Abstract
Background and Aims
Opioid-related overdose is increasingly linked to pregnancy-associated deaths, but factors associated with postpartum overdose are unknown. We aimed to estimate the strength of the association between maternal and infant characteristics and postpartum opioid-related overdose.
Design
Retrospective cohort study using a linked, population-level dataset.
Setting
Massachusetts, United States.
Participants
Women who delivered one or more live births from 2012–2014 (n=174,517).
Measurements
The primary outcome was opioid-related overdose in the postpartum year. We used multivariable logistic regression to explore the independent associations of maternal (demographics, substance use, pregnancy) and infant (gestational age, birthweight, neonatal abstinence syndrome (NAS)) characteristics with postpartum opioid overdose. Findings were stratified by maternal opioid use disorder (OUD) diagnosis.
Findings
There were 189 deliveries to women who experienced ≥1 opioid overdose in the first year postpartum (11/10,000 deliveries). Among women with postpartum opioid overdose, 46.6% had an OUD diagnosis within twelve months before delivery. In our adjusted model, maternal diagnosis of OUD (aOR 3.61, 95% CI 1.73–7.51) and prior non-fatal overdose (aOR 2.40, 95% CI 1.11–5.17) were most strongly associated with postpartum overdose. After stratifying by OUD status, infant diagnosis of NAS (OUD+ aOR 2.03, 95% CI 1.26–3.27; OUD- aOR 2.79, 95% CI 1.12–6.93), and high unscheduled healthcare utilization (OUD+ aOR 2.27, 95% CI 1.38–3.73; OUD- aOR 2.11, 95% CI 1.24–3.58) were positively associated with postpartum overdose in both groups.
Conclusion
Among women who delivered live infants in Massachusetts, USA between 2012 and 2014, maternal diagnosis of OUD, prior non-fatal overdose, infant diagnosis of NAS, and high unscheduled health care utilization appeared to be positively associated with postpartum opioid overdose. However, over half of postpartum overdoses in that period were to women without a diagnosis of OUD. Engagement in methadone or buprenorphine treatment in the month prior to delivery was not sufficient to reduce the odds of postpartum overdose.
Keywords: Pregnancy, postpartum, opioid use disorder, overdose, women, maternal, neonatal abstinence syndrome, non-fatal
Introduction
In the United States, opioid-related overdose events are increasingly implicated in pregnancy-associated deaths, defined as deaths occurring during or within a year of the end of pregnancy, contributing to 11 to 25% of deaths in several states.1–6 The majority of the reported deaths occur later in the postpartum period; in Massachusetts, over 90% of substance-use related pregnancy-associated deaths occurred after six weeks postpartum, compared with 60% of all other pregnancy-associated deaths.1–5 In Massachusetts, the seven to twelve months following delivery were found to be a period of increased risk of both fatal and non-fatal opioid overdose events (12.3/100,00 person-days) compared with the trimester just prior to delivery (3.3/100,00 person-days).7
The postpartum period is a vulnerable period where overdose can pose significant risks to maternal and child health and well-being. This time can be particularly challenging for mothers with opioid use disorder (OUD) given high rates of postpartum depression, fragmented transitions of care from prenatal to postpartum providers, lapses in insurance following delivery, physiologic changes impacting medication dose for treatment of OUD, and the shame and stigma experienced by women secondary to neonatal opioid withdrawal or loss of child custody.8–13
Overdose risk factors in the general population have been well described, including prior non-fatal overdose, greater severity of opioid use disorder, receipt of prescription opioids, recent incarceration, depression, female gender, and housing instability.14–22 Yet unique risk factors for overdose among postpartum women in the year following delivery have not been specifically examined. The purpose of this study was to identify the extent to which maternal and infant characteristics identifiable at time of delivery were associated with opioid-related fatal and non-fatal overdose in the first postpartum year utilizing a linked-statewide population-level dataset in Massachusetts. We hypothesized that in addition to the factors previously described in the general population, inadequate prenatal care and preterm delivery would be associated with opioid-related overdose in the postpartum period. Additionally, among women who experienced postpartum overdose, we aimed to compare characteristics by OUD diagnosis, an important benchmark in identification of at-risk women during pregnancy.
Methods
Design
We performed a retrospective cohort study utilizing a statewide linked-dataset, called the Public Health Data Warehouse, previously described as the Chapter 55 database. This dataset was established as part of a Massachusetts (MA) legislative mandate and is overseen by the Massachusetts Department of Public Health (MDPH).23–25 Linkage across several state data sets from 2011–2015, including the All Payer Claims Database (APCD), Vital Records (birth and death certificates), Bureau of Substance Addiction Services (BSAS) licensed substance use disorder treatment data, the Center for Health Information and Analysis Case Mix records (inpatient hospitalization, observation encounters, and emergency department discharges), the Prescription Monitoring Program (PMP), MA Ambulance Trip Record Information System, and state Medicaid (MassHealth), among others, was performed by the MDPH to allow further exploration of factors that influence opioid overdoses. A full description of the datasets linked, data structure, and linkage rates across datasets has been described previously.26
Participants
Our cohort included all MA residents who delivered a live birth in MA and a documented gestational age ≥ 20 weeks, identified using birth certificates. Birth certificate linkage rates for our study period were 91.7%. Fetal death records were excluded. Our study cohort was limited to deliveries that occurred between January 2012 and September 2014, to allow for a full year of available data before and after each delivery. The study population included birth of both singleton and multiples (treated as a single delivery episode), as well as multiple deliveries to the same woman during the study period.
Measures
Our primary outcome of interest was any fatal or nonfatal opioid-related overdose during the 365 days following delivery. Opioid-related overdose events were defined by identification of any of the following: (1) A discharge from an inpatient unit, observation unit, or an emergency department encounter with an indication of opioid overdose based on International Classification of Disease (ICD) Ninth Edition diagnosis codes for opioid poisoning (Supplementary Table 1); (2) An ambulance encounter with an indication of opioid overdose based on an algorithm created by MPDH and the Centers for Disease Control and Prevention (available only from 2013–2015); or (3) A death certificate indicating opioid overdose as cause of death.
