Abstract
Background
It is not clear whether stage II colon and rectal cancer have the same risk factors for recurrence. Thus, the purpose of this study was to identify the risk factors for postoperative recurrence in stage II colorectal cancer.
Patients and methods
We retrospectively analyzed the data of 990 patients who had undergone radical surgery for stage II colorectal cancer. Patients’ pathological features and characteristics including age, sex, family history, body mass index, tumor diameter, gross type of tumor, infiltration degree (T3/T4), tumor grade, perineural invasion, vascular invasion, lymphatic invasion, pathologic examination of lymph node number, and preoperative carcinoembryonic assay (CEA) level was compared between patients with and without recurrence. Finally, the prediction of the left and right colons was analyzed.
Results
The mean ages of the colon cancer and rectal cancer patients were 69.5 years and 66.4 years, respectively. In total, 508 (82.1%) and 285 (76.8%) patients were treated laparoscopically for colon cancer and rectal cancer, respectively, with median follow-up periods of 42.2 months and 41.8 months, respectively. Forty-four recurrences occurred in both the colon cancer (7.1%) and rectal cancer (11.9%) groups. The preoperative serum CEA level and T4 infiltration were significantly higher in recurrent colorectal cancer patients. The postoperative recurrence rate of left colon cancer (descending colon, sigmoid colon) was higher than that of right colon cancer (cecum, ascending colon, transverse colon) (OR 2.191, 95% CI 1.091–4.400, P = 0.027). In COX survival factor analysis of colon cancer, the left colon is one of the independent risk factors (risk ratio 5.377, 95% CI 0.216–0.88, P = 0.02). In disease-free survival (DFS), the left colon has a relatively poor prognosis (P = 0.05). However, in the COX analysis and prognosis analysis of OS, no difference was found between the left colon and the right colon.
Conclusion
Preoperative CEA and depth of infiltration (T4) are high-risk factors associated with recurrence and are prognostic factors in stage II colorectal cancer. Left colon is also a risk factor for postoperative recurrence of stage II colon cancer.
Keywords: Colorectal cancer, Carcinoembryonic antigen, Stage II, Left colon cancer
Colorectal cancer (CRC) is one of the most common cancers and a leading cause of cancer-related death in men and women [1]. CRC is also a major cause of death in Japan, being the leading cause in women and the third most common cause in men [2]. The efficacy of adjuvant chemotherapy for stage II CRC remains controversial, although the benefit of adjuvant chemotherapy for stage III CRC has been established [3–6]. Many studies have reported that rectal cancer differs from colon cancer in etiology, genetics, clinical manifestation, anatomy, and biological characteristics [7], but it is unclear whether stage II colon and rectal cancer have the same risk factors for recurrence. The purpose of this study was to identify the risk factors for postoperative recurrence in stage II colorectal cancer.
Patients and methods
We retrospectively analyzed the clinical data of 990 patients with stage II CRC in the Division of Gastroenterological Surgery of Saitama Medical University from 2007 to 2016. The surgery was considered therapeutic when there was no macroscopic or microscopic residual cancer after surgery. There were 579 men and 411 women, comprising 619 patients with colon cancer and 371 patients with rectal cancer. Patients receiving preoperative treatment or presenting with intestinal obstruction or perforation were excluded from the analysis.
Peripheral blood samples were collected before surgery. The serum CEA level was determined by radioimmunoassay. The CEA level was considered high at ≥ 5 ng/ml. The resected specimens were pathologically classified according to the 7th edition of the Union for International Cancer Control TNM classification of malignant tumors.
All patients underwent follow up with regular physical and blood examinations, colonoscopy, and computed tomography. All statistical analyses were performed using the SPSS software package version 22.0 for Macintosh (IBM Japan, Tokyo, Japan). The significance of the correlations between the preoperative CEA level and the pathological features was analyzed using the chi-squared test for independence according to each parameter. In order to control for confounding factors, binary logistic regression was used. Wald test was used to evaluate the significance of the association. Survival curves were plotted with the Kaplan–Meier method and analyzed with a log-rank test. P < 0.05 was considered statistically significant.
Results
Clinical characteristics of CRCs
As shown in Table 1, a total of 990 CRC patients were included, comprising 371 with rectal cancer and 619 with colon cancer. The mean ages of colon cancer and rectal cancer patients were 69.5 years and 66.4 years, respectively. Of these, 508 (82.1%) of the colon cancer patients and 285 (76.8%) of the rectal cancer patients were treated laparoscopically. The median follow-up periods were 42.2 months for colon cancer and 41.8 months for rectal cancer. Forty-four recurrences occurred in both the colon cancer (7.1%) and rectal cancer (11.9%) groups. We observed significant differences between the colon and rectal cancer patients regarding sex, average age, postoperative recurrence rate, gross type, serum CEA levels, and vascular invasion (all P < 0.05). Other features were not significantly different, including open or laparoscopic methods, differentiation, invasion depth (T), perineural invasion, cancer diameter, and infiltration of lymphatic vessels.
Table 1.
