Abstract
West Virginia is the epicenter of a national opioid crisis. We examine trends in treatment for opioid use disorder (OUD) among individuals enrolled in the West Virginia Medicaid expansion program under the Affordable Care Act using 2014–2016 claims data. Expanding Medicaid could provide services to populations that may previously have had limited access to OUD treatment. We thus sought to understand trends over time in OUD diagnosis and treatment, especially with medications. About 5.5% of all enrollees were diagnosed with OUD per year, and the monthly prevalence of OUD diagnoses nearly tripled during this three-year period. The ratio of individuals filling buprenorphine to the number diagnosed with OUD was around one-third in early 2014, increasing to more than 75% by late 2016. Mean annual duration of filled buprenorphine increased from 161 days in 2014 to 185 days in 2016, and most individuals filling buprenorphine also received counseling and drug testing during the study period. The growing use of medication treatment for OUD in the West Virginia Medicaid expansion provides an opportunity to reduce overdose deaths.
Keywords: Affordable Care Act, Medicaid, opioid use disorder, access to care
INTRODUCTION
West Virginia is the epicenter of a national opioid overdose crisis. In 2016, West Virginia had a fatal opioid overdose rate of 43.4 per 100,000 – more than triple the US average of 13.3 per 100,000.(1) Most opioid overdose fatalities in West Virginia can be linked to heroin and illicit fentanyl.(2) The West Virginia crisis has strained the capacity of health care providers, law enforcement, and social service systems, and has exacted a considerable toll on many communities.(3)
Given the high uninsured and poverty rates in West Virginia that preceded the Affordable Care Act (ACA), Medicaid expansion could be one tool to address the opioid crisis. The expansion provided Medicaid eligibility for the first time to many adults with incomes below 138 percent of the federal poverty level, a population that has elevated burden of substance use disorders. West Virginia was one of the 25 states plus the District of Columbia that implemented the optional Medicaid expansion starting in January 2014. By early 2016, there were 180,500 individuals enrolled in the West Virginia Medicaid expansion,(4)compared to the pre-ACA monthly Medicaid average of 354,444(5). The non-elderly adult uninsured rate in the state dropped from 29% in 2013 to 9% in 2015.(6) News media coverage highlights that the West Virginia Medicaid expansion has provided insurance coverage for treatment for previously ineligible low-income adults, but that there remains inadequate access to health care providers in the state.(7,8)
Substance use disorder treatment is a required benefit in ACA Medicaid expansion programs, but states have leeway in defining the benefit package.(9) In particular, states select which medications for opioid use disorder treatment (methadone, buprenorphine, and naltrexone) to include in their benefit package.(10) While methadone and buprenorphine are effective at increasing abstinence and reducing overdose risk,(11) there is pervasive stigma against these medications.(12) Buprenorphine can be prescribed by waivered office-based physicians, whereas methadone is only available through opioid treatment programs. Naltrexone is most commonly administered as a long-acting injection. It requires individuals to be fully withdrawn from opioids to begin treatment, which limits the number of individuals able to initiate it.(11) At the time of the 2014 Medicaid expansion, West Virginia did not cover methadone maintenance, and it required patients taking buprenorphine and naltrexone to receive concurrent counseling (13) and to receive prior authorization.(13)
This study examines patterns of service use related to treatment for OUD, including initiation and duration of pharmacologic and nonpharmacologic treatment, in the West Virginia Medicaid expansion program. It builds upon recent national studies that leverage data from across expansion and non-expansion states. A recent study using national survey data found that the ACA increased the number of low-income people with Medicaid coverage in substance use disorder treatment, but did not increase overall entry to treatment.(14) By contrast, another study using data from specialty care providers found that admissions to treatment for opioid use disorder increased substantially in expansion states relative to non-expansion states, especially in those states where state Medicaid covered methadone maintenance.(15) Other studies focusing specifically on buprenorphine found that prescriptions for buprenorphine paid for by Medicaid increased rapidly after expansion,(16) leading to an increase in the number of people utilizing buprenorphine in expansion states compared to non-expansion states.(17)
In sum, existing literature suggests that Medicaid expansion is picking up a growing share of the cost for OUD medication treatment in expansion states and that Medicaid may in particular be driving an increase in buprenorphine treatment. There may also be constraints, however, such as benefit design limitations or lack of adequate supply of prescribing providers, that hinder greater receipt of medication treatment among newly Medicaid-eligible individuals. Moreover, it is unknown how much of the Medicaid expansion is funding medication treatment for OUD versus other treatment modalities (e.g., counseling for OUD without medication). Questions also remain regarding how individuals are navigating treatment on the ground, such as what barriers exist to ongoing medication treatment following initiation.
Our study uses longitudinal claims data from West Virginia Medicaid and considers multiple treatment approaches (e.g., types of medications used, receipt of counseling, and drug testing) and measures of treatment duration that may speak to the quality and scope of care being received. A clearer analysis of these factors can be useful for policymakers seeking to build upon the Medicaid expansion.
DATA AND METHODS
Data
Through a data use agreement with the West Virginia Department of Health and Human Resources, we obtained the full sample of Medicaid-reimbursed inpatient, outpatient and pharmacy claims for all individuals enrolled in the West Virginia Medicaid program under ACA eligibility criteria for calendar years 2014–2016. The Medicaid expansion population is defined in the claims data using specific eligibility codes and thus encompasses only individuals who are newly eligible specifically under ACA provisions in 2014. Until the third quarter of 2015, West Virginia Medicaid expansion enrollees were primarily enrolled in Medicaid fee-for-service, after which the state transitioned to managed care.(18) For all individuals, we identified demographics (age, sex, race/ethnicity), county of residence, and number of months of enrollment using the eligibility file. We identified individuals with OUD based on the presence of a diagnosis code for OUD (ICD9: 304.0X, 305.5X; ICD10: F11.X) in any position on at least one claim. For buprenorphine and naltrexone (of any formulation), we identified therapeutic groups using the First Data Bank three-digit hierarchical ingredient code (HIC3) classification. Finally, using diagnosis codes we also created indicators for 14 common chronic conditions (hypertension, hyperlipidemia, atherosclerosis, asthma, chronic obstructive pulmonary disease, arthritis, diabetes, depression, anxiety disorder, bipolar disorder, hepatitis C, HIV, alcohol use disorder, and chronic pain).
