic bone marrow progenitors initiate the pre-metastatic niche. Nature 438, 820–827 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Malanchi I., Santamaria-Martínez A., Susanto E., Peng H., Lehr H.-A., Delaloye J.-F., Huelsken J., Interactions between cancer stem cells and their niche govern metastatic colonization. Nature 481, 85–89 (2012). [DOI] [PubMed] [Google Scholar]
- 12.Oskarsson T., Acharyya S., Zhang X. H.-F., Vanharanta S., Tavazoie S. F., Morris P. G., Downey R. J., Manova-Todorova K., Brogi E., Massagué J., Breast cancer cells produce tenascin C as a metastatic niche component to colonize the lungs. Nat. Med. 17, 867–874 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Malladi S., Macalinao D. G., Jin X., He L., Basnet H., Zou Y., de Stanchina E., Massagué J., Metastatic latency and immune evasion through autocrine inhibition of WNT. Cell 165, 45–60 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Albrengues J., Shields M. A., Ng D., Park C. G., Ambrico A., Poindexter M. E., Upadhyay P., Uyeminami D. L., Pommier A., Kuttner V., Bruzas E., Maiorino L., Bautista C., Carmona E. M., Gimotty P. A., Fearon D. T., Chang K., Lyons S. K., Pinkerton K. E., Trotman L. C., Goldberg M. S., Yeh J. T.-H., Egeblad M., Neutrophil extracellular traps produced during inflammation awaken dormant cancer cells in mice. Science 361, eaao4227 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lawson M. A., McDonald M. M., Kovacic N., Hua Khoo W., Terry R. L., Down J., Kaplan W., Paton-Hough J., Fellows C., Pettitt J. A., Neil Dear T., Van Valckenborgh E., Baldock P. A., Rogers M. J., Eaton C. L., Vanderkerken K., Pettit A. R., Quinn J. M. W., Zannettino A. C. W., Phan T. G., Croucher P. I., Osteoclasts control reactivation of dormant myeloma cells by remodelling the endosteal niche. Nat. Commun. 6, 8983 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Price T. T., Burness M. L., Sivan A., Warner M. J., Cheng R., Lee C. H., Olivere L., Comatas K., Magnani J., Lyerly H. K., Cheng Q., McCall C. M., Sipkins D. A., Dormant breast cancer micrometastases reside in specific bone marrow niches that regulate their transit to and from bone. Sci. Transl. Med. 8, 340ra73 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gao H., Chakraborty G., Lee-Lim A. P., Mavrakis K. J., Wendel H.-G., Giancotti F. G., Forward genetic screens in mice uncover mediators and suppressors of metastatic reactivation. Proc. Natl. Acad. Sci. U.S.A. 111, 16532–16537 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barney L. E., Dandley E. C., Jansen L. E., Reich N. G., Mercurio A. M., Peyton S. R., A cell-ECM screening method to predict breast cancer metastasis. Integr. Biol. 7, 198–212 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Herrick W. G., Nguyen T. V., Sleiman M., McRae S., Emrick T. S., Peyton S. R., PEG-phosphorylcholine hydrogels as tunable and versatile platforms for mechanobiology. Biomacromolecules 14, 2294–2304 (2013). [DOI] [PubMed] [Google Scholar]
- 20.Goss P. E., Chambers A. F., Does tumour dormancy offer a therapeutic target? Nat. Rev. Cancer 10, 871–877 (2010). [DOI] [PubMed] [Google Scholar]
- 21.Bragado P., Estrada Y., Parikh F., Krause S., Capobianco C., Farina H. G., Schewe D. M., Aguirre-Ghiso J. A., TGF-β2 dictates disseminated tumour cell fate in target organs through TGF-β-RIII and p38α/β signalling. Nat. Cell Biol. 15, 1351–1361 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Muranen T., Iwanicki M. P., Curry N. L., Hwang J., DuBois C. D., Coloff J. L., Hitchcock D. S., Clish C. B., Brugge J. S., Kalaany N. Y., Starved epithelial cells uptake extracellular matrix for survival. Nat. Commun. 8, 13989 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Danen E. H. J., Sonneveld P., Brakebusch C., Fassler R., Sonnenberg A., The fibronectin-binding integrins α5β1 and αvβ3 differentially modulate RhoA-GTP loading, organization of cell matrix adhesions, and fibronectin fibrillogenesis. J. Cell Biol. 129, 1071–1086 (2002). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ilić D., Kovacic B., Johkura K., Schlaepfer D. D., Tomasevic N., Han Q., Kim J. B., Howerton K., Baumbusch C., Ogiwara N., Streblow D. N., Nelson J. A., Dazin P., Shino Y., Sasaki K., Damsky C. H., FAK promotes organization of fibronectin matrix and fibrillar adhesions. J. Cell Sci. 117, 177–187 (2004). [DOI] [PubMed] [Google Scholar]
