Abstract
Purpose.
Mental health problems are a growing concern on college campuses. Although postsecondary institutions often provide mental health services to students free of charge, it is unclear which students access such treatment and why.
Methods.
This study examined predictors of mental health treatment among college students. 2,280 students completed an online survey to assess demographic variables, mental health symptoms (depression, anxiety), stress and prior/current mental health treatment.
Results.
After accounting for symptom severity, men were less likely to receive treatment for mental health problems and LGBQ students were more likely to receive treatment. That difference was not evident at higher levels of depression and anxiety. Finally, self-reported anxiety but not depressive symptoms predicted being in mental health treatment.
Conclusions.
These findings can help inform efforts to target college students who could benefit from treatment but are not seeking it.
Keywords: college students, mental health, mental health treatment, LGBQ
Introduction
College students experience high levels of stress across academic, social, and financial domains.1–3 Combined with the consistent findings suggesting traditional college age is within the typical age of onset for many mental health disorders, it is unsurprising that mental health disorders are common amongst college students.4–8 Student mental health problems at postsecondary institutions have been associated with a myriad of negative outcomes, such as poor academic performance, lower retention rates, and substance use problems.5,8–15
Given that mental health problems on college campuses are growing and that a majority of adolescents in the United States enroll at postsecondary institutions, it is important to identify students with mental health problems and provide support.16,17 Despite most colleges offer free counseling services to enrolled students, and students report deriving tangible benefits from counseling (e.g., maintaining enrollment, improving academic performance), only a small segment of college students access mental health services.9,16 An online survey of 2,785 students at a large university suggested that about 15% of students experiencing mental health problems had used counseling services or medication the prior year.9 Eisenberg et al18 found that one in three students with mental health problems had received services in the past year, and one in five were receiving services at the time of the study.
The question remains: why are so many students who would benefit from counseling not receiving mental health services? Research has found that students with current panic disorder or generalized anxiety disorder (GAD) are more likely to seek treatment than those who screen positive for depression.9 Further, several demographic variables predict the perceived need for services; being a woman, bisexual, or gay was associated with a greater perceived need for treatment.9 In contrast, students who identify as Asian or Pacific Islander were less likely than White students to perceive a need for treatment.9 Further, men, students from lower socioeconomic backgrounds, international students, and Asian American students are less likely to seek services for mental health concerns relative to their peers.18,19
Stigma is an oft-cited barrier to treatment.20,21 Eisenberg et al21 reported that, amongst a large sample of college students across 13 universities, stigmatized views of mental health were significantly and negatively associated with help-seeking. Other factors, such as a lack of perceived need for treatment and skepticism about effectiveness of treatment may also prevent college students from seeking treatment.9 Lastly, limited resources of college counseling centers (e.g., offering a limited number of counseling sessions to each student) may be a real or perceived barrier.16 Still, even given these limitations of access, a college campus is a rare place in the United States in that most people (students, at least), most of the time, have access to psychological treatment if they want it.16 That is, being a college student in the United States removes some (but certainly not all) barriers to treatment, allowing more of an exploration of what predicts treatment other than access, from demographics to mental health symptomology.
The Current Study
The present study expands what is known about who seeks mental health treatment in college and why. The following three hypotheses were tested. First, we expected that, consistent with extant literature, (H1) students who identify as men, heterosexual, White, or upper or middle SES will have lower mental health burdens. Further, and consistent with the predicted lower mental health burden, we hypothesized that (H2) fewer members of (any of) those same groups will report receiving mental health treatment during college. Finally, we hypothesized (H3) that the reduced mental health burden for students in the above groups will not fully account for the decreased treatment rates for men, heterosexual students, White students, and students who identify as upper or middle SES. Specifically, we predicted that students in those categories would report receiving treatment at a lower rate than would be explained by their lower mental health burden.
Methods
Sample
Participants were recruited from two small liberal arts colleges in the United States. All enrolled undergraduate students received an email invitation to participate in the study, along with two follow-up email invitations sent to those who did not participate within the first few days. The survey took approximately 15 minutes to complete. Data collection occurred over the course of a two-week period in the winter of 2018. Participants were offered the opportunity to enter a raffle with the chance of winning a $50 or $100 Amazon™ gift card. A total of 2,254 participants (51% of the combined enrollment) started the survey, and 2,073 (91.93% of those who started it) completed all study measures, leaving 180 (9.19%) who did not complete at least one measure and were thus excluded (pairwise) from the relevant analysis. Given the relatively small amount of missing data, missing data was not imputed. The institutional review board of the second author’s institution approved the study.
Measures
Demographics.
Participants reported their race/ethnicity, gender, sexual orientation, age, year in college and perceived socioeconomic status. Perceived SES was measured by asking participants whether they believed their families were in the lower, upper, or middle socioeconomic class.22 The majority of students identified as women (n = 1,295; 56.80%), while 39.74% (n = 906) identified as men. The remainder (n = 43; 1.89%) selected a different gender identification. The race and ethnicity of respondents corresponded to those enrolled at both institutions, with only Latino students being overenrolled in the current study. See Table 1 for demographic information by gender.
Table 1.