Maternal characteristics extracted from the birth certificate include age at time of delivery, race/ethnicity, highest educational level, marital status, and the adequacy of prenatal care utilization index.27 Enrollment in MassHealth (Medicaid) during the month of delivery was identified from the MassHealth insurance database. Additional characteristics were defined dichotomously based on any evidence in the 12 months before delivery, inclusive of month of delivery – homelessness, defined as an active casefile in the MA Department of Housing and Community Development (DHCD) dataset; incarceration, defined as release from incarceration in a prison or a jail in MA; and anxiety and depression, defined by APCD and Case Mix data. Finally, high utilization of unscheduled care, defined as three or more emergency department and/or obstetric triage visits in the 12 months before delivery, exclusive of the month of delivery based on Case Mix data.
Maternal OUD in the year prior to delivery was defined as an ICD-9 or ICD-10 code for opioid use disorder (Supplementary Table 1) in either APCD claims or Case Mix records. Women were defined as enrolled in an opioid treatment program if they had any evidence of enrollment in a state-funded program in the 12 months before delivery from BSAS records, which includes acute treatment services, crisis stabilization, residential, and intensive outpatient programs. Women were defined as receiving medication for OUD (MOUD) in the 12 months before delivery and the month of delivery if they had a claim for methadone maintenance treatment (Supplementary Table 1), record of methadone treatment from BSAS, or had filled a prescription for buprenorphine or buprenorphine/naloxone. Non-fatal overdose in the year prior to delivery was defined as a claim or ambulance record for opioid overdose in the 365 days before delivery not linked to a death record. Finally, an opioid prescription filled in the 3 months prior to delivery, excluding buprenorphine, was determined from PMP data. Prescriptions in the month of delivery were excluded to avoid opioid prescriptions for postpartum pain control.
Mothers who delivered infants with neonatal withdrawal symptoms were identified by infant diagnosis claim of neonatal abstinence syndrome (NAS) (Supplementary Table 1). Gestational age, birthweight, delivery type, and receipt of breastmilk prior to discharge were identified from birth certificate data. To account for the collinearity between gestational age and birthweight, infants were described as preterm/low birthweight if they were born before 37 weeks and/or weighed less than 2,500 grams. In order to have a single value for each delivery, infant characteristics were combined for multiple gestations (e.g., if one twin was diagnosed with NAS, the delivery was coded as NAS positive).
Analyses
We used descriptive statistics, including counts, percentages, and rates per 10,000 live births to compare the characteristics of women with postpartum overdose to women who delivered a live birth in Massachusetts but had no documented postpartum overdose for each covariate. We used generalized estimating equations logistic regression with an unstructured correlation structure to account for multiple deliveries to the same woman throughout the study period. We developed three models: an unadjusted model, a model which controlled for maternal diagnosis of OUD, and a multivariable model that evaluated the association of all a priori maternal and infant covariates described earlier and postpartum overdose. Multivariable models were examined for potential collinearity by calculating variance inflation factors and condition indices. To examine the effect of a prior diagnosis of OUD, we assessed potential interactions between OUD diagnosis and each covariate in our multivariate models. Significant interactions were identified, so the final model was stratified by prior OUD diagnosis. All analyses were performed in SAS Studio version 3.6 (Cary, NC). The Partners Institutional Review Board deemed this study exempt as non-human subjects research.
Results
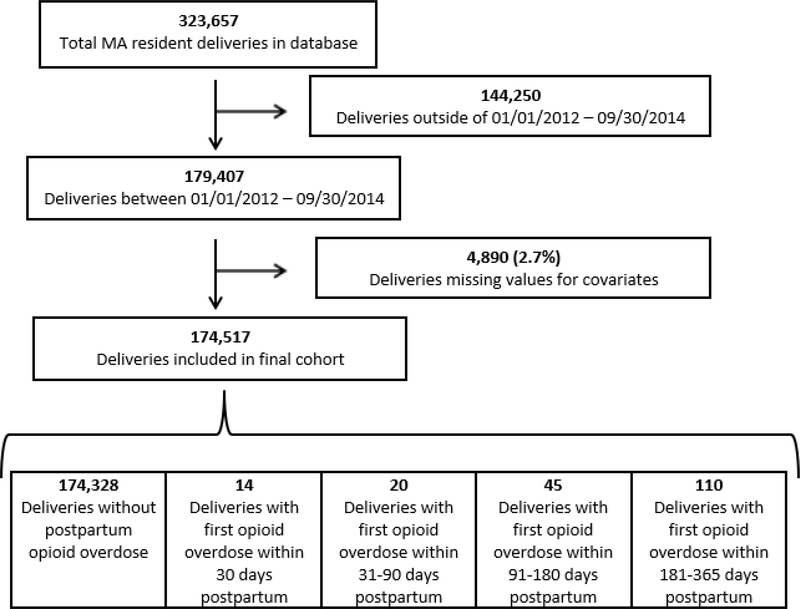
We identified 179,407 deliveries resulting in a live birth in Massachusetts during our study period. We excluded 4,890 (2.7%) deliveries that were missing maternal or infant covariates, leaving 174,517 deliveries (170,678 singleton and 3,839 multiples) in our final cohort among 164,765 unique women. There were 189 deliveries (all among unique women) with at least one postpartum opioid overdose in the year following delivery, affecting approximately 11/10,000 deliveries. Ninety-three percent of initial overdose events (176) were non-fatal and 58% (109) occurred in the 7–12 months following delivery (Figure 1).
Figure 1:
Study Schema
Descriptive statistics for women in the study population are presented in Table 1. Women who had an overdose in the year following delivery were significantly more likely to be younger than age 25, white/non-Hispanic, less educated, unmarried, receiving public insurance at delivery, and have less than adequate prenatal care, when compared to all women in MA who delivered a live birth. In terms of opioid use and treatment in the year prior to delivery, women who had a postpartum overdose were significantly more likely to: have a diagnosis of OUD, enroll in a treatment program for an opioid problem, receive MOUD during the month of delivery, and fill an opioid prescription (excluding buprenorphine) in the three months prior to delivery. With respect to psychosocial history in the year before delivery, women with an overdose were significantly more likely to have a diagnosis of depression and anxiety, high unscheduled healthcare utilization, a history of incarceration, and evidence of homelessness. Finally, deliveries among women with a postpartum overdose were more likely to result in a preterm or low birthweight infant, diagnosis of NAS, and less initiation of breastfeeding.
