Abstract
Background
The ‘golden hour’ is a well-known concept, suggesting that shortening time from injury to definitive care is critically important for better outcome of trauma patients. However, there was no established evidence to support it. We aimed to validate the association between time to definitive care and mortality in hemodynamically unstable patients for the current trauma care settings.
Methods
The data were collected from the Japan Trauma Data Bank between 2006 and 2015. The inclusion criteria were patients with systolic blood pressure (SBP) <90 mm Hg and heart rate (HR) >110 beats/min or SBP <70 mm Hg who underwent definitive care within 4 hours from the onset of injury and survived for more than 4 hours. The outcome measure was in-hospital mortality. We evaluated the relationship between time to definitive care and mortality using the generalized additive model (GAM). Subgroup analysis was also conducted using GAM after dividing the patients into the severe (SBP <70 mm Hg) and moderate (SBP ≥70 mm Hg and <90 mm Hg, and HR >110 beats/min) shock group.
Results
1169 patients were enrolled in this study. Of these, 386 (33.0%) died. Median time from injury to definitive care was 137 min. Only 61 patients (5.2%) received definitive care within 60 min. The GAM models demonstrated that mortality remained stable for the early phase, followed by a decrease over time. The severe shock group presented with a paradoxical decline of mortality with time, whereas the moderate shock group had a time-dependent increase in mortality.
Discussion
We did not observe the association of shorter time to definitive care with a decrease in mortality. However, this was likely an offset result of severe and moderate shock groups. The result indicated that early definitive care could have a positive impact on survival outcome of patients with moderate shock.
Level of evidence
Level Ⅳ, prognostic study,
Background
Time management is considered as a key factor to reduce mortality in trauma patients. The ‘golden hour’ is a concept that critically injured patients are required to receive definitive care within 60 min from the occurrence of injuries, after which mortality significantly increased.1 2 This concept was developed in 1970s without any data or reference.3 However, it has been widely accepted with clinical plausibility.
The recent systematic review has concluded that there was no established evidence supporting this principle for patients with undifferentiated trauma.4 However, a few studies have suggested that limited patients, who had hypotension requiring critical intervention, could benefit from minimizing out-of-hospital time.5 6 Another point is that trauma care strategies have been drastically developed over the last decades, for example, resuscitative endovascular balloon occlusion of the aorta (REBOA), massive transfusion and helicopter emergency medical service (EMS). Therefore, the optimal target and management should be revised in the current settings.
The objective of this study was to clarify the exact relationship between elapsed time and mortality for the current trauma care settings. We also aimed to identify patients who could benefit from earlier definitive care by hemodynamic status.
Methods
Sample and data collection
The data were collected from the Japan Trauma Data Bank (JTDB), which is a prospective multicenter trauma registry that includes more than 260 institutions in Japan. The registry contains data of patients with trauma who had an injury of a three or more on the Abbreviated Injury Scale (AIS) in at least one body region. We collected the sample for the study from the JTDB for the period from 2006 to 2015. Data consisted of demographics, injury severity characteristics, time course (EMS calls, arrival at hospitals, initiating definitive care and so on), type of initial procedures and definitive care and course of hospitalization. A dataset provided from JTDB was anonymized.
Hemodynamically unstable trauma patients who received definitive care within 4 hours from the onset of injury were enrolled in this study. Of these, we only included those who survived at least for 4 hours to minimize immortal time bias.7 The exclusion criteria were as follows: children younger than 15 years old, those who presented with no signs of life (asystole on an ECG monitor) before arrival at the hospitals, those who had neither blunt nor penetrating injuries (eg, burns, hanging or others), those who were not directly transported from the scene through EMS (eg, transferred from another hospital and transported by private vehicle), those who were transferred to another hospital within 24 hours after the admission and those with incomplete or erroneous time record.
Definition
Hemodynamically unstable status was defined as systolic blood pressure (SBP) on arrival <90 mm Hg and heart rate (HR) >110 beats/min on arrival or SBP <70 mm Hg on arrival. Information about the time of injury onset was often unclear, and many records were missing. Therefore, we used EMS call activation time as a proxy of injury onset based on the assumption that time from injury onset to EMS activation was very short.8 Definitive care was defined as surgical and radiological interventions for hemostasis or any surgeries for acute emergency purposes (eg, peritonitis surgery, brain surgery, bone fixation or vascular surgery). By definition, definitive care did not include any procedures performed to stabilize patients in the emergency departments (eg, intubation and application of REBOA and resuscitative thoracotomy (RT)). The outcome measure was in-hospital all-cause mortality.
