Abstract
Objectives
Iron deficiency (ID), with or without anaemia (IDA), is an important comorbidity in people with chronic heart failure (HF), but the prevalence and significance in those admitted with HF is uncertain. We assessed the prevalence of ID or IDA in adults (age ≥21 years) hospitalised with a primary diagnosis of HF, and examined key metrics associated with these secondary diagnoses.
Methods
A retrospective cohort study of Hospital Episode Statistics describing all adults admitted to National Health Service (NHS) hospitals across England from April 2015 through March 2016 with primary diagnostic discharge coding as HF, with or without subsidiary coding for ID/IDA.
Results
78 805 adults were admitted to 177 NHS hospitals with primary coding as HF: 26 530 (33.7%) with secondary coding for ID/IDA, and 52 275 (66.3%) without. Proportionately more patients coded ID/IDA were admitted as emergencies (94.8% vs 87.6%; p<0.0001). Tending to be older and female, they required a longer length of stay (15.8 vs 12.2 days; p<0.0001), with higher per capita costs (£3623 vs £2918; p<0.0001), the cumulative excess expenditure being £21.5 million. HF-related (8.2% vs 5.2%; p<0.0001) and all-cause readmission rates (25.8% vs 17.7%; p<0.05) at ≤30 days were greater in those with ID/IDA against those without, and they manifested a small but statistically significant increased inpatient mortality (13.5% v 12.9%; p=0.009).
Conclusions
For adults admitted to hospitals in England, principally with acute HF, ID/IDA are significant comorbidities and associated with adverse outcomes, both for affected individuals, and the health economy.
Keywords: acute heart failure, iron deficiency, anaemia, hospital episode statistics, outcomes
Key questions.
What is already known about this subject?
Iron deficiency is increasingly recognised as an important comorbidity in heart failure and impacts patient well-being. Most data on diagnosis and subsequent treatment have been garnered from ambulatory patients with chronic heart failure, and there is a relative paucity of information relating to those with acute heart failure.
What does this study add?
In this retrospective cohort study, we analysed Hospital Episode Statistics data characterising the prevalence of iron deficiency and/or iron deficiency anaemia in all 78 805 adults admitted to hospitals across England with a primary diagnosis of heart failure across a single calendar year. Overall, 91% of these patients required an unplanned hospital admission due to an acute heart failure syndrome.
We describe the demographics typical of this comorbid population, and the associated outcomes with respect to mortality, readmission rates, length of stay and costs.
How might this impact on clinical practice?
This study addresses knowledge gaps relating to the prevalence and impact of iron deficiency with or without anaemia in acute heart failure patients. As this data emanated from people presenting with a common ambulatory care sensitive condition, and treated by clinicians imbued with a range of clinical expertise working in the real-world clinical milieu, this information is germane to routine practice, and generalisable to similar populations and organisational models.
Introduction
Heart failure, iron deficiency and anaemia
It is estimated about 900 000 people are living with heart failure (HF) in the UK, this burdensome life-limiting syndrome arising from diverse aetiological cardiovascular conditions leading to systolic and diastolic ventricular dysfunction.1 Iron, an essential micronutrient, is fundamental to many metabolic pathways, including the high energy biochemical reactions required of cardiac and skeletal muscle. In recent years iron deficiency (ID) has been increasingly recognised in those with HF. Associated with negative outcomes in reduced quality of life, impaired functional capacity and a poor prognosis, this has emerged as a meaningful therapeutic target.2 3
The complex pathophysiology remains incompletely understood, but potential mechanisms of ID or iron deficiency anaemia (IDA) in HF include nutritional iron or vitamin deficiencies, and bone marrow hypoperfusion or dysfunction. ID may also stem from occult or overt blood loss, sometimes linked to anti-platelet or anticoagulant medication, or through the effects of guideline-directed HF therapies. Angiotensin-converting-enzyme inhibitors, angiotensin-receptor-blockers, and some β-blockers such as carvedilol may inhibit erythropoiesis.4 5 In contrast, the mineralocorticoid receptor antagonist spironolactone may be beneficial in down-regulating hepcidin, a key modulator of iron homeostasis.6
While the above drugs are predominantly used for HF with a reduced ejection fraction (HFrEF), all HF subtypes as described in the European Society of Cardiology (ESC) guidelines exhibit this significant comorbidity.7 A prevalence of 53% for ID was noted in a single-centre study of 1197 chronic HF patients, this diagnosed in 50%, 61% and 64% of those characterised with HFrEF, a mid-range EF (HFmrEF), and a preserved EF (HFpEF), respectively.8
Clinical setting
Despite the demonstrable adverse effects, policies on systematic screening and subsequent treatment of HF patients with ID or IDA remain inconsistent. Guidelines issued by the National Institute for Health and Care Excellence constitute the standards for treating HF for residents in England. In their latest guidance (NG106) of September 2018, pending the results of ongoing clinical trials, concern was expressed about the cost effectiveness of comprehensively assessing all HF patients beyond those with anaemia or HFrEF, and the awareness of non-specialists to consider and test for ID was questioned.9
The course of HF is unique to each individual. However those affected tend to progressively decline along a roller-coaster disease trajectory punctuated by increasingly frequent hospital admissions. These HF admissions afford the opportunity to assess the frequency and impact of ID, but such data for England are lacking. Thus, we undertook a retrospective cohort study to evaluate the prevalence, clinical significance, and healthcare costs associated with the concurrent diagnoses of ID or IDA in people admitted to hospitals across England with a primary diagnosis of HF, their care often supervised by general physicians.
