Abstract
Background
Advances in technology means that domiciliary non-invasive ventilation (NIV) devices can be remotely monitored via modems in patients’ homes. Possible benefits and challenges of modem technology have yet to be established. This study explored the perspectives and experiences of patients, their carers and healthcare professionals (HCPs) on the addition of modem technology in managing home NIV.
Methods
A qualitative study using a combination of focus groups for HCPs and interviews for carers/patients was undertaken. 12 HCPs and 22 patients/carers participated. These focus groups and interviews were audio-recorded, transcribed verbatim and analysed thematically.
Results
Five main themes were identified. ‘Surveillance: a paradox of findings’: HCPs were concerned about unduly scrutinising patients’ lives, potentially impacting on HCP patient relationships. Conversely, patients welcomed modem monitoring and did not express concerns regarding invasion of privacy. ‘Sanctions’: HCPs reported the modem increased access to care and allowed appropriate assessment of ongoing treatment. ‘Complacency and ethics’: HCPs expressed concerns patients may become complacent in seeking help due to expectations of modem monitoring, as well as being concerned regarding the ethics of modems. There was a suggestion patients and carers' expectations of monitoring were different to that of clinical practice, resulting in complacency in some cases. ‘Increased time for patient focused care’: HCPs in the focus groups described a number of ways in which using modems was more efficient. ‘Confidence: can be improved with technology’: patients and carers were positive about the impact of the modems on their health and well-being, particularly their confidence.
Conclusion
HCPs expressed concerns about surveillance were not corroborated by patients, suggesting acceptability of remote monitoring. Data suggests a need for increased clarity to patients/carers regarding clinical practice relating to responsiveness to modem data. The issue of complacency requires further consideration. Modem technology was acceptable and considered a useful addition by HCPs, patients and carers.
Trial registration number
Keywords: non invasive ventilation, respiratory measurement
Key messages.
What are the experiences and views of patients, carers’ and healthcare professionals (HCPs) on using modems in domiciliary non-invasive ventilation (NIV)?
Modem technology was acceptable and considered a useful addition by HCPs, patients and carers.
This qualitative study has provided an important and useful narrative on the use of remote monitoring for patients receiving domiciliary NIV. It could be used to inform future studies and service design and provides an example of patient and public engagement.
Background
Domiciliary non-invasive ventilation (NIV) is accepted as gold-standard care for patients with chronic hypercapnic respiratory failure.1–3 NIV in specific patient groups has been shown to reduce mortality and morbidity, while increasing quality of life.1 4 5 Traditionally, patients receiving domiciliary NIV are monitored as an outpatient at regular appointments. These appointments assess the effectiveness of NIV through arterial blood gas measurement and clinical assessment. Anecdotally these clinical assessments can sometimes be limited to subjective history taking, including NIV usage, comfort and issues with devices, with little or no objective assessment to support patients’ reports. Factors known to impact on concordance with domiciliary NIV include: interface fit, patient tolerance of pressures, facial pressure ulcers, symptoms, cognition and psychosocial influences.6 7 Understanding objectively patients’ concordance with NIV treatment is imperative for clinicians to be able to identify problems, develop solutions and improve patient concordance for the achievement of best treatment outcomes.
One method of assessing patient NIV use is analysing data stored by the patient's ventilator, the available data depends on the specific manufacturer. Typically estimated parameters available are: tidal volume, leak, respiratory rate, minute ventilation, patient triggered breaths, achieved pressures and patient compliance. Records can be downloaded from secure data cards into the manufacturers’ software for clinicians to then access and interpret or data can be viewed daily with the use of modem technology, allowing real time review of any ventilator issues. Anecdotally the practice of accessing data stored by the ventilator is not common practice in the UK within sleep and ventilation services.
A modem is a piece of hardware which allows an NIV device to connect to a network (eg, the internet or 3G/4G networks). Ventilator data can then be transferred via the modem to web-based software where clinicians can then access it. Modem technology was originally developed for the sleep industry (obstructive sleep apnoea and continuous positive airway pressure (CPAP) treatment) for use in Europe and the USA, where patients do not receive reimbursement for care from insurance companies unless they demonstrate compliance with CPAP treatment. It is unclear if modem technology is being widely utilised for the care of domiciliary NIV patients either in the UK or elsewhere, but anecdotally numbers are small.8
The potential benefits and challenges of using modem technology in domiciliary NIV services have yet to be established. Possible benefits may include; more appropriate timing of (and potentially reduced) outpatient appointment attendance, monitoring for exacerbations of underlying chronic diseases, reducing acute emergency hospital admission, targeted admissions to hospital, more personalised and timely interventions by healthcare providers and earlier identification of problems with NIV.9–13 Challenges to using modems in domiciliary NIV may include an increased workload for healthcare professionals (HCPs) and a possible sense of an invasion of privacy for the patients.14 To our knowledge the existing evidence base does not consider experiences or perspectives of patients, their carers or HCPs regarding the use of modem technology in managing patients requiring domiciliary NIV. Specifically, this study aimed to address this gap in knowledge in the use of modem technology in the management of patients with hypercapnic ventilatory failure receiving domiciliary NIV. The objectives of this study were to:
Investigate the experience of patients receiving domiciliary NIV with modem technology and explore how this compares to NIV treatment without a modem.
Investigate the experience of carers of patients receiving domiciliary NIV with modem technology and explore how this compares to NIV treatment without a modem.
To gain perspectives of HCPs on the use of modem technology in caring for patients with ventilatory failure and explore how this compares to delivering domiciliary NIV treatment without a modem.
