Abstract
Background
The concurrence of sleep and socio-emotional development in children is well accepted. However, the predictive role of sleep problems in infancy and the development of emotional and behavioural problems later in childhood remain still unclear. Therefore, in this study we examined the associations between sleep problems in early childhood and internalising, externalising and dysregulation symptoms in toddlers.
Methods
1679 families entered the study during pregnancy and 936 children participated at 24 months. Parent-reported sleep duration, sleep-onset latency, night wakings, proportion of daytime sleep and bedtime at 3, 8, 18 and 24 months were assessed with two sleep questionnaires. Externalising, internalising and dysregulation problems at 24 months were examined with the Brief Infant-Toddler Social and Emotional Assessment.
Results
Short sleep duration at 3 and 8 months, more night wakings at 3, 8, 18 and 24 months and greater proportion of daytime sleep at 24 months were associated with internalising symptoms. Shorter sleep duration at 8, 18 and 24 months and longer sleep-onset latency and more night wakings at all time points, in addition to earlier bedtime at 8 months and greater proportion of daytime sleep at 24 months, were related to dysregulation. Finally, more night wakings at 3 and 24 months, and longer sleep-onset latency at 24 months were associated with externalising problems.
Conclusion
Shorter sleep and poorer sleep quality in infancy were prospectively related to emotional and behavioural symptoms in toddlers, and these associations were strongest for internalising and dysregulation symptoms. This study contributes to the recent research on the role of early sleep problems in socio-emotional development, suggesting that shorter sleep duration, longer sleep-onset latency and higher waking frequency are related to internalising, externalising and dysregulation symptoms in toddlers, and thus it might be beneficial to provide early interventions for those infants reporting these sleep problems.
Keywords: sleep, epidemiology, child psychiatry, data collection, neurodevelopment
What is known about the subject?
Sleep problems are highly prevalent in early childhood.
Sleep problems are concurrently associated with behavioural difficulties in childhood.
The significance of sleep problems in infancy and emotional and behavioural problems in later childhood is still unclear.
What this study adds?
Night wakings at 3 months are prospectively related to internalising and externalising symptoms in toddlers.
Shorter sleep, longer sleep-onset latency and night wakings in early childhood are closely related to dysregulation in toddlers.
Introduction
Sleep problems such as frequent night waking, sleep-onset difficulties or behavioural insomnia are highly prevalent in childhood1 and are clearly associated with daytime behavioural difficulties such as problems in socio-emotional development.2 More specifically, social‐emotional problems in childhood include disruptive behaviour, lack of inhibition of impulse control, aggression, defiance, over‐activity, negative emotionality and/or anxiety.3 Despite the coexistence of sleep difficulties with emotional and behavioural problems being well accepted,4 it remains unclear whether sleep problems in infancy and early childhood are associated with emotional or behavioural symptoms later in childhood. Moreover, the specific role of each of the early sleep problems (ie, circadian rhythm problems, lack of sleep, or sleep-onset problems or sleep fragmentation) for the development of emotional and behavioural problems has not been well characterised.
Previous longitudinal studies are scarce, but the few existing studies report that short sleep duration or dyssomnia symptoms, like night sleep fragmentation during the first year of life, are associated with increased risk for internalising problems (ie, anxiety and fears) in 3–4 years old children.5 6 Another recent study showed that short sleep duration and frequent nocturnal wakings at 18 months predicted concurrent and later incidence of internalising and externalising symptoms (ie, aggressive and oppositional behaviours) at 5 years.7 Moreover, one recent study using a relatively small sample of infants (n=117) found that shorter sleep and later bedtimes at 12 months predicted higher levels of internalising problems at 18 months, but not externalising or dysregulation symptoms (ie, the inability to control one's behaviour, emotions and thoughts).8 Finally, a previous longitudinal research study in older children suggests that sleep problems may have a persistent negative impact on self-regulation, which, in turn, contributes to ongoing sleep problems and poorer attentional regulation in children over time.9 Self-regulation develops rapidly in the first years of life10 and difficulties in self-regulation are related to difficulties in psychosocial development such as externalising problems.11 More studies are required regarding sleep quality and dysregulation, especially in early stages of life, and how sleep predicts outcomes and, in turn, could help us understand potential mechanisms and discover new windows for intervention.
Despite previous studies providing some evidence on the existing links between sleep problems in 12–18-month-old toddlers and internalising and externalising symptoms in later stages,7 8 it is still unclear which sleep problems in infancy and early childhood are associated with psychiatric symptoms in toddlers. We hypothesised that the risk for negative consequences might depend on the timing or the type of the sleep difficulty. For example, sleep-onset problems and night wakings are highly prevalent in early childhood and they are considered normal in early infant development.12 13 However, they are clearly less common in 2-year-olds with 15%–30% experiencing regular difficulties with falling asleep (ie, bedtime problems) or with sleeping through the night (ie, night waking).14 Therefore, poor sleep quality might be more normative in infants and more pathological in childhood.
Our aim was to examine the associations of early sleep problems at 3, 8, 18 and 24 months with the development of internalising, externalising and dysregulation symptoms at 24 months in a large birth cohort of children. Addressing this knowledge gap provides information to parents and clinicians about whether some specific sleep problems across the first years of life are associated with subsequent emotional and behavioural problems, which, in turn, would aid recognising clinically significant sleeping problems. Parent-reported sleep problems comprised shorter sleep duration, worse sleep quality (ie, number of night wakings and sleep-onset latency) and circadian rhythm disturbances. As there are differences in social-emotional development between girls and boys among children aged 11–24 months, we also examined sex differences.15 We hypothesised that insomnia symptoms and shorter sleep duration in infants aged 3–24 months would be related to internalising and externalising symptoms, as well as to dysregulation in 2-year-old toddlers.
