Abstract
Residual pulmonary impairment is common after treatment for tuberculosis (TB). Lung function data in patients with HIV-associated TB are scarce, especially in the context of paradoxical TB-associated immune reconstitution inflammatory syndrome (TB-IRIS) and prophylactic prednisone. We aimed to determine the prevalence of lung function abnormalities in patients with HIV-associated TB and CD4 counts ≤100 cells·μL−1 and assess the effect of prophylactic prednisone and the development of paradoxical TB-IRIS on pulmonary impairment.
We performed spirometry, 6-min walk test (6MWT) and chest radiography at baseline (week 0) and at weeks 4, 12 and 28 in participants of the PredART trial, which evaluated a 28-day course of prednisone to prevent TB-IRIS in patients with HIV-associated TB commencing antiretroviral therapy.
153 participants underwent spirometry and/or 6MWT at one or more time points. Abnormal spirometry measurements were present in 66% of participants at week 0 and 50% at week 28; low forced vital capacity was the commonest abnormality. Chest radiographs showed little or no abnormalities in the majority of participants. Prednisone use resulted in a 42 m greater 6-min walk distance and a 4.9% higher percentage of predicted forced expiratory volume in 1 s at week 4; these differences were no longer significantly different from week 12 onwards. TB-IRIS did not significantly impair lung function outcome.
Residual pulmonary impairment is common in HIV-associated TB. In patients with low CD4 counts, neither prophylactic prednisone as used in our study nor the development of TB-IRIS significantly affected week-28 pulmonary outcome.
Short abstract
Post-tuberculosis lung disease is common in patients with HIV-associated TB at high risk of TB-IRIS (CD4 count ≤100 cells·μL−1). Neither TB-IRIS itself, nor prednisone treatment, affected long-term pulmonary outcomes in a South African clinical setting. http://bit.ly/2RjMl9c
Introduction
Tuberculosis (TB) is frequently complicated by lung function impairment. The odds of abnormal spirometric test results are two- to three-fold higher in patients with a history of TB compared to those without a history of TB, with both obstructive and/or restrictive impairments occuring [1, 2]. Studies of lung function in people with a history of TB found abnormal lung function in 45–87% of subjects [3–5], with even higher proportions reported in multidrug-resistant TB [6, 7]. HIV is an independent risk factor for predominantly obstructive lung function impairment [8, 9]; however, data on lung function impairment in HIV-associated TB are scarce, as HIV co-infected patients are frequently excluded from studies. TB-related lung damage may be less common in those co-infected with HIV; however, current data are conflicting. 1) A single large study found less pulmonary impairment after TB in patients who were HIV-positive [4], while other studies have not supported this beneficial association between HIV status and spirometric outcomes [5, 10, 11]; 2) furthermore, chest radiography findings in patients with HIV-associated TB and low CD4 counts (CD4 <200 cells·μL−1) are frequently normal or atypical [12]; and 3) HIV co-infection results in lower levels of several of mediators usually implicated in inflammatory lung damage [13]. Conversely, paradoxical TB immune reconstitution inflammatory syndrome (TB-IRIS) after the start of antiretroviral therapy (ART) causes inflammation and high levels of inflammatory mediators [14–17]. Two recent studies suggested that TB-IRIS may cause lung function impairment [18, 19]; one showing increased inflammation, as assessed by positron emission tomography (PET)-computed tomography (CT) scan, was associated with worse lung function outcomes [18]. However, in these cohorts only small numbers of patients developed predefined TB-IRIS, yet the authors hypothesise that increases in pulmonary inflammation can occur as part of not clinically recognised TB-IRIS. To date, the only other study exploring the relationship between TB-IRIS and lung function found worse spirometric outcomes in the three patients who developed TB-IRIS compared to 11 controls [15].
Corticosteroids reduce inflammation and inhibit several of the immune mediators implicated in lung damage during TB [20–23], and may therefore reduce lung function impairment associated with TB. Previous studies assessing this association did not find a significant effect of corticosteroid use on tests of lung function [24–27]. However, most of these studies were performed before the introduction of rifampicin, and none included HIV co-infected patients.
In this study, we determined the prevalence of lung function impairment over time in a randomised controlled trial of patients treated for HIV-associated TB. Additionally, we assessed the effect of prednisone evaluated in comparison to placebo for prevention of TB-IRIS on pulmonary outcome in this patient group.
Methods
Design and setting
This was a substudy of the PredART trial [28], a randomised, double-blind, placebo-controlled trial assessing the efficacy of prednisone to prevent TB-IRIS. Participants were recruited from Khayelitsha, a peri-urban township in Cape Town, South Africa. They were ambulant and treated in an outpatient setting. They received either prednisone or placebo (40 mg·day−1 for 2 weeks, followed by 20 mg·day−1 for 2 weeks), starting within 48 h of starting ART. The study drug could be replaced with open-label prednisone (1.5 mg·kg−1·day−1 for 2 weeks, followed by 0.75 mg·kg−1·day−1 for 2 weeks, or longer if clinically indicated) for treatment of TB-IRIS. TB-IRIS events were adjudicated by three clinical experts using the International Network for the Study of HIV-associated IRIS consensus case definition [29].
Enrolment for the substudy started later than the main trial. Participants already enrolled in the main trial could enrol in the substudy from their next eligible visit, if they had not completed the main trial yet. Participants treated for multidrug-resistant TB or who prematurely discontinued TB treatment were excluded from the analysis at week 28. Successful completion of TB treatment was defined following South African National Tuberculosis Management Guidelines [30].
The substudy was approved by the same ethical committees that approved the main trial [28]. Separate written informed consent was obtained.