For our primary analysis, we aggregated data into person years. We created counts of outpatient visits that included an OUD diagnosis and classified claims with these diagnosis into visit types using the claim’s primary Current Procedural Technology (CPT) code. To define service categories, we looked for clinically meaningful groupings of procedure codes. Specifically, we identified claims for behavioral health counseling (e.g., H0004 “Behavioral health counseling and therapy, per 15 minutes”), evaluation and management (e.g., 99213, “Office or other outpatient visit for established patient; low or moderate severity problem”), and all other services (e.g., T1017 “targeted case management”). We also counted the number of days with drug testing (“labs”) that included a diagnosis code for OUD (e.g., 81005 “Urinalysis”). Using the number of prescriptions and days supplied, we calculated the number of days individuals had a filled prescription for buprenorphine or naltrexone. As noted, methadone for OUD was not reimbursed by Medicaid during this time period.
Using adapted Census-based categories,(19) we also identified whether individuals reside in a metropolitan county (counties that contains a core city), a county adjacent to a metropolitan area (suburban counties), and counties not in a metropolitan area (rural counties).
Methods
We conducted both month-level and aggregated annual analyses. For annual measures, we restricted to individuals enrolled for at least 10 months of the calendar year. For month-level analyses, we did not impose the 10 month continuous enrollment requirement and examined the number of individuals who had a diagnosis of OUD in a month and the number of individuals filling buprenorphine and naltrexone. We calculated summary statistics of all other utilization and spending measures on an annual basis, and for continuous measures calculated means and medians. We calculated two-tailed Chi-squares tests for differences in means across years or groups, using p<.05 as the threshold for statistical significance.
To further examine predictors of treatment utilization, we pooled person-year data from the three years and estimated separate logistic regression models where the outcomes were fills for buprenorphine, fills for naltrexone, and utilization of counseling treatment without buprenorphine or naltrexone among individuals in the calendar year in which individuals had an OUD diagnosis (note that individuals could appear in both the buprenorphine and naltrexone models if they filled prescriptions for both medications in the study period). The medications are separately considered because they have different clinical profiles and may be administered to different populations. Predictors in these models were individual demographics (age, sex, race/ethnicity), presence of each of the 14 comorbidities in the calendar year, and county urban-suburban-rural status.
Limitations
Several limitations should be considered. First, data from West Virginia do not necessarily generalize to other state Medicaid expansion programs. West Virginia was the focus of this study because of both the high pre-ACA uninsured rates and because of the severity of the opioid crisis, making it likely that large numbers of individuals in the expansion population would need OUD treatment. However, West Virginia did not cover methadone maintenance during the study period, which is likely to be an important pathway into treatment in other states. West Virginia is among the most rural states, and care-seeking patterns are likely to be different in more urban states.
Second, we do not have a comparison group, such as individuals not eligible for Medicaid expansion or eligible individuals who did not enroll, preventing us from drawing causal inferences about the likely effect of Medicaid expansion on use of treatment or quality of care. Furthermore, we were unable to obtain contemporaneous data on other populations (e.g., our data use agreement did not provide access to data on Medicaid populations outside the ACA expansion). Relatedly, without pre-Medicaid enrollment data we cannot determine whether our study population had insurance coverage, access to treatment, or received any treatment, prior to the 2014 expansion. This precludes any pre-post comparison. However, it is reasonable to assume that the large majority of individuals in the ACA expansion population were previously uninsured (as has been found using national data(20)). Our study findings have descriptive value as relatively little is known about treatments used by people enrolled in the ACA Medicaid expansion.
Third, because we focus only on services with an OUD diagnosis code, we may miss services provided to individuals in this population for related conditions that may have also treated OUD (e.g., counseling for depression). Finally, we are inherently limited by claims data in our ability to examine clinically important treatment markers such as rates of abstinence and health-related quality of life.
RESULTS
Exhibit 1 displays the demographic characteristics of the full Medicaid expansion population in West Virginia (N=349,927 person-years) and those diagnosed with OUD (N=19,318 person-years) cumulatively for 2014–2016. On average, in the first three years of Medicaid expansion, 5.5% of all enrollees had a claim with an OUD diagnosis in the calendar year.
Exhibit 1.
Demographics and County Characteristics of Individuals Enrolled in the West Virginia Medicaid Expansion Overall and Individuals with OUD, 2014 to 2016
| N | 349,927 | 19,318 | 330,609 | |
| Mean Age in Years | 38.8743 | 34.35573 | 39.13833 | *** |
| Male | 47.22% | 57.97% | 46.59% | *** |
| Female | 52.78% | 42.03% | 53.41% | *** |
| Race/Ethnicity | ||||
| Non-Hispanic White | 89.86% | 90.70% | 89.81% | *** |
| Non-Hispanic Black | 4.10% | 1.65% | 4.24% | *** |
| Hispanic | 0.61% | 2.69% | 0.49% | *** |
| Other Race | 5.43% | 4.97% | 5.46% | ** |
| Rural-suburban-urban status | ||||
| In an MSA | 56.99% | 64.45% | 56.56% | *** |
| Suburban, adjacent to an MSA | 28.63% | 24.56% | 28.87% | *** |
| Rural, non-adjacent to MSA | 14.38% | 10.99% | 14.58% | *** |
| Chronic Condition | ||||
| Any Chronic Condition | 38.07% | 52.38% | 37.23% | *** |
| Hypertension | 12.99% | 10.00% | 13.16% | *** |
| Hyperlipidemia | 5.80% | 2.52% | 6.00% | *** |
| Atherosclerosis | 0.43% | 0.28% | 0.44% | ** |
| Asthma | 2.57% | 2.45% | 2.57% | |
| COPD | 3.22% | 3.41% | 3.21% | |
| Arthritis | 5.72% | 4.34% | 5.80% | *** |
| Diabetes | 7.32% | 3.57% | 7.54% | *** |
| Depression | 7.62% | 21.13% | 6.83% | *** |
| Anxiety Disorder | 6.59% | 14.92% | 6.10% | *** |
| Bipolar Disorder | 2.97% | 10.06% | 2.56% | *** |
| Hepatitis C | 1.14% | 7.31% | 0.78% | *** |
| HIV | 0.12% | 0.22% | 0.12% | *** |
| Alcohol Use Disorder | 1.14% | 4.62% | 0.93% | *** |
| Chronic Pain | 1.33% | 3.00% | 1.23% | *** |
Source: Authors’ analysis of West Virginia Medicaid expansion claims data 2014–2016.