- 25.Carraher C. L., Schwarzbauer J. E., Regulation of matrix assembly through rigidity-dependent fibronectin conformational changes. J. Biol. Chem. 288, 14805–14814 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wierzbicka-Patynowski I., Schwarzbauer J. E., The ins and outs of fibronectin matrix assembly. J. Cell Sci. 116( Pt 16), 3269–3276 (2003). [DOI] [PubMed] [Google Scholar]
- 27.Eisele G., Wick A., Eisele A. C., Clement P. M., Tonn J., Tabatabai G., Ochsenbein A., Schlegel U., Neyns B., Krex D., Simon M., Nikkhah G., Picard M., Stupp R., Wick W., Weller M., Cilengitide treatment of newly diagnosed glioblastoma patients does not alter patterns of progression. J. Neuro-Oncol. 117, 141–145 (2014). [DOI] [PubMed] [Google Scholar]
- 28.Davis G., Affinity of integrins for damaged extracellular matrix: αvβ3 binds to denatured collagen type I through RGD sites. Biochem. Biophys. Res. Commun. 182, 1025–1031 (1992). [DOI] [PubMed] [Google Scholar]
- 29.Zhang X. H.-F., Wang Q., Gerald W., Hudis C. A., Norton L., Smid M., Foekens J. A., Massague J., Latent bone metastasis in breast cancer tied to Src-dependent survival signals. Cancer Cell 16, 67–78 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hofstetter C. P., Burkhardt J. K., Shin B. J., Gursel D. B., Mubita L., Gorrepati R., Brennan C., Holland E. C., Boockvar J. A., Protein phosphatase 2A mediates dormancy of glioblastoma multiforme-derived tumor stem-like cells during hypoxia. PLOS ONE 7, e30059 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Caino M. C., Chae Y. C., Vaira V., Ferrero S., Nosotti M., Martin N. M., Weeraratna A., O'Connell M., Jernigan D., Fatatis A., Languino L. R., Bosari S., Altieri D. C., Metabolic stress regulates cytoskeletal dynamics and metastasis of cancer cells. J. Clin. Invest. 123, 2907–2920 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Endo H., Okami J., Okuyama H., Nishizawa Y., Imamura F., Inoue M., The induction of MIG6 under hypoxic conditions is critical for dormancy in primary cultured lung cancer cells with activating EGFR mutations. Oncogene 36, 2824–2834 (2016). [DOI] [PubMed] [Google Scholar]
- 33.Fluegen G., Avivar-Valderas A., Wang Y., Padgen M. R., Williams J. K., Nobre A. R., Calvo V., Cheung J. F., Bravo-Cordero J. J., Entenberg D., Castracane J., Verkhusha V., Keely P. J., Condeelis J., Aguirre-Ghiso J. A., Phenotypic heterogeneity of disseminated tumour cells is preset by primary tumour hypoxic microenvironments. Nat. Cell Biol. 19, 120–132 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kim R. S., Avivar-Valderas A., Estrada Y., Bragado P., Sosa M. S., Aguirre-Ghiso J. A., Segall J. E., Dormancy signatures and metastasis in estrogen receptor positive and negative breast cancer. PLOS ONE 7, e35569 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Roca-Cusachs P., Gauthier N. C., del Rio A., Sheetz M. P., Clustering of 5 1 integrins determines adhesion strength whereas v 3 and talin enable mechanotransduction. Proc. Natl. Acad. Sci. U.S.A. 106, 16245–16250 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Marlow R., Honeth G., Lombardi S., Cariati M., Hessey S., Pipili A., Mariotti V., Buchupalli B., Foster K., Bonnet D., Grigoriadis A., Rameshwar P., Purushotham A., Tutt A., Dontu G., A novel model of dormancy for bone metastatic breast cancer cells. Cancer Res. 73, 6886–6899 (2013). [DOI] [PubMed] [Google Scholar]
- 37.Wheeler S. E., Clark A. M., Taylor D. P., Young C. L., Pillai V. C., Stolz D. B., Venkataramanan R., Lauffenburger D., Griffith L., Wells A., Spontaneous dormancy of metastatic breast cancer cells in an all human liver microphysiologic system. Br. J. Cancer 111, 2342–2350 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gao H., Chakraborty G., Lee-Lim A. P., Mo Q., Decker M., Vonica A., Shen R., Brogi E., Brivanlou A. H., Giancotti F. G., The BMP inhibitor Coco reactivates breast cancer cells at lung metastatic sites. Cell 150, 764–779 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shibue T., Weinberg R. A., Integrin b1-focal adhesion kinase signaling directs the proliferation of metastatic cancer cells disseminated in the lungs. Proc. Natl. Acad. Sci. U.S.A. 106, 14734 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shibue T., Brooks M. W., Inan M. F., Reinhardt F., Weinberg R. A., The outgrowth of micrometastases is enabled by the formation of filopodium-like protrusions. Cancer Discov. 