Procedures
Substudy visits were scheduled at weeks 0 (initiation of ART and study drug), 4, 12 and 28. At each visit, pulmonary symptoms (cough, dyspnoea at exertion and dyspnoea at rest) were assessed by the trial doctor, and spirometry and 6-min walk tests (6MWT) were performed. Forced vital capacity (FVC) and forced expiratory volume in 1 s (FEV1) were measured using a desktop spirometer (Spirolab III; MIR, Rome, Italy). Tests were performed and results interpreted using the 2005 American Thoracic Society/European Respiratory Society guidelines for spirometry, using National Health and Nutrition Examination Survey (NHANES) reference ranges [31]. We defined four possible outcomes (supplementary figure S1): normal lung function (FEV1/FVC ≥70% predicted and FVC ≥80% pred), low FVC (FEV1/FVC ≥70% pred and FVC <80% pred), obstructive impairment with and without low FVC (FEV1/FVC <70% pred) and “technically incorrect”, comprising participants who performed spirometry, but did not meet criteria for interpretation (supplementary table S1). 6MWTs were performed following the 2002 American Thoracic Society guidelines [32] on a 20-m outdoor track. Chest radiography was performed at weeks 0 and 28. After completion of the study, digitised chest radiographs were scored by two independent blinded readers, using an adapted version of the Timika score as described by Kriel et al. [33]. Where discrepancy existed, defined as a difference in score of >10 points, a third reader evaluated the chest radiograph and consensus was found using a two-to-one vote.
Statistical methods
Analyses were performed using Stata 15.1 (StataCorp, College Station, TX, USA). For categorical variables and continuous variables, proportions and medians with interquartile ranges (IQR), respectively, were estimated at different time points. Comparison of the Karnofsky Performance Score (KPS) between groups was done using a mixed-effects proportional odds model. Correlation between chest radiograph score and lung function was done using mixed-effects regression (linear or logistic) models. Mixed-effect models including a random intercept and covariates were used to model the evolution of pulmonary function over time. The effect of prophylactic prednisone on pulmonary function was tested using a test of the interaction of prednisone and visit number; participants receiving prednisone as treatment for TB-IRIS were analysed in their intention-to-treat arm (i.e. study placebo or prednisone). The effect of TB-IRIS was tested using a joint test of the main effect of TB-IRIS and its interaction with visit number. A p-value <0.05 was considered statistically significant.
Results
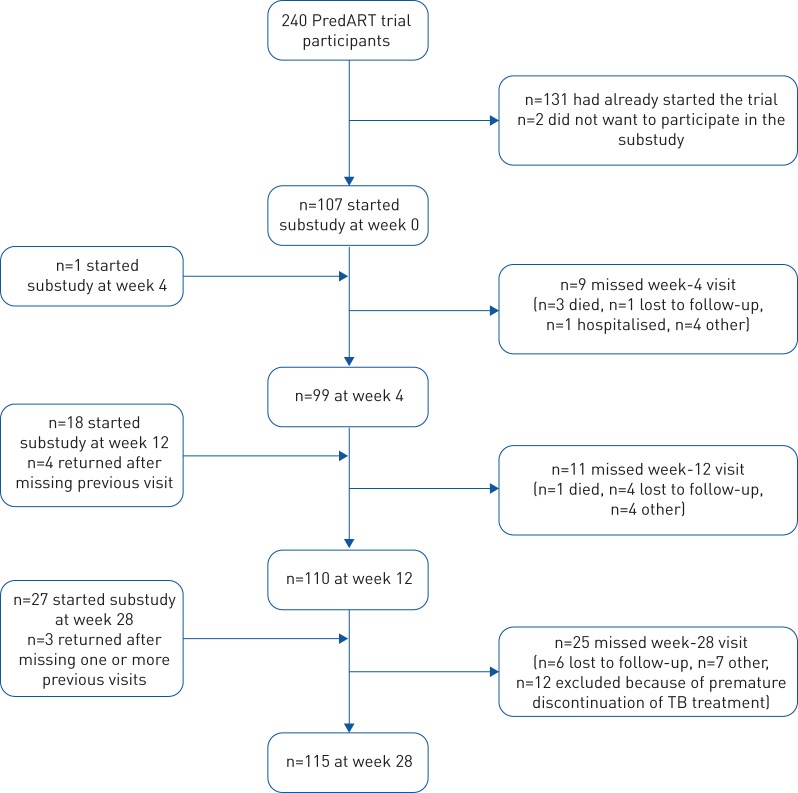
Between January 2015 and February 2016, 153 participants were enrolled, 77 from the prednisone arm and 76 from the placebo arm. The flow of participants is described in figure 1; baseline characteristics are summarised in table 1. 71 (46%) participants developed TB-IRIS: 30 in the prednisone and 41 in the placebo arm; 46 (30%) participants received open-label prednisone as treatment for TB-IRIS: 16 in the prednisone and 30 in the placebo arm.
FIGURE 1.
Number of participants per visit.
TABLE 1.
