We are well into the third decade of a public health event marked by the greatest failure in the modern history of drug safety, sustained lethality of drug use, and epochal changes in the illicit drug market. Decades of work addressing different components of substance use have been at best greatly augmented, or at worst poorly supplanted, by complex policy regimes creating a new infrastructure for supply, demand, and harm reduction. To function well under this new structure, public health programming, including surveillance activities and other research, must explicitly define the domains with which it is concerned and its goals. The most efficient and ethical means to do this remains direct engagement and collaboration with affected communities, in particular people who use drugs.
A new study by Nesoff et al. provides a description of the spatiotemporal clustering of overdose deaths involving fentanyl or its analogs in Cook County, Illinois.1 The authors employed elegant methods, offered easy-to-understand heat maps, and confirmed that fentanyl-involved overdose clusters nearly mirrored those observed in an analysis of Chicago overdose hot spots performed in 2007.2 However, it must be noted that their study did not engage drug users in the Chicago area or long-standing programs serving this population, nor was it performed by local researchers.
BIG DATA THROUGH A LOCAL LENS
A synthesis of the Nesoff et al. results serves as an important case study in the shortcomings of omitting people who use drugs and local expertise when interpreting findings, a common omission in “big data” opioid surveillance research. The authors’ findings are not a revelation in comparison with the 2007 study. For example, the authors were unable to explain why the communities hardest hit by opioid overdoses in 2002 were nearly the same as those identified in 2014 to 2018 data, whereas a 2017 report by Chicago-area experts revealed underlying disparities and their roots.3
Content and experiential expertise among researchers results in discussion sections more robustly oriented toward solutions in research and practice. In large epidemiological studies, the input of people who use drugs may drive analyses considering complex and structural factors that influence disproportionate deaths. When a participatory approach is used, the findings can be discussed in the context of the effects of racialized drug policies, structural violence, and policing on people who use drugs, particularly people of color.
Equipped with local and experiential expertise, we offer an alternative discussion of the findings. The authors hypothesized that there is a bifurcated drug market wherein drug users in resource-deprived areas may not be able to access a fentanyl-free opioid supply. However, death data are not a suitable proxy for the overall landscape of illicit drug sale and use. In Chicago specifically, overdoses involving any illicit opioid should be considered more similar than different because fentanyl is inconsistently and unpredictably incorporated into the illicit opioid supply. Alternatively, in San Francisco, California, for example, tar heroin is rarely combined with fentanyl and fentanyl is sold separately in powder form, thus making informed consumption considerably more feasible. Thus, in Chicago during the study period as well as the fentanyl overdose spike in 2005, fentanyl-involved opioid overdoses were largely the result of individuals acquiring substances in an inconsistent heroin market.4
We disagree with the notion of a bifurcated market in Chicago through 2018; we instead propose that monitoring fentanyl-involved overdoses is important because the acuity highlights and exacerbates existing vulnerabilities. In advance of pondering a redevelopment- or gentrification-focused variation of “broken windows policing” as an approach to discourage substance use, known risks for opioid overdose should be considered. Structural violence and policing of people who use drugs directly affect overdose deaths.5 Additional indirect effects of structural violence and policing on overdose risk include chilling effects on naloxone and syringe access program participation; frequent incarceration, creating high-risk postrelease periods of low opioid tolerance; reluctance to call 911 during an overdose emergency; and slower emergency medical service response times in certain neighborhoods. These effects are seen most dramatically among people of color who use drugs and the communities in which they reside. These communities were notably featured by Nesoff et al., supporting the hypothesis that fentanyl-involved fatalities highlight existing conditions.
In their discussion, Nesoff et al. suggested investigating targeted infrastructure improvements or other community development options such as park making, building renovation, or vacant lot remediation as overdose prevention strategies. However, people who use drugs and community organizations are currently highly invested in establishing or expanding programs that have an emerging evidence base, such as safer consumption and drug checking sites, and strategies for extending proven, evidence-based interventions (e.g., naloxone access and agonist-based pharmacotherapy for opioid use disorder) to untapped social networks and resource-deprived settings.6 For example, there are two residential hotels in Chicago where at least 20 fatal overdoses have occurred in the past five years. These hotels are located within some of the most vulnerable communities identified by Nesoff et al. Their approach and findings could be used to support the siting of safer consumption and drug checking sites near or within the two hotels.