2, 706–721 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shibue T., Brooks M. W., Weinberg R. A., An integrin-linked machinery of cytoskeletal regulation that enables experimental tumor initiation and metastatic colonization. Cancer Cell 24, 481–498 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Li S., Kennedy M., Payne S., Kennedy K., Seewaldt V. L., Pizzo S. V., Bachelder R. E., Model of tumor dormancy/recurrence after short-term chemotherapy. PLOS ONE 9, e98021 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sharma S. V., Lee D. Y., Li B., Quinlan M. P., Takahashi F., Maheswaran S., McDermott U., Azizian N., Zou L., Fischbach M. A., Wong K. K., Brandstetter K., Wittner B., Ramaswamy S., Classon M., Settleman J., A chromatin-mediated reversible drug-tolerant state in cancer cell subpopulations. Cell 141, 69–80 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Aguirre-Ghiso J. A., Models, mechanisms and clinical evidence for cancer dormancy. Nat. Rev. Cancer 7, 834–846 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pelham R. J. Jr., Wang Y.-l., High resolution detection of mechanical forces exerted by locomoting fibroblasts on the substrate. Mol. Biol. Cell 10, 935–945 (1999). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Genes N. G., Rowley J. A., Mooney D. J., Bonassar L. J., Effect of substrate mechanics on chondrocyte adhesion to modified alginate surfaces. Arch. Biochem. Biophys. 422, 161–167 (2004). [DOI] [PubMed] [Google Scholar]
- 47.Zaman M. H., Kamm R. D., Matsudaira P., Lauffenburger D. A., Computational model for cell migration in three-dimensional matrices. Biophys. J. 89, 1389–1397 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Balaban N. Q., Schwarz U. S., Riveline D., Goichberg P., Tzur G., Sabanay I., Mahalu D., Safran S., Bershadsky A., Addadi L., Geiger B., Force and focal adhesion assembly: A close relationship studied using elastic micropatterned substrates. Nat. Cell Biol. 3, 466–472 (2001). [DOI] [PubMed] [Google Scholar]
- 49.Grinnell F., Ho C.-H., Transforming growth factor β stimulates fibroblast-collagen matrix contraction by different mechanisms in mechanically loaded and unloaded matrices. Exp. Cell Res. 273, 248–255 (2002). [DOI] [PubMed] [Google Scholar]
- 50.Gilbert L. A., Hemann M. T., DNA damage-mediated induction of a chemoresistant niche. Cell 143, 355–366 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Franco-Barraza J., Francescone R., Luong T., Shah N., Madhani R., Cukierman G., Dulaimi E., Devarajan K., Egleston B. L., Nicolas E., Katherine Alpaugh R., Malik R., Uzzo R. G., Hoffman J. P., Golemis E. A., Cukierman E., Matrix-regulated integrin αvβ5 maintains α5β1-dependent desmoplastic traits prognostic of neoplastic recurrence. eLife 6, e20600 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ventura E., Weller M., Macnair W., Eschbach K., Beisel C., Cordazzo C., Claassen M., Zardi L., Burghardt I., TGF-β induces oncofetal fibronectin that, in turn, modulates TGF-β superfamily signaling in endothelial cells. J. Cell Sci. 131, jcs209619 (2018). [DOI] [PubMed] [Google Scholar]
- 53.Cockerill M., Rigozzi M. K., Terentjev E. M., Mechanosensitivity of the 2nd kind: TGF-β mechanism of cell sensing the substrate stiffness. PLOS ONE 10, e0139959 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Oshimori N., Oristian D., Fuchs E., TGF-β promotes heterogeneity and drug resistance in squamous cell carcinoma. Cell 160, 963–976 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yumoto K., Eber M. R., Wang J., Cackowski F. C., Decker A. M., Lee E., Nobre A. R., Aguirre-Ghiso J. A., Jung Y., Taichman R. S., Axl is required for TGF-β2-induced dormancy of prostate cancer cells in the bone marrow. Sci. Rep. 6, 36520 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hoare M., Ito Y., Kang T. W., Weekes M. P., Matheson