Methods
Design
This was a single centre study conducted at the Royal Free London National Health Service (NHS) Foundation Trust Sleep and Ventilation Service using qualitative methods. Patients and or carers were provided with study information and invited to participate in the study via 1:1 telephone or a face-to-face semistructured interview. HCPs participated via focus groups. Recruitment was a convenience sample of patients, carers and staff willing and available to participate. HCPs completed and returned their consent forms at the time of the focus groups. This study was conducted in a London based sleep and ventilation service with a wide geographical spread of patients. The modem technology in this study was a cellular modem (Cellular Modem, Philips Respironics, Murraysville, USA) which was inserted into the back of the patient’s ventilator (A40, A30 or BiPAP ST, Philips Respironics, Murraysville, USA). Data were transmitted on a daily basis and were accessible via a web-based platform (Encore Anywhere, Philips Respironics, Murraysville, USA).
Patient and public involvement
The development of this research was informed by the previous quantitative work,15 which informed the development of the topic guide as well as assisting in identification of eligible participants. The topic guide was developed by authors involved in both studies (SKM and MJW). Patients were involved in designing the topic guides and the patient information sheets. The dissemination report was reviewed by lay volunteers accessible to the researchers. The dissemination report was sent to all participants including patients, carers and HCPs.
Participants and recruitment
Patients
The study aimed to recruit 20 patients, this was a convenience sample. A sample size of 20 has been shown in other qualitative studies to provide sufficient depth of data. Patients were identified from users of domiciliary NIV within the Sleep and Ventilation Service by their current clinician through existing clinical databases. All eligible patients were contacted via telephone by a member of the research team who was not part of their day to day clinical team to ask for permission to send them information about the study. A mailshot was sent to all patients who gave permission to be contacted in relation to this study. Recruitment was conducted by a member of the research team who was independent of the clinical team to avoid potential participants feeling under duress to take part. Patients were recruited in the order that they responded to the mailshot. Patients were offered a voucher to the value of £20 for taking part in the study and in recognition of their help with the study.
Carers
Additionally, the study aimed to recruit 20 carers this was a convenience sample. A sample size of 20 has been shown in other qualitative studies to provide adequate data. Carers were recruited via current users of the domiciliary NIV service, a database of carers is not held by the Sleep and Ventilation Service. As such recruitment of carers was reliant on patients sharing information with their carers; therefore, if patients did not consent to the mailshot their carers would not have been aware of the study. Patients were asked to share the study information with anyone who provided care for them. Patients were asked to give informed consent for their carer to be approached about participating in the study; carers could participate in the study even if the patient did not wish to take part. A member of the research team who was independent of the clinical team undertook the recruitment procedure. Carers were offered a voucher to the value of £20 for taking part in the study and in recognition of their help with the study. Interviews could take place as a dyad that is, the patient and their carer, or on an individual basis.
Health care professionals
The study aimed to recruit a minimum of six and a maximum of 12 HCPs from the multidisciplinary team. A sample size of 12 was chosen for convenience and was considered to be realistic given the limited pool of staff who would have the relevant experience of delivering care to sleep and ventilation patients both with and without a modem. Potential HCP participants were identified from the respiratory team by one of the study team (SKM) who had an understanding of staff members’ backgrounds. A member of the research team independent of the clinical team sent out information via work emails highlighting the opportunity to participate in the study. Staff were invited to take part in the study during working hours with the permission of their line manager. Staff who took part in the study were provided with refreshments in appreciation of their time and certificate of participation for their professional development portfolio.
Inclusion and exclusion criteria
Patients and their carers had to have received treatment from the sites domiciliary NIV service both premodem and postmodem installation. HCPs had to have experience of looking after patients with NIV both with and without modems. Patients under the care of the domiciliary NIV service who only had experience of treatment with NIV with a modem in situ were not eligible to take part. Patients unable to verbally communicate in English were likewise excluded.
Data collection methods
Data collection took place between July and December 2017. Semistructured telephone interviews with patients and carers were audio recorded. The three HCP focus groups were conducted in the work place in a private, quiet room and audio recorded. All of the interviews and focus groups were conducted by the same male researcher (MJW) who was not part of the clinical team and this person also facilitated the three focus groups. Focus groups were chosen for the HCPs to enhance convenience and aid recruitment. Focus groups are forums for coconstructed knowledge, allowing for exchange and development of ideas among the participants as well as an opportunity to discuss differing opinions.16 Interviews were chosen for the patients and carers to allow an increased depth of data to be gathered.16 It was also felt that patients and carers may be more likely to be open and express freedom of speech in an interview than a focus group. Additionally, this patient group have poor health status and the option of a telephone interview avoided the need for patients to travel, if they so wished. Previous field work15 had provided some a priori topics and combined with experience in the clinical area enabled the researchers to develop a topic guide for both the interviews and focus groups (see online supplementary files 1 and 2). The topic guide was developed to allow participants to speak freely, encourage diversity in answers given and sought to seek experiences and opinions on the use of the modem technology. This included questions such as:
bmjresp-2019-000510supp001.pdf (24.7KB, pdf)
bmjresp-2019-000510supp002.pdf (23.5KB, pdf)
What would you say has been good about the new ventilator compared to the old?
How does using the new machine make you feel?
How does using a modem with on the ventilators impact on your practice?
Data analysis
All interviews and focus group sessions were transcribed verbatim by a transcription service and were checked for accuracy against the recordings by one of the researchers (MJW). The text was imported into QSR Nvivo (V.12) for data management and analysis. The process of data analysis used was a modified framework analysis.17 Categories were developed by the researcher (MJW) and key practitioner (SKM) deductively and inductively, the former was based on results from a previous study.15 This method is in keeping with the use of Framework Analysis17 which incorporates both deductive and inductive codes, thus allowing a priori and experiential aspects to be included. As transcripts were read several times as part of the familiarisation process, induction and deductive codes were identified and applied during the steps of data analysis. Associated words and ideas were labelled and organised into a conceptual framework of themes. MJW identified the initial codes and subsequent categories, with rigour of this stage being enhanced through discussion with the key practitioner (SKM). The conceptual framework was further developed and validated through subsequent discussions between MJW and SKM, with themes shared with the wider research team (CK, SM, FG) to ensure the themes were comprehensive and reflective of the interviews and focus group discussions.