Clinicopathological parameters in stage II colon and rectal cancer
| Clinicopathological Parameters | Rectal cancer | Colon cancer | P value |
|---|---|---|---|
| Gender (Total n=) | 371 (100.00%) | 619 (100.00%) | |
| Male | 245 (66.04%) | 334 (53.96%) | |
| Female | 126 (33.96%) | 285 (46.04%) | <0.01 |
| Age (year) | 66.4±0.55 | 69.5±0.42 | <0.01 |
| Post Operation Recurrence | |||
| No | 327 (88.14%) | 574 (92.73%) | |
| Yes | 44 (11.86%) | 44 (7.11%) | 0.011 |
| Open or Laparoscopic | |||
| Open | 86 (23.18%) | 113 (18.26%) | |
| Laparoscopic | 285 (76.82%) | 508 (82.07%) | 0.059 |
| Gross Type | |||
| Protruding | 18 (4.85%) | 56 (9.05%) | |
| Ulcerative & Infiltratie | 353 (95.15%) | 563 (90.95%) | 0.015 |
| Diameter (cm) | 5.44±0.11 | 5.24±0.10 | 0.105 |
| Differentiation | |||
| Well & Moderate | 354 (95.42%) | 581 (93.86%) | |
| Poor & Mucinous | 17 (4.58%) | 38 (6.14%) | 0.37 |
| T | |||
| T3 | 329 (89.648%) | 536 (87.39%) | |
| T4 | 39 (10.51%) | 78 (12.60%) | 0.324 |
| CEA (ng/mL) | |||
| <5 | 192 (51.75%) | 400 (64.62%) | |
| ≥5 | 179 (48.25%) | 219 (35.38%) | <0.01 |
| Number of dissected lymph nodes | |||
| <12 | 59 (15.90%) | 71 (11.47%) | |
| ≥12 | 312 (84.10%) | 548 (88.53%) | 0.05 |
| Perineural Invasion | |||
| No | 316 (85.18%) | 523 (84.49%) | |
| Yes | 55 (14.82%) | 96 (15.51%) | 0.77 |
| Vascular Invasion | |||
| No | 318 (85.71%) | 263 (42.49%) | |
| Yes | 53 (14.29%) | 356 (57.51%) | <0.01 |
| Infiltration lymphatic vessels | |||
| No | 312 (84.10%) | 501 (80.94%) | |
| Yes | 59 (15.90%) | 118 (19.06%) | 0.24 |
Comparisons of clinicopathological parameters between CRC recurrence and non-recurrence
Rectal cancer recurrence was associated with a body mass index greater than 25 kg/m2 (P = 0.0001), a larger tumor size (6.00 ± 0.34; P < 0.001), advanced T stage (P < 0.005), higher serum CEA levels (P < 0.002), poor differentiation or mucinous histology (P < 0.007), perineural invasion (P < 0.001), vascular invasion (P = 0.028), and infiltration of lymphatic vessels (P < 0.001) (Table 2).
Table 2.
Clinicopathological parameters for rectal cancer recurrence and non-recurrence
| Clinicopathological Parameters | Rectal Non-Recurrence | Rectal Recurrence | P value |
|---|---|---|---|
| Gender (Total n=) | 327 (100.00%) | 44 (100.00%) | |
| Male | 216 (66.06%) | 29 (65.91%) | |
| Female | 111 (33.94%) | 15 (34.09%) | 0.88 |
| Age (year) | 66.35±1.32 | 65.7±0.55 | 0.30 |
| Cancer Familly History | |||
| None | 140 (42.81%) | 22 (50.00%) | |
| Yes | 187 (57.19%) | 22 (50.00%) | 0.45 |
| BMI | |||
| <25 | 309 (94.50%) | 34 (77.27%) | |
| ≥25 | 18 (5.50%) | 10 (22.73%) | 0.0001 |
| Duplicate cancer | |||
| None | 298 (91.13%) | 38 (86.36%) | |
| Yes | 29 (8.87%) | 6 (13.64%) | 0.45 |
| Multiple Cancer | |||
| None | 308 (94.19%) | 38 (86.36%) | |
| Yes | 19 (5.81%) | 6 (13.64%) | 0.104 |
| Post Appendectomy | |||
| None | 266 (81.35%) | 37 (84.09%) | |
| Yes | 61 (18.65%) | 7 (15.91%) | 0.81 |
| Gross Type | |||
| Protruding | 20 (6.12%) | 2 (4.55%) | |
| Ulcerative & Infiltratie | 307 (93.88%) | 42 (95.45%) | 0.94 |
| Diameter (cm) | 5.42±0.11 | 6.00±0.34 | 0.045 |
| Differentiation | |||
| Well & Moderate | 316 (96.64%) | 38 (86.36%) | |
| Poor & Mucinous | 11 (3.36%) | 6 (13.64%) | 0.007 |
| T | |||
| T3 | 298 (91.15%) | 30 (68.17%) | |
| T4 | 29 (8.85%) | 14 (31.82%) | 0.005 |
| CEA (ng/mL) | |||
| <5 | 187 (57.19%) | 14 (31.82%) | |
| ≥5 | 140 (42.81%) | 30 (68.18%) | 0.002 |
| Number of dissected lymph nodes | |||
| <12 | 54 (16.51%) | 6 (13.64%) | |
| ≥12 | 273 (83.49%) | 38 (86.36%) | 0.78 |
| Perineural Invasion | (0.00%) | ||
| No | 49 (14.98%) | 37 (84.09%) | |
| Yes | 278 (85.02%) | 7 (15.91%) | <0.001 |
| Vascular Invasion | |||
| No | 118 (36.09%) | 8 (18.18%) | |
| Yes | 209 (63.91%) | 36 (81.82%) | 0.028 |
| Infiltration lymphatic vessels | |||
| No | 291 (88.99%) | 29 (65.91%) | |
| Yes | 36 (11.01%) | 15 (34.09%) | <0.001 |
Compared with rectal cancer, colon cancer recurrence was associated with just an advanced T stage (P < 0.0001) and higher serum CEA levels (P = 0.009) (Table 3).