Baseline characteristics and participants developing tuberculosis-associated immune reconstitution inflammatory syndrome (TB-IRIS) and receiving prednisone as treatment according to trial arm
| Prednisone | Placebo | |
| Male | 49 (64) | 41 (54) |
| Age years | 38 (31–43) | 38 (31–44) |
| CD4 count cells·μL−1 | 46 (24–81) | 50 (24–86) |
| HIV viral load log10 copies·mL−1 | 5.5 (5.2–5.8) | 5.6 (5.3–5.9) |
| Extrapulmonary TB# | 24 (38) | 33 (55) |
| Microbiologically confirmed TB | 53 (70) | 59 (79) |
| Previous TB | 6 (8) | 8 (11) |
| Time on TB treatment at week 0 days | 16 (15–22) | 16 (14–21) |
| Smoking status at week 0¶ pack-years | ||
| Never smoked | 36 (55) | 41 (67) |
| Ever smoked | 30 (45)/2.2 (0.8–5.0) | 20 (33)/3.75 (1.0–10.0) |
| Previous lung disease | 1 (1.3) | 0 (0) |
| Spirometry | ||
| FEV1 % pred | 75 (61–88) | 73 (59–86) |
| FVC % pred | 74 (66–89) | 73 (65–81) |
| FVC/FEV1 % | 83 (79–85) | 82 (77–86) |
| TB-IRIS | 30 (39) | 41 (54) |
| Treatment with open-label prednisone for suspected TB-IRIS | 16 (21) | 30 (39) |
Data are presented as n (%) or median (interquartile range). TB: tuberculosis (pulmonary TB: participants with one or more pulmonary signs or symptoms (such as cough, shortness of breath, abnormal chest radiograph) of TB at presentation; extrapulmonary TB: participants with signs of extrapulmonary tuberculosis (such as pleural effusion or enlarged lymph nodes); microbiologically confirmed TB: participants with Mycobacterium tuberculosis detected on culture, with the use of the Xpert MTB/RIF assay (Cepheid, Sunnyvale, CA, USA), or as positive acid-fast bacilli on smear microscopy); FEV1: forced expiratory volume in 1 s; FVC: forced vital capacity. #: n=123; ¶: n=127.
Overall prevalence of lung function abnormalities
Symptoms
80% of participants reported cough, dyspnoea on exertion and/or dyspnoea at rest as one of their presenting TB symptoms. At week 0, a median 16 (IQR 15–21) days into TB treatment, 50% had one or more of these symptoms. Symptoms improved over time; however, 8% of participants who successfully completed their TB treatment at week 28 still had one or more respiratory symptoms (table 2).
TABLE 2.
Symptoms, spirometric outcomes, 6-min walk distance (6MWD) and chest radiograph scores in the whole study group at different time points
| Week 0# | Week 4 | Week 12 | Week 28 | |
| Symptoms | ||||
| Participants | 107 | 99 | 110 | 111 |
| Cough | 40 (37.4) | 29 (29.3) | 14 (12.7) | 5 (4.5) |
| Dyspnoea at exertion | 37 (34.6) | 27 (27.3) | 12 (10.9) | 5 (4.5) |
| Dyspnoea at rest | 11 (10.3) | 8 (8.1) | 3 (2.7) | 1 (0.9) |
| Total¶ | 54 (50.5) | 43 (43.4) | 20 (18.2) | 9 (8.1) |
| Spirometry outcome | ||||
| Participants | 106 | 96 | 110 | 114 |
| Normal+ | 28 (26.4) | 36 (37.5) | 50 (45.5) | 54 (47.4) |
| Low FVC§ | 48 (45.3) | 42 (43.8) | 43 (39.1) | 44 (38.6) |
| Obstruction with or without low FVCƒ | 7 (6.6) | 7 (7.3) | 10 (9.1) | 11 (9.7) |
| Technically incorrect## | 23 (21.7) | 11 (11.5) | 7 (6.4) | 5 (4.4) |
| 6MWD | ||||
| Participants | 102 | 91 | 104 | 113 |
| 6MWD m | 520 (465–576) | 524 (450–579) | 539 (483–608) | 585 (520–655) |
| Chest radiography | ||||
| Participants | 135 | 61 | ||
| Chest radiograph score | 4 (0.8–11.7) | 0.9 (0–3.75) |
Data are presented as n, n (%) or median (interquartile range). FVC: forced vital capacity. #: the start day of antiretroviral therapy and prednisone/placebo (median 16 days after start of anti-tuberculosis treatment); ¶: cough and/or dyspnoea at exertion and/or dyspnoea at rest; +: forced expiratory volume in 1 s (FEV1)/FVC ≥70% predicted and FVC ≥80% pred; §: FEV1/FVC ≥70% pred and FVC <80% pred; ƒ: FEV1/FVC <70% pred; ##: test not fulfilling criteria for interpretation.
Spirometry
426 spirometry tests were performed. In 15 substudy participants, spirometry was not performed at one or more time points; five of these participants were too ill to perform spirometry, the remaining 10 were not undertaken for logistic reasons. Spirometic outcomes at different time points are shown in table 2. The proportion of participants with a normal spirometry outcome was 26.4% at week 0, increasing to 47.4% at week 28. Low FVC was the commonest abnormality. The proportion of participants with obstruction with or without low FVC was low and roughly the same over time. We found no effect of CD4 cell count recovery on change over time of spirometric outcomes (p=0.71 for FEV1).
At week 0, 23 (21.7%) participants performed a technically incorrect test; the main reason was the inability to exhale for 6 s. To assess if this possibly reflected more impaired lung function, we compared 6-min walk distance (6MWD) and KPS between participants with correctly and incorrectly performed tests. On average, the participants with an incorrect test had a 6MWD 56 m (95% CI 30–83 m, p<0.001) shorter and a lower KPS (p<0.001). At week 12, 13 out of 20 participants with an initial incorrect test had obstruction and/or a low FVC; with similar findings in 11 out of 16 participants at week 28.
6MWD
410 6MWTs were performed; 29 substudy participants did not perform a walk test at one or more time points, the main reasons being painful feet or rain. Median (IQR) 6MWD was 520 (465–576) m at week 0 and 585 (520–655) m at week 28 (table 2).
Chest radiograph score
Chest radiograph scores were available for 135 participants at week 0, and for 61 participants at week 28. Possible scores ranged from 0 to 140, with higher scores indicating more chest radiograph abnormalities. The median (IQR) chest radiograph scores were low: 4.0 (0.8–11.7) at week 0 and 0.9 (0–3.75) at week 28 (table 2). Cavities were present in eight (6%) participants at week 0 and one (2%) participant at week 28. Overall, chest radiograph scores showed significant correlation with respiratory symptoms, 6MWD and FEV1: for an increase of 10 points in chest radiograph score, an odds ratio of 1.51 for symptoms (95% CI 1.13–2.03, p=0.006) was observed (supplementary table S2), the average 6MWD decreased by 21 m (95% CI 11–31 m, p<0.001) and the average FEV1 decreased by 3.3% pred (95% CI 1.9–4.8% pred, p<0.001). However, in chest radiographs with lower scores (i.e. <10), the FEV1 varied markedly, and both normal and impaired lung function were seen in participants with little or no chest radiograph abnormalities (supplementary figure S2).