Results
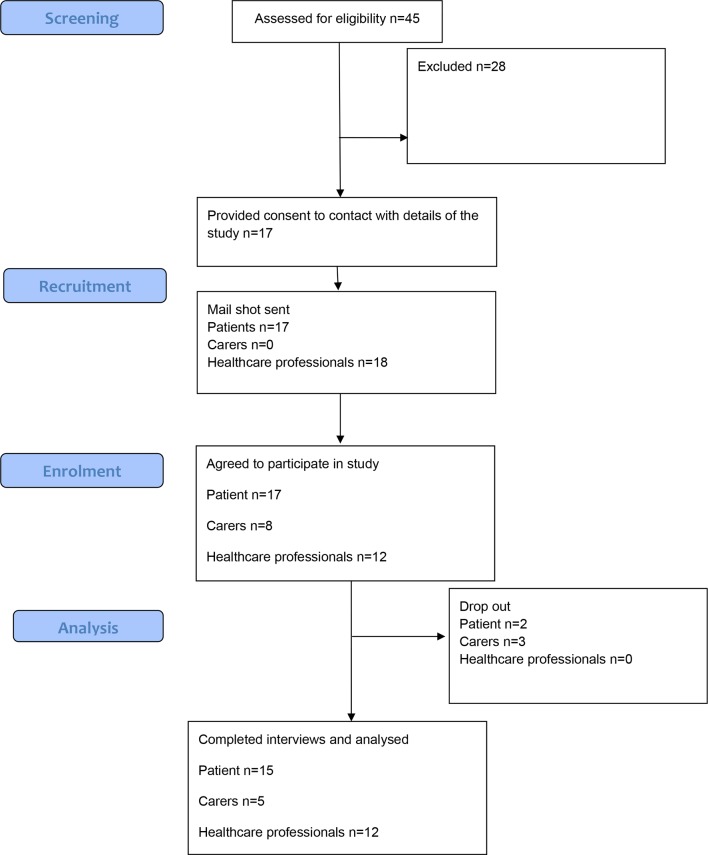
A potential 49 patients and their carers were eligible for the study. A total of 15 patient and 5 carer interviews were conducted including four dyad pairings, figure 1 shows the flow of participants through the study. Recruitment of patients and carers did not meet the intended numbers. Patients who were unable to converse in English were excluded as shown in the flow diagram. Three focus groups were conducted with 12 HCPs with an average of four per group. Demographics of the participants are available in online supplementary file 3. There was a tendency towards more male participants (M:F; HCPs 7:5, patients 11:6, carers 4:1). Most HCPs were within the age ranges of 25–34 (n=4) or 35–44 (n=6), while patients were within the age ranges of 65–74 (n=8) and 75–84 (n=5). Most participants were White British (HCPs n=9, patients n=12, carers n=4). Patients had been receiving domiciliary NIV for a mean (SD) of 4.31 (2.19) years. HCPs had been providing domiciliary NIV services for either 1–5 (n=6), 6–10 (n=3), 11–15 (n=2) or 16–20 years (n=1) years.
Figure 1.
Flowchart of recruitment of participants.
bmjresp-2019-000510supp003.pdf (35.8KB, pdf)
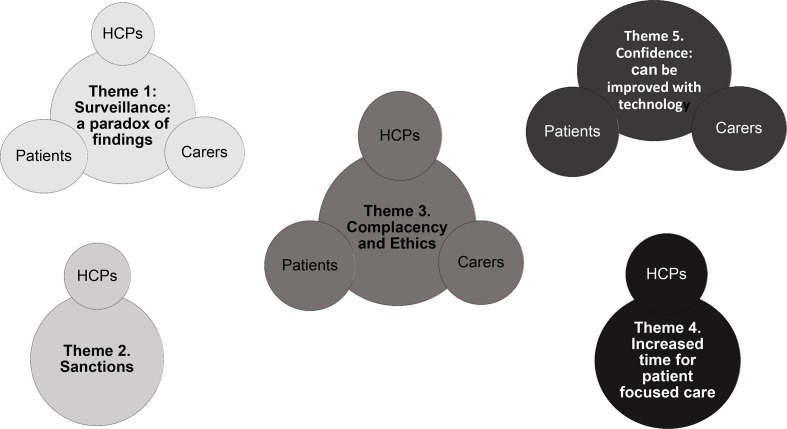
The analysis of the interviews and focus groups resulted in five themes: ‘Surveillance: a paradox of findings’, ‘Sanctions’, ‘Complacency and ethics’, ‘Efficiencies of healthcare provision’ and ‘Confidence: can be improved with technology’. These themes are discussed below and supported with representative quotations. Figure 2 illustrates how data from the HCP focus groups and patient and carer interviews' data contributed to the development of each theme.
Figure 2.
Mind map illustrating contribution of data sources to each theme. HCP, healthcare professional.
Theme 1. Surveillance: a paradox of findings
HCPs expressed concerns about the ethics of surveillance and whether patients perceived their lives were being unduly scrutinised. Additionally, staff expressed concerns regarding the impact of surveillance on the patient-HCPs relationship (Quotes 1, table 1).
Table 1.