Table 3.
Clinicopathological parameters for colon cancer recurrence and non-recurrence
| Clinicopathological Parameters | Colon Non-Recurrence | Colon Recurrence | P value |
|---|---|---|---|
| Gender (Total n=) | 575 (100.00%) | 44 (100.00%) | |
| Male | 309 (53.74%) | 24 (54.55%) | |
| Female | 266 (46.26%) | 20 (45.45%) | 0.95 |
| Age (year) | 69.7±0.43 | 70.32±1.73 | 0.35 |
| Cancer Familly History | |||
| None | 272 (47.30%) | 19 (43.18%) | |
| Yes | 303 (52.70%) | 25 (56.82%) | 0.71 |
| BMI | |||
| <25 | 448 (77.91%) | 36 (81.82%) | |
| ≥25 | 127 (22.09%) | 8 (18.18%) | 0.67 |
| Duplicate cancer | |||
| None | 493 (85.74%) | 40 (90.91%) | |
| Yes | 82 (14.26%) | 4 (9.09%) | 0.46 |
| Multiple Cancer | |||
| None | 543 (94.43%) | 42 (95.45%) | |
| Yes | 32 (5.57%) | 2 (4.55%) | 0.95 |
| Tumor location | |||
| Left colon | 278 (48.34% ) | 27( 61.37%) | |
| Right colon | 297 (51.65%) | 17 (38.63% ) | 0.09 |
| Gross Type | |||
| Protruding | 51 (8.87%) | 1 (2.27%) | |
| Ulcerative & Infiltratie | 524 (91.13%) | 43 (97.73%) | 0.21 |
| Diameter (cm) | 5.2±0.10 | 5.45±0.48 | 0.25 |
| Differentiation | |||
| Well & Moderate | 527 (91.65%) | 37 (84.09%) | |
| Poor & Mucinous | 48 (8.35%) | 7 (15.91%) | 0.15 |
| T | |||
| T3 | 511 (88.8%) | 30 (68.18%) | |
| T4 | 64 (11.2%) | 14 (31.82%) | <0.0001 |
| CEA (ng/mL) | |||
| <5 | 380 (66.09%) | 20 (45.45%) | |
| ≥5 | 195 (33.91%) | 24 (54.55%) | 0.009 |
| Number of dissected lymph nodes | |||
| <12 | 68 (11.83%) | 4 (9.09%) | |
| ≥12 | 507 (88.17%) | 40 (90.91%) | 0.76 |
| Perineural Invasion | (0.00%) | ||
| No | 494 (85.91%) | 40 (90.91%) | |
| Yes | 81 (14.09%) | 4 (9.09%) | 0.48 |
| Vascular Invasion | |||
| No | 250 (43.48%) | 13 (29.55%) | |
| Yes | 325 (56.52%) | 31 (70.45%) | 0.1 |
| Infiltration lymphatic vessels | |||
| No | 469 (81.57%) | 35 (79.55%) | |
| Yes | 106 (18.43%) | 9 (20.45%) | 0.89 |
Correlations between the preoperative CEA levels and the site of recurrence
Local recurrences were significantly more common for rectal cancers with a higher CEA level than for those with a lower CEA level (P < 0.05). However, there was no significant difference in liver metastasis, lung metastasis, or peritoneal spread between the two groups (Table 4).
Table 4.
Correlations between the preoperative CEA levels and the site of recurrence in stage II rectal cancer and colon cancer
| Rectal Cancer CEA ( ng/ml) | Colon Cancer CEA ( ng/ml) | |||||
|---|---|---|---|---|---|---|
| CEA<5 | CEA ≥5 | p-Value | CEA <5 | CEA ≥5 | p-Value | |
| n = 191 | n = 170 | n = 389 | n = 219 | |||
| Liver metastasis | ||||||
| Negative | 187 (97.91%) | 161 (94.71%) | 381 (97.94%) | 209 (95.43%) | ||
| Positive | 4 (2.09%) | 9 (5.29%) | 0.10 | 8 (2.06%) | 10 (4.57%) | 0.07 |
| Lung metastasis | ||||||
| Negative | 187 (97.91%) | 163 (95.88%) | 384 (98.71%) | 214 (97.72%) | ||
| Positive | 4 (2.09%) | 7 (4.12%) | 0.26 | 5 (1.29%) | 5 (2.28%) | 0.35 |
| Local recurrence | ||||||
| Negative | 185 (96.08%) | 157 (92.35%) | 384 (98.71%) | 213 (97.26%) | ||
| Positive | 6 (3.92%) | 13 (7.65%) | 0.028 | 5 (1.29%) | 6 (2.74%) | 0.96 |
| Peritoneal dissemination | ||||||
| Negative | 190 (99.48%) | 169 (99.41%) | 386 (99.23%) | 213 (97.26%) | ||
| Positive | 1 (0.52%) | 1 (0.59%) | 0.93 | 3 (0.77%) | 6 (2.74%) | 0.053 |
Although the patients with higher CEA levels were more likely to develop colon cancer recurrence, there was no significant difference in the site of recurrence (Table 4).