Methods
Data sources
This study is based on Hospital Episode Statistics Admitted Patient Care (HES APC) data. The HES data warehouse, curated by the National Health Service (NHS) Information Centre for Health and Social Care, collates information on clinical activity relating to all NHS hospitals in England.10 For inpatients, as well as admission and discharge dates, this comprehensive data set includes individual patient-level demographics and clinical information such as age, gender and ethnicity, place of residence, diagnoses and any relevant diagnostic, medical or surgical procedures. HES data are pseudoanonymised, manifest in the generation of a bespoke set of 32 alphanumeric characters by the application of a three-pass algorithm to a cluster of patient-specific information fields. This PSEUDO-HESID prevents individual patient identification but provides data useful to national government bodies and regulators, including NHS England and the Department of Health. Data are also made available to researchers. For this study, aggregated HES APC data were accessed through a licenced commercial organisation, Harvey Walsh Ltd, reused with permission of NHS Digital (copyright 2019, all rights reserved).
Diagnostic attribution and coding
The HES APC data set incorporates post-discharge diagnostic coding as designated by health informatics professionals trained to national standards, with oversight by local hospital clinicians, the degree of such supervision varying both within and between institutions. There is no other national data set against which to compare diagnostic coding accuracy, but as HES coding is the basis of reimbursement and benchmarking of healthcare organisations, this has driven improved accuracy and depth of coding in recent years. Until April 2017, HES coding was subject to centralised national external audit, thereafter, this responsibility has been assumed by locality-based NHS provider trusts and Clinical Commissioning Groups.
A systematic review of discharge coding accuracy suggests this is robust and applicable to research activity.11 Coding precision pertains particularly to the primary admission diagnosis, especially for conditions such as HF where the clinical features are relatively stereotyped, and there are supportive confirmatory tests such as natriuretic peptide assays and echocardiography. A recent audit comparing the concordance of clinicians’ and coders’ diagnoses reported a coding error rate of only 1.8% for those admitted with acute HF, this estimated at 10.5% across a range of secondary diagnoses.12 Documentation and information transfer relating to comorbidities tends to be more ambiguous, and specific evidence relating to the coding accuracy for ID or IDA is currently unavailable.
For the present study, codes utilised to define HF, ID or IDA were from the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10).13 There are 71 ICD-10 codes specifying the clinical spectrum of anaemia. Clinical coders cannot assume the patient has ID or IDA unless so documented in the clinical record by the responsible clinician, and they are not permitted to independently interpret test results of any kind. As defined in the national clinical coding standards,14 ‘iron deficiency’ is an Essential Modifier which requires that IDA must be extant in the clinical record for the applicable codes to be assigned. If IDA is not formally recorded in a form interpretable by coders, the coding rules stipulate that the diagnosis must be coded as D649: anaemia, unspecified. For this study, the ICD-10 codes used to differentiate HF patients with or without ID or IDA are listed in table 1. Consistent with the coding convention described above, we also included ICD-10 code D649 within the IDA coding envelope, anticipating that a proportion of HF patients with IDA would be assigned that diagnostic code given the expected variation in documentation and resultant coding practice.
Table 1.
ICD-10 codes used to identify patients with HF with or without ID/IDA
| HF codes (primary diagnosis) | ID/IDA codes (secondary diagnoses) |
| I11.0 (hypertensive heart disease with (congestive) heart failure) I25.5 (ischaemic cardiomyopathy) I42.0 (dilated cardiomyopathy) I42.9 (cardiomyopathy, unspecified) I50.0 (congestive heart failure) I50.1 (left ventricular failure) I50.9 (heart failure, unspecified) |
D500 (IDA secondary to blood loss (chronic)) D508 (other IDA) D509 (IDA unspecified) D649 (anaemia unspecified) |
HF, heart failure; ICD-10, 10th revision of the International Statistical Classification of Diseases and Related Health Problems; ID, iron deficiency; IDA, iron deficiency anaemia.
Study population
Iron deficiency was highlighted in the updated ESC HF guidelines of June 2016.2 Aware that this publication might engender transient changes in clinical practice and introduce random error, we elected to assess HES data for the financial year April 2015 through March 2016. This evaluation relates to all adult men and women admitted over that period for whom HF was coded as the primary discharge diagnosis, with possible recording of ID or IDA in any of 19 subsidiary diagnostic coding positions.