In addition, a 2018 study focusing on a safety net emergency department in Chicago revealed that only 22% of people using opioids and 2% of noninjecting opioid users had access to naloxone.7 In that study, needle exchange programs were the primary naloxone source. Geographic methods can also assist in planning where needle exchanges are sited, determining where people who use drugs via noninjection routes are located, and learning how to engage with noninjection opioid users.
REVISITING THE CHICAGO SCHOOL
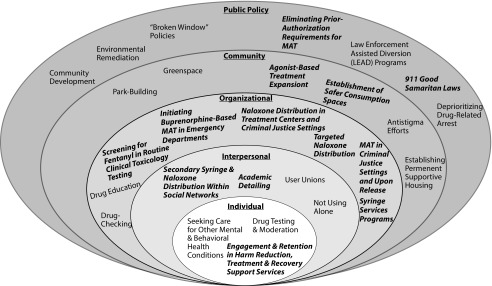
One framework that allows these diverse approaches to be well differentiated also has its roots in Chicago: the social ecological model. Under this framework, interventions acknowledge the interconnectedness of factors at all levels and include components that act at each of the levels. The proposals suggested by Nesoff et al. target the community and the different levels of public policy (Figure 1). Other harm reduction strategies that have been aggressively pursued by policymakers and community stakeholders have tended toward the middle and lower levels of the social ecological model. Although some higher-level interventions have been widely adopted (e.g., Good Samaritan laws), engagement with law enforcement–oriented programs present obvious barriers to people who use drugs.
FIGURE 1—
Social Ecological Model Diagram of Selected Interventions Designed to Reduce Opioid Overdoses
Note. MAT = medication-assisted treatment. Boldface, italicized interventions have an established evidence base.
Expanding prevention paradigms to include environmental interventions, as proposed by Nesoff et al., may provide benefits as part of a grander approach to demand reduction than has typically been considered. Ongoing psychological research is establishing the role of opioids in human social connections, building on earlier animal models. This research suggests a significant long-term role for programs profoundly altering the built and social environment, in parallel with the immediate considerations of the harm reduction movement. Such an expansive demand reduction approach may transcend the typically perceived boundaries of public health and will undoubtedly require the engagement, efforts, and leadership of individual drug users and communities.
ACKNOWLEDGMENTS
We thank Nabarun Dasgupta for enlightening discussions on the topic addressed and Ethan Foote for editorial feedback.
Note. A. A. Alexandridis is currently a postdoctoral fellow at the US Food and Drug Administration (FDA). This editorial solely reflects the views of the authors and does not necessarily represent FDA’s views or policies, nor is it related to work conducted at the FDA.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
Footnotes
See also Nesoff et al., p. 507.
REFERENCES
- 1.Nesoff ED, Branas CC, Martins SS. The geographic distribution of fentanyl-involved overdose deaths in Cook County, Illinois. Am J Public Health. 2020;110(1):98–105. doi: 10.2105/AJPH.2019.305368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Scott G, Thomas SD, Pollack HA, Ray B. Observed patterns of illicit opiate overdose deaths in Chicago, 1999–2003. J Urban Health. 2007;84(2):292–306. doi: 10.1007/s11524-007-9157-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bechteler SS, Kane-Willis K. Whitewashed: The African American Opioid Epidemic. Chicago, IL: Chicago Urban League; 2017. [Google Scholar]
- 4.Denton JS, Donoghue ER, McReynolds J, Kalelkar MB. An epidemic of illicit fentanyl deaths in Cook County, Illinois: September 2005 through April 2007. J Forensic Sci. 2008;53(2):452–454. doi: 10.1111/j.1556-4029.2008.00669.x. [DOI] [PubMed] [Google Scholar]
- 5.Bohnert ASB, Nandi A, Tracy M et al. Policing and risk of overdose mortality in urban neighborhoods. Drug Alcohol Depend. 2011;113(1):62–68. doi: 10.1016/j.drugalcdep.2010.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carroll JJ, Green TC, Noonan RK. Evidence-Based Strategies for Preventing Opioid Overdose: What’s Working in the United States: An Introduction for Public Heath, Law Enforcement, Local Organizations, and Others Striving to Serve Their Community. Atlanta, GA: Centers for Disease Control and Prevention; 2018. [Google Scholar]
- 7.Nikolaides JK, Rizvanolli L, Rozum M, Aks SE. Naloxone access among an urban population of opioid users. Am J Emerg Med. 2018;36(11):2126–2127. doi: 10.1016/j.ajem.2018.03.066. [DOI] [PubMed] [Google Scholar]