Correlations between the depth of infiltration and the site of recurrence
Local recurrences were significantly more common for colorectal cancers with T4 infiltration than for those with T3 infiltration (both P < 0.05) (Table 5). There was a higher rate of lung metastasis recurrence in patients with T4 rectal cancer compared with T3 (P = 0.004). In patients with T4 colon cancer, there was a higher rate of peritoneal metastasis (P = 0.014).
Table 5.
Correlations between the depth of infiltration and the site of recurrence in stage II rectal cancer and colon cancer
| Rectal Cancer | Colon Cancer | |||||
|---|---|---|---|---|---|---|
| T3 | T4 | p-Value | T3 | T4 | p-Value | |
| n = 332 | n = 39 | n = 542 | n = 77 | |||
| Liver metastasis | ||||||
| Negative | 320 (96.39%) | 38 (97.44%) | 526 (97.05%) | 74 (96.10%) | ||
| Positive | 12 (3.61%) | 1 (2.56%) | 0.735 | 16 (2.95%) | 3 (3.90%) | 0.651 |
| Lung metastasis | ||||||
| Negative | 325 (97.89%) | 35 (89.74%) | 535 (98.71%) | 74 (96.10%) | ||
| Positive | 7 (2.11%) | 4 (10.26%) | 0.004 | 7 (1.29%) | 3 (3.90%) | 0.089 |
| Local recurrence | ||||||
| Negative | 318 (95.78%) | 34 (87.18%) | 534 (98.52%) | 70 (90.91%) | ||
| Positive | 14 (4.22%) | 5 (12.82%) | 0.021 | 8 (1.48%) | 7 (9.09%) | <0.001 |
| Peritoneal dissemination | ||||||
| Negative | 331 (99.70%) | 38 (97.44%) | 538 (99.26%) | 74 (96.10%) | ||
| Positive | 1 (0.30%) | 1 (2.56%) | 0.067 | 4 (0.74%) | 3 (3.90%) | 0.014 |
In multivariate analysis, a higher CEA level was associated with a higher chance of recurrence of both rectal cancer (odds ratio [OR] 1.011, 95% confidence interval [95% CI] 1.00–1.021, P = 0.048) and colon cancer (OR 1.010 95% CI 1.003–1.017, P = 0.004). In addition, T4 cancer had a higher chance of recurrence in both rectal cancer (OR 3.867, 95% CI 1.547–9.663, P = 0.004) and colon cancer (OR 3.222, 95% CI 1.238–8.390, P = 0.017) (Table 6). In colon cancer, the postoperative recurrence rate of left colon cancer (descending colon, sigmoid colon) was higher than that of right colon cancer (cecum, ascending colon, transverse colon) (OR 2.191, 95% CI 1.091–4.400, P = 0.027). However, there was no significant difference between low rectal cancer and upper rectal cancer.