Statistical analysis
We estimated the odds of mortality over the time to definitive care using the generalized additive model (GAM). The non-parametric curve was drawn based on the assumption that mortality varied over time, and there was a non-linear relationship between them.9 10 The GAM model was adjusted for the following variables: age, gender, penetrating injury, vital signs on arrival (SBP, HR and Glasgow Coma Scale), Injury Severity Score and AIS in head. Given the difference in quality of trauma care over the study period, the year of occurrence of the injury was also used as a covariate.
To identify an effect modification between injury severity and elapsed time, we conducted further analysis with stratification according to the severity of shock. The patients were divided into two subgroups: patients with severe shock and moderate shock. Severe shock was defined as SBP <70 mm Hg on arrival, and moderate shock was defined as SBP between 70 mm Hg and 90 mm Hg, and HR >110 beats/min on arrival.
Sensitivity analysis was conducted to use the actual time of injury onset to validate the result, excluding patients who had a missing or erroneous record of that time.
Descriptive data were presented as median (Interquartile range; IQR) for continuous variables and proportions for categorical variables. We performed Wilcoxon rank sum test and χ2 test to compare the baseline characteristics between of the groups. All analyses were performed using R (version 3.6.2, R Foundation for Statistical Computing, Vienna, Austria).
Results
Participants
A total of 1564 adult trauma patients were identified over the study period. Of these, the following patients were excluded: those aged <15 years (n=44), those who presented with no signs of life before arrival at the hospital (n=160) and burn or other types of injury (n=13), those who were transferred from another hospital or other places (n=116), those who were transferred to another hospital within 24 hours from admission (n=13) and those with missing or erroneous records (n=49). After the exclusions, 1169 patients were enrolled in this study.
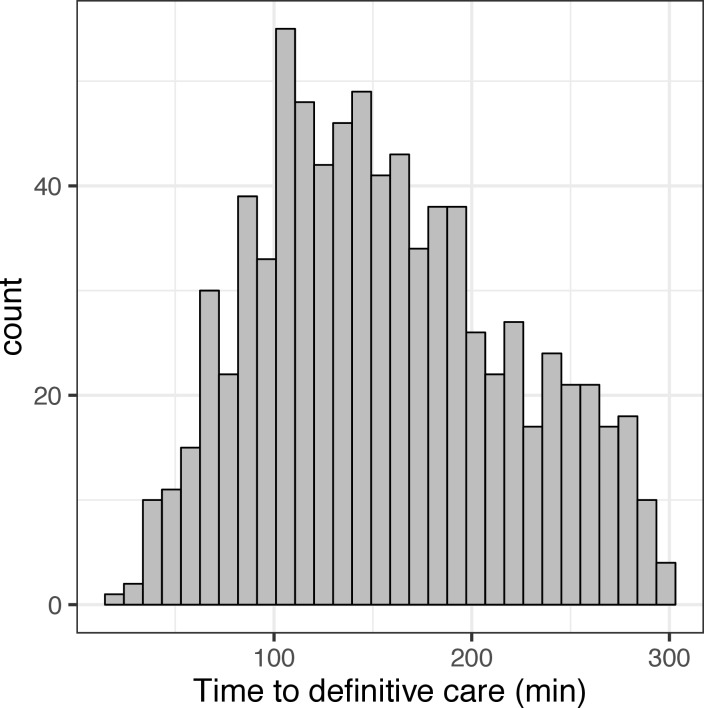
The baseline characteristics of the patients are presented in table 1. Of all, median age was 50 years (IQR 34–67 years) and 779 patients (66.6%) were male. Median ISS, SBP and HR were 29 (IQR 16–41), 62 mm Hg (IQR 40–74 mm Hg) and 119 beats/min (IQR 93–133 beats/min), respectively. In-hospital mortality of all patients was 386 (33.0%). The primary sample included 777 (66.5%) patients in the severe shock group and 392 (33.5%) patients in the moderate shock group. The distribution of time to definitive care was illustrated in figure 1. Median time from injury to definitive care was 137 min (IQR 102–177 min). Of all, only 61 patients (5.2%) received definitive care within 60 min, that is ‘golden hour’. In detail, prehospital time (time from injury to arrival at hospitals) was 37 min (IQR 28–48 min), and in-hospital time (time from arrival at hospitals) was 95 min (IQR 61–133 min).