Demographics by gender
| Men M ± SD M (%) |
Women M ± SD M (%) |
Other gender identity M ± SD M (%) |
All M ± SD M (%) |
|
|---|---|---|---|---|
| Age | 19.96a ± 1.30 | 19.91a ± 1.24 | 20.35b ± 1.07 | 19.94 ± 1.26 |
| Year in college | ||||
| First | 246a (27.15%) | 334a (25.79%) | 8 (15.09%) | 588 (26.09%) |
| Second | 258a (28.48%) | 337a (26.02%) | 15 (28.30%) | 610 (27.06%) |
| Third | 190a (20.97%) | 292a (22.55%) | 16 (30.19%) | 498 (22.09%) |
| Fourth | 212a (23.40%) | 332a (25.64%) | 14 (26.42%) | 558 (24.76%) |
| Perceived socioeconomic status | ||||
| Lower | 95a (10.50%) | 145a (11.20%) | 12b (22.64%) | 252 (11.19%) |
| Middle | 447a (49.39%) | 651a (50.27%) | 28b (52.83%) | 1126 (49.98%) |
| Upper | 363a (40.11%) | 499a (38.53%) | 13b (24.53%) | 875 (38.84%) |
| Orientation | ||||
| Heterosexual | 778a (85.97%) | 1019b (78.69%) | 10c (18.87%) | 1807 (80.20%) |
| Gay/lesbian | 64a (7.07%) | 31b (2.39%) | 8c (15.09%) | 103 (4.57%) |
| Bisexual | 18a (1.99%) | 141b (10.89%) | 6b (11.32%) | 165 (7.32%) |
| Other | 45a (4.97%) | 104b (8.03%) | 29c (54.72%) | 178 (7.90%) |
| Race/ethnicity | ||||
| Latinx | 92a (10.22%) | 118a (9.13%) | 6a (11.76%) | 216 (9.63%) |
| Black | 38a (4.22%) | 52a (4.02%) | 1a (1.96%) | 91 (4.06%) |
| Asian | 79a (8.78%) | 115a (8.90%) | 6a (11.76%) | 200 (8.92%) |
| White | 644a (71.56%) | 910a (70.43%) | 24b (47.06%) | 1578 (70.35%) |
| More than one | 14a (1.56%) | 34a (2.63%) | 2a (3.92%) | 50 (2.23%) |
| Other | 33a (3.67%) | 63a (4.88%) | 12b (23.53%) | 108 (4.81%) |
Values in the same row not sharing a subscript are significantly different at p < .05
Treatment status.
Students were asked if they had received or were receiving mental health treatment while in college. Students were further asked to select (from a pre-populated set of options - stress/trauma, ADHD, Anxiety, depression, eating disorders – with a free-text ‘other’ option) for which issue or issues they received treatment.
Depression, Anxiety and Stress.
The Depression, Anxiety, Stress Scales (DASS-21) short form was used to measure depression, anxiety and stress.23 The measure consists of 21 items, with seven items for each of the three mental health constructs. Items are rated from zero to three, with three being the most intense. Scores for each subscale thus vary from zero to 21. For categorical analysis, scores were grouped based on scorings from Lovibond and Lovibond, with depression, anxiety, and stress split into five categories each, with cutpoints set at < 10 (normal), < 15 (mild), < 21 (moderate), < 27 (severe), and 28+ (extremely severe) for depression.24 Similarly structured cutpoints for anxiety (8, 10, 15, 20) and stress (15, 19, 26, 34) were used.24
Data Analysis Plan
To test H1, one-way ANOVA tests were run, testing whether gender, perceived SES, race, and sexual orientation (separately) had an effect on depression and anxiety as measured by the DASS. This hypothesis would be considered supported if both (a) those relationships were found to be of statistically significant strength, and (b) the differences were in the predicted directions (men, heterosexual, White, and upper or middle SES would have lower mental health burdens).
To test H2, a series of χ2 analyses of the relationships between each of gender, perceived SES, race/ethnicity, and sexual orientation, and self-report of receiving treatment while in college. This hypothesis would be considered supported if participants identifying as men, heterosexual, White, and upper or middle were less likely to report receiving treatment.
To test H3, a logistic regression was conducted, predicting the report of receiving psychological treatment while in college with demographic information (gender, perceived SES, race/ethnicity, and sexual orientation) and mental health burden (anxiety and depression, as measured by the DASS-21). Categorical variables were indicator coded, with the category that was previously observed to have the lowest level of anxiety and depression selected as the reference category. Structured in this way, this logistic regression measures the influence of the demographic variables in the context of both each other and of anxious and depressive symptoms. Thus, the effect of membership in a particular demographic group can be measured while accounting for the influence of the differences in mental health amongst those demographic groups. This hypothesis would be considered supported if the odds ratios for the demographic variables remained of meaningful size, even after accounting for the influence of the mental health burden.