Representative quotes for theme 1. Surveillance: a paradox of findings
| Quotes 1 | A lot of them do say, ‘You've been spying on me’. I had one, ‘What does your spy report today?’ So they probably feel—I think they're more aware that you're keeping tabs on them. It might improve their compliance, but it might make them resent you slightly, I don't know. (HCP Focus Group 1) |
| Quotes 2 | I think it’s about the terminology that you use with the patient. I’ve had a couple where they think that I can hear and I can see what’s going on in their bedroom and then you have to explain to them, no, I can't hear and I can't see. (HCP Focus Group 2) |
| Quotes 3 | Interviewer: Okay, so how do you feel about the fact that it’s being monitored remotely? Is that something that you think about at all? Patient D: None at all. None at all, none at all. I have had friends seeing the graphs, when I visit the Royal [Free Hospital]. It doesn’t really bother me at all. Interviewer: Okay. You’ve never felt that it’s intrusive, that they are monitoring you? Patient E: No, not at all. Interviewer: Right. And how do you feel about the hospital being able to record the information? Patient F: Well, it doesn’t bother me at all dear, I’m glad I have somebody to ask how I’m getting on. Patient A: I take no notice. Patient C: I don’t even think about it. Patient E: They are keeping an eye on me. Interviewer: Are you happy that the machine is monitoring you? Do you feel safer or do you feel like you’re being watched? Patient G: I didn’t feel anything at all because when I go through the consultant, she will be able to tell me what … is going on and everything and it works out fine. Twice, at least, I have seen her and she said it’s perfectly fine. |
It was suggested that some of the patients’ concerns stemmed from misconceptions, for example, the remote monitoring system recorded sound and visual data (ie, they thought they could be seen and heard via the modem) rather than solely data from the patient’s ventilator (Quotes 2, table 1).
The patient and carer interviews focused in particular on the respondents’ perceptions about remote monitoring. The aim was to explore the range of emotive responses to being monitored via a modem. Using the topic guide, patients and carers were guided to explore any concerns about surveillance and also about whether the monitoring made them feel more secure or confident. The main narrative was they welcomed it and there were no concerns expressed from patients or carers regarding undue surveillance. During one focus group discussion, it was noted there had been no reported cases of patients declining the modem and the general perspective was that patients were not concerned about the monitoring, this observation was supported in the patient interviews (Quotes 3, table 1).
Concerns expressed by HCPs regarding surveillance were not corroborated by patients or carers.
Theme 2. Sanctions
From the HCPs focus groups it emerged that remote monitoring had enabled clinicians to conduct a more rigorous and methodical assessment of appropriate withdrawal of ventilators in patients who were non-adherent with treatment. Patients who were not using their ventilators as prescribed, were given an opportunity for review of their ventilator prescription (including the use of interfaces and humidification) with troubleshooting of any identified concerns. Risks and benefits of adherence and non-adherence to treatment were explained to the patients. Where patients were consistently non-compliant, they were advised their ventilator would be removed if utilisation did not improve following the shared problem-solving discussion. This process, it was suggested, allowed HCPs the option of offering the ventilators to assess patient compliance in their own environment even in cases where they were not initially confident about patient compliance (Quotes 1, table 2). This theme was developed from the HCPs focus groups alone and was silent in the patient and carer transcripts.
Table 2.
Representative quotes for theme 2. Sanctions
| Quotes 1 |
We’ll give patients an opportunity and we'll review them, if they're not compliant … we'll give them a chance to change that. But if they're persistently not compliant … then we're able to have that conversation with them about … about risks and benefits and they've not been compliant and say, ‘We're going to retrieve the machine’ and discharge them from our care. (HCP Focus Group 1) We say to them, ‘Okay, we're going to give you six weeks to demonstrate to us whether you can use it or not’. So it gives them more opportunity, we're able to offer it to more patients, than we maybe would have otherwise, which I think is a good thing. It makes it more equitable care. (HCP Focus Group 1) It allows you to have a much more open conversation, doesn’t it? You can say, ‘If you don’t improve your compliance by the next time I see you we’re going to take the machine away’, and they know that you’ve set out what’s going to happen. (HCP Focus Group 3) |
HCPs reported the remote monitoring increased access and equity of care.
Theme 3. Complacency and ethics
The theme of ‘complacency’ emerged from both the focus group and interview data. There was a concern expressed by the HCPs in the focus groups that patients might become complacent because they think their condition is being continuously monitored (Quotes 1, table 3). Data from the patient and carer interviews suggested that patients might mistakenly believe they are being monitored continuously (Quotes 2, table 3).
Table 3.
Representative quotes for theme 3. Complacency and ethics
| Quotes 1 |
I don't know if that's this setting, but do you ever get the feeling that they're ignoring things, because they feel like the computer would have told you about it? So that they're not going to call up or they're not going to seek help for a potential problem, because they feel like you should already know, because of the web-based system. (HCP Focus Group 1) I'm not sure about that, and I think that’s where my slight, my only concern with it really is that people may—I wonder if people might not seek medical advice because they think that they are being kept an eye on, is my concern with it, sort of where there’s a false reassurance. (HCP Focus Group 2) Yes, like Big Brother, they’re thinking that if anything goes wrong we would pick it up. Whereas now, I particular word it as, ‘If there is a problem we will look at your data and we can fix it remotely’. (HCP Focus Group 3) |
| Quotes 2 | Patient H: Well, I think if there’s something really wrong with me, the hierarchy at the other end will know about it, without me having ring up … that makes me feel much more secure. Patient I: Well, it makes you feel more comfortable, because you know that if anything goes wrong, it will immediately be spotted. Carer 3: … especially if there was to be any problems with his breathing, I know the hospital is aware of it at the same time as me probably. |
| Quotes 3 |
The main down side as I see it is that you sort of tell somebody that you’re watching them but then are you watching them all the time? I think that there’s something slightly strange ethically about that. Then the other thing is if you’re keeping an eye on them and something terrible had happened to them, I don’t think that we have a way to find that out or act upon the information. (HCP Focus Group 2) … if you’ve got a ventilator that’s got the data recorded and you’re not looking at it, that’s like taking a blood test and then not checking the result. You could argue it the other way as well, couldn’t you? Maybe the modem adds a different dimension to it but historically we had ventilators that had cards in them that were recording data and generally in the field lots of places don’t make use of the card data so then you’ve got data available to you that you’re not using, that’s maybe just as much of an ethical issue as if you’ve got data that you’re not checking every day. I don’t know. (HCP Focus Group 2) |
Therefore, data from both focus groups and the interviews seem to suggest patients may become complacent and not seek appropriate medical attention when they become unwell due to the remote monitoring (Quotes 1 and 2, table 3).