Notes: Rural-urban status is determined using the urban-rural continuum code scores. Each observation in this table represents a unique individual with at least 10 months of data during one of the three years from 2014 to 2016. P-value for pairwise t-test between people diagnosed with opioid use disorder and those without opioid use disorder diagnosis.
P<.05,
P<.01,
P<.001
People with OUD were younger than people without OUD (mean age 34.4 versus 39.1), more likely to be male (58.0% versus 46.6%), more likely to be Hispanic (2.7% versus 0.5%,), less likely to be African American (1.7% versus 4.2%), and more likely to reside in urban areas (64.5% versus 56.6%). All differences were statistically significant (p<.001). Compared to people without OUD, people with OUD were significantly more likely to have a non-OUD diagnosed chronic condition (52.4% versus 37.2%), to have diagnosed mental health conditions such as depression (21.1% versus 6.8%), %), anxiety disorder (14.9% versus 6.1%), and bipolar disorder (10.1% versus 2.6%); and to have diagnoses of alcohol use disorder (4.6% versus 0.9%) and chronic pain (3.0% versus 1.2%). They were significantly less likely than other enrollees to have diagnosed cardiovascular diseases than those without OUD, such as hypertension (10.0% versus 13.2%).
Exhibit 2 shows monthly trends from 2014 to 2016 in the percentage of enrollees who had a claim with a diagnosis of OUD in each month and the percentages receiving buprenorphine and naltrexone. Of note, rates for month-level calculations will be lower than annual rates because they pertain to individuals using services specifically in the particular study month rather than any time in the year. A gray box is overlaid on the second half of 2015 when the state transitioned to managed care (on July 1). There appears to be underreporting of outpatient claims during this time, but data become more consistent in early 2016. Diagnosed monthly prevalence of OUD more than doubled during the study period from 1.0% in January 2014 to 2.4% in December 2016. The monthly prevalence of buprenorphine use increased sixfold, from 0.3% in January 2014 of the sample to 1.8% in December 2016. The ratio between the percentage of individuals treated with buprenorphine to those with an OUD diagnosis increased from less than one-third in January 2014 to more than 75% in December 2016. The monthly percentage of people with OUD receiving naltrexone increased from 0.04% in January 2014 to 0.11% in December 2016, a nearly threefold increase. However, this represented less than 5% of all individuals with OUD in any given month of the study period.
Exhibit 2. Monthly Percentages of the Medicaid Expansion Population with an OUD Diagnosis and Receiving Buprenorphine or Naltrexone.
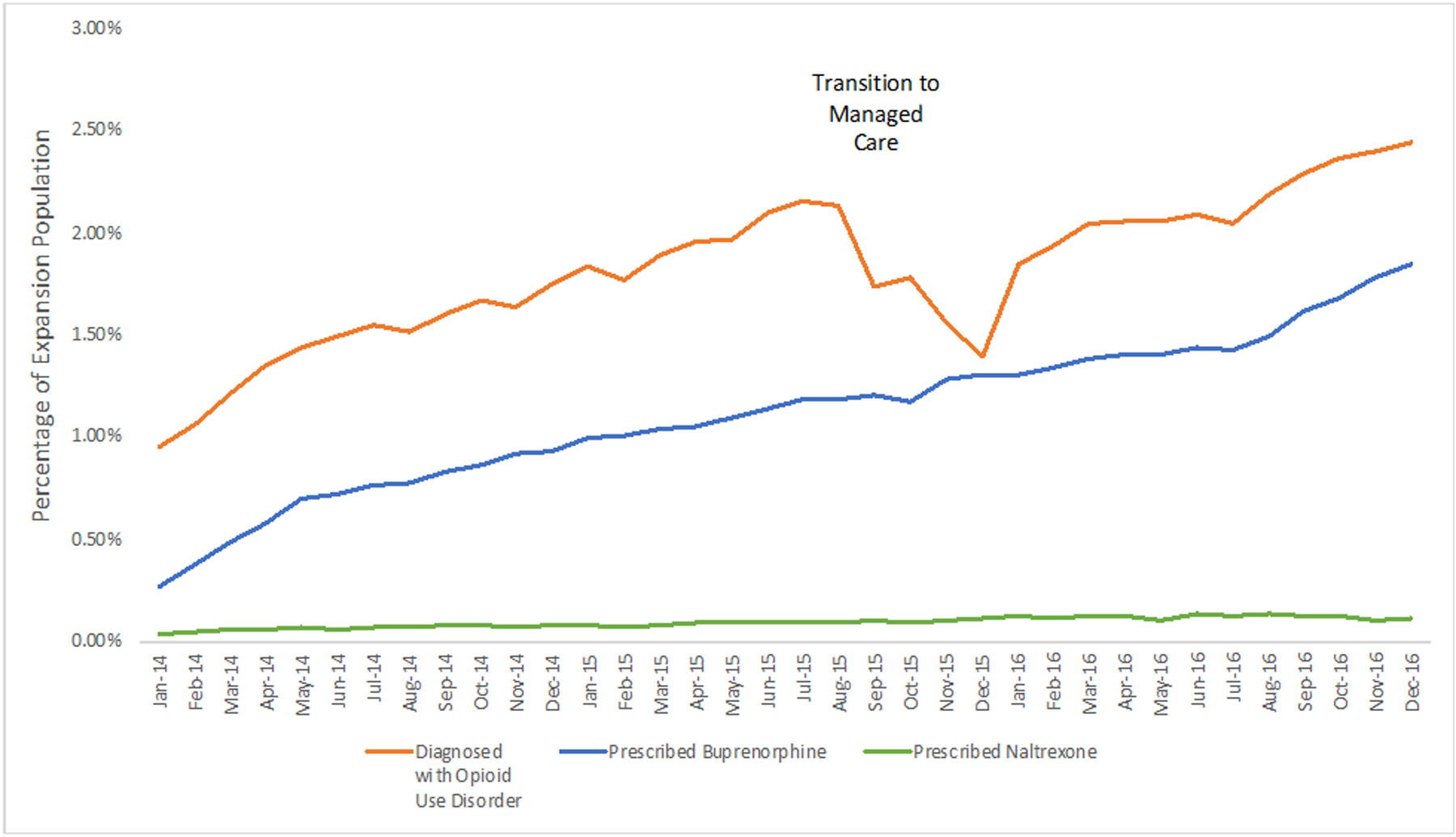
Source: Authors’ analysis of West Virginia Medicaid expansion claims data 2014–2016.