Table 6.
Multivariate logistic regression analysis evaluating possible risk factors associated with recurrence
| Rectal Cancer | Colon Cancer | |||||
|---|---|---|---|---|---|---|
| Odds ratio | 95% CI | p | Odds ratio | 95% CI | p | |
| Gender | 1.259 | 0.587-2.70 | 0.554 | 0.879 | 0.453- 1.704 | 0.702 |
| Age, year | 0.983 | 0.953 -1.014 | 0.270 | 1.017 | 0.985-1.050 | 0.300 |
| T4 vs T3 | 3.867 | 1.547-9.663 | 0.004 | 3.222 | 1.238-8.390 | 0.017 |
| CEA (ng/mL) | 1.011 | 1.000-1.021 | 0.048 | 1.010 | 1.003 -1.017 | 0.004 |
| Tumor location | Rb vs Ra, RS | Left colon vs Right colon | ||||
| 0.825 | 0.411- 1.651 | 0.589 | 2.191 | 1. 091-4.400 | 0.027 | |
Tumor location*: Rectal cancer (Rb & Ra, RS). Ra rectum above the peritoneal reflection, Rb rectum below the peritoneal reflection, RS rectosigmoid. Colon cancer: Left colon (Descending colon, sigmoid colon) & Right colon( Cecum, ascending colon, transverse colon)
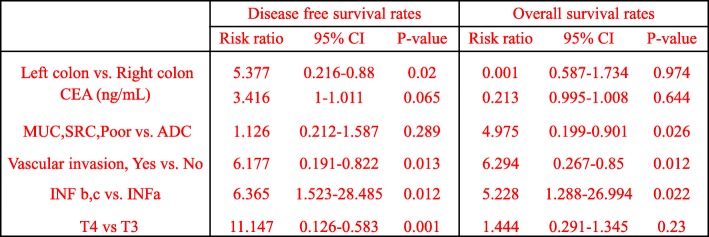
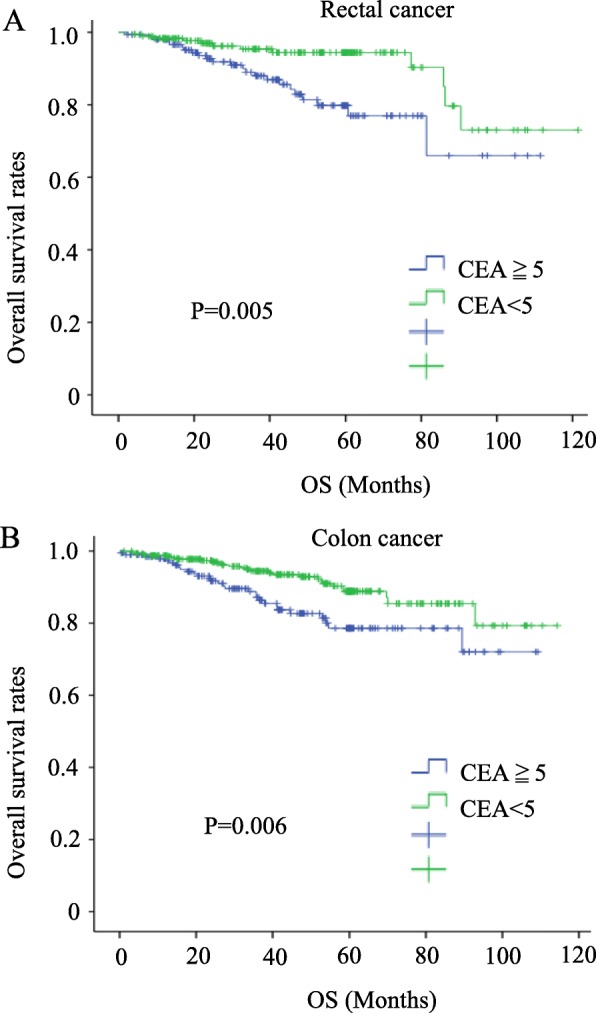
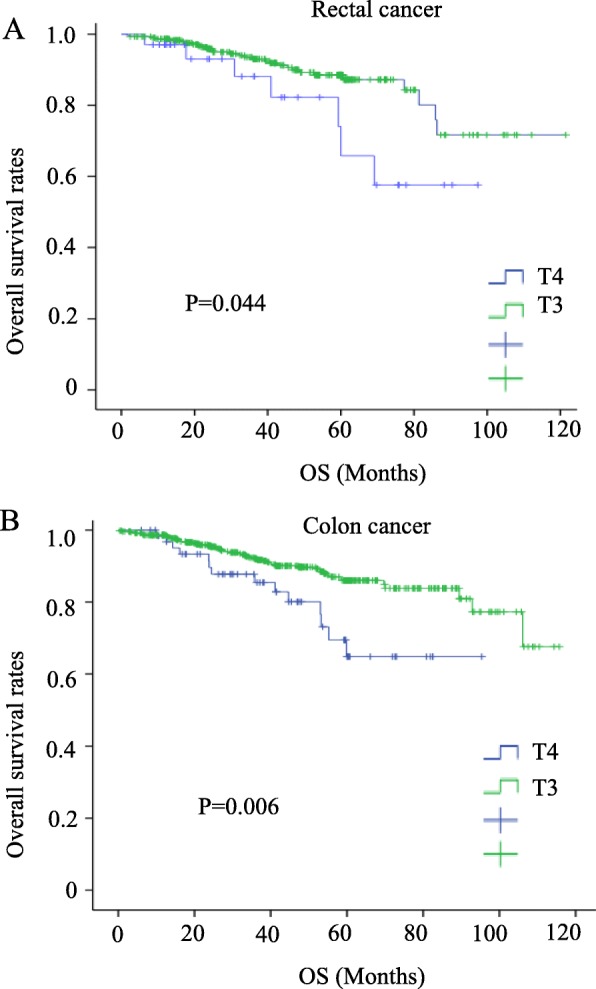
Correlations of the preoperative CEA levels and depth of infiltration with the survival rate
The overall survival rate was significantly lower in both colon and rectal cancer patients with high levels of CEA and in T4 patients (P = 0.005, 0.006, 0.0044, and 0.006, respectively) (Figs. 1a, b and 2a, b). High levels of serum CEA and T4 reduced the disease-free survival (P = 0.005, 0.001, 0.000, and 0.000) (Figs. 3a, b and 4a, b).
Fig. 1.
Survival outcomes for colorectal cancer patients with CEA ≧ 5 vs. CEA < 5
Fig. 2.
Survival outcomes for colorectal cancer patients with T3 vs. T4
Fig. 3.
Disease-free survival for colorectal cancer patients with CEA ≧ 5 vs. CEA < 5
Fig. 4.