The focus groups expressed concern about the ethical dilemma of not responding to monitored ventilator data immediately, especially if the patient was unwell, and the resulting outcomes. Similarly, there was a narrative about informing patients they were being monitored but this was not continuous or necessarily routine (Quotes 3, table 3).
HCPs were concerned some patients became complacent as a result of the modem monitoring, and there was some suggestion this was the case from the patient and carer interviews.
Theme 4. Increased time for patient focused care
HCPs in the focus groups described a number of ways in which the new system was more efficient; making clinical appointments less necessary and when they did occur, they were more effective (Quotes 1, table 4).
Table 4.
Representative quotes for theme 4. Increased time for patient focused care
| Quotes 1 |
That’s helpful, because in … another unit [where] I’ve worked before, people would phone up and say, ‘My machine’s gone wrong’, but actually you wouldn’t know [why), and you’d have to say, ‘Press this button, read what it says on the screen …’ So, I’ve not had that [facility] before. (HCP Focus Group 3) We're not having to bring them back as frequently, because we're able to see that everything is okay. We're not bringing people back. You know, they're all quite sick patients really, the fact that they're on home ventilation. So there would be a tendency to want to keep an eye on them and check on them regularly. And we're not having to do that as frequently as we might have done, historically. (HCP Focus Group 1) |
| Quotes 2 |
I'm extrapolating slightly, but whenever I do clinics where I've been able to prepare in advance with information about the patients about the tests that I've done, when I've got all that information to hand, it means that the actual clinic visit for the patient, a bit more time to have more patient-focused discussion. You've got more time for speaking, rather than you finding out about compliance and finding out- asking all these questions that you've already prepared in advance. (HCP Focus Group 1) It’s usually if they’ve rung up and said there’s a problem, then if they’re on the phone we can just ask them to press the button, we can see from the last point they’ve worn it, and try and problem solve from there. (HCP Focus Group 3) |
| Quotes 3 |
Yes, because when they first brought it in it did seem like it would reduce the workload because, obviously, you’d just wait and firefight, so wait for a phone call to come in and then sort it. Whereas now, you’re getting all the information in and you’ve got to flag up alarms, and if you’re monitoring them then you can say that, technically, it does create extra work. (HCP Focus Group 3) So I think overall it's time saving. There are some patients where it's more time consuming, because we're checking on them more regularly or they're being problematic. But if you took the cohort as a whole, I think it's more time efficient. (HCP Focus Group 1) |
HCPs described how having easy access to the ventilator data allowed them to make prompt informed assessments when dealing with patient telephone enquiries. Having ‘real time’ ventilator data available meant that patients were not having to attend hospital appointments as often as they had been (Quotes 1 and 2, table 4).
Focus group participants suggested having access to ventilator data prior to an outpatient appointment provided the opportunity to focus their attention on the patient’s key needs rather than spending time assessing and corroborating compliance data. While the narrative across all three focus groups supported the view, the new system was more efficient and effective, HCPs questioned whether it had saved time overall (Quotes 3, table 4).
It was suggested that more time had been spent preparing for the appointment and that the additional data available required further scrutiny and potentially changes to the regime which might not otherwise have occurred.
Theme 5. Confidence: can be improved with technology
When prompted to consider whether they felt more secure and/or confident as a result of the monitoring the narrative from both the patient and carer interviews was especially positive (Quotes 1, table 5).
Table 5.
Representative quotes for theme 5. Confidence: can be improved with technology
| Quotes 1 | Interviewer: Do you feel safer? Or more comfortable or confident about it? Patient F: Well I feel confident and safer that somebody knows what’s going on, and how I’m progressing. So when I go to the clinic, the consultant, you know, takes me to the room, that the lady has everything, and she deals with me. If anything is going wrong and she will tell him. Interviewer: What about feeling safer, or more confident? Patient Q: Well I feel safer because if there’s something wrong, it’s flagged up at the hospital. Carer 3: Yes, because I just know, especially if there was to be any problem with his breathing, I know that the hospital is aware of it at the same time as me probably. Or if there was a problem that I couldn't pick up, it would certainly pick up on the modem, and they would phone us and say it needs altering or whatever. That makes me feel far more confident. |
| Quotes 2 | Carer 2: We can see the difference now, because when she was using the old one she was [retaining] carbon dioxide, which means maybe the settings - even though the settings were done—it's different now, the new one now, they did the settings and the carbon dioxide level is quite low, compared with the other one, the first one. So that's why they changed it to say this one is more powerful, and it can adjust to her breathing rhythm, so that it's not too difficult for her. Interviewer: Yes. Okay. So your health, you think it's deteriorated a little bit. I'm just wondering whether you attribute that to the new modem, or do you think that would have happened anyway? Patient B: I think it would have happened anyway. Interviewer: Well that’s very good. And would you say that improvement in your health is connected to the way that they can monitor your usage of the machine? Patient F: Yes, because there’s no other way they could have done it. With one in my nose that I use in the day, they can’t monitor that. And I’m only on half a litre, so that goes right through the night, and I think it’s quite good. I feel good, because I dropped off to sleep very quick’. |
The patient perception of their health status in the interviews varied. Some reported improvements and believed the new regime had made a difference, some felt their health had remained the same (including those who claimed there had been no deterioration due to the new regime) but in other cases the patient and/or carer explained their situation had deteriorated due to the nature of their conditions and increasing age. On no occasion, however, was this deterioration attributed to the ventilator remote monitoring. On other occasions improvements were attributed to enhancements in the interface rather than to the remote monitoring (Quotes 2, table 5).