Table 1:
Maternal and Infant Characteristics by Postpartum Opioid Overdose (N=174,517)
| OD event during 365 days following delivery (n= 189) | No OD event during 365 days following delivery (n= 174,328) | OD Rate per 10,000 live births | |||
|---|---|---|---|---|---|
| Characteristics | n | % | n | % | Rate (95% CI) |
| Maternal Demographics | |||||
| Maternal Age | |||||
| ≤ 25 years old | 88 | 46.6% | 34,662 | 19.9% | 25.3 (20.0, 30.6) |
| 26–30 years old | 61 | 32.3% | 45,994 | 26.4% | 13.2 (9.9, 16.6) |
| ≥ 31 years old | 40 | 21.2% | 93,672 | 53.7% | 4.3 (2.9, 5.6) |
| Maternal Race/Ethnicity | |||||
| White non-Hispanic | 153 | 81.0% | 111,031 | 63.7% | 13.8 (11.6, 15.9) |
| Other race/ethnicity | 36 | 19.1% | 63,297 | 36.3% | 5.7 (3.8, 7.5) |
| Maternal Education | |||||
| High School or less | 117 | 61.9% | 47,295 | 27.1% | 24.7 (20.2, 29.1) |
| Some College or more | 72 | 38.1% | 127,033 | 72.9% | 5.7 (4.4, 7.0) |
| Marital Status | |||||
| Married | 35 | 18.5% | 114,985 | 66.0% | 3.0 (2.0, 4.1) |
| Not Married | 154 | 81.5% | 59,343 | 34.0% | 25.9 (21.8, 30.0) |
| Enrolled in MassHealth at Delivery | |||||
| Yes | 173 | 91.5% | 73,045 | 41.9% | 23.6 (20.1, 27.1) |
| No | 16 | 8.5% | 101,283 | 58.1% | 1.6 (0.8, 2.4) |
| Pregnancy Variables | |||||
| Breastfeeding at Discharge | |||||
| Yes | 90 | 47.6% | 145,117 | 83.2% | 6.2 (4.9, 7.5) |
| No | 99 | 52.4% | 29,211 | 16.8% | 33.8 (27.1, 40.4) |
| Preterm or Low Birth Weight (% Yes) | |||||
| Yes | 50 | 26.5% | 16,707 | 9.6% | 29.8 (21.6, 38.1) |
| No | 139 | 73.5% | 157,621 | 90.4% | 8.8 (7.3, 10.3) |
| Adequacy of Prenatal Care* | |||||
| Less than Adequate | 80 | 42.3% | 36,888 | 21.2% | 21.6 (16.9, 26.4) |
| Adequate | 50 | 26.5% | 72,899 | 41.8% | 6.9 (5.0, 8.8) |
| Intensive | 59 | 31.2% | 64,541 | 37.0% | 9.1 (6.8, 11.5) |
| Method of Delivery | |||||
| Vaginal | 120 | 63.5% | 120,866 | 69.3% | 9.9 (8.1, 11.7) |
| C-Section | 69 | 36.5% | 53,462 | 30.7% | 12.9 (9.8, 15.9) |
| NAS Diagnosis | |||||
| Yes | 66 | 34.9% | 1,892 | 1.1% | 337.1 (255.8, 418.4) |
| No | 123 | 65.1% | 172,436 | 98.9% | 7.1 (5.9, 8.4) |
| Opioid Related Variables | |||||
| Enrolled in BSAS Program for Opioid Problem (12MB) (% Yes) | 67 | 35.5% | 1,233 | 0.7% | 515.4 (392.0, 638.8) |
| Type of MOUD (12MB) | |||||
| Buprenorphine only | 32 | 16.9% | 1,210 | 0.7% | 257.6 (158.4, 346.9) |
| Methadone only | 32 | 16.9% | 1,071 | 0.6% | 290.1 (189.6, 390.6) |
| Mixed | 14 | 7.4% | 233 | 0.1% | 566.8 (269.9, 863.7) |
| None | 111 | 58.7% | 171,814 | 98.6% | 6.5 (5.3, 7.7) |
| MOUD during month of delivery (% Yes) | 56 | 29.6% | 1,935 | 1.1% | 281.3 (207.6, 354.9) |
| Non-fatal Opioid Overdose (12MB) (% Yes) | 12 | 6.4% | 67 | 0.04% | 1519.0 (659.5, 2378.4) |
| OUD Diagnosis (Casemix or APCD) (12MB) | |||||
| Yes | 88 | 46.6% | 2,431 | 1.4% | 349.3 (276.4, 422.3) |
| No | 101 | 53.4% | 171,897 | 98.6% | 5.9 (4.7, 7.0) |
| Opioid RX† Filled (3MB‡) | |||||
| Yes | 14 | 7.4% | 4,347 | 2.5% | 32.1 (15.3, 48.9) |
| No | 175 | 92.6% | 169,981 | 97.5% | 10.3 (8.8, 11.8) |
| Healthcare Utilization | |||||
| Any Emergency department visit (12MB‡ | |||||
| Yes | 116 | 61.4% | 36,280 | 20.8% | 31.9 (26.1, 37.7) |
| No | 73 | 38.6% | 138,048 | 79.2% | 5.3 (4.1, 6.5) |
| Any Hospital admission (12MB‡) | |||||
| Yes | 51 | 27.0% | 8,637 | 5.0% | 58.7 (42.6. 74.8) |
| No | 138 | 73.0% | 165,691 | 95.1% | 8.3 (6.9, 9.7) |
| Any Observational Stay (12MB‡) | |||||
| Yes | 24 | 12.7% | 7,925 | 4.6% | 30.2 (18.1, 42.3) |
| No | 165 | 87.3% | 166,403 | 95.5% | 9.9 (8.4, 11.4) |
| Any Inpatient or ED utilization (12MB‡) | |||||
| Yes | 122 | 64.6% | 43,711 | 25.1% | 27.8 (22.9, 32.8) |
| No | 67 | 35.5% | 130,617 | 74.9% | 5.2 (3.9, 6.4) |
| High Utilization of ED (12MB‡) | |||||
| 3 or more ED or OB triage visits | 77 | 40.7% | 9,292 | 5.3% | 82.2 (66.8, 100.5) |
| Less than three visits | 112 | 59.3% | 165,036 | 94.7% | 6.8 (5.5, 8.0) |
| Mental Health Variables | |||||
| Anxiety Diagnosis (12MB) | |||||
| Yes | 69 | 36.5% | 7,821 | 4.5% | 87.5 (66.8, 108.1) |
| No | 120 | 63.5% | 166,507 | 95.5% | 7.2 (5.2, 8.5) |
| Depression Diagnosis (12MB) | |||||
| Yes | 71 | 37.6% | 9,646 | 5.5% | 73.1 (56.1, 90.1) |
| No | 118 | 62.4% | 164,682 | 94.4% | 7.2 (5.2, 8.5) |
| Incarceration and Homelessness Variables | |||||
| Incarcerated in Prison or Jail (12MB) | |||||