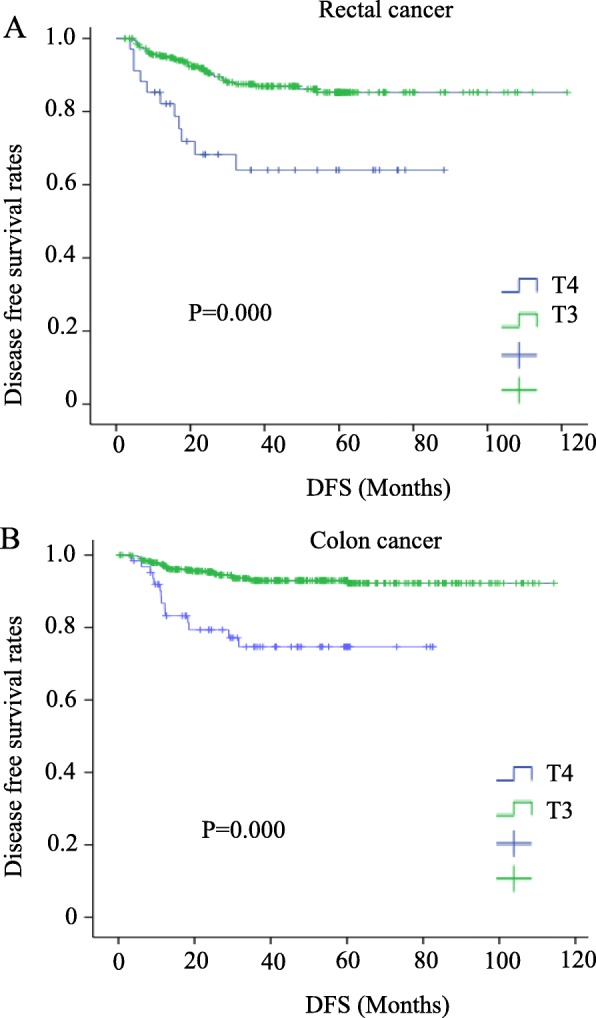
Disease-free survival for colorectal cancer patients with T3 vs. T4
Prognostic differences between the left colon and the right colon
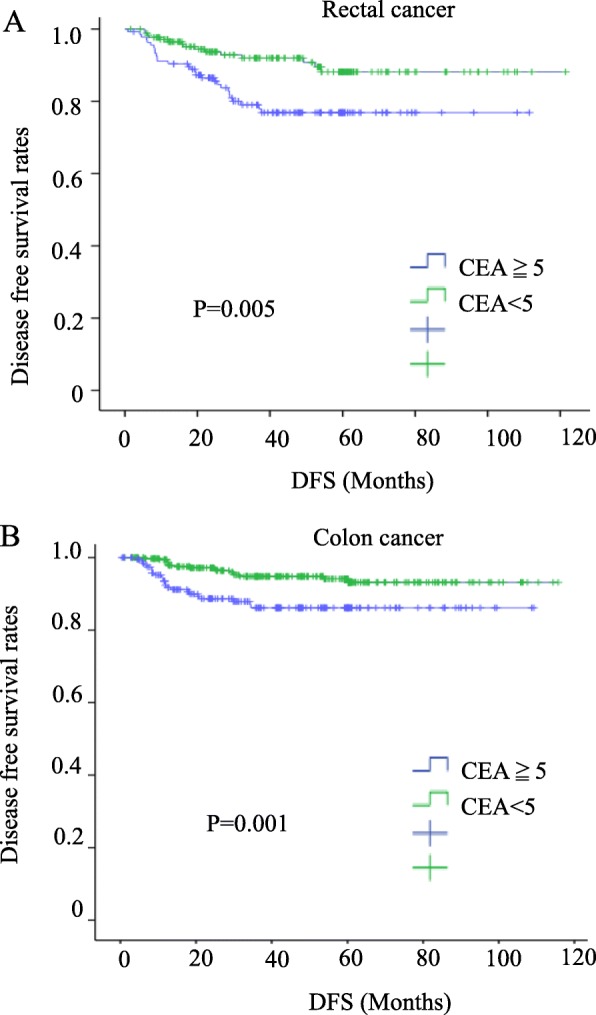
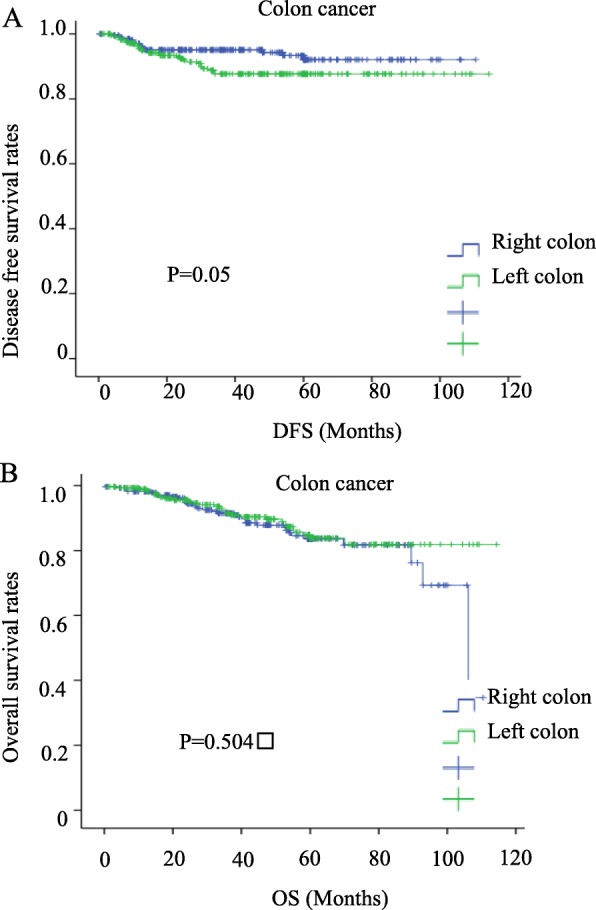
To compare the prognosis of histological parameters determined in univariate analysis, Cox’s proportional hazard regression model was applied. For DFS, left colon, vascular invasion, infiltrating pattern, and T4 were all shown to be independent risk factors. For OS, signet ring cell carcinoma, mucinous carcinoma, poorly differentiated carcinoma, vascular invasion, infiltrating pattern etc. were shown to be independent risk factors (Table 7). For the DFS Kaplan-Meier survival curve, the left colon also has a relatively poor prognosis. However, in the OS curve, there is no difference between the left colon and the right colon (Fig. 5a, b). There is no statistical difference in the ratio of T4:T3 (P = 0.337) and CEA ≥ 5 ng/ml (P = 0.32) in left colon cancer and right colon cancer (detailed data not shown).
Table 7.
