1. Case report
A 45-year-old male with well-controlled HIV presented with 1-week history of blurred vision in both eyes without other ocular or systemic symptoms. His recent CD4 T-cell count was 688 cells/μL with undetectable viral load and routine syphilis EIA (enzyme immunoassay) was negative five months before this presentation.
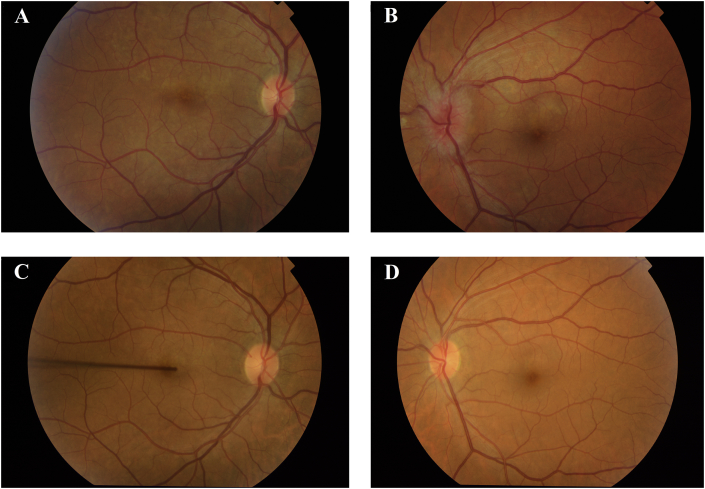
On examination, his VA (visual acuity) was 0.6logMAR (20/80) on the right (OD) and 0.48logMAR (20/63) on the left (OS). Colour vision was reduced to 5/17 OD and 7/17 OS with no relative afferent pupillary defect. Anterior segments were quiet. Fundus examination revealed bilateral multiple creamy subretinal lesions at posterior pole with left gross optic disc oedema without vitritis (Fig. 1A-B).
Fig. 1.
A. Right scattered creamy subretinal lesions.
B. Left gross optic disc oedema with creamy subretinal lesions at posterior pole.
C-D. Normal bilateral appearance of the discs and resolved subretinal lesions.
Blood tests on presentation were positive for syphilis EIA with RPR (rapid plasma reagin) of 1:16 titre, and negative for toxoplasma and borrelia. He was commenced on 14-day course of intramuscular Procaine Penicillin 2.4 million units with Probenecid 500 mg orally four times daily, followed by two-week course of Doxycycline 200 mg twice daily. He also received 40 mg oral Prednisolone for first three days.
On day-14 of treatment, his VA recovered to −0.2logMAR (20/12) bilaterally with marked improvement in colour vision – 14/17 (OD) and 16/17 (OS). Repeated RPR titre also decreased by 4-fold. Ten months later his VA was −0.2logMAR (20/12) and colour vision 17/17 bilaterally. Both eyes were quiescent on examination with complete resolution of bilateral subretinal lesions and left optic disc oedema (Fig. 1C-D).
2. Discussion
Syphilis “the great imitator” is known to mimic many conditions in all body systems, often leading to diagnostic delay. In the eye, it can manifest as any ocular inflammation and may be the only sign of systemic syphilis.1 Ocular syphilis is uncommon with estimated annual incidence of 0.3 per million UK adult population.2 Therefore, a high index of suspicion is required for early diagnosis as it responds well to treatment with potential full visual recovery. It is particularly important now that the incidence of ocular syphilis is rising.3
Our patient had neurosyphilis with bilateral eye involvement without other systemic symptoms. With negative syphilis test five months before presentation, this shows that ocular involvement can be the first presentation of syphilis and occur at any stage of infection. Previous observations proposed that concurrent HIV infection may affect the clinical presentation of syphilis with faster progression to neurosyphilis, abnormal serological response to infection and atypical response to treatment. Therefore, high level of suspicion and the need for repeated serological testing is paramount especially in immunocompromised patients.
3. Conclusions
Ocular inflammation may be the presenting sign of syphilis infection, particularly in HIV-positive individuals. High index of suspicion ensures syphilis is included in the differential diagnosis. Ophthalmologists play an important role in this context.
Patient consent
Consent to publish this case report has been obtained from the patient in writing.
Funding
No funding or grant support
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Conflict of interest
All authors have no financial disclosures.
Acknowledgments
None.
References
- 1.Kiss S. Semin Ophthalmol. 2005 01/01;20(3):161–167. doi: 10.1080/08820530500232092. [DOI] [PubMed] [Google Scholar]
- 2.Mathew R.G. Invest Ophthalmol Vis Sci. 2014 Jun 12;55(8):5394–5400. doi: 10.1167/iovs.14-14559. [DOI] [PubMed] [Google Scholar]
- 3.Wells J. Eye (Lond) 2018 Jan;32(1):99–103. doi: 10.1038/eye.2017.155. [DOI] [PMC free article] [PubMed] [Google Scholar]