N. J., Patten D. A., Shetty S., Parry A. J., Menon S., Salama R., Antrobus R., Tomimatsu K., Howat W., Lehner P. J., Zender L., Narita M., NOTCH1 mediates a switch between two distinct secretomes during senescence. Nat. Cell Biol. 18, 979–992 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.de Gramont A., Faivre S., Raymond E., Novel TGF-β inhibitors ready for prime time in onco-immunology. Oncoimmunology 6, e1257453 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cook L. M., Araujo A., Pow-Sang J. M., Budzevich M. M., Basanta D., Lynch C. C., Predictive computational modeling to define effective treatment strategies for bone metastatic prostate cancer. Sci. Rep. 6, 29384 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Harper K. L., Sosa M. S., Entenberg D., Hosseini H., Cheung J. F., Nobre R., Avivar-Valderas A., Nagi C., Girnius N., Davis R. J., Farias E. F., Condeelis J., Klein C. A., Aguirre-Ghiso J. A., Mechanism of early dissemination and metastasis in Her2+ mammary cancer. Nature 540, 588–592 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Afasizheva A., Devine A., Tillman H., Fung K. L., Vieira W. D., Blehm B. H., Kotobuki Y., Busby B., Chen E. I., Tanner K., Mitogen-activated protein kinase signaling causes malignant melanoma cells to differentially alter extracellular matrix biosynthesis to promote cell survival. BMC Cancer 16, 186 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Fedorenko I. V., Abel E. V., Koomen J. M., Fang B., Wood E. R., Chen Y. A., Fisher K. J., Iyengar S., Dahlman K. B., Wargo J. A., Flaherty K. T., Sosman J. A., Sondak V. K., Messina J. L., Gibney G. T., Smalley K. S. M., Fibronectin induction abrogates the BRAF inhibitor response of BRAF V600E/PTEN-null melanoma cells. Oncogene 35, 1225–1235 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Leicht M., Briest W., Hölzl A., ZImmer H.-G., Serum depletion induces cell loss of rat cardiac fibroblasts and increased expression of extracellular matrix proteins in surviving cells. Cardiovasc. Res. 52, 429–437 (2001). [DOI] [PubMed] [Google Scholar]
- 63.Constantinides G., Kalcioglu Z. I., McFarland M., Smith J. F., Van Vliet K. J., Probing mechanical properties of fully hydrated gels and biological tissues. J. Biomech. 41, 3285–3289 (2008). [DOI] [PubMed] [Google Scholar]
- 64.Gu J., Fujibayashi A., Yamada K. M., Sekiguchi K., Laminin-10/11 and fibronectin differentially prevent apoptosis induced by serum removal via phosphatidylinositol 3-kinase/Akt- and MEK1/ERK-dependent pathways. J. Biol. Chem. 277, 19922–19928 (2002). [DOI] [PubMed] [Google Scholar]
- 65.Fringer J., Grinnell F., Fibroblast quiescence in floating or released collagen matrices: Contribution of the ERK signaling pathway and actin cytoskeletal organization. J. Biol. Chem. 276, 31047–31052 (2001). [DOI] [PubMed] [Google Scholar]
- 66.Korah B. M., Integrin α5β1 promotes survival of growth-arrested breast cancer cells. Cancer Res. 64, 4514–4522 (2004). [DOI] [PubMed] [Google Scholar]
- 67.Zhang Z., Vuori K., Reed J. C., Ruoslahti E., The alpha 5 beta 1 integrin supports survival of cells on fibronectin and up-regulates Bcl-2 expression. Proc. Natl. Acad. Sci. U.S.A. 92, 6161–6165 (1995). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Giancotti F. G., Mechanisms governing metastatic dormancy and reactivation. Cell 155, 750–764 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Aguirre-Ghiso J. A., The problem of cancer dormancy: Understanding the basic mechanisms and identifying therapeutic opportunities. Cell Cycle 5, 1740–1743 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Davis G. E., Bayless K. J., Mavila A., Molecular basis of endothelial cell morphogenesis in three-dimensional extracellular matrices. Anat. Rec. 268, 252–275 (2002). [DOI] [PubMed] [Google Scholar]