There was no significant association between chest radiograph score at week 0 and spirometry results at week 28 (odds ratio for normal lung function at week 28 per 10-point increase in chest radiograph score at week 0 was 0.77 (95% CI 0.55–1.08, p=0.13) and average FEV1 at week 28 was 1.87% pred lower (95% CI 3.98–−0.24% pred, p=0.08) for every 10-point increase of week 0 chest radiograph score).
Effect of prednisone
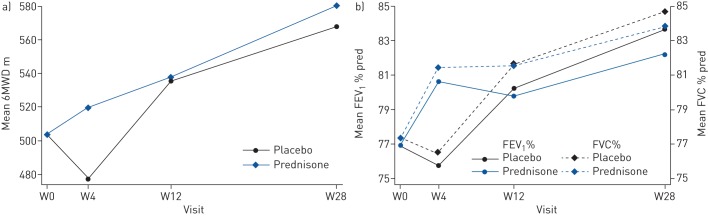
There was no statistically significant difference in the change over time of symptoms (p=0.13) or chest radiograph score (p=0.92) between the prednisone and the placebo arm. The change in 6MWD over time was statistically significantly different between the groups (p=0.03), with the largest difference at week 4: participants in the prednisone arm walked 42 (95% CI 13–72) m further compared to participants in the placebo arm. In addition, change over time of both FEV1 and FVC were statistically significantly different between the two arms (p=0.03 and p=0.01), again most obvious at week 4, with those in the prednisone arm having FEV1 4.9% pred (95% CI 0.7–9.0% pred) higher and FVC 4.9% pred (95% CI 1.3–8.5% pred) higher at week 4 compared to those in the placebo arm. Adjusting for the use of prednisone as treatment for TB-IRIS gave similar results (supplementary table S3). Baseline lung function did not statistically significantly affect the impact of prednisone (p=0.56 for FEV1) (supplementary table S4). At week 28, there was no longer a clear difference in either the 6MWD or FEV1 and FVC between the arms (figure 2 and table 3 and supplementary table S5).
FIGURE 2.
The effect of prednisone prophylaxis to prevent tuberculosis-associated immune reconstitution inflammatory syndrome (TB-IRIS) on lung function. Patients treated for HIV-associated TB received either prednisone or identical placebo during the first 4 weeks of antiretroviral therapy. Week (W)0 is the day when antiretroviral therapy and prednisone or placebo were started. a) Change over time of 6-min walk distance (6MWD) was statistically significantly associated with prednisone use (p=0.034); b) change over time of forced expiratory volume in 1 s (FEV1) and forced vital capacity (FVC) % predicted was statistically significantly associated with prednisone use (p=0.029 and p=0.015, respectively). Graphs represent data for nonsmokers. Curves for smokers are parallel.
TABLE 3.
The effect of prednisone prophylaxis on change over time of pulmonary function parameters
| Change over time of 6MWD m | p-value | Change in FEV1 % pred | p-value | |
| Intercept average at week 0 for non-smokers | 504 (484–523) | 504 (484–523) | ||
| Mean change | ||||
| Effect of smoking (ever versus never) | 14 (−11–39) | 0.275 | 14 (−11–39) | 0.275 |
| Mean change from week 0 | ||||
| Effect of time (visit) | <0.0001 | <0.0001 | ||
| Week 4 | −27 (−50–−3) | −1.1 (−4.4–2.1) | ||
| Week 12 | 32 (10–54) | 3.3 (0.2–6.4) | ||
| Week 28 | 64 (42–86) | 6.8 (3.6–10.0) | ||
| Effect of prophylactic prednisone | 0.034 | 0.029 | ||
| Week 4 | 42 (13–72) | 4.9 (0.7–9.0) | ||
| Week 12 | 2 (−26–30) | −0.4 (−4.4–3.5) | ||
| Week 28 | 13 (−15–41) | −1.5 (−5.6–2.6) |
Data are presented as intercept and estimated coefficients (95% CI) from the mixed-effects regression models, unless otherwise stated. Data are adjusted for all other covariates presented in the table. Effect of time (visit) refers to the effect of time in the placebo arm. Because allocation to either the prednisone or the placebo arm was randomised, no adjustment for baseline variables other than smoking was made. 6MWD: 6-min walk distance; FEV1: forced expiratory volume in 1 s.
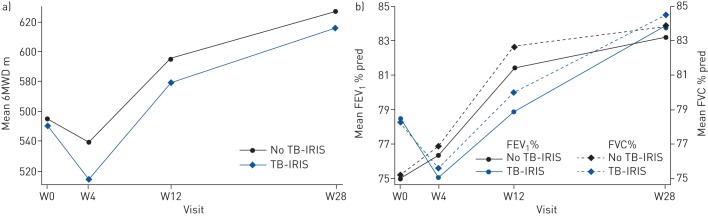
Effect of TB-IRIS
When comparing participants who developed paradoxical TB-IRIS to those who did not, TB-IRIS was associated with a change in the presence of symptoms over time (p=0.03), but there was no statistically significant difference in change over time of FEV1 % pred (p=0.11), FVC % pred (p=0.054), 6MWD (p=0.62) or chest radiograph score (p=0.20) (figure 3, table 4 and supplementary table S6).
FIGURE 3.