Cox proportional hazard regression model comparing the effects of different parameters on the prognosis of patients with stage II Colon cancer
ADC adenocarcinoma, CEA carcinoembryonic antigen, CI confidence interval, SRC signet ring cell carcinoma, HR hazard ratio, Poor poor poorly differentiated adenocarcinoma, INF Infiltrating pattern of invasion, INFa Swelling proliferation, INF c Invasive proliferation, INF b between a and c. vs. versus, Left colon(Descending colon, sigmoid colon); Right colon( Cecum, ascending colon, transverse colon)
Fig 5.
Prognosis of left colon cancer vs. right colon cancer
Discussion
The question of whether colon and rectal cancer should be treated as a single entity or as two separate entities remains controversial [8]. The treatment of stage II CRCs has also been extensively debated [7, 9]. Our findings indicate that these two groups show considerable differences in many clinic-pathological characteristics. Significant differences were seen between the two groups in sex, average age, postoperative recurrence, gross type, surgical procedure (open/laparoscopic), serum CEA level, and vascular invasion. Therefore, our results showed that, in stage II CRC, the characteristics of colon cancer and rectal cancer were different, which is why they should be considered two separate entities.
Out of 4,244 primary CRC patients, 990 cases (23.3%) of stage II CRC were found in our hospital in the past 10 years. In view of the different characteristics of rectal cancer and colon cancer, we independently analyzed their relapse characteristics. The depth of infiltration and level of the preoperative tumor marker CEA were directly related to recurrence in the colon cancer recurrence group compared with the non-recurrence group. This is consistent with the results of another study [10]. However, rectal cancer recurrence is much more complicated. It was not only related to the serum CEA level and depth of infiltration, but also obesity, tumor size, tumor type, and postoperative pathological lymphatic infiltration and perineural invasion. Therefore, CEA level and depth of infiltration are the common factors for the recurrence of the stage II CRC. These results are largely consistent with those of another study that also found that CEA and CA19-9 were factors associated with recurrence [11, 12].
We then looked at whether CEA was associated with the site of tumor recurrence. Although CEA is a complex glycoprotein that is the most commonly used tumor marker for CRC, it is highly nonspecific. In colon cancer, we did not find any relationship between CEA and the location of tumor recurrence but it was significantly associated with the local recurrence of rectal cancer. Local recurrence of rectal cancer involves lymph nodes near the sacrum, lymph nodes around the great arteries, and lateral lymph nodes. In this study, the preoperative CEA level and depth of infiltration (T4) were risk factors and prognostic factors for recurrence of stage II colon cancer. The different biological characteristics between rectal cancer and colon cancer lead to diverse recurrence factors and prognostic factors.
We found that the incidence of postoperative recurrence for left colon cancer was higher than that of right, and left colon is one of the independent risk factors of poorer DFS, which was consistent with some reports [13, 14]. The majority of the literature differs, reporting that there is no difference [15] or that the right colon has a relatively poor prognosis [16–19]. The inclusion of the rectum in the left colon is the biggest difference between these reports. This study also shows that many biological characteristics of the colon and rectum are different. The distinction between the descending colon and the sigmoid colon from the rectum may be more conducive to future treatment.
But more surprisingly, there was no difference in OS between the left colon and the right colon. This may be because the left colon, when compared with the right colon, even though RAS/BRAF are wild-type, has more advantages in the choice of chemotherapy drugs cetuximab or panitumumab [20]. It is important to recognize the limitations of this study. The chemotherapy effect of CRC is closely related to KRAS and BRAF gene mutations or microsatellite instability (MSI) [21]. In future analysis, research on genetic components needs to be strengthened. Second, this study is a single-center retrospective study with a relatively small sample size, and we look forward to future multi-center clinical studies.
Conclusion
Our results indicate that the preoperative CEA level and depth of infiltration (T4) are high-risk factors associated with recurrence and are prognostic factors in stage II colorectal cancer. Left colon is also a risk factor for the postoperative recurrence of stage II colon cancer, and special attention should be paid during follow-up.
Acknowledgements
The authors thank the experts at BioMed Proofreading for English copy editing.
Authors’ contributions
LMW and YH drafted the manuscript and provided the original pictures. TI, HK, KH, NO, and SY reviewed the manuscript. All authors read and approved the final manuscript.
Funding
The authors declare that they have no funding.
Availability of data and materials
Not applicable
Ethics approval and consent to participate
All the study participants provided their informed consent. The study design was approved by the Ethics Committee of the Saitama Medical University International Medical Center (Number: 18-274).