Patients and carers were positive about the impact of the modems on their health and well-being, particularly their confidence.
Discussion
To our knowledge this is the first qualitative study conducted in the field of sleep and ventilation investigating patients, carers and HCPs' opinions on the use of modem technology to manage patients with domiciliary NIV.
The use of domiciliary NIV for patients with chronic hypercapnic ventilatory failure is standard care for patients with neuromuscular disease and chest wall deformities and is increasingly recognised as appropriate for those with obesity related respiratory failure and Chronic Obstructive Pulmonary Disease (COPD).3 5 18–22 However, clinicians recognise that patients’ ability to comply with NIV at home is multifactorial and complex. There are often many socioeconomic factors to take into consideration when reasoning whether a patient should be issued with domiciliary NIV or not. In our clinical practice, and as supported by the results of this study, the use of modem technology enables increased equity and accessibility of care for patients at high risk of non-concordance with treatment. The use of remote monitoring technology allows the clinicians working in the service to support patients in the community to assess their ability to concord with treatment. Additionally, the approach of ongoing assessment of concordance with treatment and subsequent removal of ventilators where patients are unable to be concordant with treatment despite all supportive strategies, as highlighted in the HCP focus groups, could be viewed as ensuring judicious use of healthcare resources.
The HCPs in the focus groups highlighted they felt the modem technology had increased their efficiency. Overall, they did not necessarily report the use of modem technology had saved them time, it was not within the aims and objectives of this study to assess cost effectiveness or healthcare utilisation and so there is no quantitative data to support or refute this qualitative finding. Certainly, further investigation is warranted into the cost benefit implications of modem technology for patients receiving domiciliary NIV. The results of this study could help inform the design of a cost benefit analysis.
Concerns regarding surveillance expressed by HCPs were not corroborated by patients, suggesting acceptability of the concept of remote monitoring. This is in contrast to a European Respiratory Society/European Lung Foundation survey which found that in European countries (primarily Germany, Netherlands, Italy and Spain) only 47% of patients and 62% of carers were happy to be monitored remotely.23 This suggests that maybe UK patients and carers are more willing to accept remote monitoring than their European counterparts. Perhaps the clinical area where surveillance is most routinely used is in cardiology where implantable devices with remote monitoring have been used for many years. Results from our study suggests remote monitoring is acceptable to patients and concurs with patient satisfaction questionnaires in cardiology studies which reported remote monitoring of implantable devices was acceptable for patients and healthcare workers.24 25 Similarly stroke survivors using virtual reality for lower limb rehabilitation found the technology acceptable and demonstrated an increased compliance with treatment.26 Conversely, a stroke survivor study that explored the use of technology at home reported concern about a ‘big brother’ effect, although of note these participants lacked confidence with technology.26
Despite a potentially negative impact on self-efficacy resulting in complacency, both patients and carers reported an increase in confidence due to the remote monitoring. It is recognised that domiciliary NIV is associated with a high carer burden.27 28 The results of this study suggest the use of remote monitoring can increase confidence of carers. Further research is required to investigate whether remote monitoring could help to reduce carer burden. The results of this study could help inform such a study design.
The theme of Complacency requires further investigation. Complacency was a concern expressed by the HCPs in the focus groups and it seems from the patient and carer interviews there may be a degree of complacency brought about by the surveillance aspect of the modem technology. Previously, the use of telemonitoring in patients receiving domiciliary NIV has been investigated.29 Telemonitoring is a different, but perhaps in some ways, comparable technology to remote monitoring via modems.13 In the TELECraft study the authors found a reduction in self-efficacy when patients underwent telemonitoring.29 It could be speculated therefore that the use of any form of remote monitoring can reduce self-efficacy and potentially bring about complacency in seeking appropriate medical interventions. Conversely, there is a move towards increasing patients’ ability to self-manage their conditions. In the UK, the use of technology to facilitate self-management is heavily referenced and relied on in the government’s aim to increase efficiencies and deliver its objective of future proofing the NHS.30 In the ‘ethics’ theme, HCPs expressed concerns regarding the ethics of how frequently data would be monitored. However, domiciliary NIV devices have had the ability to monitor data via secure data cards prior to the development of modem technology and yet anecdotally, the use of data from ventilators is not routine practice in many services. One could argue there are ethical concerns regarding having assessment data available which is not routinely reviewed or acted on. HCPs should ensure a careful narrative with patients about how frequently data received via remote monitoring is checked and assessed. Furthermore, a narrative regarding seeking appropriate medical attention and advice is imperative in ensuring appropriate healthcare utilisation in these patients with chronic health conditions. Information regarding these discussions should be provided in a variety of mediums including both verbally and written.
Within the UK, it is recognised there are geographical areas where a lack of digital skills and literacy is impacting on health outcomes.31 In order to use digital technology to enhance health outcomes for populations, further qualitative research is required to comprehend the acceptability of technology by patients, their carers and HCPs. Furthermore, research is required into patients, carers and HCPs willingness to engage in education to develop their digital literacy skills.31 In the UK, Health Education England have developed a framework for increasing the digital literacy of staff and NHS digital have commissioned work to engage patient populations to develop methods of embedding digital literacy training into communities.31 32 Qualitative research will be a useful tool in comprehending both the barriers and enablers to use of digital and technology in healthcare. Further understanding is required of how we can best use digital and technology in healthcare.