Mindful that in a higher proportion of younger people, HF would stem from cyanotic congenital heart disease with secondary polycythaemia, a distinctive disruption of iron homeostasis which might disproportionately confound assessment of ID or IDA compared with the general HF population, we chose to define adulthood as 21 years. In accepting this compromise, data on only 41 patients aged 18 to 20 years admitted over the above period were excluded from study evaluation.
Analyses
In HES data, a hospital admission is classified as a ‘spell’, defined as a period of continuous inpatient care on the premises of a single healthcare provider. Transfer to another hospital for further care or rehabilitation would start a new spell, and linking consecutive inpatient spells would constitute a ‘superspell’. Markers of sequential inpatient spells are not routinely logged on HES data.15 Therefore, for the purpose of this study, we elected to undertake evaluation of the HES APC data extract relating to the first hospital spell.
The following analyses were undertaken for the year specified: total number of HF admissions; patients’ gender and age; type of admission – emergency (non-elective), elective, or day case; ≤30 days unplanned readmission rate under the same HF-related primary diagnostic ICD-10 code; ≤30 days all-cause unplanned readmission rate; length of stay (LOS) of the initial hospital spell; inhospital mortality rate. We compared direct costs associated with these HF admissions for patients with and without secondary coded diagnoses of ID or IDA based on the NHS National Tariff Payment System for the 2015 to 2016 financial year.
Statistical methods
X2 testing was used to examine the independence of categorical variables linked to HF admissions. For continuous variables, the independent t-test was utilised to assess whether differences between group means achieved statistical significance. Significance was accepted at the p<0.05 level. Descriptive statistics are provided throughout.
Results
Between April 2015 through March 2016, 78 805 adults with a primary diagnosis of HF were admitted to 177 NHS acute provider hospitals throughout England. Of these, 26 530 (33.7%) had a documented secondary diagnosis of ID or IDA, while 52 275 (66.3%) did not (table 2). For these HF patients, 12 690 were coded as exhibiting ID and 6840 coded IDA as single diagnostic categories. Coding for both ID and IDA was evident in 7000 patients. To avoid double counting, we excluded one of these duplicated records from analysis. Given the extent of joint coding for ID and IDA (26.3%), and without specific information on the laboratory tests differentiating between these diagnostic subgroups, we chose to pool data relating to those coded for either ID, IDA or these in combination, as a single clinical descriptor (ID/IDA) with respect to subsequent analyses.
Table 2.
Hospital admissions with a primary diagnosis of heart failure in England in 2015/2016
| N | Age range | Overall | Emergency (non-elective) |
Elective | Day cases | ||||
| Patients | Spells | Patients* | Spells | Patients* | Spells | Patients* | Spells | ||
| With secondary ID/IDA | ≥21 years | 26 530 | 33 711 | 25 160 | 30 584 | 1063 | 1146 | 991 | 1981 |
| ≥75 years | 19 312 | 23 918 | 18 654 | 22 291 | 542 | 573 | 434 | 1054 | |
| Without secondary ID/IDA | ≥21 years | 52 275 | 62 064 | 45 784 | 52 478 | 3581 | 3789 | 4492 | 5797 |
| ≥75 years | 33 402 | 38 747 | 31 287 | 35 475 | 1365 | 1438 | 1328 | 1834 | |
*Patients could be counted in more than one column for emergency, elective and day case admissions if they required more than one type of admission during the period analysed.
ID, iron deficiency; IDA, iron deficiency anaemia.
Demographics
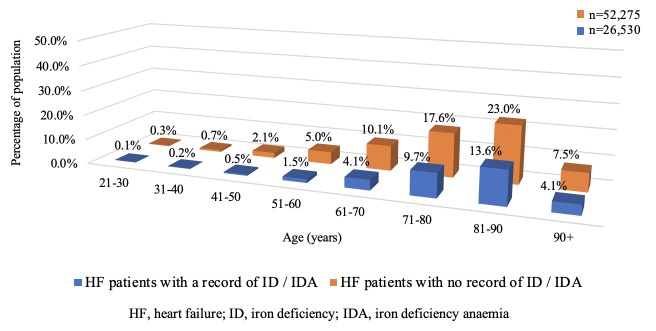
The majority of HF patients coded with ID/IDA were female compared with those without this secondary coding (50.2% vs 45.0%, respectively; p<0.0001). Mean age also differed significantly between the two groups: 79.1 years (range: 21 to 105) versus 76.6 years (range: 21 to 106) for those with and without a secondary diagnosis of ID/IDA, respectively (p<0.0001). The distribution of patient ages for each group is shown in figure 1.
Figure 1.
Distribution of ages in HF patients with and without a secondary diagnosis of ID/IDA.
Classification of admissions
For all of these HF admissions, 91.2% were classified as emergency, the remainder being categorised as elective for diagnostic investigation or to facilitate provision of treatment elements consistent with contemporary HF therapy. Among HF patients exhibiting secondary ID/IDA coding, 94.8% (n=25 160/26 530) had emergency admissions compared with 87.6% for those without this designation (n=45 784/52 275; p<0.0001).
Readmission rates
Heart failure patients with a secondary diagnosis of ID/IDA had both higher ≤30 day HF-related and all-cause readmission rates compared with those without: 8.2% versus 5.2%, (difference: 3.0% (95% CI: 2.64 to 3.40); p<0.0001), and 25.8% versus 17.7%, (difference: 8.1% (95% CI: 7.49 to 8.73); p<0.05), respectively. Table 3 shows admission data for the whole study cohort, and also the results of a subanalysis for patients aged ≥75 years at the time of initial admission.
Table 3.
Summary of heart failure admission data
| Analysis | All HF patients aged ≥21 years n=78 805 | All HF patients aged ≥75 years n=52 714 | ||||||
| With ID/IDA | Without ID/IDA | RR (95% CI) |
P value | With ID/IDA | Without ID/IDA | RR (95% CI) |
P value | |
| Proportion with emergency admissions | 94.8% | 87.6% | 1.08 (1.07 to 1.09) |
p<0.0001 | 96.6% | 93.7% | 1.03 (1.02 to 1.04) |
p<0.0001 |
| Heart failure readmission rate ≤30 days* | 8.2% | 5.2% | 1.59 (1.50 to 1.68) |
p<0.0001 | 7.7% | 5.5% | 1.47 (1.41 to 1.54) |
p<0.0001 |
| All-cause readmission rate ≤30 days | 25.8% | 17.7% | 1.46 (1.42 to 1.50) |
p<0.05 | 25.3% | 18.7% | 1.35 (1.31 to 1.40) |
p<0.05 |
*Under the same ICD-10 HF code.13
HF, heart failure; ICD-10, 10th revision of the International Statistical Classification of Diseases and Related Health Problems; ID, iron deficiency; IDA, iron deficiency anaemia; RR, Relative risk.
Length of stay and costs
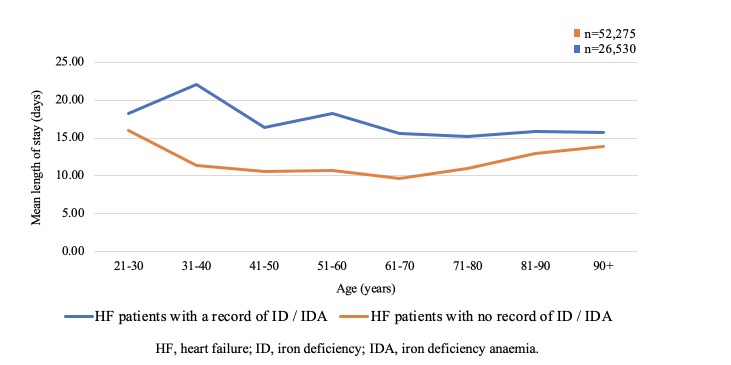
For emergency admissions, the mean LOS was longer for patients with a supplementary diagnosis of ID/IDA compared with those without (15.8 vs 12.2 days). The inter-group difference of 3.6 days was statistically significant (95% CI: 3.32 to 3.80; p<0.0001). The difference in mean LOS between HF patients with and without ID/IDA was maintained across all age groups (figure 2). For the 30 584 emergency hospital spells recorded for HF patients with a secondary diagnosis of ID/IDA, this equates to an additional 108 946 bed-days.
Figure 2.
Length of stay and age for HF patients with and without a secondary diagnosis of ID/IDA.
The mean estimated cost associated with emergency hospital admissions was higher among HF patients with secondary diagnostic coding of ID/IDA compared with those without (£3623 vs £2918, respectively) which equates to a per capita excess of £705 for patients so described (95% CI: £662 to £748; p<0.0001). This additional expenditure summates to £21.5 million across the English health economy for HF patients admitted with this secondary coding during the 2015 to 2016 financial year.
Correction for age showed that this was not a significant covariate in relation to the classification of admissions, readmission rates, LOS or cost. Our analyses are based on aggregated data, therefore it is not possible to provide sex-standardised results with respect to these metrics.
Mortality
There was a small but statistically significant greater inhospital mortality rate for HF patients with ID/IDA versus those without, 13.5% (n=3592) and 12.9% (n=6730), respectively (95% CI: 0.16 to 1.17; relative risk 1.05 (95% CI: 1.01 to 1.09); p=0.009). Importantly, while this observation is based on documentation of patients having died in hospital, the cause of death is not defined within the HES data set, and we had no access to the applicable Office for National Statistics death registration data. Therefore, it cannot be concluded, nor should it be assumed, that these deaths were specifically attributable to the primary admission diagnosis of HF.
Comorbidities
Acute kidney injury or chronic kidney disease (CKD) are common comorbidities in HF patients. We compared the relative distribution of CKD in HF patients exhibiting ID/IDA or no ID/IDA based on any additional ICD-10 diagnostic coding as N183 (Stage 3 CKD; estimated glomerular filtration rate 30 to 49 mL/min/1.73 m2). There was a significant association between ID/IDA coding and coding for CKD, 12.6% (n=3349), against 8.3% (n=4354) for the non-ID/IDA group (95% CI: 3.8 to 4.8; p<0.002).
While ID in HF patients has been linked to gastrointestinal malignancy,16 for this study population there were no discernible differences between the ID/IDA and non-ID/IDA groups with respect to the relative frequency of coding for these diagnoses or other conditions associated with blood loss such as peptic ulcer disease in the index HF admission, or for any subsequent admission over a 90-day period thereafter.
Discussion
The results of our analyses derive from HES data characterising all adults admitted with a primary diagnosis of HF to every NHS provider hospital in England over the specified period. We note that the mean age of this unselected real-world clinical cohort is typical of those admitted with HF in the UK.1 People with a secondary diagnosis of ID/IDA were significantly older and more commonly female, and a relative preponderance of female HF patients exhibiting ID or IDA has been previously described.17 18
We noted that HF admissions coded with a secondary diagnosis of ID/IDA were longer and more expensive than those without such diagnoses, these associations persisting across the age range. Comparable to our data, Caughey and colleagues found that for 6291 HF patients hospitalised in the USA, the presence of anaemia, defined by the WHO as a haemoglobin <13 g/L for men and <12 g/L for women, disproportionately increased LOS by 3.5 days for those with HFpEF, who also tended to be older and female, against 1.8 days for their counterparts with HFrEF.19 20
Patients with ID/IDA appeared to be at higher risk of early readmission, and the inhospital mortality rate was greater at 13.5% for HF patients with these secondary codes compared with 12.9% for those without. These mortality rates are similar to those documented at 13.3% and 12.6% for HF patients treated on elderly care wards or without specialist HF input, respectively, as reported in the relevant iteration of the National Heart Failure Audit (NHFA) for England and Wales, which included 82% of all HF patients admitted in England during this study period.21 For that audit cycle, only 46% of patients were admitted to cardiology wards, the majority being treated on non-specialist wards. Of data submitted to the 2015/2016 NHFA, 68.3% were characterised as pertaining to patients with HFrEF. HF subtypes are not differentiated in the HES database, and at present, data on ID or IDA are not logged on the NHFA system. However, the recently established linkage of information archived in these national data repositories, intended to facilitate a more in-depth study of the acute HF population (NCT03733665 (ClinicalTrials.gov identifier)), might provide the opportunity for triangulation.
While 33.7% of these hospital admissions with a primary diagnostic coding of HF included ID/IDA in a subsidiary coding position, this figure is less than the approximately 50% previously reported for HF patients.2 8 22 23 However, most studies describing this association have involved ambulant patients with chronic HF. By contrast, the vast majority of those constituting the basis of this study required emergency admission, inferring they exhibited de novo acute HF or acute decompensation of chronic HF. To date there is a relative paucity of data relating to ID or IDA in patients presenting with these clinical scenarios, and accepted measures of assessment might be compromised by the pathophysiological responses intrinsic to the acute HF state.24
HF patients may exhibit absolute or functional ID, the former reflecting depleted iron stores. With functional ID, iron stores are replete, but stored iron trafficking is suppressed and too ineffectual to drive normal erythropoiesis or maintain cellular metabolic function.3 Under normal physiological conditions, serum ferritin correlates well with body iron stores, hence, is used as a proxy measure of iron status. By convention, but largely based on assessing those with chronic HF, a serum ferritin <100 ng/mL has been adopted as the cut point defining absolute ID. Similarly, functional ID in HF is delineated as a serum ferritin of 100 to 299 ng/mL with a transferrin saturation (TSAT) <20%.7 However, ferritin reacts as an acute phase protein and increases in response to inflammation and oxidative stress.17 Conversely, transferrin is a negative acute phase reactant, and may be suppressed under these conditions.25 Thus dilemmas exist in the diagnosis of ID in the acute HF setting.
Jankowska and colleagues found that only 34% of 165 patients presenting with acute HF fulfilled the diagnostic criteria for ID based on the ferritin and TSAT levels described above.26 This group compared those results with other potentially more robust tests of ID, these defined as a low serum hepcidin (<14.5 ng/mL), reflecting depleted iron stores, and an elevated soluble transferrin receptor (sTfR, 1.59 mg/L), a marker of reduced cytosolic iron less sensitive to inflammation driven perturbation. An isolated low hepcidin or elevated sTfR were evident in 9% and 29%, respectively, of these patients, whereas 37% exhibited both laboratory features. While their reported prevalence of ID is similar to that seen in our much larger population, a French group also examined ID and inflammatory biomarkers in a relatively small acute HF cohort.27 Serum hepcidin and sTfR levels were available for 41 patients. Based on the diagnostic criteria for these parameters outlined above, 34 (83%) exhibited ID on admission, with a trend towards increasing hepcidin and reducing sTfR levels by day 30. There was a weak correlation between changes in ferritin and TSAT status against sequentially assessed activity of a range of inflammatory markers, not evident for hepcidin and sTfR. These observations confirm the dynamic nature of conventionally perceived iron status and inflammatory responses which flux through the early phase and resolution of acute HF.
Once ID is diagnosed in those with HF, treatment needs to be considered. As demonstrated in the IRONOUT HF study, oral iron supplementation is seemingly ineffective.28 Alternatively, the use of intravenous (IV) iron therapy appears to be beneficial.29 30 Both the ESC and US guidelines propose that this treatment should be offered in symptomatic patients with HFrEF and ID,7 31 these recommendations based primarily on two major studies examining the effects of IV ferric carboxymaltose in chronic HFrEF patients, the FAIR-HF and CONFIRM-HF trials.29 32
The efficacy and safety of IV iron for those with acute HF and ID are still uncertain, but two studies in progress may provide clarification. Akin to the clinical population analysed in this study, the multinational AFFIRM-AHF study (NCT02937454) will assess a composite endpoint of HF rehospitalisation and cardiovascular death in 1100 HFrEF patients (EF <50%) with acute HF and ID, treated with IV ferric carboxymaltose. In the UK, the IRONMAN study (NCT02642562) will compare cardiovascular mortality in 1300 HFrEF patients (EF <45%) and ID treated with IV iron, as isomaltoside 1000, against placebo. Eligibility criteria include acute HF inpatients <48 hours before discharge, or those within 6 months of a previous HF admission.
ID may be particularly important in those with HFpEF.33 The FAIR-HFpEF study (NTC03074591) is underway to assess responses to IV ferric carboxymaltose in ambulatory HFpEF patients (EF ≥45%) with ID, some patients recruited within 12 months of hospitalisation.
Study strengths and limitations
The main strength of our study is that our analyses are based on data arising from everyday practice, collated for almost 80 000 adult patients, admitted with HF to 177 different hospital sites over a single calendar year and constituting all such clinical activity across England over that period. This appears to be the first study to systematically evaluate HES data relating to ID/IDA in this clinical population, and to determine outcomes related to these comorbidities.
However, given the complexity of the typically multimorbid HF population, we cannot presume a causal relationship for ID or IDA and the disparities we have described between the patient groups with and without these documented diagnoses. It is possible that such haematology features are to some extent surrogate markers of those with greater activation of the renin-angiotensin-aldosterone system and increased levels of proinflammatory cytokines, and likely therefore to have a more complicated clinical course.
There are some potential limitations to our study. Although HES coding is considered relatively accurate,11 we acknowledge that the quality of data subject to analysis was dependent on the expertise of local clinicians in diagnosing HF and ID/IDA with subsequent correct coding for these conditions, over which we have no means of adjudication. We have no information on how comprehensively this admitted HF cohort was screened for these comorbidities, which laboratory tests were employed and their timing in those subject to investigation, or whether these conditions were pre-existing or newly diagnosed. It is likely that a range of laboratory test abnormalities will have been evident in those investigated, reflecting nuanced differences in their individual health status, but to some extent ID and IDA also represent a clinical continuum, and in the absence of specific information on laboratory data, and given that >26% of patients were coded for both ID and IDA, we felt that amalgamating this patient data under a single descriptor as ‘ID/IDA’ was a realistic approach. Similarly, incorporating HES coding as D649 (anaemia, unspecified), may be regarded as a confounder, but we have explained our rationale above, and our results suggest that no ensuing excess diagnosis of ID/IDA emerged compared with previous studies. Finally we have no knowledge of the nature or effectiveness of any relevant therapy provided to these HF inpatients to determine whether or not this might have affected the observed study metrics or outcomes. This paper has been written on the assumptions of the best available data and a reasonable degree of appropriate clinical practice.
Conclusion
Based on analyses of the nationally accredited HES database, we have demonstrated that, for the calendar year April 2015 through March 2016, ID or IDA appeared to be relatively common comorbidities, impacting a significant proportion of an unselected clinical cohort representing all adults admitted to hospitals in England with HF, of whom more than 90% exhibited an acute HF syndrome. The results of this study emanate from the real-world clinical milieu, beyond the bounds of clinical trials, and as illustrated in the contemporaneous data from the NHFA, many patients would have been treated by non-specialists who ascertained and documented these accompanying conditions. As evidence accrues to address other knowledge gaps regarding the accuracy of diagnostic testing and effective therapy for ID or IDA across the spectrum of acute and chronic HF, including the refinement of iron repletion protocols and the emergence of other novel treatment modalities, it is incumbent on us as clinicians to ensure robust screening strategies and treatment regimens are in place, consistent with evolving national and international guidelines.34This may improve outcomes for affected individuals and decrease the financial burden on health economies.
Footnotes
Contributors: All authors (JMB, RK, CJP, SGW) were involved in the conception and design of the study, and interpretation of the results. All authors had access to all of the study data and can take responsibility for data integrity and the accuracy of analyses. CJP conducted the statistical analysis. JMB undertook primary drafting of the paper and all authors contributed to significant redrafting. JMB is the guarantor of the paper.
Funding: Vifor Pharma UK Ltd funded unrestricted access to the HES data through Harvey Walsh Ltd.
Competing interests: All authors have previously received consultancy fees from Vifor. JMB has also received meeting support and honoraria from Vifor. RK has received additional fees and educational grants from Novartis. All authors declare no conflict of interest in terms of this study and have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: There are no additional data relevant to this paper.
References
- 1.Conrad N, Judge A, Tran J, et al. Temporal trends and patterns in heart failure incidence: a population-based study of 4 million individuals. Lancet 2018;391:572–80. 10.1016/S0140-6736(17)32520-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Klip IT, Comin-Colet J, Voors AA, et al. Iron deficiency in chronic heart failure: an international pooled analysis. Am Heart J 2013;165:575–82. 10.1016/j.ahj.2013.01.017 [DOI] [PubMed] [Google Scholar]
- 3.McDonagh T, Macdougall IC. Iron therapy for the treatment of iron deficiency in chronic heart failure: intravenous or oral? Eur J Heart Fail 2015;17:248–62. 10.1002/ejhf.236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cheungpasitporn W, Thongprayoon C, Chiasakul T, et al. Renin-angiotensin system inhibitors linked to anemia: a systematic review and meta-analysis. QJM 2015;108:879–84. 10.1093/qjmed/hcv049 [DOI] [PubMed] [Google Scholar]
- 5.Komajda M, Anker SD, Charlesworth A, et al. The impact of new onset anaemia on morbidity and mortality in chronic heart failure: results from comet. Eur Heart J 2006;27:1440–6. 10.1093/eurheartj/ehl012 [DOI] [PubMed] [Google Scholar]
- 6.Mleczko-Sanecka K, da Silva AR, Call D, et al. Imatinib and spironolactone suppress hepcidin expression. Haematologica 2017;102:1173–84. 10.3324/haematol.2016.162917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 2016;37:2129–200. 10.1093/eurheartj/ehw128 [DOI] [PubMed] [Google Scholar]
- 8.Martens P, Nijst P, Verbrugge FH, et al. Impact of iron deficiency on exercise capacity and outcome in heart failure with reduced, mid-range and preserved ejection fraction. Acta Cardiol 2018;73:1–9. 10.1080/00015385.2017.1351239 [DOI] [PubMed] [Google Scholar]
- 9.National Institute for Health and Care Excellence NG106. chronic heart failure in adults: diagnosis and management, 2018. Available: http://www.nice.org.uk/guidance/NG106 [Accessed 21 May 2019]. [PubMed]
- 10.NHS Digital Hospital Episode Statistics [Internet]. NHS Digital, 1 Trevelyan Square, Boar Lane, Leeds, LS1 6AE, UK. Available: http://content.digital.nhs.uk/hes [Accessed 12 Nov 2019].
- 11.Burns EM, Rigby E, Mamidanna R, et al. Systematic review of discharge coding accuracy. J Public Health 2012;34:138–48. 10.1093/pubmed/fdr054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nouraei SAR, Virk JS, Hudovsky A, et al. Accuracy of clinician-clinical coder information handover following acute medical admissions: implication for using administrative datasets in clinical outcomes management. J Public Health 2016;38:352–62. 10.1093/pubmed/fdv041 [DOI] [PubMed] [Google Scholar]
- 13.ICD 10 International statistical classification of diseases and related health problems. 10th revision. 2nd edition Geneva: World Health Organisation, 2010. [Google Scholar]
- 14.Health and Social Care Information Centre, “National ICD-10 Clinical Coding Standards”, NHS Delen website. Published 2019https://hscic.kahootz.com/gf2.ti/f/762498/46448165.2/PDF/-/National_Coding_Standards_ICD10_reference_book_2019.pdf (accessed 7 Dec 2019). [Google Scholar]
- 15.Herbert A, Wijlaars L, Zylbersztejn A, et al. Data resource profile: Hospital episode statistics admitted patient care (hES APC). Int J Epidemiol 2017;46:1093–1093i. 10.1093/ije/dyx015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Martens P, Minten L, Dupont M, et al. Prevalence of underlying gastrointestinal malignancies in iron-deficient heart failure. ESC Heart Fail 2019;6:37–44. 10.1002/ehf2.12379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fitzsimons S, Doughty RN. Iron deficiency in patients with heart failure. Eur Heart J Cardiovasc Pharmacother 2015;1:58–64. 10.1093/ehjcvp/pvu016 [DOI] [PubMed] [Google Scholar]
- 18.van Veldhuisen DJ, Anker SD, Ponikowski P, et al. Anemia and iron deficiency in heart failure: mechanisms and therapeutic approaches. Nat Rev Cardiol 2011;8:485–93. 10.1038/nrcardio.2011.77 [DOI] [PubMed] [Google Scholar]
- 19.UNICEF, UNU WHO. Iron deficiency anaemia: assessment, prevention, and control. WHO/NHD/01.3. Geneva, Switzerland: World Health Organization, 2001. [Google Scholar]
- 20.Caughey MC, Avery CL, Ni H, et al. Outcomes of patients with anemia and acute decompensated heart failure with preserved versus reduced ejection fraction (from the ARIC study community surveillance). Am J Cardiol 2014;114:1850–4. 10.1016/j.amjcard.2014.09.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Healthcare Quality Improvement Partnership National heart failure audit report April 2015-March 2016, 2017. Available: https://www.hqip.org.uk/resource/national-heart-failure-audit-2015-2016/#.W0XRMC2ZOu4 [Accessed 20 June 2019].
- 22.Wienbergen H, Pfister O, Hochadel M, et al. Usefulness of Iron Deficiency Correction in Management of Patients With Heart Failure [from the Registry Analysis of Iron Deficiency-Heart Failure (RAID-HF) Registry]. Am J Cardiol 2016;118:1875–80. 10.1016/j.amjcard.2016.08.081 [DOI] [PubMed] [Google Scholar]
- 23.von Haehling S, Gremmler U, Krumm M, et al. Prevalence and clinical impact of iron deficiency and anaemia among outpatients with chronic heart failure: the PreP registry. Clin Res Cardiol 2017;106:436–43. 10.1007/s00392-016-1073-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jankowska EA, von Haehling S, Anker SD, et al. Iron deficiency and heart failure: diagnostic dilemmas and therapeutic perspectives. Eur Heart J 2013;34:816–29. 10.1093/eurheartj/ehs224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ritchie RF, Palomaki GE, Neveux LM, et al. Reference distributions for the negative acute-phase serum proteins, albumin, transferrin and transthyretin: a practical, simple and clinically relevant approach in a large cohort. J Clin Lab Anal 1999;13:273–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jankowska EA, Kasztura M, Sokolski M, et al. Iron deficiency defined as depleted iron stores accompanied by unmet cellular iron requirements identifies patients at the highest risk of death after an episode of acute heart failure. Eur Heart J 2014;35:2468–76. 10.1093/eurheartj/ehu235 [DOI] [PubMed] [Google Scholar]
- 27.Van Aelst LNL, Abraham M, Sadoune M, et al. Iron status and inflammatory biomarkers in patients with acutely decompensated heart failure: early in-hospital phase and 30-day follow-up. Eur J Heart Fail 2017;19:1075–6. 10.1002/ejhf.837 [DOI] [PubMed] [Google Scholar]
- 28.Lewis GD, Malhotra R, Hernandez AF, et al. Effect of oral iron repletion on exercise capacity in patients with heart failure with reduced ejection fraction and iron deficiency: the IRONOUT HF randomized clinical trial. JAMA 2017;317:1958–66. 10.1001/jama.2017.5427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ponikowski P, van Veldhuisen DJ, Comin-Colet J, et al. Beneficial effects of long-term intravenous iron therapy with ferric carboxymaltose in patients with symptomatic heart failure and iron deficiency†. Eur Heart J 2015;36:657–68. 10.1093/eurheartj/ehu385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jankowska EA, Tkaczyszyn M, Suchocki T, et al. Effects of intravenous iron therapy in iron-deficient patients with systolic heart failure: a meta-analysis of randomized controlled trials. Eur J Heart Fail 2016;18:786–95. 10.1002/ejhf.473 [DOI] [PubMed] [Google Scholar]
- 31.Yancy CW, Jessup M, Bozkurt B, et al. ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American heart association Task force on clinical practice guidelines and the heart failure Society of America. J Am Coll Cardiol 2017;2017:776–803. 10.1016/j.jacc.2017.04.025 [DOI] [PubMed] [Google Scholar]
- 32.Anker SD, Comin Colet J, Filippatos G, et al. FAIR-HF trial Investigators. ferric carboxymaltose in patients with heart failure and iron deficiency. N Engl J Med 2009;361:2436–48. 10.1056/NEJMoa0908355 [DOI] [PubMed] [Google Scholar]
- 33.Beale AL, Warren JL, Roberts N, et al. Iron deficiency in heart failure with preserved ejection fraction: a systematic review and meta-analysis. Open Heart 2019;6:e001012 10.1136/openhrt-2019-001012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Anand IS, Gupta P. Anemia and iron deficiency in heart failure: current concepts and emerging therapies. Circulation 2018;138:80–98. 10.1161/CIRCULATIONAHA.118.030099 [DOI] [PubMed] [Google Scholar]