Table 1.
Characteristics of patients
| Total | Severe shock | Moderate shock | ||||
| n=1169 | n=777 | n=392 | ||||
| Median age, year (IQR) | 50.0 | (34.0–67.0) | 54.0 | (36.0–70.0) | 43.5 | (30.0–60.0) |
| Male (%) | 779 | (66.6) | 513 | (66.0) | 266 | (67.9) |
| Year of occurrence | ||||||
| 2006–2010 (%) | 478 | (40.9) | 306 | (39.4) | 392 | (43.9) |
| 2011–2015 (%) | 691 | (59.1) | 471 | (60.6) | 220 | (56.1) |
| Penetrating injury (%) | 271 | (23.2) | 169 | (21.8) | 102 | (26.0) |
| Transport measure (%) | ||||||
| Ambulance | 975 | (83.4) | 649 | (83.5) | 326 | (83.2) |
| Doctor-staffed car | 82 | (7.0) | 57 | (7.3) | 25 | (6.4) |
| Helicopter | 112 | (9.6) | 71 | (9.1) | 41 | (10.5) |
| Median ISS (IQR) | 29.0 | (16.0–41.0) | 27.0 | (16.0–41.0) | 29.0 | (16.0–41.0) |
| Median AIS (IQR) | ||||||
| Brain | 0.0 | (0.0–3.0) | 0.0 | (0.0–3.0) | 0.0 | (0.0–3.0) |
| Chest | 3.0 | (0.0–4.0) | 2.0 | (0.0–4.0) | 3.0 | (0.0–4.0) |
| Abdomen | 2.0 | (0.0–3.0) | 2.0 | (0.0–4.0) | 2.0 | (0.0–3.0) |
| Lower extremities and pelvis | 2.0 | (0.0–4.0) | 2.0 | (0.0–4.0) | 1.0 | (0.0–4.0) |
| Vital signs on arrival, median (IQR) | ||||||
| SBP | 62.0 | (40.0–74.0) | 54.0 | (40.0–62.0) | 80.0 | (74.0–84.0) |
| RR | 25.0 | (20.0–30.0) | 24.0 | (20.0–30.0) | 26.0 | (20.0–32.0) |
| HR | 119.0 | (93.0–133.0) | 107.0 | (82.0–127.0) | 126.0 | (118.0–140.0) |
| GCS | 12.0 | (6.0–14.0) | 12.0 | (6.0–14.0) | 13.0 | (7.0–14.0) |
| Type of procedure in ED (%) | ||||||
| Intubation | 770 | (65.9) | 524 | (67.4) | 246 | (62.8) |
| ERT | 69 | (5.9) | 51 | (6.6) | 18 | (4.6) |
| REBOA | 154 | (13.2) | 120 | (15.4) | 34 | (8.7) |
| Transfusion | 948 | (81.1) | 626 | (80.6) | 322 | (82.1) |
| Type of definitive care (%) | ||||||
| Craniotomy | 50 | (4.3) | 33 | (4.2) | 17 | (4.3) |
| Thoracotomy | 159 | (13.6) | 105 | (13.5) | 54 | (13.8) |
| Laparotomy | 387 | (33.1) | 256 | (32.9) | 131 | (33.4) |
| Orthopedic surgery | 141 | (12.1) | 99 | (12.7) | 42 | (10.7) |
| TAE | 340 | (29.1) | 226 | (29.1) | 114 | (29.1) |
| Median time interval, min (IQR) | ||||||
| From injury to arrival at hospital | 37.0 | (28.0–48.0) | 36.0 | (28.0–48.0) | 37.0 | (28.0–49.0) |
| From arrival at hospital to definitive care | 95.0 | (61.0–133.0) | 93.0 | (60.0–132.0) | 100.0 | (63.0–137.0) |
| From injury to definitive care | 137.0 | (102.0–177.0) | 136.0 | (101.0–177.0) | 139.0 | (103.8–179.2) |
| Hospital course | ||||||
| In-hospital mortality | 386 | (33.0) | 282 | (36.3) | 104 | (26.5) |
| Median length of stay in hospital (IQR) | 20.0 | (2.0–58.8) | 17.0 | (1.0–59.0) | 24.0 | (4.0–58.0) |
AIS, Abbreviated Injury Scale; ED, emergency department; ERT, emergency resuscitative thoracotomy; GCS, Glasgow Coma Scale; HR, heart rate; IQR, Interquartile range; ISS, Injury Severity Score; REBOA, resuscitative endovascular balloon occlusion of the aorta; RR, respiratory rate; SBP, systolic blood pressure; TAE, transarterial embolization.