| Yes | 18 | 9.5% | 359 | 0.2% | 477.5 (256.9, 698.0) |
| No | 171 | 90.5% | 173,969 | 99.9% | 9.8 (8.3, 11.3) |
| Homelessness - shelter/hotel case file (12MB) | |||||
| Yes | 15 | 7.9% | 2,049 | 1.2% | 72.7 (35.9, 109.5) |
| No | 174 | 92.1% | 172,279 | 98.8% | 10.1 (8.6, 11.6) |
Excluding Buprenorphine, 3MB‡ = in the 3 months before delivery - exclusive, 12MB= in the 12 months before delivery - inclusive, 12MB‡ = in the 12 months before delivery - exclusive, SP=in study period (2011–2015)
APCD = All Payer Claims Database, BSAS = Bureau of Substance Addiction Services, Casemix = Hospital discharge data, DHCD = Department of Housing and Community Development, DPH = Department of Public Health, MOUD=Medication for Opioid Use Disorder NAS = Neonatal Abstinence Syndrome
We compared the characteristics of the deliveries of women who had an overdose who had evidence of OUD in the year before delivery (n=88) with those who did not have evidence of OUD (n=101) in Table 2. Women without prior evidence of OUD but who experienced a postpartum overdose were more likely to have adequate prenatal care and breastfeed their infant compared with women with a prior OUD diagnosis. Additionally, this group was less likely to have high unscheduled healthcare utilization and less likely to have a prior diagnosis of anxiety or depression, compared with deliveries to women with a prior OUD diagnosis.
Table 2:
Comparison of Maternal and Infant Characteristics among Women with Postpartum Overdose by Evidence of Opioid Use Disorder (N=189)
| Evidence of OUD in 12 months before delivery, inclusive (n= 88) | No Evidence of OUD in 12 months before delivery, inclusive (n= 101) | ||||
|---|---|---|---|---|---|
| Characteristics | n | % | n | % | p-value |
| Maternal Demographics | |||||
| Maternal Age | 0.200 | ||||
| ≤ 25 years old | 35 | 39.8% | 53 | 52.5% | |
| 26–30 years old | 31 | 35.2% | 30 | 29.7% | |
| ≥ 31 years old | 22 | 25.0% | 18 | 17.8% | |
| Maternal Race/Ethnicity | 0.001 | ||||
| White non-Hispanic | * | * | 73 | 72.3% | |
| Other race/ethnicity | * | * | 28 | 27.7% | |
| Maternal Education | 0.024 | ||||
| High School or less | 62 | 70.5% | 55 | 54.5% | |
| Some College or more | 26 | 29.6% | 46 | 45.5% | |
| Marital Status | 0.911 | ||||
| Married | 16 | 18.2% | 19 | 18.8% | |
| Not Married | 72 | 81.8% | 82 | 81.2% | |
| Enrolled in MassHealth at Delivery (% Yes) | * | * | 11 | 10.9% | 0.199 |
| Pregnancy Variables | |||||
| Breastfeeding at Discharge (% Yes) | 28 | 31.8% | 62 | 61.4% | <0.001 |
| Preterm or Low Birth Weight (% Yes) | 25 | 28.4% | 25 | 24.8% | 0.570 |
| Adequacy of Prenatal Care | <0.001 | ||||
| Less than Adequate | 51 | 58.0% | 29 | 28.7% | |
| Adequate | 13 | 14.8% | 37 | 36.6% | |
| Intensive | 24 | 27.3% | 35 | 34.7% | |
| Method of Delivery | 0.344 | ||||
| Vaginal | 59 | 67.1% | 61 | 60.4% | |
| C-Section | 29 | 33.0% | 40 | 39.6% | |
| NAS Diagnosis (% Yes) | 56 | 63.6% | * | * | <0.001 |
| Opioid Related Variables | |||||
| Enrolled in BSAS Program for Opioid Problem (12MB) (% Yes) | 50 | 56.8% | 17 | 16.8% | <0.001 |
| Any MOUD (12MB) (% Yes) | 67 | 76.1% | 11 | 10.9% | <0.001 |
| MOUD during month of delivery (% Yes) | 50 | 56.8% | * | * | <0.001 |
| Non-fatal Opioid Overdose (12MB) (% Yes) | 11 | 12.5% | * | * | 0.001 |
| Healthcare Utilization | |||||
| Any Emergency department visit (12MB‡) (% Yes) | 67 | 76.1% | 49 | 48.5% | <0.001 |
| Any Hospital admission (12MB‡) (% Yes) | 38 | 43.2% | 13 | 12.9% | <0.001 |
| Any Observational Stay (12MB‡) (% Yes) | 19 | 21.6% | * | * | 0.001 |
| Any Inpatient or ED utilization (12MB‡) (% Yes) | 70 | 79.6% | 52 | 51.5% | <0.001 |
| ED Visits (12MB‡) (% Yes) | 48 | 51.4% | 29 | 28.7% | <0.001 |
| Mental Health Variables | |||||
| Anxiety Diagnosis (12MB) (% Yes) | 50 | 56.8% | 19 | 18.8% | <0.001 |
| Depression Diagnosis (12MB) (% Yes) | 50 | 56.8% | 21 | 20.8% | <0.001 |
| Incarceration and Homelessness Variables | |||||
| Incarcerated in Prison or Jail (12MB) (% Yes) | 11 | 12.5% | * | * | 0.193 |
| DHCD shelter/hotel case file (12MB) (% Yes) | 11 | 12.5% | * | * | 0.030 |
Values suppressed due to privacy restrictions. Any non-zero value < 11 is suppressed. If only one value is suppressed in a category, the next smallest value is also suppressed to prevent back calculation.