- 71.Barney L. E., Jansen L. E., Polio S. R., Galarza S., Lynch M. E., Peyton S. R., The predictive link between matrix and metastasis. Curr. Opin. Chem. Eng. 11, 85–93 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Carlson P., Dasgupta A., Grzelak C. A., Kim J., Barrett A., Coleman I. M., Shor R. E., Goddard E. T., Dai J., Schweitzer E. M., Lim A. R., Crist S. B., Cheresh D. A., Nelson P. S., Hansen K. C., Ghajar C. M., Targeting the perivascular niche sensitizes disseminated tumour cells to chemotherapy. Nat. Cell Biol. 21, 238–250 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Dembo M., Wang Y.-L., Stresses at the cell-to-substrate interface during locomotion of fibroblasts. Biophys. J. 76, 2307–2316 (1999). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bäuerle T., Komljenovic D., Merz M., Berger M. R., Goodman S. L., Semmler W., Cilengitide inhibits progression of experimental breast cancer bone metastases as imaged noninvasively using VCT, MRI and DCE-MRI in a longitudinal in vivo study. Int. J. Cancer 128, 2453–2462 (2011). [DOI] [PubMed] [Google Scholar]
- 75.Bretschi M., Cheng C., Witt H., Dimitrakopoulou-Strauss A., Strauss L. G., Semmler W., Bäuerle T., Cilengitide affects tumor compartment, vascularization and microenvironment in experimental bone metastases as shown by longitudinal 18F-FDG PET and gene expression analysis. J. Cancer Res. Clin. Oncol. 139, 573–583 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bos P. D., Zhang X. H.-F., Nadal C., Shu W., Gomis R. R., Nguyen D. X., Minn A. J., van de Vijver M. J., Gerald W. L., Foekens J. A., Massagué J., Genes that mediate breast cancer metastasis to the brain. Nature 459, 1005–1009 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kang Y., Siegel P. M., Shu W., Drobnjak M., Kakonen S. M., Cordón-Cardo C., Guise T. A., Massagué J., A multigenic program mediating breast cancer metastasis to bone. Cancer Cell 3, 537–549 (2003). [DOI] [PubMed] [Google Scholar]
- 78.Minn A. J., Gupta G. P., Siegel P. M., Bos P. D., Shu W., Giri D. D., Viale A., Olshen A. B., Gerald W. L., Massagué J., Genes that mediate breast cancer metastasis to lung. Nature 436, 518–524 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Uhlén M., Fagerberg L., Hallström B. M., Lindskog C., Oksvold P., Mardinoglu A., Sivertsson Å., Kampf C., Sjöstedt E., Asplund A., Olsson I. M., Edlund K., Lundberg E., Navani S., Szigyarto C. A.-K., Odeberg J., Djureinovic D., Takanen J. O., Hober S., Alm T., Edqvist P.-H., Berling H., Tegel H., Mulder J., Rockberg J., Nilsson P., Schwenk J. M., Hamsten M., von Feilitzen K., Forsberg M., Persson L., Johansson F., Zwahlen M., von Heijne G., Nielsen J., Pontén F., Tissue-based map of the human proteome. Science 347, 1260419 (2015). [DOI] [PubMed] [Google Scholar]
- 80.Jansen L. E., McCarthy T., Lee M. J., Peyton S. R., A synthetic, three-dimensional bone marrow hydrogel. Biorxiv, 275842 (2018). [Google Scholar]
- 81.Castelló-Cros R., Cukierman E., Stromagenesis during tumorigenesis: Characterization of tumor-associated fibroblasts and stroma-derived 3D matrices. Methods Mol. Biol. 522, 275–305 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wilder C. L., Park K.-Y., Keegan P. M., Platt M. O., Manipulating substrate and pH in zymography protocols selectively distinguishes cathepsins K, L, S, and V activity in cells and tissues. Arch. Biochem. Biophys. 516, 52–57 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kupai K., Szucs G., Cseh S., Hajdu I., Csonka C., Csont T., Ferdinandy P., Matrix metalloproteinase activity assays: Importance of zymography. J. Pharmacol. Toxicol. Methods 61, 205–209 (2010). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material for this article is available at http://advances.sciencemag.org/cgi/content/full/6/11/eaaz4157/DC1
Supplemental Methods
Fig. S1. Heat map of percent decrease in confluence and viability for bottom performing cell lines.
Fig. S2. Survival is maximized on collagen I coverslips.
Fig. S3. Serum-starved cells are cell cycle arrested and nonproliferative.
Fig. S4. Proteomic of ECM produced by HCC 1954 during serum starvation and recovery.
Fig. S5. Dormant cells organize fibronectin.
Fig. S6. Fibronectin is locally degraded during reactivation via MMPs.
Fig. S7. Integrin expression of dormant cells determined by quantitative polymerase chain reaction.
Fig. S8. ERK mediates survival in other cell lines.
Table S1. Inhibitors and activators used in experiments.
Table S2. Antibodies used for immunofluorescence.
Table S3. Integrin and CDKN primers.
Movie S1. Rare cells divide after 4 weeks of serum-free culture.