Notes: Monthly average are calculated as the percentage of all Medicaid expansion enrollees in the month with either a claim that included a diagnosis for an opioid use disorder, a prescription filled for buprenorphine, or a prescription filled for naltrexone. The gray box indicates the period when the state transitioned the Medicaid expansion population from fee-for-service to managed care.
| Month | Diagnosed with Opioid Use Disorder | Prescribed Buprenorphine | Prescribed Naltrexone |
|---|---|---|---|
| Jan-14 | 0.90% | 0.27% | 0.04% |
| Feb-14 | 1.02% | 0.38% | 0.05% |
| Mar-14 | 1.18% | 0.49% | 0.06% |
| Apr-14 | 1.30% | 0.58% | 0.05% |
| May-14 | 1.39% | 0.69% | 0.07% |
| Jun-14 | 1.46% | 0.72% | 0.06% |
| Jul-14 | 1.50% | 0.76% | 0.07% |
| Aug-14 | 1.48% | 0.78% | 0.07% |
| Sep-14 | 1.56% | 0.83% | 0.08% |
| Oct-14 | 1.63% | 0.87% | 0.08% |
| Nov-14 | 1.60% | 0.92% | 0.07% |
| Dec-14 | 1.70% | 0.93% | 0.08% |
| Jan-15 | 1.80% | 1.00% | 0.08% |
| Feb-15 | 1.73% | 1.01% | 0.07% |
| Mar-15 | 1.84% | 1.04% | 0.08% |
| Apr-15 | 1.92% | 1.05% | 0.09% |
| May-15 | 1.93% | 1.09% | 0.09% |
| Jun-15 | 2.06% | 1.13% | 0.10% |
| Jul-15 | 2.11% | 1.18% | 0.09% |
| Aug-15 | 2.10% | 1.18% | 0.09% |
| Sep-15 | 1.70% | 1.21% | 0.10% |
| Oct-15 | 1.77% | 1.17% | 0.09% |
| Nov-15 | 1.55% | 1.28% | 0.10% |
| Dec-15 | 1.39% | 1.30% | 0.11% |
| Jan-16 | 1.84% | 1.30% | 0.12% |
| Feb-16 | 1.93% | 1.34% | 0.11% |
| Mar-16 | 2.04% | 1.38% | 0.12% |
| Apr-16 | 2.05% | 1.41% | 0.13% |
| May-16 | 2.06% | 1.40% | 0.10% |
| Jun-16 | 2.09% | 1.43% | 0.13% |
| Jul-16 | 2.05% | 1.42% | 0.12% |
| Aug-16 | 2.18% | 1.49% | 0.14% |
| Sep-16 | 2.29% | 1.61% | 0.12% |
| Oct-16 | 2.36% | 1.67% | 0.13% |
| Nov-16 | 2.39% | 1.77% | 0.11% |
| Dec-16 | 2.44% | 1.84% | 0.11% |
Exhibit 3 provides information on the service utilization characteristics of individuals with diagnosed OUD overall, and the subgroups who used either any buprenorphine or any naltrexone in 2014–2016. It also provides p-values for tests of significant time trends in means over the three-year period. In 2014, individuals with OUD received an average of 6.6 behavioral counseling sessions, 5.3 drug tests, and 5.4 evaluation and maintenance visits. However, these data are skewed by high utilizers as the median for each of these measures is only 0 or 1 service received. The mean number of counseling sessions did not significantly change. However, there was a significant increase over time in the mean number of drug tests (p<.001) and office visits for OUD (p<.001).
Exhibit 3.
Average Annual Outpatient Services Used Among Individuals with OUD, and subsets receiving Buprenorphine and Naltrexone, 2014 – 2016
| 2014 | 2015 | 2016 | P-Value | |
|---|---|---|---|---|
| All Individuals with Diagnosed OUD | 4,144 | 6,856 | 8,318 | |
| Percent with any counseling | 60.91% | 62.08% | 60.69% | *** |
| Mean number of counseling sessions | 6.6 | 7.0 | 6.6 | |
| Percent with any drug tests | 1 | 1 | 1 | |
| Mean number of drug tests | 44.31% | 50.54% | 56.42% | *** |
| Median number of labs | 5.3 | 5.5 | 6.3 | *** |
| Percent with any evaluation & management visits | 0 | 1 | 1 | |
| Mean number evaluation & management visits | 62.45% | 68.28% | 71.81% | *** |
| Median number evaluation & management visits | 5.4 | 5.6 | 7.0 | *** |
| Percent any buprenorphine | 1 | 2 | 2 | |
| Percent any naltrexone | 32.70% | 40.94% | 45.72% | *** |
| Percent with counseling only | 4.87% | 5.88% | 6.91% | *** |
| All Individuals with OUD and Buprenorphine Fills | 30.77% | 26.37% | 22.39% | *** |
| Mean days supply buprenorphine | 1,355 | 2,807 | 3,803 | |
| Median days supply buprenorphine | 161.3 | 183.4 | 185.3 | *** |
| Percent with any counseling | 140 | 161 | 168 | |
| Mean number of counseling sessions | 17.5 | 18.2 | 18.5 | * |
| Median number of counseling sessions | 15 | 16 | 16 | |
| Percent of with any drug tests | 82.66% | 78.34% | 74.97% | *** |
| Mean number of drug tests | 11.9 | 11.3 | 9.3 | *** |
| Median number of drug tests | 8 | 6 | 5 | |
| Percent with any evaluation & management visits | 89.59% | 87.64% | 85.83% | *** |
| Mean number evaluation & management visits | 14.8 | 12.3 | 12.3 | *** |
| Median number evaluation & management visits | 11 | 8 | 8 | |
| All Individuals with OUD and Naltrexone Fills | 89.59% | 93.05% | 91.61% | *** |
| Mean days supply of naltrexone | 13.9 | 11.9 | 13.5 | |
| Median days supply of naltrexone | 11 | 8 | 10 | |
| Percent with any counseling | 202 | 403 | 575 | |
| Mean number of counseling sessions | 57.5 | 43.6 | 38.3 | *** |
| Median number of counseling sessions | 30 | 30 | 29 | |
| Percent with any drug test | 2.3 | 1.9 | 1.9 | * |
| Mean number of drug tests | 1 | 1 | 1 | |
| Median number of drug tests | 73.76% | 75.68% | 71.30% | *** |
| Percent with any evaluation & management visits | 11.2 | 9.8 | 9.6 | |
| Mean number evaluation & management visits | 3 | 3 | 3 | |
| Median number evaluation & management visits | 46.04% | 48.64% | 60.17% | *** |
Source: Authors’ analysis of West Virginia Medicaid expansion claims data 2014–2016.
Notes: Drug tests, counseling sessions, and physician visits defined using procedure codes. Medication fills determined using three-level hierarchical ingredient code (HIC3) codes. Each observation in these tables is a person year with at least 10 months of enrollment in the Medicaid expansion. N.A. is displayed next to median statistics because p-values were not calculated for changes in medians.
P<.05,
P<.01,
P<.001
In 2014, individuals who received any buprenorphine received an average of 11.9 behavioral counseling sessions, had an average of 14.8 drug tests, and 13.9 evaluation and management visits. At the mean, these individuals also received 161.3 days of buprenorphine (the median was 140) in 2014. The mean number of days significantly increased to 185.3 by 2016 (p<.001). Among people using buprenorphine, there were significant decreases over time in the mean number of counseling sessions (p<.001) and drug tests (p<.001). Individuals using naltrexone had shorter average duration of medication use: at the mean they only received about 57.5 days of naltrexone treatment (the median was 30 days in 2014). This significantly decreased over the study period to 38.3 days by 2016 (p<.001). They received an average of 11.2 counseling sessions, 3.1 drug tests, and 3.6 physician visits in 2014. These indicators did not significantly change during the study period.
Exhibit 4 provides odds ratios from logistic regression models predicting fills of buprenorphine, fills of naltrexone, and utilization of counseling without medication, in each calendar year where individuals had a diagnosis of OUD, combining data across the three study years.
Exhibit 4.
Odds Ratios for Logistic Regressions Predicting Fills for Buprenorphine, Naltrexone, and Receipt of Counseling Without Medication
| Buprenorphine | Naltrexone | Counseling without Medication | |
|---|---|---|---|
| Variable | OR | OR | OR |
| Race/Ethnicity (Ref=NH white) | |||
| Black | 0.47*** | 1.76** | 1.27 |
| Hispanic | 0.59*** | 2.29*** | 1.74*** |
| Other Race/Ethnic | 0.81** | 0.96 | 1.05 |
| Sex (Ref=Male) | |||
| Female | 0.99 | 1.03 | 0.9** |
| Age (Ref=25–34) | |||
| <25 | 0.64*** | 1.08 | 1.45*** |
| 35–44 | 1.09* | 0.92 | 0.83*** |
| 45–54 | 0.9 | 0.77* | 0.62*** |
| >54 | 0.57*** | 0.26*** | 0.66*** |
| Chronic conditions | |||
| Hypertension | 0.83** | 1.06 | 0.88* |
| Hyperlipidemia | 0.73** | 1.14 | 1.17 |
| Atherosclerosis | 0.77 | 0.87 | 0.93 |
| Asthma | 0.83 | 0.89 | 0.88 |
| COPD | 1.04 | 1.02 | 0.89 |
| Arthritis | 0.77** | 0.66* | 1.04 |
| Diabetes | 0.85 | 0.77 | 0.87 |
| Depression | 0.65*** | 2.11*** | 1.49*** |
| Anxiety Disorder | 0.79*** | 1.13 | 1.29*** |
| Bipolar Disorder | 0.71*** | 1.45*** | 1.26*** |
| Hepatitis C | 0.97 | 1.46*** | 1.08 |
| HIV | 0.51 | 0.57 | 1.13 |
| Alcohol Use Disorder | 0.4*** | 3.39*** | 1.55*** |
| Chronic Pain | 0.61*** | 0.46** | 0.66*** |
| Metro status (Ref=Urban) | |||
| Suburban | 1.11** | 0.97 | 1.02 |
| Rural | 1.52*** | 0.6*** | 0.83** |
Source: Authors’ analysis of West Virginia Medicaid expansion claims data 2014–2016.
Notes: Analyses includes individuals with >10 months enrollment in any year 2014–2016 (N=19,093). Separate models were estimated to predict the odds of fills of buprenorphine and naltrexone and receipt of counseling without medication.
P<.05,
P<.01,
P<.001
Among individuals with OUD, odds of filling buprenorphine were significantly lower among Hispanics and Non-Hispanic blacks compared to non-Hispanic whites and were significantly lower among older individuals versus those age 25–34. Odds of filling buprenorphine were significantly lower among people with hypertension, hyperlipidemia, arthritis, depression, anxiety disorder, bipolar disorder, alcohol use disorder, and chronic pain, compared to people without these conditions. Compared to people in urban areas, people in suburban and rural areas were significantly more likely to fill prescriptions for buprenorphine.
Odds of filling naltrexone were significantly higher among Hispanics and non-Hispanic blacks compared to non-Hispanic whites. Compared to individuals age 25–34, older individuals were significantly less likely to fill naltrexone. Odds of filling naltrexone were significantly lower for people with comorbid arthritis and chronic pain, but significantly higher for people with depression, bipolar disorder, hepatitis C, and alcohol use disorder compared to people without these conditions. Compared to people in urban areas, people in rural areas were significantly less likely to fill naltrexone.
Odds of receiving counseling without medication were significantly higher for Hispanic individuals compared to non-Hispanic whites. Compared to individuals age 25–34, odds were significantly higher for individuals <25, and significantly lower for all older groups. Odds of receiving counseling without medication were significantly lower for individuals with comorbid hypertension and chronic pain, and higher for depression, anxiety disorder, bipolar disorder, and alcohol use disorder. Finally, odds were significantly lower for individuals in rural areas compared to those in urban areas.
DISCUSSION
We examined trends in utilization of OUD treatment among individuals enrolled in the West Virginia Medicaid expansion. We found that the diagnosed prevalence of OUD steadily grew during the 2014–2016 study period. Underscoring the scope of the West Virginia opioid crisis, the annual diagnosed OUD prevalence in the sample was 5.5%. This is dramatically higher than previously-reported rates reported for Medicaid enrollees with 2013 claims data where the national average was 0.9% and the West Virginia average was about 1.7%.(21) The true prevalence of OUD in the expansion population is likely to be much higher than our data indicate, given the considerable under identification of OUD, stigma, and under-coding of substance use disorders in claims data.(22)
The steady increase in diagnosed OUD may reflect a “ramp up” effect as it can take time for individuals to establish contact with care providers and receive screening or self-identify as wanting treatment. The share of individuals with an OUD diagnosis filling buprenorphine also increased during the study period: increasing from under one-third of individuals with an OUD diagnosis in the month in early 2014 to around three-quarters by late 2016. We also found that individuals were filling buprenorphine for slightly longer periods of time per year by 2016. Naltrexone fill rates were consistently lower than buprenorphine. While naltrexone fill rates increased substantially during the study period, average duration among people using naltrexone actually decreased over time.
The majority of individuals with buprenorphine also received counseling and drug tests. The counseling rates are consistent with state policy, as individuals in buprenorphine treatment in West Virginia Medicaid were required to receive counseling.(13) Providing these services could be one component of comprehensive addiction treatment, and counseling has been proposed as a process measure for quality treatment.(23) On the other hand, concerns have been expressed that requiring adherence to counseling requirements may reduce utilization of buprenorphine treatment, reducing the overall benefit to the diagnosed population. In particular, if counseling is a requirement of buprenorphine treatment, the requirement may make it more difficult for providers to deliver the treatment and may increase reluctance to participate among some individuals.(24) Some studies indicate that individuals receiving intensive counseling alongside buprenorphine do not fare better than those receiving medication without counseling.(25)
We also found that individuals who filled buprenorphine did so for just under half the days in the year, and that buprenorphine was on average filled for about three or four times more days per year than naltrexone. Prior studies have found that longer duration of medication is protective against overdose, but that duration of naltrexone is much shorter than buprenorphine(26). While the duration of buprenorphine we found is similar to other state averages during this period,(17) it underscores that there remains room to improve continuity and duration of treatment.
Among individuals with diagnosed OUD, we found striking differences in factors that predicted fills of buprenorphine and naltrexone versus treatment without medication. These differences are especially important given the substantially stronger evidence base supporting treatment with buprenorphine versus treatment without medication.(27) Naltrexone is a treatment that may be well-suited for some populations, but does not appear to be as protective against overdose risk when accounting for high rates of discontinuation.(28)
Relative to non-Hispanic whites, the odds of receiving counseling without medication were higher among Hispanics. Conversely, Blacks and Hispanics were significantly less likely than whites to receive buprenorphine, and more likely to use naltrexone. These differences may reflect racial/ethnic differences in perceived acceptability of using buprenorphine versus naltrexone or differences in provider attitudes about giving patients these treatments. Medication-free treatment versus buprenorphine and methadone use has previously been shown to be higher among non-white than white populations with OUD, and more common at treatment facilities serving non-white populations.(29) Conversely, buprenorphine treatment uptake among Medicaid enrollees is known to have been higher in lower-poverty, predominantly white communities.(30) As documented in prior studies, use of treatment with medication was inversely related to age among people with OUD.(31,32) Perhaps more surprisingly, people with comorbid psychiatric disorders like depression had significantly lower odds of treatment with buprenorphine and higher odds of treatment without medication or with naltrexone. One possibility is that these patients may be receiving a diagnosis from mental health professionals who do not prescribe buprenorphine, but are providing ongoing counseling for a comorbid mental health disorder and diagnose OUD as part of a broader treatment plan. Finally, individuals in rural areas were more likely than those in urban areas to receive buprenorphine but less likely to receive naltrexone. This is unexpected as access to care is generally worse in rural areas. Our finding but may reflect selection differences, as individuals who come forward to be diagnosed in rural areas may have higher acuity than those in more urban areas.
Our study adds to a growing literature on Medicaid expansion and the opioid crisis. Recent studies suggest that Medicaid expansion has been especially important in providing health insurance coverage to previously uninsured low-income adults with OUD and other substance use disorders and has increased the role of Medicaid in paying for treatment for these adults.(15,16,33) Less well understood, however, are the specific pathways through which individuals are accessing Medicaid-financed services for OUD. Our detailed longitudinal data provide new insights into the types of services individuals with OUD are receiving in the Medicaid expansion state that arguably has the most widespread and severe opioid crisis. Despite documented challenges related to access to OUD treatment in West Virginia,(34) our study finds a growing population of individuals in the Medicaid expansion receiving medication treatment.
Conclusions
In the first three years of Medicaid expansion, a growing number of West Virginians were treated for opioid use disorder, and treatment with buprenorphine was a major area of expansion. However, uptake of treatment was uneven, with substantial differences by race/ethnicity, rural status, and diagnosed comorbid health conditions. Our findings provide a baseline for further analysis on long-term changes in use of these services in the West Virginia Medicaid expansion, as well as an opportunity for further study of changes in benefit design. Most notably, in 2017 West Virginia received a Section 1115 waiver from the federal government in which it added methadone maintenance as a benefit and increased the full continuum of services reimbursed by Medicaid. Tracking trends in treatment over time can help inform efforts to provide all people with opioid use disorder access to the services that reduce overdose and promote recovery.
Contributor Information
Brendan Saloner, Johns Hopkins Bloomberg School of Public Health.
Rachel Landis, Johns Hopkins Bloomberg School of Public Health.
Bradley Stein, RAND Corporation.
Colleen L. Barry, Johns Hopkins Bloomberg School of Public Health.
References
- 1.Kaiser Family Foundation. Opioid Overdose Death Rates and All Drug Overdose Death Rates per 100,000 Population (Age-Adjusted) [Internet]. Kaiser Family Foundation. 2018. [cited 2018 Aug 13]. Available from: https://www.kff.org/other/state-indicator/opioid-overdose-death-rates/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Opioid%20Overdose%20Death%20Rate%20(Age-Adjusted)%22,%22sort%22:%22desc%22%7D [Google Scholar]
- 2.US Centers for Disease Control and Prevention. Synthetic Overdose Data [Internet]. US Centers for Disease Control and Prevention. 2016. [cited 2018 Aug 13]. Available from: https://www.cdc.gov/drugoverdose/data/fentanyl.html [Google Scholar]
- 3.Johnson J, Allen S, Coben J, Frattaroli S, Loudin S. West Virginia Opioid Response Plan. Charleston, WV: Johns Hopkins and Marshall University; 2018. [Google Scholar]
- 4.Kaiser Family Foundation. Medicaid in West Virginia [Internet]. 2017. [cited 2018 Aug 13]. Available from: http://files.kff.org/attachment/fact-sheet-medicaid-state-WV
- 5.Kaiser Family Foundation. Total Monthly Medicaid and CHIP Enrollment [Internet]. 2016. [cited 2018 Dec 10]. Available from: https://www.kff.org/health-reform/state-indicator/total-monthly-medicaid-and-chip-enrollment/?currentTimeframe=31&selectedRows=%7B%22states%22:%7B%22west-virginia%22:%7B%7D%7D%7D&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D
- 6.Cohen R, Martinez M, Zammitti E. Health Insurance Coverage: Early Release of Estimates From the National Health Interview Survey, 2015. Rockville, MD: National Center for Health Statistics; 2016. [Google Scholar]
- 7.Alonso-Zaldivar R Republicans’ Medicaid Rollback Collides With Opioid Epidemic. Available from: https://www.usnews.com/news/best-states/kentucky/articles/2017-06-20/gops-health-care-rollback-collides-with-the-opioid-epidemic
- 8.Beck E Revised GOP health bill doesn’t do enough to combat opioid epidemic, experts say [Internet]. WV Gazette Mail. 2017. [cited 2018 Aug 13]. Available from: https://www.wvgazettemail.com/news/health/revised-gop-health-bill-doesn-t-do-enough-to-combat/article_abef502a-4e4e-5405-aa0c-35c41ee45e52.html [Google Scholar]
- 9.Beronio K, Glied S, Frank R. How the Affordable Care Act and Mental Health Parity and Addiction Equity Act Greatly Expand Coverage of Behavioral Health Care. J Behav Health Serv Res. 2014. October;41(4):410–28. [DOI] [PubMed] [Google Scholar]
- 10.Andrews CM, Grogan CM, Smith BT, Abraham AJ, Pollack HA, Humphreys K, et al. Medicaid Benefits For Addiction Treatment Expanded After Implementation Of The Affordable Care Act. Health Aff (Millwood). 2018. August;37(8):1216–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Institute on Drug Abuse (NIDA). Medications to Treat Opioid Use Disorder Bethesda, MD: National Institute on Drug Abuse (NIDA); 2018. [Google Scholar]
- 12.Olsen Y, Sharfstein JM. Confronting the Stigma of Opioid Use Disorder—and Its Treatment. JAMA. 2014. April 9;311(14):1393. [DOI] [PubMed] [Google Scholar]
- 13.American Society of Addiction Medicine. Medicaid Coverage of Medications for the Treatment of Opioid Use Disorder: West Virginia [Internet]. 2016. [cited 2018 Aug 14]. Available from: https://www.asam.org/docs/default-source/advocacy/state-medicaid-reports/state-medicaid-reports_wv.pdf?sfvrsn=6