The effect of the development of tuberculosis-associated immune reconstitution inflammatory syndrome (TB-IRIS) on lung function. Patients with TB-IRIS are compared to those without TB-IRIS. a) Change over time of 6-min walk distance (6MWD) was not statistically significantly associated with TB-IRIS (p=0.62); b) change over time of forced expiratory volume in 1 s (FEV1) and forced vital capacity (FVC) % predicted was not statistically significantly associated with TB-IRIS (p=0.11 and p=0.054, respectively). Graphs represent data for male nonsmokers in the placebo arm aged 40 years with pulmonary TB, an HIV viral load at screening of 800 000 copies·mL−1, a CD4 at screening of 100 cells·μL−1 and did not have previous TB. The differences between TB-IRIS and no TB-IRIS were similar for other patient profiles. W: week.
TABLE 4.
The effect of tuberculosis-associated immune reconstitution inflammatory syndrome (TB-IRIS) on change over time of pulmonary function parameters
| 6MWD m | p-value | Mean change in FEV1% pred | p-value | |
| Change over time | ||||
| Intercept (average if all other covariates are 0) | 837 (711–964) | 83.9 (57.5–110.3) | ||
| Mean change | ||||
| Effect of TB-IRIS at week 0 | −4 (−35–27) | 0.79 | 3.2 (−2.7–9.2) | 0.29 |
| Effect of smoking (ever versus never) | −44 (−69–−19) | 0.001 | −5.9 (−10.6–−1.1) | 0.02 |
| Effect of age (per increase of 1 year in age at week 0) | −3 (−4–−2) | <0.001 | 0.04 (−0.2–0.3) | 0.76 |
| Effect of sex (female versus male) | −112 (−138–−86) | <0.001 | −3.6 (−9.0–1.8) | 0.19 |
| Effect of type of TB (participants without signs of extrapulmonary TB versus those with signs of extrapulmonary TB) | 30 (−14–74) | 0.19 | 0.7 (−8.6–10.1) | 0.88 |
| Effect of HIV viral load (per log10 cps·mL−1 increase at screening) | −32 (−50–−13) | 0.001 | −0.5 (−4.5–3.4) | 0.79 |
| Effect of CD4 count (per increase of 10 CD4 cells·μL−1 at screening) | −2 (−4–1) | 0.21 | −0.8 (−1.3–−0.2) | 0.005 |
| Effect of previous tuberculosis | −21 (−60–18) | 0.28 | −14.8 (−23.4–−6.1) | 0.001 |
| Mean change week 0 | ||||
| Effect of time (visit) | <0.0001 | <0.001 | ||
| Week 4 | −16 (−45–14) | 1.4 (−3.0–5.7) | ||
| Week 12 | 40 (13–67) | 6.3 (2.3–10.4) | ||
| Week 28 | 72 (44–100) | 8.1 (3.9–12.3) | ||
| Effect of TB-IRIS | 0.68 | 0.06 | ||
| Week 4 | −21 (−54–13) | −4.7 (−9.4–−0.1) | ||
| Week 12 | −11 (−44–21) | −6.0 (−10.5–−1.4) | ||
| Week 28 | −7 (−40–27) | −2.8 (−7.6–2.0) | ||
| Effect of prophylactic prednisone | 0.036 | 0.07 | ||
| Week 4 | 41 (13–70) | 4.4 (0.2–8.7 | ||
| Week 12 | 0 (−27–26) | −0.1 (−4.8– 3.2) | ||
| Week 28 | 4 (−22–31) | −1.3 (−5.5–2.8) |
Data are presented as intercept and estimated coefficients (95% CI) from the mixed-effects regression models, unless otherwise stated. Data are adjusted for all other covariates presented in the table. 6MWD: 6-min walk distance; FEV1: forced expiratory volume in 1 s.
16 participants developed TB-IRIS without any respiratory signs or symptoms. Exclusion of these nonpulmonary IRIS cases from the analysis did not affect the results (data not shown).
Discussion
We assessed pulmonary function in a cohort of patients with HIV-associated TB at high risk of TB-IRIS, enrolled in a trial investigating the efficacy of prophylactic prednisone in preventing TB-IRIS.
Respiratory symptoms were common early during TB treatment and abnormal spirometry (low FVC and airflow obstruction with and without low FVC) was found in 66% of participants with acceptable spirometry. At the end of TB treatment, symptoms persisted in 8% and abnormal spirometry in 50% of participants. The proportion of abnormal spirometry results is higher than expected for either the general or HIV-infected population [1, 34], but is comparable to results from other studies in HIV-associated TB patients [4, 5, 19].
In our trial, open-label treatment of TB-IRIS with prednisone was allowed. This resulted in 30 out of 76 participants in the placebo arm receiving prednisone for the treatment of TB-IRIS and the majority of the participants who developed TB-IRIS receiving prednisone, either as prophylaxis, as treatment, or both, with prednisone treatment given to the more severe cases of TB-IRIS. This limits our evaluation of the individual effects of both prednisone as well as TB-IRIS on lung function.
Within these limitations, we did not find an effect of TB-IRIS on spirometric lung function over time. This contradicts findings of two recent studies [18, 19] that hypothesised that TB-IRIS-like increases in inflammation may lead to decreased lung function, which may occur in patients with HIV-associated TB initiating ART, even in the absence of clinically overt TB-IRIS. It is possible that in the present study, mild TB-IRIS did not result in sufficient additional pulmonary inflammation to affect long-term respiratory outcomes, whereas in severe TB-IRIS the effect was ameliorated by treatment with prednisone.
We found prophylactic prednisone affected change over time of 6MWD and FEV1 and FVC, primarily at week 4, when participants completed their study prednisone, potentially by preventing TB-IRIS. Consequently, the higher proportion of participants with TB-IRIS in the placebo arm may be responsible for the demonstrated favourable effect of prophylactic prednisone on lung function. Additionally, prednisone can directly improve exercise performance [35] and FEV1 in other disease processes, for example acute exacerbations of chronic obstructive pulmonary disease [36]. Ravimohan et al. [18] found that decreased lung function after 4 weeks of TB treatment impacts negatively on long-term lung function, and Auld et al. [19] found similar associations, but only in severe lung function declines. In the current study, despite an increase in lung function at week 4, we did not observe any long-term effects of prophylactic prednisone on lung function. This could be due to Type 2 error, with a large proportion of participants in the placebo arm receiving prednisone as treatment for TB-IRIS. Alternatively, prednisone may have been given too late in the disease process and prescribed only after lung damage had already occurred.
We found a high proportion of participants with technically incorrect spirometry results early on during treatment: a finding not reported previously. In studies performed in participants without TB, in the latter stages of TB treatment or after TB treatment, 2–30% did not perform spirometry correctly and these patients were subsequently excluded [1, 3–5, 9, 18, 37]. We considered that the participants who did not perform spirometry correctly might include those with worse pulmonary status: for example, in severely ill patients, and in those with significant cough and/or shortness of breath spirometry is technically challenging. This hypothesis was supported in our study by finding that the majority of technically incorrect spirometric results were due to inability of patients to exhale for 6 s. Furthermore, the association with a shorter 6MWD and a lower KPS, and abnormal lung function in the majority of these participants at follow-up spirometry testing adds weight to this argument. Thus, excluding these participants from the analyses may underestimate the burden of lung function impairment in TB. In our study, when technically incorrect results were included as abnormal, the percentage abnormal tests at baseline increased from 66% to 74%.
In keeping with published data on HIV-associated TB patients with a low CD4 count [12], only a small proportion of participants demonstrated extensive chest radiograph abnormalities, while cavitation was uncommon. Our finding of a negative association between chest radiograph score and FEV1, although statistically significant, needs to be interpreted with caution. Although a high score is unsurprisingly associated with lower FEV1, a low score does not appear to rule out significant abnormality in FEV1. Several other studies, using many different scoring methods, have reported the relationship between FEV1 and chest radiograph score in TB [3, 5, 10, 38, 39]. However, all studies describe more severe chest radiograph abnormalities than our present study, and few included HIV-positive patients. Those that did chose not to report data on HIV patients specifically, or claimed that the numbers were too small for meaningful subanalysis. Our observation that the presence of a normal chest radiograph in HIV-associated TB patients with a CD4 count ≤100 cells·μL−1 does not exclude lung function abnormalities, is probably explained by the insensitivity of chest radiograph to detect changes responsible for the reduced FEV1, for example small airways and subtle parenchymal abnormalities.
Besides the considerable overlap between participants developing TB-IRIS and participants prescribed prednisone to treat TB-IRIS, our study has other limitations. First, as consequence of the substudy commencing after the main trial, we do not have complete data on all participants. Second, we do not have reliable information about the time between the start of symptoms and the start of TB treatment, with longer duration of symptoms being a risk factor for pulmonary impairment [5, 40]. Third, normal values for 6MWD in our population are lacking. Most participants walked relatively far, possibly because of the relatively short duration of illness and possibly younger age of participants when compared with other chronic lung diseases. Finally, the use of the NHANES reference range (derived in North American populations) may have resulted in an overestimate of lung function impairment, as normal values for FEV1 and FVC tend to be higher than those for African populations [41].
In conclusion, we found that lung function impairment is common in patients with HIV-associated TB. Prednisone to prevent TB-IRIS improved lung function at week 4, possibly by reducing TB-IRIS; however, the 28-day course of prednisone did not improve lung function from week 12 onwards in patients with CD4 counts ≤100 cells·μL−1. Overlap between the groups through the development of TB-IRIS and subsequent use of prednisone as treatment limits our ability to make definitive conclusions. Prednisone remains recommended to prevent TB-IRIS in this population based on the findings of the main PredART trial [28], despite this study being unable to demonstrate long-term benefits in lung function. Further studies, using PET-CT imaging and other biomarkers of inflammation and lung damage in TB [13] are needed to better understand the pathogenesis of lung function impairment in HIV-associated TB.
Supplementary material
Please note: supplementary material is not edited by the Editorial Office, and is uploaded as it has been supplied by the author.
Supplementary material ERJ-01692-2019.SUPPLEMENT (464.5KB, pdf)
Shareable PDF
Acknowledgements
The authors thank Nobom Masimini (Wellcome Centre for Infectious Diseases Research in Africa, University of Cape Town, South Africa) for her help performing the lung function tests; the Tygerberg Pulmonary Function Unit for their spirometry training; and Shamila Manie (Dept of Physiotherapy, University of Cape Town, South Africa) for the loan of the spirometer.
Footnotes
This article has supplementary material available from erj.ersjournals.com
Support statement: The main study was supported by the European and Developing Countries Clinical Trials Partnership through a Strategic Primer Grant (SP.2011.41304.074) that was awarded to the University of Cape Town, the Institute of Tropical Medicine, and Imperial College London, funding from the Department of Science and Technology of the government of South Africa, grants (098316, 084323, 104803, 203135) from the Wellcome Trust, and a doctoral fellowship (awarded to C. Stek) from the Institute for Tropical Medicine. RJW is supported by the Francis Crick Institute which receives funding from UKRI (FC0010218), CRUK (FC00102180) and Wellcome (FC0010218).
Conflict of interest: B. Allwood has nothing to disclose.
Conflict of interest: E. Du Bruyn has nothing to disclose.
Conflict of interest: J. Buyze has nothing to disclose.
Conflict of interest: C. Schutz has nothing to disclose.
Conflict of interest: F. Thienemann has nothing to disclose.
Conflict of interest: A. Lombard has nothing to disclose.
Conflict of interest: R.J. Wilkinson reports grants from Wellcome, UK Research and Innovation, National Institutes of Health, Foundation for the National Institutes of Health and the European and Developing Countries Clinical Trials Partnership, during the conduct of the study.
Conflict of interest: G. Meintjes has nothing to disclose.
Conflict of interest: L. Lynen has nothing to disclose.
Conflict of interest: C. Stek has nothing to disclose.
References
- 1.Pefura-Yone EW, Balkissou AD, Kengne AP. Determinants of restrictive spirometric pattern in a sub-Saharan urban setting: a cross-sectional population-based study. Open Respir Med J 2016; 10: 86–95. doi: 10.2174/1874306401610010086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Allwood BW, Myer L, Bateman ED. A systematic review of the association between pulmonary tuberculosis and the development of chronic airflow obstruction in adults. Respiration 2013; 86: 76–85. doi: 10.1159/000350917 [DOI] [PubMed] [Google Scholar]
- 3.Akkara SA, Shah AD, Adalja M, et al. Pulmonary tuberculosis: the day after. Int J Tuberc Lung Dis 2013; 17: 810–813. doi: 10.5588/ijtld.12.0317 [DOI] [PubMed] [Google Scholar]
- 4.Manji M, Shayo G, Mamuya S, et al. Lung functions among patients with pulmonary tuberculosis in Dar es Salaam – a cross-sectional study. BMC Pulm Med 2016; 16: 58. doi: 10.1186/s12890-016-0213-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mbatchou Ngahane BH, Nouyep J, Nganda Motto M, et al. Post-tuberculous lung function impairment in a tuberculosis reference clinic in Cameroon. Respir Med 2016; 114: 67–71. doi: 10.1016/j.rmed.2016.03.007 [DOI] [PubMed] [Google Scholar]
- 6.de Vallière S, Barker RD. Residual lung damage after completion of treatment for multidrug-resistant tuberculosis. Int J Tuberc Lung Dis 2004; 8: 767–771. [PubMed] [Google Scholar]
- 7.Singla R, Mallick M, Mrigpuri P, et al. Sequelae of pulmonary multidrug-resistant tuberculosis at the completion of treatment. Lung India 2018; 35: 4–8. doi: 10.4103/lungindia.lungindia_269_16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fitzpatrick ME, Kunisaki KM, Morris A. Pulmonary disease in HIV-infected adults in the era of antiretroviral therapy. AIDS 2018; 32: 277–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pefura-Yone EW, Fodjeu G, Kengne AP, et al. Prevalence and determinants of chronic obstructive pulmonary disease in HIV infected patients in an African country with low level of tobacco smoking. Respir Med 2015; 109: 247–254. doi: 10.1016/j.rmed.2014.12.003 [DOI] [PubMed] [Google Scholar]
- 10.Ralph AP, Kenangalem E, Waramori G, et al. High morbidity during treatment and residual pulmonary disability in pulmonary tuberculosis: under-recognised phenomena. PLoS One 2013; 8: e80302. doi: 10.1371/journal.pone.0080302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fiogbe AA, Agodokpessi G, Tessier JF, et al. Prevalence of lung function impairment in cured pulmonary tuberculosis patients in Cotonou, Benin. Int J Tuberc Lung Dis 2019; 23: 195–202. doi: 10.5588/ijtld.18.0234 [DOI] [PubMed] [Google Scholar]
- 12.Kwan CK, Ernst JD. HIV and tuberculosis: a deadly human syndemic. Clin Microbiol Rev 2011; 24: 351–376. doi: 10.1128/CMR.00042-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stek C, Allwood B, Walker NF, et al. The immune mechanisms of lung parenchymal damage in tuberculosis and the role of host-directed therapy. Front Microbiol 2018; 9: 2603. doi: 10.3389/fmicb.2018.02603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nakiwala JK, Walker NF, Diedrich CR, et al. Neutrophil activation and enhanced release of granule products in HIV-TB immune reconstitution inflammatory syndrome. J Acquir Immune Defic Syndr 2018; 77: 221–229. 10.1097/QAI.0000000000001582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ravimohan S, Tamuhla N, Kung SJ, et al. Matrix metalloproteinases in tuberculosis-immune reconstitution inflammatory syndrome and impaired lung function among advanced HIV/TB co-infected patients initiating antiretroviral therapy. EBioMedicine 2015; 3: 100–107. doi: 10.1016/j.ebiom.2015.11.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Walker NF, Wilkinson KA, Meintjes G, et al. Matrix degradation in human immunodeficiency virus type 1-associated tuberculosis and tuberculosis immune reconstitution inflammatory syndrome: a prospective observational study. Clin Infect Dis 2017; 65: 121–132. doi: 10.1093/cid/cix231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lai RP, Meintjes G, Wilkinson RJ. HIV-1 tuberculosis-associated immune reconstitution inflammatory syndrome. Semin Immunopathol 2016; 38: 185–198. doi: 10.1007/s00281-015-0532-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ravimohan S, Auld SC, Maenetje P, et al. Lung injury on antiretroviral therapy in adults with HIV/TB. Clin Infect Dis 2019 10.1093/cid/ciz560. In press doi: 10.1093/cid/ciz560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Auld SC, Maenetje P, Ravimohan S, et al. Declines in lung function after antiretroviral therapy initiation in adults with human immunodeficiency virus and tuberculosis: a potential manifestation of respiratory immune reconstitution inflammatory syndrome. Clin Infect Dis 2019 10.1093/cid/ciz733. In press doi: 10.1093/cid/ciz733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bongiovanni B, Mata-Espinosa D, D'Attilio L, et al. Effect of cortisol and/or DHEA on THP1-derived macrophages infected with Mycobacterium tuberculosis. Tuberculosis 2015; 95: 562–569. doi: 10.1016/j.tube.2015.05.011 [DOI] [PubMed] [Google Scholar]