Figure 1.
Distribution of time from injury to definitive care.
Generalized additive model
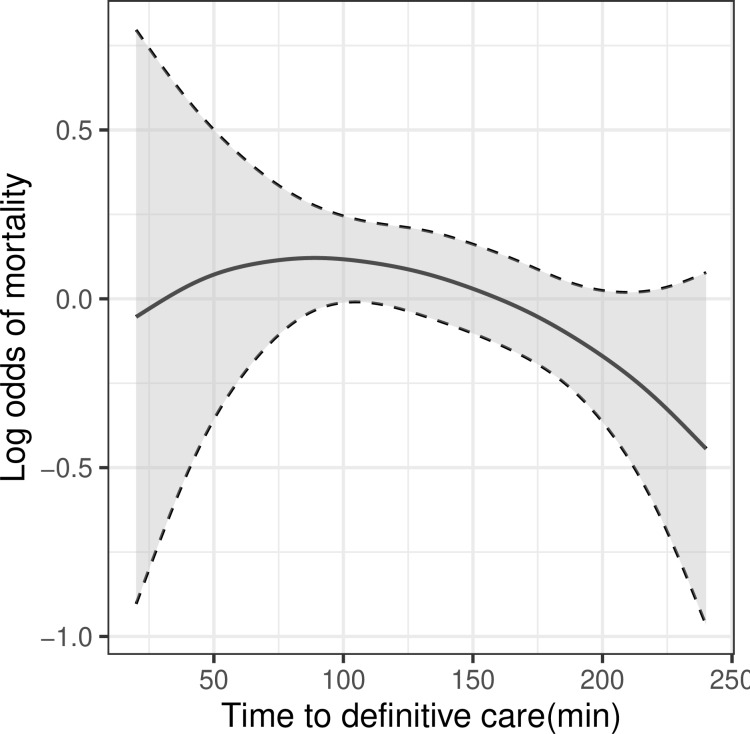
In the GAM model, the trend of mortality for all patients by the time to definitive care is shown in figure 2. The fitted curve showed relative stability in mortality for the early phase, followed by a decreasing trend in mortality with time.
Figure 2.
Non-parametric curves of trend in log odds of in-hospital mortality with time to definitive care using the generalized additive model for total patients (n=1169). The shade bands showed 95% CI.
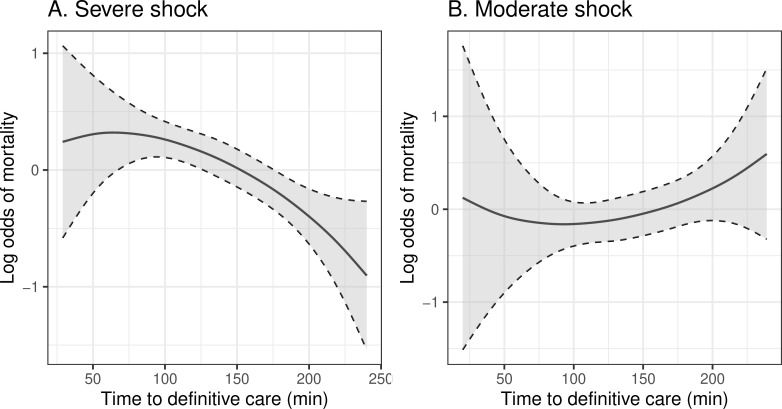
In the subgroup analysis, patients were stratified into the severe shock (n=777) and moderate shock group (n=392). The curves of mortality over the time between patients with severe and moderate shock are depicted in figure 3A and B, respectively. A decrease in mortality with increasing time was noted in the severe shock group. In contrast, an upward curve over the time was observed in the moderate shock group.