- 14.Olfson M, Wall M, Barry CL, Mauro C, Mojtabai R. Impact Of Medicaid Expansion On Coverage And Treatment Of Low-Income Adults With Substance Use Disorders. Health Aff (Millwood). 2018. August;37(8):1208–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Meinhofer A, Witman AE. The role of health insurance on treatment for opioid use disorders: Evidence from the Affordable Care Act Medicaid expansion. J Health Econ. 2018. July;60:177–97. [DOI] [PubMed] [Google Scholar]
- 16.Wen H, Hockenberry JM, Borders TF, Druss BG. Impact of Medicaid Expansion on Medicaid-covered Utilization of Buprenorphine for Opioid Use Disorder Treatment: Med Care. 2017. April;55(4):336–41. [DOI] [PubMed] [Google Scholar]
- 17.Saloner B, Levin J, Chang H-Y, Jones C, Alexander GC. Changes in Buprenorphine-Naloxone and Opioid Pain Reliever Prescriptions After the Affordable Care Act Medicaid Expansion. JAMA Netw Open. 2018. August 17;1(4):e181588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Foundation Delmarva. West Virginia External Quality Review Mountain Health Trust Annual Technical Report. Washington, DC: West Virginia Department of Health and Human Resources; 2017. [Google Scholar]
- 19.USDA Economic Research Services. Rural-Urban Continuum Codes [Internet]. 2016. [cited 2018 Sep 11]. Available from: https://www.ers.usda.gov/data-products/rural-urban-continuum-codes.aspx
- 20.Frean M, Gruber J, Sommers BD. Premium subsidies, the mandate, and Medicaid expansion: Coverage effects of the Affordable Care Act. J Health Econ. 2017. May;53:72–86. [DOI] [PubMed] [Google Scholar]
- 21.Davenport S, Matthews K. Opioid use disorder in the United States: Diagnosed prevalence by payer, age, sex, and state. Washington, DC: Milliman; 2018. [Google Scholar]
- 22.Kim HM, Smith EG, Stano CM, Ganoczy D, Zivin K, Walters H, et al. Validation of key behaviourally based mental health diagnoses in administrative data: suicide attempt, alcohol abuse, illicit drug abuse and tobacco use. BMC Health Serv Res [Internet]. 2012. December [cited 2018 Aug 16];12(1). Available from: http://bmchealthservres.biomedcentral.com/articles/10.1186/1472-6963-12-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pietras S, Azur M, Brown J. Review of Medication-Assisted Treatment Guidelines and Measures for Opioid and Alcohol Use. Washington, DC: Mathematica Policy Research; 2015. [Google Scholar]
- 24.Hostetter M, Klein S. In Focus: Expanding Access to Addiction Treatment Through Primary Care [Internet]. Commonwealth Fund. 2017. [cited 2018 Aug 17]. Available from: https://www.commonwealthfund.org/publications/newsletter/2017/sep/focus-expanding-access-addiction-treatment-through-primary-care [Google Scholar]
- 25.Amato L, Minozzi S, Davoli M, Vecchi S. Psychosocial combined with agonist maintenance treatments versus agonist maintenance treatments alone for treatment of opioid dependence. Cochrane Drugs and Alcohol Group, editor. Cochrane Database Syst Rev [Internet] 2011. October 5 [cited 2018 Jul 31]; Available from: http://doi.wiley.com/10.1002/14651858.CD004147.pub4 [Google Scholar]
- 26.Larochelle MR, Bernson D, Land T, Stopka TJ, Wang N, Xuan Z, et al. Medication for Opioid Use Disorder After Nonfatal Opioid Overdose and Association With Mortality: A Cohort Study. Ann Intern Med. 2018. August 7;169(3):137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mattick RP, Breen C, Kimber J, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Drugs and Alcohol Group, editor. Cochrane Database Syst Rev [Internet] 2014. February 6 [cited 2018 Sep 12]; Available from: http://doi.wiley.com/10.1002/14651858.CD002207.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jarvis BP, Holtyn AF, Subramaniam S, Tompkins DA, Oga EA, Bigelow GE, et al. Extended-release injectable naltrexone for opioid use disorder: a systematic review: Review of XR-NTX for OUD. Addiction. 2018. July;113(7):1188–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Knudsen HK, Roman PM. Racial and Ethnic Composition as a Correlate of Medication Availability within Addiction Treatment Organizations. Sociol Focus. 2009;42:133–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stein BD, Dick AW, Sorbero M, Gordon AJ, Burns RM, Leslie DL, et al. A population-based examination of trends and disparities in medication treatment for opioid use disorders among Medicaid enrollees. Subst Abuse. 2018. June 22;1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stein BD, Gordon AJ, Sorbero M, Dick AW, Schuster J, Farmer C. The impact of buprenorphine on treatment of opioid dependence in a Medicaid population: Recent service utilization trends in the use of buprenorphine and methadone. Drug Alcohol Depend. 2012. June;123(1–3):72–8. [DOI] [PubMed] [Google Scholar]
- 32.Mohlman MK, Tanzman B, Finison K, Pinette M, Jones C. Impact of Medication-Assisted Treatment for Opioid Addiction on Medicaid Expenditures and Health Services Utilization Rates in Vermont. J Subst Abuse Treat. 2016. August;67:9–14. [DOI] [PubMed] [Google Scholar]
- 33.Maclean JC, Saloner B. The Effect of Public Insurance Expansions on Substance Use Disorder Treatment: Evidence from the Affordable Care Act [Internet]. Cambridge, MA: National Bureau of Economic Research; 2017. April [cited 2018 May 30]. Report No.: w23342. Available from: http://www.nber.org/papers/w23342.pdf [PMC free article] [PubMed] [Google Scholar]
- 34.Patrick SW, Buntin MB, Martin PR, Scott TA, Dupont W, Richards M, et al. Barriers to Accessing Treatment for Pregnant Women with Opioid Use Disorder in Appalachian States. Subst Abuse. 2018. June 27;1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]