Consent for publication
All patients have agreed to use their personal medical data for research and publication. Please refer to the attached file for details.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018 68(6):394-424. [DOI] [PubMed]
- 2.Watanabe T, Itabashi M, Shimada Y, Tanaka S, Ito Y, Ajioka Y, et al. Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2010 for the treatment of colorectal cancer. Int J Clin Oncol. 2012;17(1):1–29. doi: 10.1007/s10147-011-0315-2. [DOI] [PubMed] [Google Scholar]
- 3.Akiyoshi T, Kobunai T, Watanabe T. Recent approaches to identifying biomarkers for high-risk stage II colon cancer. Surg Today. 2012;42(11):1037–1045. doi: 10.1007/s00595-012-0324-4. [DOI] [PubMed] [Google Scholar]
- 4.Meyers BM, Cosby R, Quereshy F, Jonker D. Adjuvant systemic chemotherapy for stages II and III colon cancer after complete resection: a clinical practice guideline. Current oncology. 2016;23(6):418–424. doi: 10.3747/co.23.3330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Benson AB, 3rd, Schrag D, Somerfield MR, Cohen AM, Figueredo AT, Flynn PJ, et al. American Society of Clinical Oncology recommendations on adjuvant chemotherapy for stage II colon cancer. J Clin Oncol. 2004;22(16):3408–3419. doi: 10.1200/JCO.2004.05.063. [DOI] [PubMed] [Google Scholar]
- 6.Fujita S, Yamamoto S, Akasu T, Moriya Y. Outcome of patients with clinical stage II or III rectal cancer treated without adjuvant radiotherapy. Int J Colorectal Dis. 2008;23(11):1073–1079. doi: 10.1007/s00384-008-0513-1. [DOI] [PubMed] [Google Scholar]
- 7.Frattini M, Balestra D, Suardi S, Oggionni M, Alberici P, Radice P, et al. Different genetic features associated with colon and rectal carcinogenesis. Clinical cancer research : an official journal of the American Association for Cancer Research. 2004;10(12 Pt 1):4015–4021. doi: 10.1158/1078-0432.CCR-04-0031. [DOI] [PubMed] [Google Scholar]
- 8.Boyle P, Zaridze DG, Smans M. Descriptive epidemiology of colorectal cancer. Int J Cancer J Int Cancer. 1985;36(1):9–18. doi: 10.1002/ijc.2910360103. [DOI] [PubMed] [Google Scholar]
- 9.Link KH, Staib L, Kreuser ED, Beger HG. Adjuvant treatment of colon and rectal cancer: impact of chemotherapy, radiotherapy, and immunotherapy on routine postsurgical patient management. Forschungsgruppe Onkologie Gastrointestinaler Tumoren (FOGT) Recent results in cancer research Fortschritte der Krebsforschung Progres dans les recherches sur le cancer. 1996;142:311–352. doi: 10.1007/978-3-642-80035-1_19. [DOI] [PubMed] [Google Scholar]
- 10.Petersen VC, Baxter KJ, Love SB, Shepherd NA. Identification of objective pathological prognostic determinants and models of prognosis in Dukes' B colon cancer. Gut. 2002;51(1):65–69. doi: 10.1136/gut.51.1.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shibutani M, Maeda K, Nagahara H, Ohtani H, Sakurai K, Toyokawa T, et al. Significance of CEA and CA19-9 combination as a prognostic indicator and for recurrence monitoring in patients with stage II colorectal cancer. Anticancer Res. 2014;34(7):3753–3758. [PubMed] [Google Scholar]
- 12.Betge J, Langner C. Vascular invasion, perineural invasion, and tumour budding: predictors of outcome in colorectal cancer. Acta Gastroenterol Belg. 2011;74(4):516–529. [PubMed] [Google Scholar]
- 13.Leijssen LGJ, Dinaux AM, Kunitake H, Bordeianou LG, Berger DL. Pathologic factors are more important than tumor location in long-term survival in colon cancer. Int J Colorectal Dis. 2018;33(6):709–717. doi: 10.1007/s00384-018-3027-5. [DOI] [PubMed] [Google Scholar]
- 14.Moritani K, Hasegawa H, Okabayashi K, Ishii Y, Endo T, Kitagawa Y. Difference in the recurrence rate between right- and left-sided colon cancer: a 17-year experience at a single institution. Surg Today. 2014;44(9):1685–1691. doi: 10.1007/s00595-013-0748-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Qin Q, Yang L, Sun YK, Ying JM, Song Y, Zhang W, et al. Comparison of 627 patients with right- and left-sided colon cancer in China: differences in clinicopathology, recurrence, and survival. Chronic Dis Trans Med. 2017;3(1):51–59. doi: 10.1016/j.cdtm.2017.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yang KM, Park IJ, Lee JL, Yoon YS, Kim CW, Lim SB, et al. Does the different locations of colon cancer affect the oncologic outcome? A propensity-score matched analysis. Ann Coloproctol. 2019;35(1):15–23. doi: 10.3393/ac.2018.07.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee JM, Han YD, Cho MS, Hur H, Min BS, Lee KY, et al. Impact of tumor sidedness on survival and recurrence patterns in colon cancer patients. Annals of surgical treatment and research. 2019;96(6):296–304. doi: 10.4174/astr.2019.96.6.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fukata K, Yuasa N, Takeuchi E, Miyake H, Nagai H, Yoshioka Y, et al. Clinical and prognostic differences between surgically resected right-sided and left-sided colorectal cancer. Surg Today. 2019. 10.1007/s00595-019-01889-4. [DOI] [PubMed]
- 19.Ben-Aharon I, Goshen-Lago T, Sternschuss M, Morgenstern S, Geva R, Beny A, et al. Sidedness matters: surrogate biomarkers prognosticate colorectal cancer upon anatomic location. The oncologist. 2019;24(8):e696–e701. doi: 10.1634/theoncologist.2018-0351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hashiguchi Y, Muro K, Saito Y, Ito Y, Ajioka Y, Hamaguchi T, et al. Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2019 for the treatment of colorectal cancer. Int J Clin Oncol. 2020;25(1):1–42. doi: 10.1007/s10147-019-01485-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reynolds IS, Furney SJ, Kay EW, McNamara DA, Prehn JHM, Burke JP. Meta-analysis of the molecular associations of mucinous colorectal cancer. Br J Surg. 2019;106(6):682–691. doi: 10.1002/bjs.11142. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable