Dear Editor,
Historically, fungal infections have not been considered an important influenza complication. In 2018, a retrospective multicenter cohort study in Belgium and the Netherlands identified aspergillosis in 19% of patients with severe influenza. As influenza seemed independently associated with IPA, the term influenza-associated pulmonary aspergillosis (IAPA) was introduced [1, 2]. In contrast, a single-center retrospective Canadian study reported an incidence of 7.2% [3]. Incidence seemingly varies between geographical regions and centers, but awareness among physicians may also vary. Diagnosis of IAPA is still challenging. Since culture has low sensitivity, non-culture-based diagnostic methods like galactomannan (GM) should be used [4].
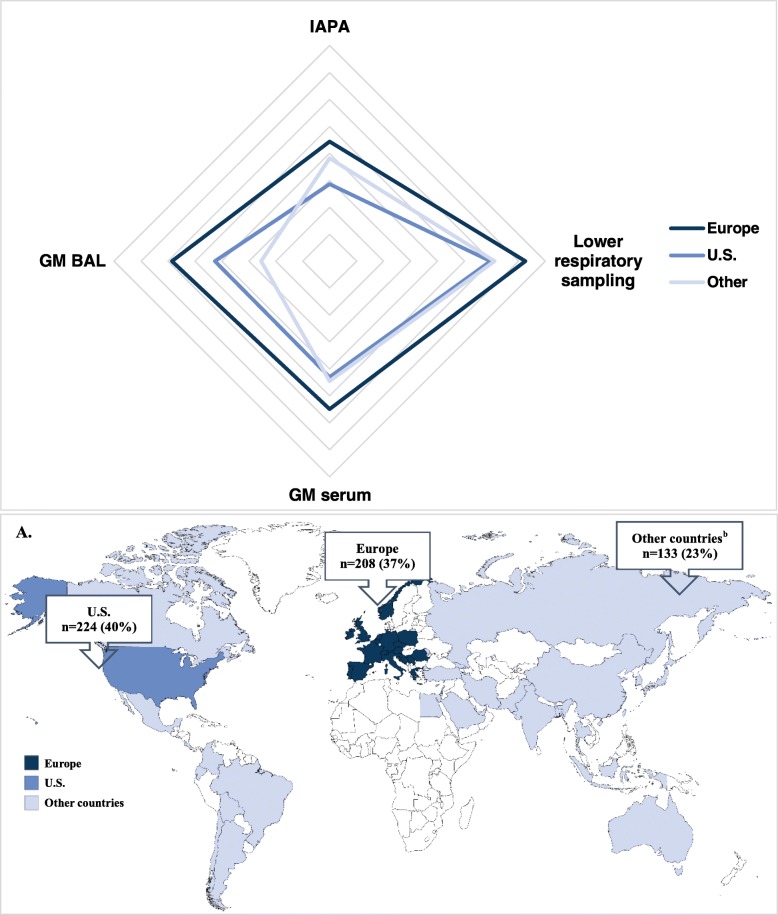
As no data exist on IAPA awareness in different parts of the world, nor on differences in clinical use of GM in broncho-alveolar lavage (BAL) or serum in critically ill influenza patients, we designed a simple survey (Table 1) and invited 20,093 members of the ELSO, SCCM, and ESICM to participate. A total of 565 responses were received, of which 90% from critical care physicians. Notably, 40% respondents were based in the US, 37% in Europe, and 22% in other continents (Fig. 1a).
Table 1.
Overview of respondent’s input based on the survey
| Responses | ||||
|---|---|---|---|---|
| Total | Europe | U.S. | Othera | |
| Valid respondents | 565 (100%) | 208 (37%) | 224 (40%) | 133 (23%) |
| Role at ICU | ||||
| Critical care physician | 509/565 (90%) | 197/208 (95%) | 186/224 (83%) | 126/133 (95%) |
| Infectious diseases physician | 8/565 (1%) | 4/208 (2%) | 3/224 (1%) | 1/133 (0.5%) |
| Nurse | 9/565 (2%) | 1/208 (1%) | 7/224 (3%) | 1/133 (0.5%) |
| Other | 39/565 (7%) | 6/208 (2%) | 28/224 (13%) | 5/133 (4%) |
| Number of ICU beds | ||||
| < 20 beds | 176/554 (32%) | 94/207 (46%) | 27/222 (12%) | 55/125 (44%) |
| 21–60 beds | 226/554 (41%) | 85/207 (41%) | 89/222 (40%) | 52/125 (42%) |
| 61–100 beds | 68/554 (12%) | 17/207 (8%) | 43/222 (19%) | 8/125 (6%) |
| > 100 beds | 84/554 (15%) | 11/207 (5%) | 63/222 (29%) | 10/125 (8%) |
| Number of severe influenza cases per season | ||||
| < 10 cases | 132/557 (23%) | 56/206 (27%) | 32/222 (14%) | 44/129 (34%) |
| 11–30 cases | 272/557 (49%) | 118/206 (57%) | 99/222 (45%) | 55/129 (43%) |
| 31–50 cases | 60/557 (11%) | 18/206 (9%) | 30/222 (14%) | 12/129 (9%) |
| > 50 cases | 49/557 (9%) | 10/206 (5%) | 27/222 (12%) | 12/129 (9%) |
| I do not know | 44/557 (8%) | 4/206 (2%) | 34/222 (15%) | 6/129 (5%) |
| NAIs as standardized treatment | ||||
| Yes | 416/556 (75%) | 162/206 (79%) | 165/222 (74%) | 89/128 (70%) |
| Yes, but only if influenza symptoms started ≤ 48–72 h before ICU admission | 97/556 (17%) | 34/206 (17%) | 41/222 (19%) | 22/128 (17%) |
| No | 27/556 (5%) | 7/206 (3%) | 3/222 (1%) | 17/128 (13%) |
| I do not know | 16/556 (3%) | 3/206 (1%) | 13/222 (6%) | 0 |
| Obtaining lower respiratory samples | ||||
| Always | 78/554 (14%) | 52/205 (25%) | 10/220 (5%) | 16/129 (12%) |
| Very often | 139/554 (25%) | 67/205 (33%) | 43/220 (19%) | 29/129 (22%) |
| Sometimes | 187/554 (34%) | 50/205 (24%) | 97/220 (44%) | 40/129 (31%) |
| Rarely | 129/554 (23%) | 31/205 (15%) | 65/220 (29%) | 33/129 (26%) |
| Never | 16/554 (3%) | 5/205 (3%) | 1/220 (1%) | 10/129 (8%) |
| N/A—have not treated patients | 5/554 (1%) | 0 | 4/220 (2%) | 1/129 (1%) |
| Galactomannan testing in BAL | ||||
| Always | 52/551 (9%) | 38/204 (19%) | 5/220 (2%) | 9/127 (7%) |
| Very often | 65/551 (12%) | 38/204 (19%) | 14/220 (6%) | 13/127 (10%) |
| Sometimes | 107/551 (19%) | 37/204 (18%) | 46/220 (21%) | 24/127 (19%) |
| Rarely | 163/551 (30%) | 43/204 (21%) | 83/220 (38%) | 37/127 (29%) |
| Never | 143/551 (26%) | 44/204 (21%) | 61/220 (28%) | 38/127 (30%) |
| N/A—have not treated patients | 21/551 (4%) | 4/204 (2%) | 11/220 (5%) | 6/127 (5%) |
| Galactomannan testing in serum | ||||
| Always | 39/554 (7%) | 28/205 (14%) | 5/220 (2%) | 6/129 (5%) |
| Very often | 60/554 (11%) | 36/205 (18%) | 11/220 (5%) | 13/129 (10%) |
| Sometimes | 115/554 (21%) | 42/205 (20%) | 46/220 (21%) | 27/129 (21%) |
| Rarely | 175/554 (31%) | 47/205 (23%) | 94/220 (43%) | 34/129 (26%) |
| Never | 142/554 (26%) | 48/205 (23%) | 51/220 (23%) | 43/129 (33%) |
| N/A—have not treated patients | 23/554 (4%) | 4/205 (2%) | 13/220 (6%) | 6/129 (5%) |
| Number of IAPA in influenza patients in the past 5 years | ||||
| No | 347/553 (63%) | 85/204 (41%) | 183/220 (83%) | 79/129 (61%) |