Results
For the DASS-21 scale, observed alphas were acceptable; .82 (DASS-Anxiety) and .91 (DASS-Depression). These approximately match those previously observed (.82 for DASS-Anxiety, and .93 for DASS-Depression).23 Table 2 shows mental health measures by demographic variables of interest and the results of the one-way ANOVAs described above. See Table 2 for detailed statistics and effect sizes. Consistent with H1, for both anxiety and depression, men had the lowest mental health burden, followed by women and those who identified their gender in another way. Similarly, those who reported being in a high SES had the lowest level of depressive symptoms, followed by middle SES and low SES. A similar pattern was observed for symptoms of anxiety, with low SES having a significantly higher burden than middle and upper, with no significant differenced observed between middle and upper. For orientation, those who identified as heterosexual had a significantly lower mental health burden than any other orientation. For race and ethnicity, significant differences were not observed for anxiety, while a complex pattern emerged for depression. White, Black, and Asian students, and those who reported more than one race or ethnicity had the lowest levels of depressive symptoms, while Latinx and those who identified as a different race or ethnicity had the highest. H1 is thus partially supported; with the exception that the predicted relationship between race/ethnicity and anxiety, the expected pattern of results was otherwise observed. Table 2 for details, including exact values.
Table 2.
Continuous mental health measures and receipt of treatment by demographic factors
| Anxiety (DASS) | Depression (DASS) | Not receiving treatment n (%) | Receiving treatment n (%) | ||
|---|---|---|---|---|---|
| Gender |
F(2,2069) = 22.30 p < .001 η2 = .02 |
F(2,2069) = 21.42, p < .001 η2 = .02 |
χ2 (2, n = 2,079) = 86.75 p < .001 Cramer’s V = .20 |
||
| Men | 5.94a ± 6.84 | 8.69a ± 9.12 | 636 (76.44%) | 196 (23.56%) | |
| Women | 7.57b ± 7.89 | 9.02a ± 9.24 | 695 (57.92%) | 505 (42.08%) | |
| Other | 12.13c ± 10.23 | 17.79b ± 12.60 | 19 (40.43%) | 28 (59.57%) | |
| Year in college |
F(3,2069) = 0.97 p = .40 η2 = .001 |
F(3,2069) = 0.65 p = .58 η2 = .001 |
NA (see note) | ||
| First | 6.59 ± 7.46 | 9.50a ± 9.73 | 437 (81.53%) | 99 (18.47%) | |
| Second | 7.31 ± 7.53 | 9.12a ± 9.42 | 389 (69.84%) | 168 (30.16%) | |
| Third | 7.24 ± 8.08 | 9.01a ± 9.48 | 253 (54.53%) | 211 (45.47%) | |
| Fourth | 6.98 ± 7.51 | 8.70a ± 8.85 | 271 (51.82%) | 252 (48.18%) | |
| Perceived SES |
F(2,2069) = 9.14 p < .001 η2 = .01 |
F(2,2069) = 14.53, p < .001 η2 = .01 |
χ2 (2, n = 2,079) = 0.88 p = .01 Cramer’s V = .07 |
||
| Lower | 9.00a ± 8.98 | 11.91a ± 10.56 | 128 (55.65%) | 102 (44.35%) | |
| Middle | 6.95b ± 7.59 | 9.20b ± 9.43 | 692 (66.47%) | 349 (33.53%) | |
| Upper | 6.58b ± 7.19 | 8.16c ± 8.77 | 529 (65.47%) | 279 (34.53%) | |
| Sexual orientation |
F(3,2069) = 24.10, p < .001 η2 = .05 |
F(3,2069) = 35.51 p < .001 η2 = .05 |
χ2 (3, n = 2,080) = 86.11, p < .001 Cramer’s V = .20 |
||
| Heterosexual | 6.35a ± 7.07 | 8.06a ± 8.64 | 1160 (69.67%) | 505 (30.33%) | |
| Gay/Lesbian | 9.59b ± 8.53 | 12.27b ± 10.64 | 50 (51.55%) | 47 (48.45%) | |
| Bisexual | 10.74b ± 9.93 | 14.01b ± 11.46 | 63 (41.18%) | 90 (58.82%) | |
| Other | 8.86b ± 8.44 | 12.94b ± 10.62 | 77 (46.67%) | 88 (53.33%) | |
| Race/ethnicity |
F(5,2058) = 1.58, p = .16 η2 = .004 |
F(5,2058) = 3.10 p = .01 η2 = .007 |
χ2 (5, n = 2,071) = 7.47 p = .19 Cramer’s V = .06 |
||
| Latinx | 7.26 ± 7.64 | 10.34a ± 9.91 | 119 (61.98%) | 73 (38.02%) | |
| Black | 8.48 ± 9.93 | 10.60a,b ± 10.73 | 51 (62.20%) | 31 (37.80%) | |
| Asian | 7.40 ± 7.43 | 9.42a,b ± 9.37 | 132 (71.74%) | 52 (28.26%) | |
| White | 6.79 ± 7.49 | 8.58b ± 9.05 | 952 (64.89%) | 515 (35.11%) | |
| More than one | 6.89 ± 5.40 | 10.34a,b ± 8.59 | 30 (65.22%) | 16 (34.78%) | |
| Other | 8.32 ± 8.74 | 11.05a ± 10.96 | 57 (57.00%) | 43 (43.00%) | |
Within each subtable and column, values with different subscripts are significantly difference at p < .05 based on a one-way ANOVA and post-hoc follow-up tests. Results of one-way ANOVA tests are shown for each demographic category; post-hoc tests were not run and are thus not reported if the ANOVA or χ2 results were not significant. Relationship between receipt of treatment at any point in college career and year in college are logically related, and thus the significance of that relationship is not meaningful and was not analyzed.
Table 2 shows the percentage of each demographic category receiving mental health treatment during college. Consistent with differences in mental health burden, women and participants identifying as a gender category different than man and woman were significantly more likely to report receiving treatment. Participants who reported being in a lower SES group were more likely to receive treatment, and heterosexual participants were significantly less likely to receive treatment. A significant relationship between race/ethnicity and receiving treatment was not observed. Since participants were asked if they had received treatment at some point in their college career, the increasing rate of treatment associated with increased seniority is best interpreted as a measurement artifact and not otherwise meaningful. These results are consistent with those discussed above and consistent with H2: women and other gender identities, lower SES, and sexual orientations other than heterosexual are more likely to have received treatment.
Table 3 presents the percentage of participants receiving treatment by mental health severity category. Consistent with expectations, increased severity was found to be associated with increased likelihood of receiving treatment for both anxiety and depression.
Table 3.
Percent of participants receiving treatment by mental health severity category
| Participants in category N |
Receiving treatment N (%) |
|
|---|---|---|
| Anxiety categories | χ2 (4, n = 2,034) = 174.83, p < .001, Cramer’s V = .29 | |
| Low anxiety | 1279 | 333 (26.04%) |
| Mild anxiety | 189 | 66 (34.92%) |
| Moderate anxiety | 288 | 139 (48.26%) |
| Severe anxiety | 96 | 49 (51.04%) |
| Extremely severe anxiety | 182 | 127 (69.78%) |
| Depression categories | χ2 (4, n = 2,034) = 124.19, p < .001, Cramer’s V = .25 | |
| Low depression | 1291 | 347 (26.88%) |
| Mild depression | 223 | 93 (41.70%) |
| Moderate depression | 270 | 125 (46.30%) |
| Severe depression | 115 | 65 (56.52%) |
| Extremely severe depression | 135 | 84 (62.22%) |
Table 4 presents the results of a logistic regression predicting the receipt of treatment with the demographic categories of interest.
Table 4.
Results of a logistic regression predicting receipt of treatment by mental health burden and demographic category membership
| Odds Ratio (95%) | ||||||
|---|---|---|---|---|---|---|
| B | SE | Lower | Odds | Upper | p | |
| Constant | −1.87 | 0.12 | 0.16 | < .001 | ||
| Mental health burden | ||||||
| Anxiety (DASS) | 0.05 | 0.01 | 1.04 | 1.06 | 1.07 | < .001 |
| Depression (DASS) | 0.03 | 0.01 | 1.02 | 1.03 | 1.04 | < .001 |
| Gender | < .001 | |||||
| Woman (vs. man) | 0.84 | 0.11 | 1.86 | 2.32 | 2.88 | < .001 |
| Other (vs. man) | 0.92 | 0.37 | 1.23 | 2.52 | 5.17 | < .001 |
| Socioeconomic status | .27 | |||||
| Middle (vs. high) | 0.13 | 0.19 | 0.79 | 1.14 | 1.66 | .49 |
| Low (vs. high) | −0.12 | 0.11 | 0.72 | 0.89 | 1.10 | .28 |
| Sexual orientation | ||||||
| Gay/lesbian (vs. heterosexual) | 0.74 | 0.24 | 1.32 | 2.09 | 3.32 | < .001 |
| Bisexual (vs. heterosexual) | 0.68 | 0.19 | 1.36 | 1.97 | 2.86 | < .001 |
| Other (vs. heterosexual) | 0.64 | 0.18 | 1.33 | 1.90 | 2.73 | < .001 |
| Race/ethnicity | .22 | |||||
| Latinx (vs. White) | −0.02 | 0.19 | 0.67 | 0.98 | 1.42 | .91 |
| Black (vs. White) | −0.11 | 0.27 | 0.53 | 0.90 | 1.52 | .69 |
| Asian (vs. White) | −0.49 | 0.19 | 0.42 | 0.61 | 0.89 | .01 |
| More than one (vs. White) | −0.23 | 0.33 | 0.41 | 0.79 | 1.53 | .49 |
| Other (vs. White) | 0.01 | 0.24 | 0.63 | 1.01 | 1.60 | .98 |
R2 (Cox & Snell) = .14; R2 (Nagelkerke) = .19. Model χ2 (14) = 307.46, p < .001
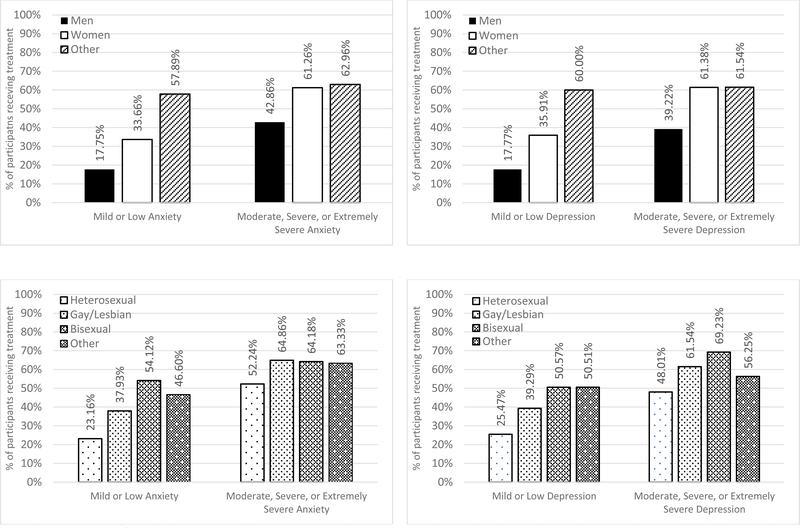
The overall model was found to significantly predict the report of the receipt of mental health treatment. Anxiety and depression were found to significantly predict treatment, as did gender and sexual orientation, even after accounting for the influence of anxious and depressive symptoms. Socioeconomic status and race/ethnicity were not found to be predictive of receiving treatment. After accounting for the influence of anxious and depressive symptoms, the odds of being in treatment for women were 2.32x (vs. men), and the odds of being in treatment were 2.52x for students who identified as a gender other than man or woman (vs. men). Similarly, the odds of being in treatment were 3.32x for students who identified as gay or lesbian, 2.86x for bisexual students, and 2.73 for any other orientation vs. heterosexual students. The only racial or ethnic category that rose to statistical significance was that of Asian students, for whom the odds of being in treatment were 0.61x (vs. White students). See Table 4 for odds ratios and 95% confidence intervals for these analyses. Figure 1 illustrate these results by showing the percent of participants receiving treatment by dichotomized (as per Lovibond & Lovibond 24 after grouping Low and Mild vs. Moderate, Severe, and Extremely Severe) categories for anxiety and depression. H3 was supported; participants who identified as either men or heterosexual were less likely to receive treatment, even after accounting for their lower levels of anxiety and depressive symptoms.
Figure 1:
Percent of participants receiving treatment by gender and sexual orientation and grouped mental health severity category
Discussion
This study offers additional evidence of the significant mental health needs of college students. Approximately 35% of the students in our study received treatment during college, with almost half of fourth year students receiving treatment while in college. While we did not examine use of counseling services in the previous year, we did find that among first year students (who had been on campus for five months when data collection occurred), 18.47% were already receiving treatment. Given that Eisenberg found that in 2007, 15% of students had received treatment in the past year, our data are consistent with an increase in the rate of treatment.9 Data from college counseling center directors support this, as Gallagher reports substantial increases usage of college counseling centers.16 The Center for Collegiate Mental Health reports usage rates increased 30–40% in the previous five years, while enrollment had only increased by 5%.2 Our results provide further support for these findings in the population of students attending small colleges.
This increase in usage makes it all the more important to test how limited treatment resources are used. We found demographic differences in symptomology for depression and anxiety, with men (vs. both women and people identifying as an other gender identity) reporting the lowest levels of depression and anxiety. These findings replicate other work, such as the systematic review by Ibrahim et al25 documenting depression amongst college students. The World Health Organizations international survey of college student mental health found that in middle- and high-income countries, sexual minority and female students compared with their heterosexual and male students experienced higher rates of depression and anxiety.8
While we found no significant differences in anxiety scores by race and ethnicity, we did observe significant differences in depressive symptomology. Latinx and students who identify as an other race/ethnicity had higher rates of depressive symptoms vs. White students. Mokrue and Acri26 found no significant differences in race/ethnicity in measures of depression and anxiety in their sample of college students. Similarly, Liu et al27 note that racial/ethnic minority college students were less likely than White peers to report an existing MH diagnosis; however, the same research found that rates of suicidal ideation and attempts were higher for mixed race and Asian students compared with White students. The different rates of suicidality and suicide attempts were explained by greater levels of exposure to stressful/traumatic events which greatly increased the likelihood of suicidal thoughts and behaviors. Additional researchers have noted stress—particularly minority stress—as a significant factor contributing to mental health challenges. Arbona and Jimenez 28 found that minority stress, particularly in the context of academic experiences and perception of negative campus cultures, were predictive of Latninx students’ experiences of depression. Cookley et al29 described the experience of depression and anxiety among racial/ethnic minority students through models that consider both the students’ experience of discrimination and feelings of being an impostor. Similarly, Gummadam et al30 note that a sense of belonging to a particular college was significantly negatively related to racial/ethnic minority students’ experience of depressive symptoms. In this regard, the higher rates of depressive symptoms may be reflective of students’ experience of campus cultures and their exposure to minority stress.
Minority stress is also theorized to be a strong contributing factor to the disparities in mental health outcomes among sexual minorities.31 Meyer31 explains higher rates of mental health disorders among sexual minorities as a response to experiences of rejection, prejudice, internalized stigma, and the additional burdens of hiding or disclosing one’s sexual orientation. Russell and Fish32 note that despite increased acceptance for LGBT people, LGBT adolescents experience higher rates of mental health burdens vs. heterosexual peers. The American Freshman National Norms Study noted higher rates of depression among gay/lesbian, bisexual and questioning first year students vs. their heterosexual peers.33 Consistent with the minority stress model, Woodford & Kulick34 found experiences of heterosexism on a college campus predicted negative mental health outcomes for sexual minority college students, and that campus integration was a protective factor for sexual minority students. Of concern, our data suggest that students in our study report higher rates of depressive and anxious symptomology. As Stall et al35 have documented, the coexistence of multiple mental health burdens can have a synergistic effect in sexual minority populations, leading to even greater negative outcomes across multiple health domains (physical health, substance use, etc.).
Two primary findings are worth exploring in greater detail regarding the demographic factors associated with help-seeking behaviors. While there was a meaningful increase in the percent of students seeking mental health treatment as scores for depression and anxiety increased, our results indicate that a large number of students with scores suggesting they may benefit from treatment are, in fact, untreated. Approximately 38% of students with depressive scores in the extremely severe depression range reported that they had not sought treatment for their depressive symptoms. Similarly, 31% of students with symptoms of extremely severe anxiety also had not sought treatment. It is particularly concerning that this undertreatment was observed amongst students who have access to mental health services free of charge, which should reduce one of the more prominent barriers to getting mental health treatment.
While a considerable percentage of students who may benefit from mental health services are not receiving them, we observed significant demographic differences in who seeks these services. In our study we found women were 2.32 times as likely to be receiving treatment compared to men, even while controlling for the higher rates of depression and anxiety among women. Students identifying as gay or lesbian were 3.32 times as likely as their heterosexual peers to be seeking treatment as well their bisexual peers were 2.86 times as likely to be seeking treatment compared with heterosexual peers. The only noted difference with regard to race/ethnicity was among Asian and White students, such that Asian students were less likely to be receiving treatment while accounting for rates of depressive and anxious symptomology. Students self-reported socioeconomic status was not found to be related to the likelihood of receiving treatment, which was in contrast to the research of Eisenberg et al9 who found that students from lower socioeconomic backgrounds were less likely to be in treatment. The difference may be an issue of access, as Eisenberg9 notes insurance coverage was a barrier to receiving services, and all students in our sample were provided with the opportunity to use campus mental health centers at no (additional) charge. An additional study by Eisenberg et al21 found male students and Asian students were more likely to have personal stigma associated with use of mental health services, and were less likely to utilize available services. Shame and stigma, as well as parental and peer norms to mental health services have been demonstrated to be strong predictors of use of mental health treatment among male college students.36,37
The higher rates of mental health treatment among sexual minority students in our sample are similar to other studies that have found a similar trend.38 The results are encouraging, as they indicate sexual minority students are using services available to them. McKinley et al39 note that college counseling websites play an important role in encouraging sexual minorities to utilize their services, with explicit information about LGBT issues an important component of signaling safe inclusive spaces for mental health services. The two institutions in our study both have prominent statements addressing a commitment to equity and diversity which may be a factor influencing the high rates of mental health services utilization for sexual minorities.
Finally, while the results indicate that many groups at higher risk for mental health burdens are indeed seeking treatment, they also clearly indicate that men are seeking treatment at significantly lower rates than their anxiety and depression symptomology suggest. It may thus be beneficial to target men more directly to help normalize the experience of seeking treatment, reduce stigma, or otherwise explore the barriers to help-seeking in greater detail. Rosenthal and Wilson40 similarly found that higher rates of psychological distress were associated with greater use of college counseling centers, while also noting no differences in mental health outcomes in their sample with regard to race/ethnicity, gender and socioeconomic status. Despite this positive trend, it is important to note that approximately 38% of students with symptomology consistent with extremely severe depression and 31% of students with symptomology consistent with extremely severe anxiety were not receiving treatment.
This study has a number of limitations. This was a cross-sectional analysis which does not provide a clear picture of the number of students seeking help in a given year. While students reported whether or not they were seeking mental health treatment, we don’t know what specifically they were seeking help for. The students in this study are not broadly representative of all undergraduate students. The students in this study do represent a cross section of geographic, racial/ethnic, and socio-economic-statuses, however, the students attend highly selective colleges, which are not representative of the larger population of college students.
The results of this study demonstrate both that at least some colleges are able to reach high risk student populations, and that significant additional work remains. Specifically, addressing some of the barriers to male students receiving treatment should be pursued, likely by addressing issues of stigma, normalizing mental health treatment and possibly offering screening services for larger numbers of students. It is important to also recognize that while there is a need for more students to receive mental health treatment, colleges are reporting challenges keeping up with the increased demand in counseling services. Therefore, any attempt to address the college mental health crisis must also explore opportunities for expanding treatment while addressing prevention. Addressing minority students’ experience of campus culture as well as creating greater opportunities for all students to find meaningful relationships and a sense of belonging may be useful for reducing the negative mental health outcomes.
Acknowledgments
Research reported in this publication was supported by an Institutional Development Award (IDeA) from the National Institute of General Medical Sciences of the National Institutes of Health under grant number P20GM103449. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NIGMS or NIH.
Research was also supported by the Middlebury College Research Leave Program.
Additionally, we would like to thank our colleagues at the Vermont Genetics Network and Keith Burt, Ph.D.
References
- 1.Aldridge-Gerry AA, Roesch SC, Villodas F, McCabe C, Leung QK, Da Costa M. Daily stress and alcohol consumption: modeling between-person and within-person ethnic variation in coping behavior. J Stud Alcohol Drugs 2011;72(1):125–134. doi:doi: 10.15288/jsad.2011.72.125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Center for Collegiate Mental Health. Annual Report Center for Collegiate Mental Health; 2017. https://sites.psu.edu/ccmh/files/2018/01/2017_CCMH_Report-1r3iri4.pdf. Accessed December 28, 2018. [Google Scholar]
- 3.Pierceall EA, Keim MC. Stress and coping strategies among community college students. Community Coll J Res Pract 2007;31(9):703–712. doi:doi: 10.1080/10668920600866579 [DOI] [Google Scholar]
- 4.Jones PB. Adult mental health disorders and their age at onset. Br J Psychiatry 2013;202(s54):s5–s10. doi: 10.1192/bjp.bp.112.119164 [DOI] [PubMed] [Google Scholar]
- 5.Kessler RC, Amminger GP, Aguilar-Gaxiola S, Alonso J, Lee S, Ustin TB. Age of onset of mental disorders: A review of recent literature. Curr Opin Psychiatry 2008;20(4):359–364. doi:doi: 10.1097/YCO.0b013e32816ebc8c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de Girolamo G, Dagani J, Purcell R, Cocchi A, McGorry PD. Age of onset of mental disorders and use of mental health services: needs, opportunities and obstacles. Epidemiol Psychiatr Sci 2012;21(1):47–57. doi: 10.1017/S2045796011000746 [DOI] [PubMed] [Google Scholar]
- 7.Blanco C, Okuda M, Wright C, et al. Mental Health of College Students and Their Non–College-Attending Peers: Results From the National Epidemiologic Study on Alcohol and Related Conditions. Arch Gen Psychiatry 2008;65(12):1429–1437. doi: 10.1001/archpsyc.65.12.1429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Auerbach RP, Mortier P, Bruffaerts R, et al. Mental disorder comorbidity and suicidal thoughts and behaviors in the World Health Organization World Mental. Health Surv Int Coll Stud Initiat Int J Methods Psychiatr Res 2018;1752. doi:doi: 10.1002/mpr.1752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eisenberg D, Gollust SE, Golberstein E, Hefner JL. Prevalence and correlates of depression, anxiety, and suicidality among university students. Am J Orthopsychiatry 2007;77(4):534–542. doi:doi: 10.1037/0002-9432.77.4.534 [DOI] [PubMed] [Google Scholar]
- 10.Kessler RC, Birnbaum H, Demler O, et al. The prevalence and correlates of nonaffective psychosis in the National Comorbidity Survey Replication (NCS-R). Biol Psychiatry 2005;58(8):668–676. doi:doi: 10.1016/j.biopsych.2005.04.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kessler RC, Wang PS. The descriptive epidemiology of commonly occurring mental disorders in the United States. Annu Rev Public Health 2008;29:115–129. doi:doi: 10.1146/annurev.publhealth.29.020907.090847 [DOI] [PubMed] [Google Scholar]
- 12.Andrews B, Wilding JM. The relation of depression and anxiety to life-stress and achievement in students. Br J Psychol 2004;95(4):509–521. doi:doi: 10.1348/0007126042369802 [DOI] [PubMed] [Google Scholar]
- 13.Pedrelli P, Nyer M, Yeung A, Zulauf C, Wilens T. College students: mental health problems and treatment considerations. Acad Psychiatry 2015;39(5):503–511. doi:doi: 10.1007/s40596-014-0205-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pritchard ME, Wilson GS. Using emotional and social factors to predict student success. J Coll Stud Dev 2003;44(1):18–28. doi:doi: 10.1353/csd.2003.0008 [DOI] [Google Scholar]
- 15.Weitzman ER. Poor mental health, depression, and associations with alcohol consumption, harm, and abuse in a national sample of young adults in college. J Nerv Ment Dis 2004;192(4):269–277. doi:doi: 10.1097/01.nmd.0000120885.17362.94 [DOI] [PubMed] [Google Scholar]
- 16.Gallagher RP. National survey of college counseling centers. Am Coll Couns Assoc Retrieved December 2014. scholarship.pitt.edu/28178/1/survey_2014.pdf.
- 17.Lauff E, Ingels SJ. Education Longitudinal Study of 2002 (ELS: 2002): A First Look at 2002. later National Center for Education Statistics; 2014. https://nces.ed.gov/pubsearch/pubsinfo.asp. [Google Scholar]
- 18.Eisenberg D, Hunt J, Speer N, Zivin K. Mental health service utilization among college students in the United States. J Nerv Ment Dis 2011;199(5):301–308. doi:doi: 10.1097/NMD.0b013e3182175123 [DOI] [PubMed] [Google Scholar]
- 19.Yorgason JB, Linville D, Zitzman B. Mental health among college students: do those who need services know about and use them? J Am Coll Health 2008;57(2):173–182. doi:doi: 10.3200/JACH.57.2.173-182 [DOI] [PubMed] [Google Scholar]
- 20.Cooper AE, Corrigan PW, Watson AC. Mental illness stigma and care-seeking. J Nerv Ment Dis 2003;191:339–341. doi:doi: 10.1097/01.NMD.0000066157.47101.22 [DOI] [PubMed] [Google Scholar]
- 21.Eisenberg D, Downs M, Golberstein E, Zivin K. Stigma and help seeking for mental health among college students. Med Care Res Rev 2009;66(5):522–541. doi:doi: 10.1177/1077558709335173 [DOI] [PubMed] [Google Scholar]
- 22.Goodman E, Huang B, Schafer-Kalkhoff T, Adler NE. Perceived socioeconomic status: a new type of identity that influences adolescents’ self-rated health. J Adolesc Health 2007;41(5):479–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Henry JD, Crawford JR. The short-form version of the Depression Anxiety Stress Scales (DASS-21): Construct validity and normative data in a large non-clinical sample. Br J Clin Psychol 2005;44(2):227–239. doi:doi: 10.1348/014466505X29657 [DOI] [PubMed] [Google Scholar]
- 24.Lovibond SH, Lovibond PH. Manuals for the Depression Anxiety Stress Scales 2nd edition. Sydney, Australia: Psychology Foundation of Australia; 1995. [Google Scholar]
- 25.Ibrahim AK, Kelly SJ, Glazebrook C. Analysis of an Egyptian study on the socioeconomic distribution of depressive symptoms among undergraduates. Soc Psychiatry Psychiatr Epidemiol 2012;47(6):927–937. [DOI] [PubMed] [Google Scholar]
- 26.Mokrue K, Acri MC. Subjective health and health behaviors as predictors of symptoms of depression and anxiety among ethnic minority college students. Soc Work Ment Health 2015;13(2):186–200. [Google Scholar]
- 27.Liu CH, Stevens C, Wong SH, Yasui M, Chen JA. The prevalence and predictors of mental health diagnoses and suicide among US college students: Implications for addressing disparities in service use. Depress Anxiety 2018. [DOI] [PMC free article] [PubMed]
- 28.Arbona C, Jimenez C. Minority stress, ethnic identity, and depression among Latino/a college students. J Couns Psychol 2014;61(1):162–168. doi:doi: 10.1037/a0034914 [DOI] [PubMed] [Google Scholar]
- 29.Cokley K, Smith L, Bernard D, et al. Impostor feelings as a moderator and mediator of the relationship between perceived discrimination and mental health among racial/ethnic minority college students. J Couns Psychol 2017;64(2):141–154. doi:doi: 10.1037/cou0000198 [DOI] [PubMed] [Google Scholar]
- 30.Gummadam P, Pittman LD, Ioffe M. School belonging, ethnic identity, and psychological adjustment among ethnic minority college students. J Exp Educ 2016;84(2):289–306. doi:doi: 10.1080/00220973.2015.1048844 [DOI] [Google Scholar]
- 31.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay and bisexual populations: conceptual issues and research evidence. Psychol Sex Orientat Gend Divers 2013;1:3–26. doi:doi: 10.1037/2329-0382.1.S.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Russell ST, Fish JN. Mental health in lesbian, gay, bisexual, and transgender (LGBT) youth. Annu Rev Clin Psychol 2016;12:465–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Eagan K, Stolzenberg EB, Bates AK, Aragon MC, Suchard MR, C R-A. The American Freshman: National norms fall In: Los Angeles: Higher Education Research Institute, UCLA. Retreived; 2015. [Google Scholar]
- 34.Woodford MR, Kulick A. Academic and social integration on campus among sexual minority students: The impacts of psychological and experiential campus climate. Am J Community Psychol 2015;55(1–2):13–24. [DOI] [PubMed] [Google Scholar]
- 35.Stall R, Friedman M, Catania JA. Interacting epidemics and gay men’s health: a theory of syndemic production among urban gay men. Unequal Oppor Health Disparities Affect Gay Bisexual Men U S 2008;1:251–274. [Google Scholar]
- 36.Barksdale CL, Molock SD. Perceived norms and mental health seeking among African American college students. J Behav Health Serv Res 2009;36(3):285–299. [DOI] [PubMed] [Google Scholar]
- 37.Corrigan PW, Kosyluk KA, Markowitz F, et al. Mental illness stigma and disclosure in college students. J Ment Health 2016;25(3):224–230. doi:doi: 10.3109/09638237.2015.1101056 [DOI] [PubMed] [Google Scholar]
- 38.Dunbar MS, Sontag-Padilla L, Ramchand R, Seelam R, Stein BD. Mental health service utilization among lesbian, gay, bisexual, and questioning or queer college students. J Adolesc Health 2017;61(3):294–301. [DOI] [PubMed] [Google Scholar]
- 39.McKinley CJ, Luo Y, Wright PJ, Kraus A. Reexamining LGBT resources on college counseling center websites: An over-time and cross-country analysis. J Appl Commun Res 2015;43(1):112–129. [Google Scholar]
- 40.Rosenthal B, Wilson WC. Mental health services: Use and disparity among diverse college students. J Am Coll Health 2008;57(1):61–68. [DOI] [PubMed] [Google Scholar]