Figure 3.
Non-parametric curves of trend in log odds of in-hospital mortality with time to definitive care using generalized additive models ((A) severe shock patients: n=777; (B) moderate shock patients: n=392). The shade bands showed 95% CI.
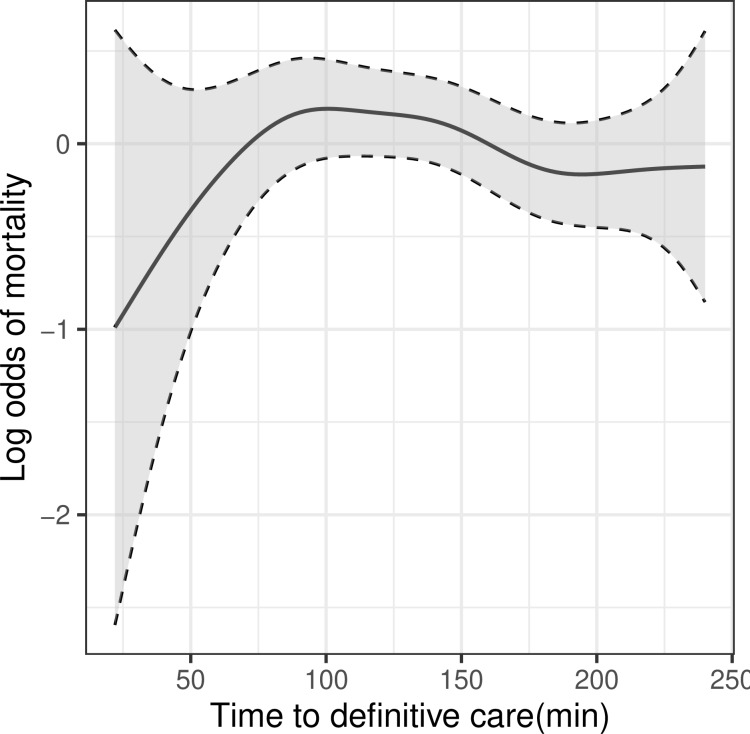
In the sensitivity analysis, 798 patients who held the record of actual onset time were identified. The association of time to definitive care with mortality was generally consistent with the main model (figure 4).
Figure 4.
Non-parametric curves of trend in log odds of in-hospital mortality with time from actual time from injury onset to definitive care using the generalized additive model (n=798). The shade bands showed 95% CI.
Discussion
In the present study, there were only a small number of patients who received definitive care within 60 min from injury, suggesting the golden hour was practically difficult to achieve in the current trauma care settings. The GAM models indicated that the trend in mortality remained stable and subsequently decreased over the time. In addition, we observed the different associations of elapsed time with mortality between severe and moderate shock patients. The former showed that time was inversely correlated with mortality. The latter showed that mortality had a time-dependent increase.
For the last three decades, there has been a debate about whether EMS providers should follow ‘scoop-and-run’ or ‘stay-and-treat’ approach in the prehospital settings.4 Only a limited number of studies in 1990s have revealed that longer prehospital time was significantly associated with increased odds of mortality in severely injured patients.11–13 Those studies have supported the concept of the golden hour. However, several studies conducted recently have demonstrated inconclusive results about the concept of the golden hour. A large cohort study by Newgard et al8 has presented that any EMS interval was not associated with mortality. Similar results were also found in other studies.14–16 In comparison, a limited number of studies have evaluated the association between in-hospital time course and mortality. Those studies also did not find the association between elapsed time in hospital and mortality.12 16 Our results did not show a significant impact of shortening time to definitive care on mortality, which was consistent with most previous studies.
The results of subgroup analysis indicated that the GAM model of all patients had a mixed result of the two curves with inverse directions in severe and moderate shock status. A paradoxical association between the elapsed time and decreased mortality was found in the severe shock group, whereas a time-dependently increase in mortality was found in the moderate shock group. The conflicting results could be partly attributed to the difference in the tolerance of patients between those two strata. SBP between 70 mm Hg and 90 mm Hg is comparable with the range of ‘permissive hypotension’ which prevents dislodgement of blood clots during resuscitation. Permissive hypotension was strongly recommended in the European guidelines (grade 1C).17In addition, a recent meta-analysis has concluded that the management of permissive hypotension had a positive effect on survival outcome.18 Therefore, one possible explanation is that providers assumed that they had a margin of time before performing definitive care for patients with permissive hypotension. However, experimental studies have reported that a positive effect of permissive hypotension on survival outcome was seen only when it was maintained for a short interval, and longer duration hypotensive resuscitation led to severe organ damage.19 20 Those studies indicated that a critical delay for hemostasis outweighed a protective effect of permissive hypotension. That could be one of the reasons for the time-dependently increase of mortality in moderate shock patients. However, the same studies suggested that severe shock status could not be tolerated even for a short interval, resulting in high mortality after hemostasis in any case.19 20
Another potential explanation of the paradoxical result in the severe shock group was a risk of residual confounding. In fact, the inverse association between time and mortality were observed among several studies.4 21–25 Conventionally, medical staff could screen severely injured patients based on their knowledge and experience. Therefore, the severity of injury might accelerate a provider’s action to transport, stabilize and initiate critical intervention with haste. Lerner et al21 have reported that patients classified as ‘critical’ or ‘unstable’ according to the subjective perception of EMS providers had shorter total prehospital time than those who were ‘stable’. Moreover, non-survivors had even shorter out-of-hospital time than survivors among the critical or unstable groups. Those findings suggested that provider’s perception of high severity hastened medical attention. In other words, the perception itself could be an important predictor of mortality, leading to confounding. Since such a factor was not be measured and adjusted, our model in patients with severe shock status also inherently contained such risk of residual confounding. In contrast, the moderate shock group was presumably less influenced by such behavior than the severe shock group.
The strength of this study is to present the effect of timeliness of hospital-based intervention on mortality. To date, a large majority of studies focused only on out-of-hospital time.4–6 8 11–16 21 22 24 26 Since the golden hour principally depends on the timeliness of critical intervention,8 27 a more cautious consideration should be paid to the in-hospital time course. We believe that this study could contribute to building a part of the evidence in both prehospital and in-hospital settings. Moreover, the non-parametric fitted curves of the GAM analysis visually demonstrated a different time trends of mortality between severe and moderate shock status. The observed differences could partly answer the question of the inexplicable results in several of the previous studies.
There were several limitations in this study. First, there was a potential residual confounding as described above. Therefore, cautious interpretation is required to apply our results to clinical settings, especially for severe shock patients. We never deny any effort to minimize time to definitive care for those patients. However, time management to reduce the time to definitive care alone might be insufficient to improve the survival outcome of those with an inherently worse prognosis. To improve this issue, the development of an innovative approach is required. Such a topic is beyond the scope of this study. Further studies are needed in the future. Second, we used EMS call activation time as a surrogate of onset time based on the past studies.5 6 8 16 21 22 It might have been different from actual time of injury onset. However, sensitivity analysis assessing around two-thirds of enrolled patients showed the similar trend, supporting the main result. Third, this study had a risk of inherent heterogeneity of the system of regional trauma care as well as several studies.8 15 16 Unfortunately, we could not identify the region where injuries occurred from the registry. However, such variability might have reflected a real-world condition. Lastly, the present study is at potential risk of another selection bias in the study population. We restricted the enrollment to those who survived for at least 4 hours to address the immortal time bias.7 Since we might have excluded patients who died before undergoing definitive care, the restriction could cause an underestimation of the effect. Conversely, we might also have missed patients who died early of a complication of definitive care, leading to an overestimation of the effect. For a better understanding, further information such as a cause of death should be assessed in the future studies.
Conclusion
We observed no association of shorter time to definitive care with a decrease in mortality of hemodynamically unstable trauma patients. However, our study indicated that patients with moderate shock could benefit from prompt time management to initiate definitive care.
Acknowledgments
We would like to thank all staff of Shock and Trauma Center in Nippon Medical School Chiba Hokusoh Hospital to help our research. We would also like to thank Japan Trauma Data Bank and all staff in institution that were participating in it.
Footnotes
Contributors: KO and ML designed the study. KO searched the literature. KO and ML conducted statistical analysis. HM critically revised the manuscript. TY and NS handled the data.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: This study was approved by the institutional review board of Nippon Medical School Chiba Hokusoh Hospital.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data may be obtained from a third party and are not publicly available. Japan Trauma Data Bank (JTDB). https://www.jtcr-jatec.org/traumabank/index.htm (in Japanese).
References
- 1.Lerner EB, Moscati RM. The golden hour: scientific fact or medical "urban legend"? Acad Emerg Med 2001;8:758–60. 10.1111/j.1553-2712.2001.tb00201.x [DOI] [PubMed] [Google Scholar]
- 2.Kidher E, Krasopoulos G, Coats T, Charitou A, Magee P, Uppal R, Athanasiou T. The effect of prehospital time related variables on mortality following severe thoracic trauma. Injury 2012;43:1386–92. 10.1016/j.injury.2011.04.014 [DOI] [PubMed] [Google Scholar]
- 3.Cowley RA. A total emergency medical system for the state of Maryland. Md State Med J 1975;24:37–45. [PubMed] [Google Scholar]
- 4.Harmsen AMK, Giannakopoulos GF, Moerbeek PR, Jansma EP, Bonjer HJ, Bloemers FW. The influence of prehospital time on trauma patients outcome: a systematic review. Injury 2015;46:602–9. 10.1016/j.injury.2015.01.008 [DOI] [PubMed] [Google Scholar]
- 5.Newgard CD, Meier EN, Bulger EM, Buick J, Sheehan K, Lin S, Minei JP, Barnes-Mackey RA, Brasel K, et al. ROC Investigators . Revisiting the "Golden Hour": An Evaluation of Out-of-Hospital Time in Shock and Traumatic Brain Injury. Ann Emerg Med 2015;66:30–41. 10.1016/j.annemergmed.2014.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Swaroop M, Straus DC, Agubuzu O, Esposito TJ, Schermer CR, Crandall ML. Pre-Hospital transport times and survival for hypotensive patients with penetrating thoracic trauma. J Emerg Trauma Shock 2013;6:16–20. 10.4103/0974-2700.106320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Andersen LW, Grossestreuer AV, Donnino MW. "Resuscitation time bias"-A unique challenge for observational cardiac arrest research. Resuscitation 2018;125:79–82. 10.1016/j.resuscitation.2018.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Newgard CD, Schmicker RH, Hedges JR, Trickett JP, Davis DP, Bulger EM, Aufderheide TP, Minei JP, Hata JS, Gubler KD, et al. Emergency medical services intervals and survival in trauma: assessment of the "golden hour" in a North American prospective cohort. Ann Emerg Med 2010;55:235–46. 10.1016/j.annemergmed.2009.07.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Figueiras A, Cadarso-Suárez C. Application of nonparametric models for calculating odds ratios and their confidence intervals for continuous exposures. Am J Epidemiol 2001;154:264–75. 10.1093/aje/154.3.264 [DOI] [PubMed] [Google Scholar]
- 10.Røislien J, Lossius HM, Kristiansen T. Does transport time help explain the high trauma mortality rates in rural areas? new and traditional predictors assessed by new and traditional statistical methods. Inj Prev 2015;21:367–73. 10.1136/injuryprev-2014-041473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sampalis JS, Lavoie A, Williams JI, Mulder DS, Kalina M. Impact of on-site care, prehospital time, and level of in-hospital care on survival in severely injured patients. J Trauma 1993;34:252–61. 10.1097/00005373-199302000-00014 [DOI] [PubMed] [Google Scholar]
- 12.Sampalis JS, Denis R, Lavoie A, Fréchette P, Boukas S, Nikolis A, Benoit D, Fleiszer D, Brown R, Churchill-Smith M, et al. Trauma care regionalization: a process-outcome evaluation. J Trauma 1999;46:565–79. 10.1097/00005373-199904000-00004 [DOI] [PubMed] [Google Scholar]
- 13.Feero S, Hedges JR, Simmons E, Irwin L. Does out-of-hospital EMS time affect trauma survival? Am J Emerg Med 1995;13:133–5. 10.1016/0735-6757(95)90078-0 [DOI] [PubMed] [Google Scholar]
- 14.Ringburg AN, de Ronde G, Thomas SH, van Lieshout EMM, Patka P, Schipper IB. Validity of helicopter emergency medical services dispatch criteria for traumatic injuries: a systematic review. Prehosp Emerg Care 2009;13:28–36. 10.1080/10903120802472012 [DOI] [PubMed] [Google Scholar]
- 15.McCoy CE, Menchine M, Sampson S, Anderson C, Kahn C. Emergency medical services out-of-hospital scene and transport times and their association with mortality in trauma patients presenting to an urban level I trauma center. Ann Emerg Med 2013;61:167–74. 10.1016/j.annemergmed.2012.08.026 [DOI] [PubMed] [Google Scholar]
- 16.Di Bartolomeo S, Valent F, Rosolen V, Sanson G, Nardi G, Cancellieri F, Barbone F. Are pre-hospital time and emergency department disposition time useful process indicators for trauma care in Italy? Injury 2007;38:305–11. 10.1016/j.injury.2006.10.005 [DOI] [PubMed] [Google Scholar]
- 17.Rossaint R, Bouillon B, Cerny V, Coats TJ, Duranteau J, Fernández-Mondéjar E, Filipescu D, Hunt BJ, Komadina R, Nardi G, et al. The European guideline on management of major bleeding and coagulopathy following trauma: fourth edition. Crit Care 2016;20:100 10.1186/s13054-016-1265-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tran A, Yates J, Lau A, Lampron J, Matar M. Permissive hypotension versus conventional resuscitation strategies in adult trauma patients with hemorrhagic shock: a systematic review and meta-analysis of randomized controlled trials. J Trauma Acute Care Surg 2018;84:802–8. 10.1097/TA.0000000000001816 [DOI] [PubMed] [Google Scholar]
- 19.Skarda DE, Mulier KE, George ME, Bellman GJ. Eight hours of hypotensive versus normotensive resuscitation in a porcine model of controlled hemorrhagic shock. Acad Emerg Med 2008;15:845–52. 10.1111/j.1553-2712.2008.00202.x [DOI] [PubMed] [Google Scholar]
- 20.Li T, Zhu Y, Hu Y, Li L, Diao Y, Tang J, Liu L. Ideal permissive hypotension to resuscitate uncontrolled hemorrhagic shock and the tolerance time in rats. Anesthesiology 2011;114:111–9. 10.1097/ALN.0b013e3181fe3fe7 [DOI] [PubMed] [Google Scholar]
- 21.Lerner EB, Billittier AJ, Dorn JM, Wu Y-WB. Is total out-of-hospital time a significant predictor of trauma patient mortality? Acad Emerg Med 2003;10:949–54. 10.1197/S1069-6563(03)00313-0 [DOI] [PubMed] [Google Scholar]
- 22.Gonzalez RP, Cummings GR, Phelan HA, Mulekar MS, Rodning CB. Does increased emergency medical services prehospital time affect patient mortality in rural motor vehicle crashes? A statewide analysis. Am J Surg 2009;197:30–4. 10.1016/j.amjsurg.2007.11.018 [DOI] [PubMed] [Google Scholar]
- 23.Ryb GE, Dischinger P, Cooper C, Kufera JA. Does helicopter transport improve outcomes independently of emergency medical system time? J Trauma Acute Care Surg 2013;74:149–56. 10.1097/TA.0b013e31827890cc [DOI] [PubMed] [Google Scholar]
- 24.Alarhayem AQ, Myers JG, Dent D, Liao L, Muir M, Mueller D, Nicholson S, Cestero R, Johnson MC, Stewart R, et al. Time is the enemy: Mortality in trauma patients with hemorrhage from torso injury occurs long before the "golden hour". Am J Surg 2016;212:1101–5. 10.1016/j.amjsurg.2016.08.018 [DOI] [PubMed] [Google Scholar]
- 25.Clarke JR, Trooskin SZ, Doshi PJ, Greenwald L, Mode CJ. Time to laparotomy for intra-abdominal bleeding from trauma does affect survival for delays up to 90 minutes. J Trauma 2002;52:420–5. 10.1097/00005373-200203000-00002 [DOI] [PubMed] [Google Scholar]
- 26.Pons PT, Haukoos JS, Bludworth W, Cribley T, Pons KA, Markovchick VJ. Paramedic response time: does it affect patient survival? Acad Emerg Med 2005;12:594–600. 10.1197/j.aem.2005.02.013 [DOI] [PubMed] [Google Scholar]
- 27.Fleet R, Poitras J. Have we killed the golden hour of trauma? Ann Emerg Med 2011;57:73–4. 10.1016/j.annemergmed.2010.08.003 [DOI] [PubMed] [Google Scholar]