| Yes, 1 patient | 77/553 (14%) | 34/204 (17%) | 21/220 (9%) | 22/129 (17%) |
| Yes, 2–5 patients | 99/553 (18%) | 61/204 (30%) | 15/220 (7%) | 23/129 (18%) |
| Yes, > 5 patients | 30/553 (5%) | 24/204 (12%) | 1/220 (1%) | 5/129 (4%) |
Descriptive statistics were used to analyze the differences in proportions of responses between Europe, the US, and other countries. Fisher’s exact or χ2 test was used to calculate the p values. Correction for multiple comparisons was applied. The Spearman rank-order correlation coefficient was used to determine univariate correlations between parameters. A p value of < 0.05 was considered statistically significant. Results were analyzed using SPSS (IBM SPSS Statistics version 26). ICU intensive care unit, N/A not applicable, BAL bronchoalveolar lavage, IAPA influenza-associated pulmonary aspergillosis
aOther countries + unknown
Fig. 1.
Number of respondents and their geographical location and web diagram representing the mean response for Europe, United States and other countries. aaAustria, Belgium, Bosnia and Herzegovina, Croatia, Czech Republic, Denmark, France, Germany, Greece, Ireland, Italy, Netherlands, Norway, Poland, Portugal, Romania, Serbia, Slovenia, Spain, Switzerland, United Kingdom; bArgentina, Australia, Bangladesh, Barbados, Bolivia, Brazil, Canada, Chile, China, Colombia, Costa Rica, Ecuador, Egypt, El Salvador, Georgia, India, Indonesia, Iran, Israel, Japan, Lebanon, Malaysia, Mexico, Moldova, Pakistan, Palestine, Philippines, Russia, Saudi Arabia, South Korea, Taiwan, Thailand, Tunisia, Turkey, United Arab Emirates b Mean responses were calculated based on histograms. Subdivisions represent 0.5 arbitrary units for each of the correlation variables. For the GM BAL, GM serum and lower respiratory sampling variables, we used following units: 1 combining the categories ‘never’ and ‘rarely’; 2: sometimes; and 3 combining the categories ‘very often’ and ‘always’
The majority (72%, n = 404) of respondents reported up to 30 severe influenza cases per season. Globally, 63% (n = 347) of respondents had never heard of or seen IAPA in the past 5 years. In contrast to the US (17%, n = 37) and other countries (39%, n = 50), a majority of European participants (58%, n = 119) was familiar with IAPA.
Less than half of respondents (39%, n = 217) indicated frequent sampling of lower respiratory specimens, whereas 26% (n = 145) rarely or never performed sampling. We observed differences across different countries: European respondents performed lower respiratory sampling very often or always (58%, n = 119). This was more than the respondents in the US (24%, n = 53; p < 0.001) or those in other countries (33%, n = 45; p < 0.001).
While 39% of respondents did take lower respiratory samples, the majority of respondents (79%, n = 434) seldom determined GM in BAL. In general, GM determination in BAL/serum was more frequently reported by respondents in Europe than in the US (p < 0.01) or other countries (p < 0.01). Interestingly, both GM determination in BAL and serum correlated with the reported number of IAPA cases in all regions. Based on the calculated mean of response histograms, a web diagram was constructed, showing that a higher number of observed IAPA cases were associated with more intensive sampling (Fig. 1b).