Methods
Participants
The study is based on the CHILD-SLEEP birth cohort, comprising all Finnish-speaking pregnant women who belonged to the area of the Tampere University Hospital, in the hospital district of Pirkanmaa, in southern Finland within the recruitment window (April 2011–January 2013). The recruitment took place during a routine visit to the maternity clinics in the 32nd week of pregnancy. Maternity care in Finland is accessible and free to everybody living in Finland and widely used (over 99.7% of women). The coverage in this study was about 29% of pregnant women in the area at the time of recruitment. The sample was representative concerning age and number of previous children, but participants in this study had somewhat higher educational level compared with the general level in the target area. Other details of the recruitment procedure have been reported previously.16 We used information regarding parental questionnaires during pregnancy, infants’ sleep at 3, 8, 18 and 24 months and emotional and behavioural symptoms at 24 months.
Initially, 1679 families returned the baseline questionnaire and 950 filled the 24-month questionnaire. We excluded all cases with parent-reported severe chronic illnesses or developmental disabilities, such as Down syndrome or Hirschsprung’s disease (n=10) and the co-twins (n=14), leaving 936 children for the analyses. Of these, 900 infants had data at 3 months, 893 at 8 months and 866 at 18 months. In the drop-out analysis, we found that mothers participating at 24 months were older than those who did not (F(1,1412)=14.766, p<0.001, η2=0.010), had higher educational levels (X2(2,1425)=22.811, p<0.001, φ=0.127) and lower levels of anxiety (F(1,1422)=10.015, p=0.002, η2=0.007) and depression (F(1,1421)=11.237, p=0.001; η2=0.008).
Written informed consent was obtained from all parents.
Measures
The parental forms included several questions on sociodemographic factors and health. Additional questions related to their child development were asked from the parents. Sleep in early childhood was measured by the Brief Infant Sleep Questionnaire (BISQ)17 and the Infant Sleep Questionnaire (ISQ),18 which are validated instruments and some of the most commonly used tools for screening sleep problems among infants and young children.
The BISQ was developed to characterise infant sleep quality with 13 items about duration of sleep, settling, night waking and sleep arrangements. We selected the following sleep variables: (i) total number of sleep hours; and (ii) bedtime. Furthermore, we created a measure of circadian rhythm development, which was operationalised as the proportion of daytime sleep per total sleep.
The ISQ is a 10-item questionnaire that assesses infant sleep habits and parental strategies for managing infant sleep. For this study, we selected the following variables concerning sleep quality: (i) sleep-onset latency, in minutes (0≤10 min; 1=10–19 min; 2=20–29 min; 3=30–39 min; 4=40–49 min; 5=50–59 min; 6≥60 min); and (ii) number of night wakings per night, which referred to signalled night waking requiring parental soothing between 10 pm and 6 am (0=does not wake; 1=once; 2=twice; 3=three times; 4=four times; 5=five or more).
Emotional and behavioural symptoms at 24 months were assessed using the Brief Infant-Toddler Social and Emotional Assessment (BITSEA),19 which consists of 42 items to identify children at risk for social-emotional/behavioural problems. According to our initial hypothesis, we used the externalising (7 items), internalising (8 items), and dysregulation subscales (8 items).
Covariates
Based on previous research,7 the covariates selected were: child’s age (in years) at 24 months and sex (female vs male), prenatal maternal health (generally healthy vs some health-related problem or disability), age (in years) and the highest education level (primary, secondary or high), and gestational age at birth (in weeks). Prevalence rates and descriptive values of these covariates are reported in tables 1 and 2.
Table 1.
Sociodemographic variables during pregnancy and in early childhood
| Sociodemographic variables during pregnancy/early childhood | Mean (SD) |
| Child birth weight in grams | 3573.4 (452.7) |
| Gestational age at birth in weeks | 40.0 (1.3) |
| Children’s age in days | |
| 3 months | 98.1 (14.7) |
| 8 months | 246.6 (9.6) |
| 18 months | 561.7 (47.7) |
| 24 months | 752.1 (42.6) |
| Maternal age during pregnancy in years | 31.1 (4.4) |
| N (%) | |
| Sex | |
| Male | 495 (52.9%) |
| Female | 441 (47.1%) |
| Maternal health during pregnancy | |
| Good health | 718 (76.9%) |
| Maternal education during pregnancy | |
| Primary | 40 (4.4%) |
| Secondary | 518 (56.6%) |
| High | 357 (39.0%) |
| Infantile colic in early childhood | |
| 3 months | 36 (4.0%) |
| 8 months | 21 (2.3%) |
Table 2.
Sleep variables in early childhood and socio-emotional functioning at 24 months
| Sleep variables in early childhood | ||||
| Mean (SD) | Median | Minimum | Maximum | |
| BISQ total sleep duration, hours | ||||
| 3 months | 14.3 (1.8) | 14.5 | 6.0 | 20.0 |
| 8 months | 13.3 (1.2) | 13.5 | 9.0 | 20.0 |
| 18 months | 12.3 (0.9) | 12.2 | 8.0 | 16.0 |
| 24 months | 11.9 (0.9) | 12.0 | 8.3 | 15.0 |
| BISQ proportion daytime sleep | ||||
| 3 months | 36.2 (8.2) | 36.4 | 10.0 | 77.8 |
| 8 months | 25.5 (6.5) | 25.0 | 10.0 | 53.8 |
| 18 months | 16.7 (4.9) | 16.0 | 6.0 | 39.3 |
| 24 months | 15.7 (5.0) | 15.9 | 0.0 | 40.0 |
| BISQ bedtime, hh:mm | ||||
| 3 months | 21:48 (1:11) | 21:32 | 18:00 | 02:10 |
| 8 months | 20:52 (0:54) | 21:00 | 18:20 | 01:30 |
| 18 months | 20:42 (0:42) | 20:30 | 18:30 | 23:40 |
| 24 months | 20:55 (0:40) | 21:00 | 18:45 | 23:30 |
| ISQ sleep-onset latency | ||||
| 3 months | 1.9 (1.8) | 1.0 | 0.0 | 6.0 |
| 8 months | 1.1 (1.2) | 1.0 | 0.0 | 6.0 |
| 18 months | 1.0 (1.1) | 1.0 | 0.0 | 6.0 |
| 24 months | 1.4 (1.5) | 1.0 | 0.0 | 6.0 |
| ISQ number of night wakings | ||||
| 3 months | 1.6 (1.3) | 2.0 | 0.0 | 5.0 |
| 8 months | 2.0 (1.4) | 2.0 | 0.0 | 5.0 |
| 18 months | 1.0 (1.2) | 1.0 | 0.0 | 5.0 |
| 24 months | 1.0 (1.0) | 1.0 | 0.0 | 5.0 |
| Socio-emotional functioning at 24 months | ||||
| Symptom scores | Mean (SD) | Median | Minimum | Maximum |
| BITSEA externalising | 3.1 (2.2) | 3.0 | 0.0 | 11.0 |
| BITSEA internalising | 1.6 (1.5) | 1.0 | 0.0 | 9.0 |
| BITSEA dysregulation | 3.1 (2.4) | 3.0 | 0.0 | 12.0 |
BISQ variables are all continuous variables, while ISQ sleep-onset latency and ISQ number of night wakings are categorical variables: in ISQ sleep-onset latency, 0=<10 min; 1=10–19 min; 2=20–29 min; 3=30–39 min; 4=40–49 min; 5=50–59 min; and 6=≥60 min; and in ISQ number of night wakings, 0=0 times/night; 1=once/night; 2=twice/night; 3=three times/night; 4=four times/night; and 5=five times/night.
BISQ=Brief Infant Sleep Questionnaire; BITSEA, Brief Infant-Toddler Social and Emotional Assessment; ISQ, Infant Sleep Questionnaire.
Statistical analysis
Statistical analyses were performed with SPSS V.25.0 (IBM Corporation) for Windows/Apple Mac. Descriptive statistics were calculated to obtain means, SD, frequencies and percentages. The three outcome variables and the explanatory variables except for sleep duration and proportion of daytime sleep were skewed, but due to the large sample size, parametric statistical testing was considered appropriate.20 However, due to the skewness of the earlier mentioned variables, we did sensitivity analyses after normality transformations of the skewed variables. Because the main findings were virtually unchanged, we present only the original results.
To test the hypothesis that sleep is related to emotional and behavioural symptoms, linear regression analysis was used. Independent variables comprised the sleep variables at 3, 8, 18 and 24 months, and dependent variables were BITSEA subscales at 24 months. Series of linear regression models were computed to study which sleep variables in early childhood were associated with BITSEA subscales in toddlers, with child’s age at 24 months and sex, and maternal health, age and education, and gestational age being included as covariates. To do this, all the sleep variables from the same time point were included within the same regression model (eg, total sleep duration, sleep-onset latency, night awakenings, proportion of daytime sleep and bedtime were all included within the same model), together with the covariates. Each time point (ie, 3, 8, 18 and 24 months) was treated in separate regression models. Furthermore, to study sex differences in emotional and behavioural problems,15 interaction terms between sex and sleep variables were entered to the models in a separate step and significant interaction terms were reported.21
Further, taking into account that the prevalence rate of infantile colic (IC) is about 5%,22 23 and that we found 39 cases in our total sample (ie, 4.2%: 36 cases at 3 months and 3 new cases at 8 months), we conducted the same linear regression analyses after excluding all cases with IC.
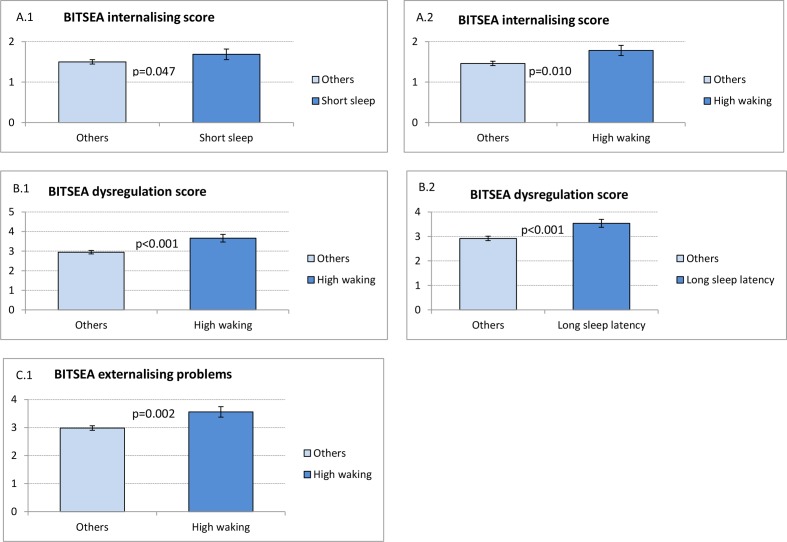
Finally, to graphically describe significant mean differences in BITSEA subscales at 24 months, the variables representing short sleep, high night waking and long sleep-onset latency were created, using the 25th (for short sleep) or 75th percentiles (for high night waking and long sleep-onset latency), to indicate deviance from the average development within our sample.
Patient and public involvement
Patient representatives were involved in the design of this follow-up study.
Results
Sociodemographic variables are described in table 1. Briefly, 47.1% of the sample were girls, the average gestational age at birth was 40 weeks, the average maternal age during pregnancy was 31 years, 76.9% of the mothers reported having good health and 39.0% of the mothers had high educational level. Descriptive information on sleep and socio-emotional functioning can be found in table 2.
Associations between parent-reported sleep and BITSEA
The results obtained from the linear regression models can be found in table 3.
Table 3.
Associations between sleep in early childhood and BITSEA internalising, dysregulation and externalising problems at 24 months
| Internalising symptoms | Dysregulation symptoms | Externalising symptoms | |||||||
| β | P value | 95% CI for B | β | P value | 95% CI for B | β | P value | 95% CI for B | |
| 3 months | |||||||||
| Total sleep | −0.08 | 0.041 | −0.13 to 0.00 | −0.07 | 0.051 | −0.19 to 0.00 | −0.02 | 0.647 | −0.11 to 0.07 |
| Sleep-onset latency | 0.06 | 0.090 | −0.01 to 0.16 | 0.15 | < 0.001 | 0.10 to 0.29 | 0.01 | 0.830 | −0.08 to 0.10 |
| Number of night waking | 0.13 | 0.001 | 0.06 to 0.23 | 0.13 | < 0.001 | 0.12 to 0.38 | 0.10 | 0.006 | 0.05 to 0.29 |
| Proportion daytime sleep | 0.03 | 0.535 | −0.01 to 0.02 | 0.03 | 0.488 | −0.01 to 0.03 | 0.02 | 0.699 | −0.02 to 0.03 |
| Bedtime | −0.04 | 0.345 | −0.16 to 0.06 | 0.00 | 0.950 | −0.17 to 0.16 | 0.05 | 0.246 | −0.06 to 0.25 |
| Child’s age at 24 months | 0.01 | 0.873 | 0.00 to 0.00 | 0.04 | 0.255 | 0.00 to 0.01 | 0.00 | 0.993 | 0.00 to 0.00 |
| Sex | −0.09 | 0.010 | −0.49 to − 0.07 | −0.04 | 0.250 | −0.52 to 0.14 | 0.13 | 0.000 | 0.27 to 0.88 |
| Maternal age during pregnancy | −0.08 | 0.041 | −0.05 to 0.00 | −0.09 | 0.011 | −0.09 to − 0.01 | −0.05 | 0.202 | −0.06 to 0.01 |
| Maternal education | 0.01 | 0.835 | −0.17 to 0.21 | 0.02 | 0.633 | −0.23 to 0.37 | −0.04 | 0.301 | −0.43 to 0.13 |
| Maternal health | −0.01 | 0.818 | −0.29 to 0.23 | 0.04 | 0.308 | −0.19 to 0.61 | 0.02 | 0.635 | −0.29 to 0.47 |
| Gestational age | −0.01 | 0.748 | −0.10 to 0.07 | −0.01 | 0.683 | −0.16 to 0.10 | −0.03 | 0.477 | −0.16 to 0.08 |
| 8 months | |||||||||
| Total sleep | −0.10 | 0.037 | −0.23 to − 0.01 | −0.17 | < 0.001 | −0.52 to − 0.17 | −0.03 | 0.456 | −0.23 to 0.11 |
| Sleep-onset latency | 0.07 | 0.061 | 0.00 to 0.18 | 0.10 | 0.006 | 0.06 to 0.34 | 0.07 | 0.067 | −0.01 to 0.27 |
| Number of night waking | 0.07 | 0.049 | 0.00 to 0.15 | 0.17 | < 0.001 | 0.17 to 0.41 | 0.02 | 0.534 | −0.08 to 0.15 |
| Proportion daytime sleep | 0.03 | 0.575 | −0.02 to 0.03 | 0.05 | 0.331 | −0.02 to 0.05 | 0.01 | 0.851 | −0.03 to 0.04 |
| Bedtime | −0.07 | 0.142 | −0.28 to 0.04 | −0.13 | 0.006 | −0.60 to − 0.10 | −0.04 | 0.398 | −0.34 to 0.14 |
| Child’s age at 24 months | −0.02 | 0.640 | 0.00 to 0.00 | 0.04 | 0.321 | 0.00 to 0.01 | −0.02 | 0.624 | −0.00 to 0.00 |
| Sex | −0.05 | 0.181 | −0.35 to 0.07 | −0.03 | 0.382 | −0.48 to 0.18 | 0.16 | 0.000 | 0.37 to 1.00 |
| Maternal age during pregnancy | −0.07 | 0.051 | −0.05 to 0.00 | −0.11 | 0.004 | −0.10 to − 0.02 | −0.06 | 0.114 | −0.07 to 0.01 |
| Maternal education | 0.01 | 0.744 | −0.16 to 0.23 | 0.02 | 0.639 | −0.23 to 0.38 | 0.00 | 0.991 | −0.29 to 0.29 |
| Maternal health | −0.04 | 0.258 | −0.40 to 0.11 | 0.04 | 0.309 | −0.19 to 0.60 | 0.02 | 0.597 | −0.28 to 0.48 |
| Gestational age | −0.02 | 0.603 | −0.10 to 0.06 | −0.01 | 0.678 | −0.16 to 0.10 | −0.04 | 0.283 | −0.19 to 0.06 |
| 18 months | |||||||||
| Total sleep | −0.01 | 0.862 | −0.14 to 0.12 | −0.11 | 0.004 | −0.50 to − 0.09 | 0.04 | 0.346 | −0.10 to 0.30 |
| Sleep-onset latency | 0.07 | 0.073 | −0.01 to 0.18 | 0.11 | 0.002 | 0.09 to 0.38 | 0.07 | 0.09 | −0.02 to 0.26 |
| Number of night waking | 0.08 | 0.019 | 0.02 to 0.20 | 0.25 | < 0.001 | 0.36 to 0.64 | 0.07 | 0.057 | 0.00 to 0.26 |
| Proportion daytime sleep | 0.04 | 0.385 | −0.01 to 0.04 | 0.08 | 0.057 | 0.00 to 0.08 | −0.01 | 0.730 | −0.05 to 0.03 |
| Bedtime | 0.01 | 0.776 | −0.15 to 0.20 | −0.07 | 0.102 | −0.50 to 0.05 | 0.01 | 0.866 | −0.24 to 0.29 |
| Child’s age at 24 months | 0.00 | 0.945 | 0.00 to 0.00 | 0.02 | 0.545 | 0.00 to 0.01 | −0.03 | 0.453 | −0.01 to 0.00 |
| Sex | −0.09 | 0.007 | −0.48 to − 0.08 | −0.01 | 0.702 | −0.37 to 0.25 | 0.133 | 0.000 | 0.28 to 0.89 |
| Maternal age during pregnancy | −0.11 | 0.002 | −0.06 to − 0.01 | −0.12 | 0.001 | −0.11 to − 0.03 | −0.062 | 0.086 | −0.07 to 0.01 |
| Maternal education | 0.01 | 0.678 | −0.15 to 0.23 | 0.03 | 0.339 | −0.15 to 0.42 | −0.009 | 0.810 | −0.31 to 0.24 |
| Maternal health | −0.02 | 0.635 | −0.30 to 0.19 | 0.01 | 0.791 | −0.32 to 0.42 | 0.003 | 0.927 | −0.35 to 0.38 |
| Gestational age | −0.02 | 0.553 | −0.10 to 0.06 | −0.02 | 0.498 | −0.17 to 0.08 | −0.010 | 0.767 | −0.14 to 0.10 |
| 24 months | |||||||||
| Total sleep | −0.03 | 0.535 | −0.19 to 0.10 | −0.12 | 0.002 | −0.54 to − 0.12 | −0.06 | 0.191 | −0.37 to 0.07 |
| Sleep-onset latency | 0.06 | 0.084 | −0.01 to 0.14 | 0.22 | < 0.001 | 0.25 to 0.45 | 0.10 | 0.007 | 0.04 to 0.25 |
| Number of night waking | 0.11 | 0.002 | 0.06 to 0.27 | 0.39 | < 0.001 | 0.83 to 1.12 | 0.07 | 0.047 | −0.01 to 0.31 |
| Proportion daytime sleep | 0.09 | 0.037 | 0.00 to 0.05 | 0.08 | 0.039 | 0.00 to 0.07 | 0.04 | 0.336 | −0.02 to 0.06 |
| Bedtime | 0.01 | 0.912 | −0.18 to 0.21 | −0.07 | 0.066 | −0.53 to 0.02 | 0.00 | 0.983 | −0.29 to 0.29 |
| Child’s age at 24 months | −0.01 | 0.784 | 0.00 to 0.00 | 0.01 | 0.739 | 0.00 to 0.00 | −0.04 | 0.229 | −0.01 to 0.00 |
| Sex | −0.07 | 0.043 | −0.39 to − 0.01 | 0.00 | 0.931 | −0.29 to 0.26 | 0.14 | 0.000 | 0.34 to 0.92 |
| Maternal age during pregnancy | −0.13 | 0.000 | −0.07 to − 0.02 | −0.11 | 0.000 | −0.10 to − 0.03 | −0.05 | 0.129 | −0.06 to 0.01 |
| Maternal education | 0.03 | 0.450 | −0.11 to 0.24 | 0.02 | 0.526 | −0.17 to 0.33 | −0.02 | 0.627 | −0.33 to 0.12 |
| Maternal health | −0.01 | 0.692 | −0.28 to 0.19 | 0.01 | 0.760 | −0.28 to 0.38 | 0.02 | 0.583 | −0.25 to 0.45 |
| Gestational age | −0.01 | 0.866 | −0.08 to 0.07 | −0.03 | 0.306 | −0.17 to 0.05 | 0.00 | 0.968 | −0.12 to 0.11 |
Covariates: child’s age at 24 months, sex, maternal age, maternal education, maternal health and gestational age.
Shorter sleep at 3 and 8 months, and more night wakings at 3, 8 and 18 months were prospectively related to more internalising symptoms at 24 months. Further, more night wakings and higher proportion of daytime sleep were concurrently associated with more internalising symptoms at 24 months. Girls with more night wakings at 24 months had higher risk for internalising symptoms than boys (B=0.243, p=0.022).
Shorter sleep at 8 and 18 months, longer sleep-onset latency and more night wakings at 3, 8 and 18 months, and earlier bedtime at 8 months were significantly related to higher levels of dysregulation at 24 months. Moreover, shorter sleep, longer sleep-onset latency, more night wakings and slower circadian development were concurrently related to higher dysregulation at 24 months. Boys with longer sleep-onset latency at 3 months had higher risk for dysregulation at 24 months (B=0.205, p=0.035), and girls with more night wakings at 24 months presented higher risk for dysregulation (B=0.355, p=0.018).
More night wakings at 3 months were related to more externalising symptoms at 24 months. Furthermore, longer sleep-onset latency and more night wakings at 24 months were concurrently linked with more externalising symptoms. There were no statistically significant interactions between sex and sleep.
After excluding the 39 cases with IC, we observed that the main findings remained, which suggests that the results are not due to IC (data not shown).
The main significant differences in each of the BITSEA subscales at 24 months are presented in figure 1. In this figure, infants with short sleep duration, high night wakings frequency and long sleep-onset latency are compared with other infants.
Figure 1.
Significant differences in BITSEA subscales at 24 months in terms of the onset of sleep problems at 3 months (short sleep, long sleep-onset latency and high frequency of night waking). These graphs describe the results where significant differences between groups were observed. All the variables concerning sleep problems described here (ie, short sleep, high frequency of night waking and long sleep-onset latency) represent the 25th or 75th percentile, which indicate deviance from the average development. Short sleep at 3 months refers to those infants reporting 13 hours of sleep duration or less, per 24 hours, while non-short sleep refers to all those cases sleeping more than 13 hours per 24 hours. High frequency of night waking at 3 months refers to those infants who wake up at night three times or more, while those cases reporting between 0 and 2 night wakings comprise the group non-high waking. Finally, long sleep-onset latency at 3 months refers to those infants who spend more than 30 min awake before falling asleep, while infants with a sleep-onset latency lower than 30 min comprise the group non-long sleep-onset latency. Graphs A.1–2 shows that those infants with short sleep duration (A.1) and infants with high frequency of night waking (A.2) at 3 months report higher scores in BITSEA internalising subscale than their comparison group. Graphs B.1–2 indicate that infants with high frequency of night waking (B.1) and infants with long sleep-onset latency (B.2) at 3 months score higher in BITSEA dysregulation subscale at 24 months. Finally, graph C.1 shows that infants with high frequency of night waking at 3 months report higher score in BITSEA externalising subscale at 24 months. Error bars represent 95% CI.
Discussion
Our findings supported our initial hypothesis that some sleep problems (ie, frequent night wakings and longer sleep-onset latency) in early childhood are related to internalising and externalising symptoms at 24 months. Importantly, we found that night wakings already at the age of 3 months related to internalising and externalising symptoms in toddlers. Furthermore, sleep quality and shorter sleep duration in early childhood were closely associated with dysregulation at 24 months.
We found that shorter sleep duration and frequent night wakings at 3 months were related to internalising problems at 24 months, which is consistent with previous research reporting that short sleep duration and night wakings at 18 months related to internalising symptoms at 5 years.7 Our findings are particularly important from clinical perspective, suggesting that it might be relevant to evaluate infants’ sleep already at 3 months, to recognise those cases with short sleep duration and frequent night wakings and to provide them behavioural counselling and/or sleep hygiene habits to improve their sleep quality.
Profound increases in regulatory capacity take place in later toddlerhood,24 25 and factors that modify this development have been poorly characterised. We found that all sleeping difficulties in early childhood were prospectively related to dysregulation at 24 months. While one previous study did not find any significant associations between early sleep and self-regulation at 18 months,8 the study had a more limited sample size (117 mother–child dyads). Moreover, they excluded the sleep variables from the dysregulation subscale. However, we did not exclude the two sleep-related items from our dysregulation subscale, as we consider sleep an integral and modifiable part of self-regulation that is controlled by various regulatory pathways and can be affected also by many environmental factors. Our findings indicate that sleep quality in early childhood and development of self-regulation are closely intertwined. While there are no other similar studies in early childhood, such associations have been reported in teenagers and adults.26–28 Our findings raise the question whether timely treatment of sleeping problems in infancy could improve development of self-regulation in early childhood. More studies are needed in future to further inform this issue.
Notably, we also found that frequent night wakings at 3 months and externalising symptoms at 24 months were associated. This finding suggests that frequent night waking already at 3 months may warrant clinical evaluation. Even though night wakings are normal and quite prevalent till the age of 2 years, the very frequent night wakings seem to indicate risk for further social-emotional development. More studies are needed to characterise risk factors for night wakings at the age of 3 months and to evaluate effectiveness of clinical interventions to improve sleep quality. We also found associations between frequent night wakings and long sleep-onset at 24 months and concurrent externalising symptoms. Typical sleeping difficulties at 24 months are behavioural insomnias (ie, bedtime resistance),29 which will lead, in turn, to longer sleep-onset latency. Furthermore, toddlers with externalising problems are characterised by increases in bedtime resistance,30 which supports the existing associations between longer sleep-onset latency and externalising symptoms at 24 months.
The associations reported in this study may be due to several potential underpinning mechanisms. First, sleep and emotional problems can be induced by similar biological mechanisms related to predisposing genetic factors. In other words, individual variability in sleep-wake behaviour problems has been linked to affect and emotions through hypothesised shared central nervous system to sleep and the neurobehavioural systems underlying arousal and emotions.31 32 In accordance with this assumption, difficult temperament33 and genetic factors34 are related to both sleeping and emotional problems in children. Second, sleep and emotional problems may be explained by the same environmental factors. At early stages of life when infants spend most of their time in their family environment, the associations between early sleep problems and emotional and behavioural problems at 24 months might be also explained by family-related factors, like sleeping practices in the family such as co-sleeping versus independent sleeping, parental reactions to infant crying and/or maternal depression and anxiety. Moreover, both prenatal and postnatal maternal stress are associated with socio-emotional development,35 child behaviour36 and adverse psychological outcomes in children.37 Consequently, numerous underlying parenting factors could explain the association between sleep and socio-emotional development in childhood. Further studies are needed to understand why early sleeping difficulties and social-emotional problems are associated. Third, there is a well-established link between sleep deprivation and increased risk for emotional symptoms in different age groups. Altogether, converging evidence suggests that sleep deprivation impairs the connectivity between prefrontal cortex and amygdala, which can have significant effects on the individual’s ability to regulate emotions. Evidence suggests that one of the strongest adverse effects of sleep deprivation is increased negative mood.38 Furthermore, previous studies of children and adolescents have revealed significant associations between sleep deprivation and irritability/aggression and difficulties with self-regulation.39 40
The strengths of this study lie in its relatively large population-based sample and the coverage of sleep measures from the age of 3 months. However, there are some limitations. First, although we controlled for some confounding factors, there are other environmental and parental factors that may play a role beyond the studied phenomena. Second, assessment of socio-emotional functioning at 24 months was solely based on parental report. Third, reciprocal influence among sleep and socio-emotional problems such as dysregulation9 and externalising symptoms41 can also occur, and thus further studies concerning the reciprocal associations are needed.
Conclusions
Our findings show that night wakings at 3 months are prospectively related to internalising and externalising symptoms in toddlers. Furthermore, shorter sleep, longer sleep-onset latency and night wakings in early childhood are closely related to dysregulation in toddlers. This study contributes to recent research on the role of early sleep problems in socio-emotional development, showing that sleep duration, sleep-onset latency and waking frequency are associated with later emotional and behavioural problems. Future studies should focus on addressing the efficacy of sleep interventions not only to ameliorate sleeping problems per se but also to emotional symptoms later on. Further, a key study would be adapting and trialling in younger ages (ie, infancy and toddlers), the already existing sleep interventions that have been conducted in school-aged children.42 43 If children’s emotional symptoms are reduced by providing behavioural interventions for infants with sleep problems and the families, this would be highly relevant for the improvement of children’s quality of life.
Supplementary Material
Footnotes
Contributors: IMM designed the study, drafted the initial manuscript, conducted data analysis and reviewed and revised the manuscript. SL assisted with data analysis and reviewed and revised the manuscript. OS-H, AK, PP and TP conceptualised and designed the study, designed the data collection instruments, coordinated and supervised data collection and critically reviewed the manuscript for important intellectual content. MB conceptualised the study and critically reviewed the manuscript for important intellectual content. JP conceptualised and designed the study, designed the data collection instruments, coordinated and supervised data collection and data analysis and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Funding: This project was funded by The Academy of Finland (#134880, #253346, #308588, #277557, #315035, and #326631), the Signe and Ane Gyllenberg Foundation, the Yrjö Jahnsson Foundation, the Foundation for Pediatric Research, the Finnish Cultural Foundation, the Competitive Research Financing of the Expert Responsibility area of Tampere University Hospital, the Arvo ja Lea Ylppö Foundation, and Doctors’ Association in Tampere.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting or dissemination plans of this research. Refer to the Methods section for further details.
Patient consent for publication: Not required.
Ethics approval: This study was approved by the local hospital district ethical committee.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data may be obtained from a third party and are not publicly available.
References
- 1. Williamson AA, Mindell JA, Hiscock H, et al. . Child sleep behaviors and sleep problems from infancy to school-age. Sleep Med 2019;63:5–8. 10.1016/j.sleep.2019.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chaput J-P, Gray CE, Poitras VJ, et al. . Systematic review of the relationships between sleep duration and health indicators in the early years (0-4 years). BMC Public Health 2017;17:855 10.1186/s12889-017-4850-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ogundele MO. Behavioural and emotional disorders in childhood: a brief overview for paediatricians. World J Clin Pediatr 2018;7:9–26. 10.5409/wjcp.v7.i1.9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Spruyt K. A review of developmental consequences of poor sleep in childhood. Sleep Med 2019;60:3–12. 10.1016/j.sleep.2018.11.021 [DOI] [PubMed] [Google Scholar]
- 5. Jansen PW, Saridjan NS, Hofman A, et al. . Does disturbed sleeping precede symptoms of anxiety or depression in toddlers? the generation R study. Psychosom Med 2011;73:242–9. 10.1097/PSY.0b013e31820a4abb [DOI] [PubMed] [Google Scholar]
- 6. Lam P, Hiscock H, Wake M. Outcomes of infant sleep problems: a longitudinal study of sleep, behavior, and maternal well-being. Pediatrics 2003;111:e203–7. 10.1542/peds.111.3.e203 [DOI] [PubMed] [Google Scholar]
- 7. Sivertsen B, Harvey AG, Reichborn-Kjennerud T, et al. . Later emotional and behavioral problems associated with sleep problems in toddlers: a longitudinal study. JAMA Pediatr 2015;169:575–82. 10.1001/jamapediatrics.2015.0187 [DOI] [PubMed] [Google Scholar]
- 8. Mindell JA, Leichman ES, DuMond C, et al. . Sleep and Social-Emotional development in infants and toddlers. J Clin Child Adolesc Psychol 2017;46:236–46. 10.1080/15374416.2016.1188701 [DOI] [PubMed] [Google Scholar]
- 9. Williams KE, Berthelsen D, Walker S, et al. . A developmental cascade model of behavioral sleep problems and emotional and attentional self-regulation across early childhood. Behav Sleep Med 2017;15:1–21. 10.1080/15402002.2015.1065410 [DOI] [PubMed] [Google Scholar]
- 10. Kopp CB, Neufeld SJ. Emotional development during infancy : Davidson R, Scherer KR GH, Handbook of affective sciences. London: Oxford Univ. Press, 2003. [Google Scholar]
- 11. Wang Z, Deater-Deckard K, Petrill SA, et al. . Externalizing problems, attention regulation, and household chaos: a longitudinal behavioral genetic study. Dev Psychopathol 2012;24:755–69. 10.1017/S0954579412000351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jenni OG, Borbély AA, Achermann P. Development of the nocturnal sleep electroencephalogram in human infants. Am J Physiol Regul Integr Comp Physiol 2004;286:R528–38. 10.1152/ajpregu.00503.2003 [DOI] [PubMed] [Google Scholar]
- 13. Paavonen EJ, Saarenpää-Heikkilä O, Morales-Munoz I, et al. . Normal sleep development in infants: findings from two large birth cohorts. Sleep Med. In Press 2020;69:145–54. 10.1016/j.sleep.2020.01.009 [DOI] [PubMed] [Google Scholar]
- 14. Petit D, Touchette E, Tremblay RE, et al. . Dyssomnias and parasomnias in early childhood. Pediatrics 2007;119:e1016–25. 10.1542/peds.2006-2132 [DOI] [PubMed] [Google Scholar]
- 15. Alakortes J, Fyrstén J, Carter AS, et al. . Finnish mothers' and fathers' reports of their boys and girls by using the brief Infant-Toddler social and emotional assessment (BITSEA). Infant Behav Dev 2015;39:136–47. 10.1016/j.infbeh.2015.02.016 [DOI] [PubMed] [Google Scholar]
- 16. Juulia Paavonen E, Saarenpää-Heikkilä O, Pölkki P, et al. . Maternal and paternal sleep during pregnancy in the Child-sleep birth cohort. Sleep Med 2017;29:47–56. 10.1016/j.sleep.2016.09.011 [DOI] [PubMed] [Google Scholar]
- 17. Sadeh A. A brief screening questionnaire for infant sleep problems: validation and findings for an Internet sample. Pediatrics 2004;113:e570–7. 10.1542/peds.113.6.e570 [DOI] [PubMed] [Google Scholar]
- 18. Morrell JMB. The infant sleep questionnaire: a new tool to assess infant sleep problems for clinical and research purposes. Child psychol. psychiatr. rev. 1999;4:20–6. 10.1017/S1360641798001816 [DOI] [Google Scholar]
- 19. Briggs-Gowan MJ, Carter AS, Irwin JR, et al. . The brief Infant-Toddler social and emotional assessment: screening for social-emotional problems and delays in competence. J Pediatr Psychol 2004;29:143–55. 10.1093/jpepsy/jsh017 [DOI] [PubMed] [Google Scholar]
- 20. Ghasemi A, Zahediasl S. Normality tests for statistical analysis: a guide for non-statisticians. Int J Endocrinol Metab 2012;10:486–9. 10.5812/ijem.3505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Aiken LS, West SG. Multiple regression: testing and interpreting interactions. London: Sage Publications, 1991. [Google Scholar]
- 22. Brand S, Furlano R, Sidler M, et al. . ‘Oh, baby, please don't cry!’: in infants suffering from infantile colic hypothalamic-pituitary-adrenocortical axis activity is related to poor sleep and increased crying intensity. Neuropsychobiology 2011;64:15–23. 10.1159/000322456 [DOI] [PubMed] [Google Scholar]
- 23. Brand S, Furlano R, Sidler M, et al. . Associations between infants' crying, sleep and cortisol secretion and mother's sleep and well-being. Neuropsychobiology 2014;69:39–51. 10.1159/000356968 [DOI] [PubMed] [Google Scholar]
- 24. Rothbart MK, Sheese BE, Rueda MR, et al. . Developing mechanisms of self-regulation in early life. Emot Rev 2011;3:207–13. 10.1177/1754073910387943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Montroy JJ, Bowles RP, Skibbe LE, et al. . The development of self-regulation across early childhood. Dev Psychol 2016;52:1744–62. 10.1037/dev0000159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Owens JA, Dearth-Wesley T, Lewin D, et al. . Self-Regulation and sleep duration, sleepiness, and Chronotype in adolescents. Pediatrics 2016;138 10.1542/peds.2016-1406. [Epub ahead of print: 03 Nov 2016]. [DOI] [PubMed] [Google Scholar]
- 27. Minkel J, Htaik O, Banks S, et al. . Emotional expressiveness in sleep-deprived healthy adults. Behav Sleep Med 2011;9:5–14. 10.1080/15402002.2011.533987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Baum KT, Desai A, Field J, et al. . Sleep restriction worsens mood and emotion regulation in adolescents. J Child Psychol Psychiatry 2014;55:180–90. 10.1111/jcpp.12125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Vriend J, Corkum P. Clinical management of behavioral insomnia of childhood. Psychol Res Behav Manag 2011;4:69–79. 10.2147/PRBM.S14057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Conway A, Miller AL, Modrek A. Testing reciprocal links between trouble getting to sleep and internalizing behavior problems, and bedtime resistance and Externalizing behavior problems in toddlers. Child Psychiatry Hum Dev 2017;48:678–89. 10.1007/s10578-016-0692-x [DOI] [PubMed] [Google Scholar]
- 31. Dahl RE. The impact of inadequate sleep on children's daytime cognitive function. Semin Pediatr Neurol 1996;3:44–50. 10.1016/S1071-9091(96)80028-3 [DOI] [PubMed] [Google Scholar]
- 32. Walker MP. The role of sleep in cognition and emotion. Ann N Y Acad Sci 2009;1156:168–97. 10.1111/j.1749-6632.2009.04416.x [DOI] [PubMed] [Google Scholar]
- 33. Hayes MJ, McCoy SK, Fukumizu M, et al. . Temperament and sleep-wake behaviors from infancy to Toddlerhood. Infant Child Dev 2011;20:495–508. 10.1002/icd.720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Bouvette-Turcot A-A, Pluess M, Bernier A, et al. . Effects of genotype and sleep on temperament. Pediatrics 2015;136:e914–21. 10.1542/peds.2015-0080 [DOI] [PubMed] [Google Scholar]
- 35. Madigan S, Oatley H, Racine N, et al. . A meta-analysis of maternal prenatal depression and anxiety on child Socioemotional development. J Am Acad Child Adolesc Psychiatry 2018;57:645–57. 10.1016/j.jaac.2018.06.012 [DOI] [PubMed] [Google Scholar]
- 36. Satyanarayana VA, Lukose A, Srinivasan K. Maternal mental health in pregnancy and child behavior. Indian J Psychiatry 2011;53:351–61. 10.4103/0019-5545.91911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Verkuijl NE, Richter L, Norris SA, et al. . Postnatal depressive symptoms and child psychological development at 10 years: a prospective study of longitudinal data from the South African birth to twenty cohort. Lancet Psychiatry 2014;1:454–60. 10.1016/S2215-0366(14)70361-X [DOI] [PubMed] [Google Scholar]
- 38. Van Dongen HPA, Maislin G, Mullington JM, et al. . The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep 2003;26:117–26. 10.1093/sleep/26.2.117 [DOI] [PubMed] [Google Scholar]
- 39. Chervin RD, Dillon JE, Archbold KH, et al. . Conduct problems and symptoms of sleep disorders in children. J Am Acad Child Adolesc Psychiatry 2003;42:201–8. 10.1097/00004583-200302000-00014 [DOI] [PubMed] [Google Scholar]
- 40. Ireland JL, Culpin V. The relationship between sleeping problems and aggression, anger, and impulsivity in a population of juvenile and young offenders. J Adolesc Health 2006;38:649–55. 10.1016/j.jadohealth.2005.05.027 [DOI] [PubMed] [Google Scholar]
- 41. Quach JL, Nguyen CD, Williams KE, et al. . Bidirectional associations between child sleep problems and internalizing and Externalizing difficulties from preschool to early adolescence. JAMA Pediatr 2018;172:e174363 10.1001/jamapediatrics.2017.4363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Hiscock H, Sciberras E, Mensah F, et al. . Impact of a behavioural sleep intervention on symptoms and sleep in children with attention deficit hyperactivity disorder, and parental mental health: randomised controlled trial. BMJ 2015;350:h68 10.1136/bmj.h68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Quach J, Hiscock H, Ukoumunne OC, et al. . A brief sleep intervention improves outcomes in the school entry year: a randomized controlled trial. Pediatrics 2011;128:692–701. 10.1542/peds.2011-0409 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.