Limitations
This was a UK, urban, large city-based study and the authors acknowledge that different cultures and socioeconomic settings would probably produce different results. This fact could reduce the transferability of the findings from this study outside of the UK. The study aimed to recruit 20 patients and 20 carers: recruiting carers was particularly challenging. The participants in this study were predominantly White British. A larger sample size may have allowed for a greater demographic spread which may have resulted in different themes emerging. An independent researcher (MJW) conducted the interviews and focus groups thus increasing credibility.33 The use of an incentive voucher (for a UK high street retailer) may have affected the willingness of patients and carers and encouraged them to participate in the study. The participants were self-selecting and it is acknowledged in research methodology that patients who engage in research are not always truly representative of the population, this fact may have created some selection bias in our sample. Additionally, the carers could only be recruited from patients who had agreed to be contacted about the study and where patients provided their carers with the information about the study. This may have created further selection bias. Furthermore, the numbers of carers recruited were less than the number of patients and less than the intended numbers. However, given the paucity of data in this field including the carer data was felt to be relevant. Finally, the HCPs were those working at the research site, many of whom had mostly worked in London, which could have limited the experiences shared and therefore the themes developed from the HCPs focus group.
Conclusion
This is the first study to investigate patients, carers and HCPs' experiences and perspectives on using modem technology in the management of domiciliary NIV. Modem technology was acceptable and considered a useful addition by HCPs, patients and carers. Further research is required into the issue of complacency associated with modem technology. This qualitative study has provided an important and useful narrative on the use of remote monitoring for patients receiving domiciliary NIV. It could be used to inform future studies and service design and provides an example of patient and public engagement.
Acknowledgments
The authors would like to thank the participants of this study, including staff at the Royal Free London NHS Foundation Trust.
Footnotes
Contributors: SKM: conceived the idea, sourced funding, developed the protocol, sought ethical and other permissions, acted as the principal and chief investigator and developed the manuscript. MJW: developed the protocol, collected the data, analysed the results and contributed to the manuscript development. FG: recruited participants, gained signed informed consent, maintained the site file, assisted in permissions and day to day operational running of the study and contributed to the manuscript. CK: assisted in permissions and day to day operational running of the study and made substantial contributions to the development of the manuscript. SM: developed the protocol, recruited participants and made substantial contributions to the development of the manuscript.
Funding: This study was partially funded by Philips Respironics UK. The funding provided covered the cost of: postage and packaging for recruitment, the independent researcher who both conducted and analysed the interviews and focus groups, the incentive voucher is provided to patients and carers, and refreshments provided the focus groups. Philips Respironics UK were not involved in the design of the study, the data collection, the data analysis, the interpretation of the data or the preparation of this manuscript.
Competing interests: SKM and SM have received honorarium from Philips Respironics for providing lectures and education. SKM and SM have received research grants from Philips Respironics.
Patient consent for publication: Not required.
Ethics approval: Ethical approval for this study was obtained from East Midlands—Nottingham 2 Research Ethics Committee Reference: 16/EM/0427.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: No data are available. The datasets generated and/or analysed during the current study are not publicly available in order to maintain participant anonymity, but are available from the corresponding author on reasonable request.
References
- 1.Murphy PB, Rehal S, Arbane G, et al. . Effect of home noninvasive ventilation with oxygen therapy vs oxygen therapy alone on hospital readmission or death after an acute COPD exacerbation: a randomized clinical trial. JAMA 2017;317:2177–86. 10.1001/jama.2017.4451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Institute for Health and Clinical Excellance Motor neurone disease: the use of non-invasive ventilation in the management of motor neurone disease. London: National Institute for Health and Clinical Excellance, 2010. [PubMed] [Google Scholar]
- 3.National Institute for Health and Care Excellence Motor neurone disease: assessment and management: NICE guideline NG42 2016.
- 4.Bourke SC, Tomlinson M, Williams TL, et al. . Effects of non-invasive ventilation on survival and quality of life in patients with amyotrophic lateral sclerosis: a randomised controlled trial. Lancet Neurol 2006;5:140–7. 10.1016/S1474-4422(05)70326-4 [DOI] [PubMed] [Google Scholar]
- 5.Simonds AK, Elliott MW. Outcome of domiciliary nasal intermittent positive pressure ventilation in restrictive and obstructive disorders. Thorax 1995;50:604–9. 10.1136/thx.50.6.604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Elliott MW. The interface: crucial for successful noninvasive ventilation. Eur Respir J 2004;23:7–8. 10.1183/09031936.03.00115903 [DOI] [PubMed] [Google Scholar]
- 7.Boussaïd G, Lofaso F, Santos DB, et al. . Factors influencing compliance with non-invasive ventilation at long-term in patients with myotonic dystrophy type 1: a prospective cohort. Neuromuscul Disord 2016;26:666–74. 10.1016/j.nmd.2016.07.014 [DOI] [PubMed] [Google Scholar]
- 8.Werpachowska A, Inayat B, Howard M, et al. . One-Year experience of domiciliary non-invasive ventilation (NIV) monitoring via wireless modem in a district general Hospital (DGH). Eur Respir J 2016;48:PA2163. [Google Scholar]
- 9.Lopes de Almeida JP, Pinto A, Pinto S, et al. . Economic cost of home-telemonitoring care for BiPAP-assisted ALS individuals. Amyotroph Lateral Scler 2012;13:533–7. 10.3109/17482968.2012.703675 [DOI] [PubMed] [Google Scholar]
- 10.Pinto A, Almeida JP, Pinto S, et al. . Home telemonitoring of non-invasive ventilation decreases healthcare utilisation in a prospective controlled trial of patients with amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry 2010;81:1238–42. 10.1136/jnnp.2010.206680 [DOI] [PubMed] [Google Scholar]
- 11.Borel J-C, Pelletier J, Taleux N, et al. . Parameters recorded by software of non-invasive ventilators predict COPD exacerbation: a proof-of-concept study. Thorax 2015;70:284–5. 10.1136/thoraxjnl-2014-206569 [DOI] [PubMed] [Google Scholar]
- 12.Villanueva JA, Suarez MC, Garmendia O, et al. . The role of telemedicine and mobile health in the monitoring of sleep-breathing disorders: improving patient outcomes. Smart Homecare Technology TeleHealth 2017;4:1–11. 10.2147/SHTT.S108048 [DOI] [Google Scholar]
- 13.Ambrosino N, Vitacca M, Dreher M, et al. . Tele-monitoring of ventilator-dependent patients: a European respiratory Society statement. Eur Respir J 2016;48:648–63. 10.1183/13993003.01721-2015 [DOI] [PubMed] [Google Scholar]
- 14.Gallar P, Vigil A, Rodríguez I, et al. . Two-Year experience with telemedicine in the follow-up of patients in home peritoneal dialysis. J Telemed Telecare 2007;13:288–92. 10.1258/135763307781644906 [DOI] [PubMed] [Google Scholar]
- 15.Mansell SK, Cutts S, Hackney I, et al. . Using domiciliary non-invasive ventilator data downloads to inform clinical decision-making to optimise ventilation delivery and patient compliance. BMJ Open Respir Res 2018;5:e000238 10.1136/bmjresp-2017-000238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 17.Gale NK, Heath G, Cameron E, et al. . Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13:117 10.1186/1471-2288-13-117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shneerson JM, Simonds AK. Noninvasive ventilation for chest wall and neuromuscular disorders. Eur Respir J 2002;20:480–7. 10.1183/09031936.02.00404002 [DOI] [PubMed] [Google Scholar]
- 19.Agency for Clinical Innovation Respiratory Network Domiciliary non-invasive ventilation in adult patients: a consensus statement. Australia: Agency for Clinical Innovation Respiratory Network, 2012. [Google Scholar]
- 20.Simonds AK. Home mechanical ventilation: an overview. Ann Am Thorac Soc 2016;13:2035–44. 10.1513/AnnalsATS.201606-454FR [DOI] [PubMed] [Google Scholar]
- 21.Priou P, Hamel J-F, Person C, et al. . Long-Term outcome of noninvasive positive pressure ventilation for obesity hypoventilation syndrome. Chest 2010;138:84–90. 10.1378/chest.09-2472 [DOI] [PubMed] [Google Scholar]
- 22.Köhnlein T, Windisch W, Köhler D, et al. . Non-Invasive positive pressure ventilation for the treatment of severe stable chronic obstructive pulmonary disease: a prospective, multicentre, randomised, controlled clinical trial. Lancet Respir Med 2014;2:698–705. 10.1016/S2213-2600(14)70153-5 [DOI] [PubMed] [Google Scholar]
- 23.Masefield S, Vitacca M, Dreher M, et al. . Attitudes and preferences of home mechanical ventilation users from four European countries: an ERS/ELF survey. ERJ Open Res 2017;3:15–7. 10.1183/23120541.00015-2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ricci RP, Morichelli L, Quarta L, et al. . Long-Term patient acceptance of and satisfaction with implanted device remote monitoring. Europace 2010;12:674–9. 10.1093/europace/euq046 [DOI] [PubMed] [Google Scholar]
- 25.Marzegalli M, Lunati M, Landolina M, et al. . Remote monitoring of CRT-ICD: the multicenter Italian CareLink evaluation--ease of use, acceptance, and organizational implications. Pacing Clin Electrophysiol 2008;31:1259–64. 10.1111/j.1540-8159.2008.01175.x [DOI] [PubMed] [Google Scholar]
- 26.Warland A, Paraskevopoulos I, Tsekleves E, et al. . The feasibility, acceptability and preliminary efficacy of a low-cost, virtual-reality based, upper-limb stroke rehabilitation device: a mixed methods study. Disabil Rehabil 2019;41:1–16. 10.1080/09638288.2018.1459881 [DOI] [PubMed] [Google Scholar]
- 27.Aoun SM, Bentley B, Funk L, et al. . A 10-year literature review of family caregiving for motor neurone disease: moving from caregiver burden studies to palliative care interventions. Palliat Med 2013;27:437–46. 10.1177/0269216312455729 [DOI] [PubMed] [Google Scholar]
- 28.MacLaren J, Smith P, Rodgers S, et al. . A qualitative study of experiences of health and social care in home mechanical ventilation. Nurs Open 2019;6:283–92. 10.1002/nop2.213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chatwin M, Hawkins G, Panicchia L, et al. . Randomised crossover trial of telemonitoring in chronic respiratory patients (TeleCRAFT trial). Thorax 2016;71:305–11. 10.1136/thoraxjnl-2015-207045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.National Health Service NHS Long term plan. NHS, 2019. [Google Scholar]
- 31.NHS Digital Digital inclusion for health and social care. NHS Digital, 2018. [Google Scholar]
- 32.NHS Health Education England NHS Long Term Plan : NHS digital. digital inclusion for health and social care. NHS Digital, 2018. [Google Scholar]
- 33.Guba EG, Lincoln YS. Competing paradigms in qualitative research In: Handbook of qualitative research. 2, 1994: 163–94. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjresp-2019-000510supp001.pdf (24.7KB, pdf)
bmjresp-2019-000510supp002.pdf (23.5KB, pdf)
bmjresp-2019-000510supp003.pdf (35.8KB, pdf)