- 21.Mayanja-Kizza H, Jones-Lopez E, Okwera A, et al. Immunoadjuvant prednisolone therapy for HIV-associated tuberculosis: a phase 2 clinical trial in Uganda. J Infect Dis 2005; 191: 856–865. doi: 10.1086/427995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Meintjes G, Skolimowska KH, Wilkinson KA, et al. Corticosteroid-modulated immune activation in the tuberculosis immune reconstitution inflammatory syndrome. Am J Respir Crit Care Med 2012; 186: 369–377. doi: 10.1164/rccm.201201-0094OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tadokera R, Meintjes GA, Wilkinson KA, et al. Matrix metalloproteinases and tissue damage in HIV-tuberculosis immune reconstitution inflammatory syndrome. Eur J Immunol 2014; 44: 127–136. doi: 10.1002/eji.201343593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Malik SK, Martin CJ. Tuberculosis, corticosteroid therapy, and pulmonary function. Am Rev Respir Dis 1969; 100: 13–18. [DOI] [PubMed] [Google Scholar]
- 25.Marcus H, Yoo OH, Akyol T, et al. A randomized study of the effects of corticosteroid therapy on healing of pulmonary tuberculosis as judged by clinical, roentgenographic, and physiologic measurements. Am Rev Respir Dis 1963; 88: 55–64. [DOI] [PubMed] [Google Scholar]
- 26.Angel JH, Chu LS, Lyons HA. Corticotropin in the treatment of tuberculosis. A controlled study. Arch Intern Med 1961; 108: 353–369. doi: 10.1001/archinte.1961.03620090025004 [DOI] [PubMed] [Google Scholar]
- 27.Park IW, Choi BW, Hue SH. Prospective study of corticosteroid as an adjunct in the treatment of endobronchial tuberculosis in adults. Respirology 1997; 2: 275–281. doi: 10.1111/j.1440-1843.1997.tb00089.x [DOI] [PubMed] [Google Scholar]
- 28.Meintjes G, Stek C, Blumenthal L, et al. Prednisone for the prevention of paradoxical tuberculosis-associated IRIS. N Engl J Med 2018; 379: 1915–1925. doi: 10.1056/NEJMoa1800762 [DOI] [PubMed] [Google Scholar]
- 29.Meintjes G, Lawn SD, Scano F, et al. Tuberculosis-associated immune reconstitution inflammatory syndrome: case definitions for use in resource-limited settings. Lancet Infect Dis 2008; 8: 516–523. doi: 10.1016/S1473-3099(08)70184-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Department of Health, Republic of South Africa. 2014. National Tuberculosis Management Guidelines https://health-e.org.za/wp-content/uploads/2014/06/NTCP_Adult_TB-Guidelines-27.5.2014.pdf.
- 31.Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J 2005; 26: 319–338. doi: 10.1183/09031936.05.00034805 [DOI] [PubMed] [Google Scholar]
- 32.ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med 2002; 166: 111–117. doi: 10.1164/ajrccm.166.1.at1102 [DOI] [PubMed] [Google Scholar]
- 33.Kriel M, Lotz JW, Kidd M, et al. Evaluation of a radiological severity score to predict treatment outcome in adults with pulmonary tuberculosis. Int J Tuberc Lung Dis 2015; 19: 1354–1360. doi: 10.5588/ijtld.15.0098 [DOI] [PubMed] [Google Scholar]
- 34.Gupte AN, Wong ML, Msandiwa R, et al. Factors associated with pulmonary impairment in HIV-infected South African adults. PLoS One 2017; 12: e0184530. doi: 10.1371/journal.pone.0184530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Arlettaz A, Portier H, Lecoq AM, et al. Effects of short-term prednisolone intake during submaximal exercise. Med Sci Sports Exerc 2007; 39: 1672–1678. doi: 10.1249/mss.0b013e3180dc992c [DOI] [PubMed] [Google Scholar]
- 36.Singh JM, Palda VA, Stanbrook MB, et al. Corticosteroid therapy for patients with acute exacerbations of chronic obstructive pulmonary disease: a systematic review. Arch Intern Med 2002; 162: 2527–2536. doi: 10.1001/archinte.162.22.2527 [DOI] [PubMed] [Google Scholar]
- 37.North CM, Muyanja D, Kakuhikire B, et al. Systemic inflammation, immune activation and impaired lung function among people living with HIV in rural Uganda. J Acquir Immune Defic Syndr 2018; 78: 543–548. doi: 10.1097/QAI.0000000000001711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Báez-Saldaña R, López-Arteaga Y, Bizarrón-Muro A, et al. A novel scoring system to measure radiographic abnormalities and related spirometric values in cured pulmonary tuberculosis. PLoS One 2013; 8: e78926. doi: 10.1371/journal.pone.0078926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Plit ML, Anderson R, Van Rensburg CE, et al. Influence of antimicrobial chemotherapy on spirometric parameters and pro-inflammatory indices in severe pulmonary tuberculosis. Eur Respir J 1998; 12: 351–356. doi: 10.1183/09031936.98.12020351 [DOI] [PubMed] [Google Scholar]
- 40.Gandhi K, Gupta S, Singla R. Risk factors associated with development of pulmonary impairment after tuberculosis. Indian J Tuberc 2016; 63: 34–38. doi: 10.1016/j.ijtb.2016.01.006 [DOI] [PubMed] [Google Scholar]
- 41.Musafiri S, van Meerbeeck JP, Musango L, et al. Spirometric reference values for an East-African population. Respiration 2013; 85: 297–304. doi: 10.1159/000337256 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Please note: supplementary material is not edited by the Editorial Office, and is uploaded as it has been supplied by the author.
Supplementary material ERJ-01692-2019.SUPPLEMENT (464.5KB, pdf)
This one-page PDF can be shared freely online.
Shareable PDF ERJ-01692-2019.Shareable (332.3KB, pdf)