Our results show that differences exist in awareness and diagnostic practices related to IAPA among surveyed ICU clinicians in Europe, the US, and other countries. Moreover, many clinicians were unaware of the association between influenza and aspergillosis, with European respondents having seen or heard more frequently of IAPA cases than those in the US and other countries. Although the observed differences in IAPA cases could be explained by true variation in IAPA prevalence (e.g., due to differences in environmental/genetic factors, influenza vaccination coverage, use of antiviral therapy or steroids [5, 6]), the condition might be underdiagnosed outside Europe, which is supported by lower use of GM testing on BAL or serum. Of course, these findings might not necessarily be generalizable due to the low response rate (3%). Actually, the questions were deliberately kept simple and straightforward to increase the response rate. Anyway, greater awareness of IAPA is needed as are rapid diagnostic tests. Based on the conclusions of this survey, it is clear that more multicentric prospective studies are needed to assess the incidence and risk factors for IAPA in different parts of the world, thereby taking the most updated guidelines on diagnostic and sampling practices into account, as well as the use of steroids and the consensus definitions regarding fungal infection versus colonization.
Acknowledgements
Not applicable.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of CDC.
Abbreviations
- IAPA
Influenza-associated pulmonary aspergillosis
- IPA
Invasive pulmonary aspergillosis
- GM
Galactomannan
- BAL
Broncho-alveolar lavage
- ELSO
Extracorporeal Life Support Organization
- SCCM
Society of Critical Care Medicine
- ESICM
European Society of Intensive Medicine
- US
United States
- ICU
Intensive care unit
Authors’ contributions
All authors were involved in designing the study. KT and CJ wrote the manuscript, and JW supervised the study and finalized the manuscript. MH and CJ organized the e-mail-based survey and analyzed the responses. The authors read and approved the final manuscript.
Funding
JW received a C3 grant (C32/18/043) from Industrial Research Fund, KU Leuven, Belgium, and also received a clinical FWO (Flanders Research Foundation) grant. PV received limited support of the ECCM. KT acknowledges receipt of an IOF (Industrial Research Fund) mandate of the KU Leuven.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Karin Thevissen and Cato Jacobs are shared first authors.
References
- 1.Vanderbeke L, Spriet I, Breynaert C, Rijnders BJA, Verweij PE, Wauters J. Invasive pulmonary aspergillosis complicating severe influenza. Curr Opin Infect Dis. 2018;31:471–80. [DOI] [PubMed]
- 2.Schauwvlieghe AFAD, Rijnders BJA, Philips N, Verwijs R, Vanderbeke L, Van Tienen C, et al. Invasive aspergillosis in patients admitted to the intensive care unit with severe influenza: a retrospective cohort study. Lancet Respir Med. 2018;6:782–92. [DOI] [PubMed]
- 3.Schwartz IS, Friedman DZP, Zapernick L, Dingle TC, Lee N, Sligl W, et al. High rates of influenza-associated invasive pulmonary aspergillosis may not be universal: a retrospective cohort study from Alberta, Canada. Clin Infect Dis. 2020; Available from: https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciaa007/5697276. [cited 2020 Jan 17]. [DOI] [PubMed]
- 4.Meersseman W, Lagrou K, Maertens J, Wilmer A, Hermans G, Vanderschueren S, et al. Galactomannan in bronchoalveolar lavage fluid. Am J Respir Crit Care Med. 2008;177:27–34. [DOI] [PubMed]
- 5.Krammer F, Smith GJD, Fouchier RAM, Peiris M, Kedzierska K, Doherty PC, et al. Influenza. Nat Rev Dis Prim. 2018;4:1–21. [DOI] [PMC free article] [PubMed]
- 6.Uyeki TM, Bernstein HH, Bradley JS, Englund JA, File TM, Fry AM, et al. Clinical practice guidelines by the Infectious Diseases Society of America: 2018 update on diagnosis, treatment, chemoprophylaxis, and institutional outbreak management of seasonal influenza. Clin Infect Dis. 2019;68:895–902. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.