3MB‡ = in the 3 months before delivery - exclusive, 12MB= in the 12 months before delivery - inclusive, 12MB‡ = in the 12 months before delivery - exclusive, SP=in study period (2011–2015)
APCD = All Payer Claims Database, Casemix = Hospital discharge data, DHCD = Department of Housing and Community Development, MOUD=Medication for Opioid Use Disorder, NAS = Neonatal Abstinence Syndrome
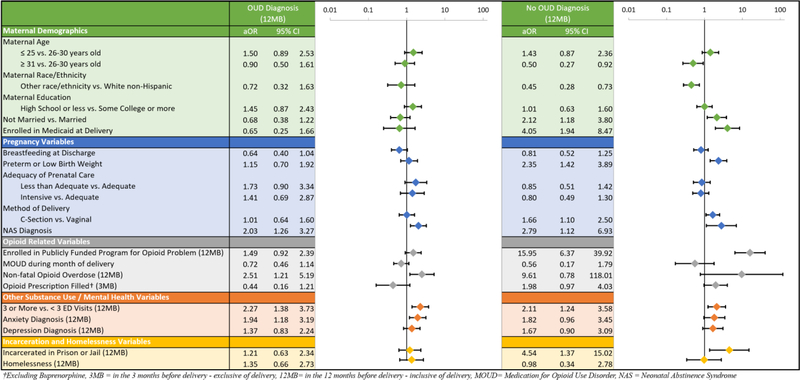
Our unadjusted model (Model 1) identified that diagnosis of OUD and opioid-related variables were most highly associated with a postpartum overdose. After adjusting for OUD status (Model 2) and all other covariates (Model 3) we found a significant reduction in the magnitude of the adjusted odds ratios (Supplementary Table 2). We identified evidence of a significant interaction between OUD diagnosis and the association between multiple covariates and postpartum overdose in our adjusted model. These findings led us to present our final model stratified by OUD diagnosis (Figure 2).
Figure 2:
Adjusted Odds Ratios for Postpartum Opioid Overdose, Stratified by OUD Diagnosis (N=174,517)
In the OUD positive group, infant NAS diagnosis, prior overdose in last 12 months, high ED utilization, and maternal anxiety were associated with postpartum overdose. In the OUD negative group, in addition to infant NAS diagnosis and higher ED utilization, we found that marital status, public insurance, preterm/low birthweight, C-section delivery, opioid treatment program involvement, opioid prescribing, and incarceration status were positively associated with postpartum overdose (Figure 2). For three covariates, marital status, enrollment in Medicaid, and opioid prescription three months before delivery, the direction of the adjusted odds ratio differed by OUD status, but they were not statistically significant in the final models. In both models, MOUD during the month of delivery was not statistically significantly associated with postpartum overdose.
Discussion
In a population-level cohort of more than 174,000 deliveries resulting in live births between 2012–2014 in Massachusetts using a linked administrative dataset, postpartum overdose occurred at a rate of 11/10,000 deliveries. In our cohort, less than half of women with a postpartum overdose had a documented OUD diagnosis in the year prior to or during their delivery hospitalization, and maternal and infant characteristics associated with overdose differed by OUD status. In our final stratified models, factors significantly associated with postpartum overdose in both groups included infant diagnosis of NAS and high unscheduled healthcare utilization. For women in the OUD negative group, additional characteristics positively associated with postpartum overdose included public insurance, being unmarried, enrollment in a public opioid treatment program, preterm/low birth weight, cesarean delivery, and history of incarceration; conversely, older age and non-white race were associated with decreased odds of postpartum overdose.
We found that postpartum overdose is an uncommon event that occurs at a lower rate than overdose in the general population in Massachusetts (31/10,000 in 2015).25 While this rate was lower than reported national rates of other conditions affecting postpartum women in the United States such as depression (impacting 9–20% of all deliveries)28 or obstetrical complications requiring readmission (1–2% of all deliveries),29 we found the postpartum opioid-related overdose rate was similar to that of postpartum psychosis (0.1–0.5% of deliveries).28,30 Given postpartum overdose can result in significant morbidity and mortality for women and the prevalence of OUD in pregnancy continues to rise,31 identifying women at risk of overdose is important to offer harm reduction services such as naloxone distribution and provide addiction treatment.32,33
Similar to prior studies, we found that a known history of an OUD and prior overdose were substantially associated with increased odds of postpartum overdose.15–19,34 Unique to postpartum women, we identified that an infant diagnosis of NAS at delivery and preterm/low birthweight at delivery were associated with a greater likelihood of postpartum overdose. For infant NAS diagnosis, we hypothesize that this association is most likely a proxy for maternal evidence of opioid use or recent opioid prescribing (70% of cases of NAS were to women with evidence of OUD). However, the shame and stigma women experience from watching their infant display withdrawal symptoms, grief from loss of parental custody, and stresses of caring for a potentially fussier baby could also contribute to this positive association. There remains great heterogeneity in the way providers classify opioid-exposed infants as having a diagnosis of NAS.35 Based on NAS claims diagnoses alone, we were unable to determine if an infant required pharmacologic treatment or not, and if differences in overdose exist by infant treatment status. Preterm or low birthweight infants may have special health care needs that increase the burden on caretakers in the year postpartum. Additionally, higher unscheduled health care utilization, but not inadequate prenatal care receipt, was associated with postpartum overdose. A qualitative study of low-income pregnant women with high unscheduled care found utilization may be driven by experiences of illness insufficiently addressed by outpatient prenatal care.36 The experience of women having unmet health needs may portend future postpartum overdose risk, regardless of whether a diagnosis of OUD is identified at delivery.
In our stratified analysis among women with an OUD diagnosis, we found that a diagnosis of anxiety, but not depression in the year before delivery was significantly associated with postpartum overdose. In the OUD negative group, we found a similar but not statistically significant association between prior mental health diagnosis and postpartum overdose, likely due to insufficient power to detect an association. A history of psychopathology during pregnancy has been previously shown to be strongly associated with postpartum depression, which could contribute to postpartum relapse and overdose.8,37
Notably, there was no independent association between receiving MOUD the month of delivery and adjusted odds of postpartum overdose. This suggests that engagement in treatment with methadone or buprenorphine at time of delivery is not sufficient to reduce the odds of postpartum overdose. While our study design focused on factors identifiable at delivery, research has shown that discontinuation of MOUD increases overdose risk in the general population.33,38 Pregnancy represents a time where many women newly engage in treatment and receive MOUD, and the exploration of factors contributing to postpartum disengagement from treatment is an underexplored area for future research. For example, research exploring how caretaking responsibilities may interfere with the ability to engage in treatment and recovery supports, particularly as few treatment centers nationally have gender-specific and child care supports for women and their families.39
Finally, there has been an increasing body of literature examining opioid prescribing in women after delivery, as prescribing is routine after cesarean delivery40 but also common after vaginal delivery.41 In our stratified analysis among women without a diagnosis of OUD, we found a statistically significant association between cesarean delivery and postpartum overdose, which could be a proxy for postpartum opioid prescribing. However, a recent analysis by Ladha and colleagues assessed overdose risk for 90 days following several common surgical procedures, and found post-cesarean delivery had one of the lowest odds of overdose among 22 surgical procedures studied.42 Future research examining specific postpartum prescribing patterns and overdose risk is warranted.
Compared with our prior work that restricted analyses to individuals with an OUD diagnosis in the year prior to delivery,7 this analysis included all live births in MA. Our study was designed to look at maternal and infant factors identifiable at time of delivery associated with postpartum overdose, to help identify individuals who may be at higher risk in the postpartum period, and thus be able to offer more intensive services and resources tailored to this population. While we found that OUD diagnosis was strongly associated with increased odds of postpartum overdose, over half the deliveries with a postpartum overdose were to women with no documented OUD diagnosis in the year prior to and including month of delivery. We hypothesize several explanations for this finding. First, women with an existing OUD may not have received prenatal substance use screening, or disclosed their substance use history fully during pregnancy for fear of losing custody of their child or stigma surrounding substance use disorder during pregnancy, and thus were not identified prior to delivery. Second, given our reliance on administrative rather than clinical data, women with OUD may not have been properly characterized/documented with a diagnosis code of OUD despite being known to have one, as prior work showed that OUD is underdocumented in claims data in Massachusetts.43 Third, women may have developed a new OUD or newly used opioids resulting in an overdose following delivery but did not have OUD prior to delivery. Finally, not all women who overdose meet criteria for OUD, particularly as overdose becomes more frequent due to contamination of fentanyl into the opioid and non-opioid drug supply.15
Our subgroup analysis comparing those with a postpartum overdose by OUD status showed that these two groups of women had important differences in their characteristics. Those without a diagnosis claim for OUD had more adequate prenatal care engagement, less psychiatric comorbidity, less unscheduled health care utilization, higher rates of breastfeeding, and were less likely to deliver an infant with NAS, suggesting either less in-utero opioid exposure during pregnancy or a lack of appropriate prenatal identification rather than absence of diagnosis due to lack of access to care. For this group of women, identifying ways in the postpartum period to have increased contact for screening for substance use disorder is important, particularly given 25–35% of all women do not attend their postpartum visit.44 Pediatric providers who have frequent visits with families in the first year following delivery could play an important role in screening for OUD and identifying risk factors among families including postpartum depression, isolation, and limited supports in caring for a new baby.45
Our study has several important limitations. First, our observational cohort using administrative data is subject to both selection bias and misclassification bias. We attempted to minimize this risk by removing deliveries with an implausible gestational age and controlling for maternal demographics in our final adjusted model. Second, as overdose was a rare event, we may not have had enough power in our model to show all factors associated with postpartum overdose, such as homelessness and depression. Third, our study design focused on maternal and infant factors identifiable at time of delivery, but given more than half of the overdoses happened greater than six months after delivery, important characteristics just prior to the overdose such as engagement in MOUD were not known. Fourth, ambulance trip overdose data were only available from 2013–2015, so it is possible overdoses that did not result in hospital visits were missed, resulting in an underestimation of the overdoses in 2012. Fifth, stratifying our analysis by OUD status likely limited our ability to fully detect associations. Despite these limitations, our analysis is strengthened by the ability to report population-level data in Massachusetts and utilize a novel linked public health dataset.
We identified that maternal diagnosis of OUD, prior non-fatal overdose, infant diagnosis of NAS, and high unscheduled health care utilization are associated with postpartum overdose. Engagement in methadone or buprenorphine treatment in the month prior to delivery was not sufficient to reduce the odds of postpartum overdose, suggesting that early screening, continuous access to health care, and tight linkage to postpartum care providers are essential for women to maintain treatment adherence. Finally, more than 50% of women with a postpartum overdose did not have prior evidence of OUD, suggesting that an additional focus on screening women for OUD at delivery and postpartum, with sustained postpartum maternal support, is critical to efforts to reduce pregnancy-associated morbidity and improve the health of families.
Supplementary Material
Acknowledgments
Funding Support: Mr. Nielsen was supported by the Applied Epidemiology Fellowship Program administered by the Council of State and Territorial Epidemiologists and funded by the Centers for Disease Control and Prevention Cooperative Agreement Number 1U38OT000143-04; Dr. Yule was supported by AACAP/NIDA (K12 DA000357); Dr. Taveras was supported by NIDDK (K24 DK105989); Dr. Schiff was supported by NIDA (K12 DA043490 and K23DA048169).
Footnotes
Declarations of Interest: Dr. Timothy Wilens is or has been a consultant for: Alcobra, Neurovance/Otsuka, and Ironshore. Dr. Wilens serves as a clinical consultant to the US National Football League (ERM Associates), U.S. Minor/Major League Baseball, Phoenix/Gavin House, and Bay Cove Human Services. Dr. Sarah Wakeman received research funding from OptumLabs. No other authors report any declarations to disclose.
Literature Cited
- 1.MacDorman MF, Declercq E, Thoma ME. Trends in Texas maternal mortality by maternal age, race/ethnicity, and cause of death, 2006–2015. Birth. January 2018. doi: 10.1111/birt.12330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kavanaugh V Pregnancy-Associated Deaths From Drug Overdose in Virginia, 1999–2007: A Report from the Virginia Maternal Mortality Review Team; 2015.
- 3.Metz TD, Rovner P, Hoffman MC, Allshouse AA, Beckwith KM, Binswanger IA. Maternal Deaths From Suicide and Overdose in Colorado, 2004–2012. Obstet Gynecol. 2016;128(6):1233–1240. doi: 10.1097/AOG.0000000000001695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mehta PK, Bachhuber MA, Hoffman R, Srinivas SK. Deaths From Unintentional Injury, Homicide, and Suicide During or Within 1 Year of Pregnancy in Philadelphia. Am J Public Health. 2016;106(12):2208–2210. doi: 10.2105/AJPH.2016.303473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Massachusetts Department of Public Health. Substance Use among Pregnancy-Associated Deaths — 2005–2014. In: Maternal Mortality and Morbidity Review in Massachusetts: 2018. [Google Scholar]
- 6.Smid MC, Stone NM, Baksh L, et al. Pregnancy-Associated Death in Utah. Obstet Gynecol. 2019;133(6):1131–1140. doi: 10.1097/AOG.0000000000003279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schiff DM, Nielsen T, Terplan M, et al. Fatal and Nonfatal Overdose Among Pregnant and Postpartum Women in Massachusetts. Obstet Gynecol. 2018;132(2):466–474. doi: 10.1097/AOG.0000000000002734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chapman SLC, Wu L-T. Postpartum substance use and depressive symptoms: a review. Women Health. 2013;53(5):479–503. doi: 10.1080/03630242.2013.804025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Benningfield MM, Dietrich MS, Jones HE, et al. Opioid dependence during pregnancy: relationships of anxiety and depression symptoms to treatment outcomes. Addiction. 2012;107 Suppl:74–82. doi: 10.1111/j.1360-0443.2012.04041.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Klaman SL, Isaacs K, Leopold A, et al. Treating Women Who Are Pregnant and Parenting for Opioid Use Disorder and the Concurrent Care of Their Infants and Children: Literature Review to Support National Guidance. J Addict Med. 2017;11(3):178–190. doi: 10.1097/adm.0000000000000308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pace CA, Kaminetzky LB, Winter M, et al. Postpartum changes in methadone maintenance dose. J Subst Abuse Treat. 2014;47:229–232. doi: 10.1016/j.jsat.2014.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Auguste T, Gulati M. Recommendations and Conclusions Presidential Task Force on Redefining the Postpartum Visit Committee on Obstetric Practice Optimizing Postpartum Care Committee Opinion Optimizing Postpartum Care E141. Vol 131.; 2018. https://www.acog.org/-/media/Committee-Opinions/Committee-on-Obstetric-Practice/co736.pdf?dmc=1&ts=20180731T0225509403. Accessed July 30, 2018.
- 13.Daw JR, Hatfield LA, Swartz K, Sommers BD. Women In The United States Experience High Rates Of Coverage ‘Churn’ In Months Before And After Childbirth. Health Aff. 2017;36(4):598–606. doi: 10.1377/hlthaff.2016.1241. [DOI] [PubMed] [Google Scholar]
- 14.Walley AY, Cheng DM, Coleman SM, et al. Risk factors for recent nonfatal overdose among HIV-infected Russians who inject drugs. AIDS Care. 2014;26(8):1013–1018. doi: 10.1080/09540121.2013.871218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Somerville NJ, O’Donnell J, Gladden RM, et al. Characteristics of Fentanyl Overdose — Massachusetts, 2014–2016. MMWR Morb Mortal Wkly Rep. 2017;66(14):382–386. doi: 10.15585/mmwr.mm6614a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mack KA, Jones CM, Ballesteros MF. Illicit Drug Use, Illicit Drug Use Disorders, and Drug Overdose Deaths in Metropolitan and Nonmetropolitan Areas — United States. MMWR Surveill Summ. 2017;66(19):1–12. doi: 10.15585/mmwr.ss6619a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Caudarella A, Dong H, Milloy MJ, Kerr T, Wood E, Hayashi K. Non-fatal overdose as a risk factor for subsequent fatal overdose among people who inject drugs. Drug Alcohol Depend. 2016;162:51–55. doi: 10.1016/j.drugalcdep.2016.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Powis B, Strang J, Griffiths P, et al. Self-reported overdose among injecting drug users in London: extent and nature of the problem. Addiction. 1999;94(4):471–478. http://www.ncbi.nlm.nih.gov/pubmed/10605843. Accessed February 23, 2018. [DOI] [PubMed] [Google Scholar]
- 19.Martins SS, Sampson L, Cerdá M, Galea S. Worldwide Prevalence and Trends in Unintentional Drug Overdose: A Systematic Review of the Literature. Am J Public Health. 2015;105(11):e29–e49. doi: 10.2105/AJPH.2015.302843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chahua M, Sordo L, Barrio G, et al. Non-fatal opioid overdose and major depression among street-recruited young heroin users. Eur Addict Res. 2014;20(1):1–7. doi: 10.1159/000346787. [DOI] [PubMed] [Google Scholar]
- 21.Bohnert ASB, Valenstein M, Bair MJ, et al. Association Between Opioid Prescribing Patterns and Opioid Overdose-Related Deaths. JAMA. 2011;305(13):1315. doi: 10.1001/jama.2011.370. [DOI] [PubMed] [Google Scholar]
- 22.Larochelle MR, Liebschutz JM, Zhang F, Ross-Degnan D, Wharam JF. Opioid Prescribing After Nonfatal Overdose and Association With Repeated Overdose. Ann Intern Med. 2016;164(1):1. doi: 10.7326/M15-0038. [DOI] [PubMed] [Google Scholar]
- 23.Massachusetts Department of Public Health. An Assessment of Opioid-Related Deaths in Massachusetts (2013–2014).; 2016. https://www.mass.gov/files/documents/2016/09/pg/chapter-55-report.pdf. Accessed April 11, 2018.
- 24.Commonwealth of Massachusetts. An Act Requiring Certain Reports for Opiate Overdoses; 2015. https://malegislature.gov/Laws/SessionLaws/Acts/2015/Chapter55. Accessed October 8, 2017.
- 25.MA Department of Public Health. An Assessment of Fatal and Nonfatal Opioid Overdoses in Massachusetts (2011 – 2015). Boston; 2017. https://www.mass.gov/files/documents/2017/08/31/legislative-report-chapter-55-aug-2017.pdf. Accessed October 8, 2017. [Google Scholar]
- 26.Massachusetts Department of Public Health. Data Brief: Opioid-Related Overdose Deaths among Massachusetts Residents. Boston, MA; 2017. [Google Scholar]
- 27.Kotelchuck M An Evaluation of the Kessner Adequacy of Prenatal Care Index and a Proposed Adequacy of Prenatal Care Utilization Index. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1615177/pdf/amjph00460-0056.pdf. Accessed December 10, 2017. [DOI] [PMC free article] [PubMed]
- 28.Vesga-López O, Blanco C, Keyes K, Olfson M, Grant BF, Hasin DS. Psychiatric disorders in pregnant and postpartum women in the United States. Arch Gen Psychiatry. 2008;65(7):805–815. doi: 10.1001/archpsyc.65.7.805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Clapp MA, Little SE, Zheng J, Robinson JN. A multi-state analysis of postpartum readmissions in the United States. Am J Obstet Gynecol. 2016;215(1):113.e1–113.e10. doi: 10.1016/j.ajog.2016.01.174. [DOI] [PubMed] [Google Scholar]
- 30.VanderKruik R, Barreix M, Chou D, et al. The global prevalence of postpartum psychosis: a systematic review. BMC Psychiatry. 2017;17(1):272. doi: 10.1186/s12888-017-1427-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Haight SC, Ko JY, Tong VT, Bohm MK, Callaghan WM. Opioid Use Disorder Documented at Delivery Hospitalization — United States, 1999–2014. MMWR Morb Mortal Wkly Rep. 2018;67(31):845–849. doi: 10.15585/mmwr.mm6731a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hawk KF, Vaca FE, D’Onofrio G. Reducing Fatal Opioid Overdose: Prevention, Treatment and Harm Reduction Strategies. Yale J Biol Med. 2015;88(3):235–245. http://www.ncbi.nlm.nih.gov/pubmed/26339206. Accessed May 10, 2019. [PMC free article] [PubMed] [Google Scholar]
- 33.Larochelle MR, Bernson D, Land T, et al. Medication for Opioid Use Disorder After Nonfatal Opioid Overdose and Association With Mortality. Ann Intern Med. 2018;169(3):137. doi: 10.7326/M17-3107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bagley SM, Cabral H, Saia K, et al. Frequency and associated risk factors of non-fatal overdose reported by pregnant women with opioid use disorder. Addict Sci Clin Pract. 2018;13(1):26. doi: 10.1186/s13722-018-0126-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wachman EM, Schiff DM, Silverstein M. Neonatal Abstinence Syndrome: Advances in Diagnosis and Treatment. JAMA. 2018;319(13):1362–1374. doi: 10.1001/jama.2018.2640. [DOI] [PubMed] [Google Scholar]
- 36.Mehta PK, Carter T, Vinoya C, Kangovi S, Srinivas SK. Understanding High Utilization of Unscheduled Care in Pregnant Women of Low Socioeconomic Status. Women’s Heal Issues. 2017;27(4):441–448. doi: 10.1016/j.whi.2017.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.O’hara MW, Swain AM. Rates and risk of postpartum depression—a meta-analysis. Int Rev Psychiatry. 1996;8(1):37–54. doi: 10.3109/09540269609037816. [DOI] [Google Scholar]
- 38.Sordo L, Barrio G, Bravo MJ, et al. Mortality risk during and after opioid substitution treatment: systematic review and meta-analysis of cohort studies. BMJ. 2017;357:j1550. doi: 10.1136/BMJ.J1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Terplan M, Longinaker N, Appel L. Women-Centered Drug Treatment Services and Need in the United States, 2002–2009. Am J Public Health. 2015;105(11):e50–e54. doi: 10.2105/AJPH.2015.302821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bateman BT, Franklin JM, Bykov K, et al. Persistent opioid use following cesarean delivery: patterns and predictors among opioid-naïve women. Am J Obstet Gynecol. 2016;215(3):353.e1–353.e18. doi: 10.1016/j.ajog.2016.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Prabhu M, Garry EM, Hernandez-Diaz S, MacDonald SC, Huybrechts KF, Bateman BT. Frequency of Opioid Dispensing After Vaginal Delivery. Obstet Gynecol. 2018;132(2):459–465. doi: 10.1097/AOG.0000000000002741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ladha KS, Gagne JJ, Patorno E, et al. Opioid Overdose After Surgical Discharge. JAMA. 2018;320(5):502. doi: 10.1001/jama.2018.6933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Barocas JA, White LF, Wang J, et al. Estimated Prevalence of Opioid Use Disorder in Massachusetts, 2011–2015: A Capture–Recapture Analysis. Am J Public Health. 2018;108(12):1675–1681. doi: 10.2105/AJPH.2018.304673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.National Committee for Quality Assurance. Prenatal and Postpartum Care (PPC) - NCQA. https://www.ncqa.org/hedis/measures/prenatal-and-postpartum-care-ppc/. Published 2017. Accessed May 10, 2019.
- 45.Earls MF, Yogman MW, Mattson G, Rafferty J, COMMITTEE ON PSYCHOSOCIAL ASPECTS OF CHILD AND FAMILY HEALTH COPAOCAF. Incorporating Recognition and Management of Perinatal Depression Into Pediatric Practice. Pediatrics. 2019;143(1):e20183259. doi: 10.1542/peds.2018-3259. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.