Abstract
Nuclear scintigraphy is functional imaging and can be combined with anatomical imaging to improve diagnostic yield. Detection of parathyroid lesion by technetium-99m methoxyisobutylisonitrile (Tc-99m MIBI) can facilitate an appropriate operative approach in a patients with primary hyperparathyroidism. Tc-99m MIBI is concentrated in highly cellular or metabolically active tissues, which have abundant mitochondria. False-positive scintigraphic findings could be from head-and-neck carcinomas, thyroid neoplasm, and multinodular goiter. In addition, multiple organs outside of the neck region, such as lung and breast, can take up the Tc-99m MIBI. Herein, we report the occurrence of abnormal focal uptake in the breast region during the preoperative localization of parathyroid adenoma and later discovered breast carcinoma.
Keywords: Breast neoplasms, incidental findings, parathyroid neoplasm, radionuclide imaging
INTRODUCTION
Primary hyperparathyroidism is characterized by hypercalcemia with a concomitant inappropriately elevated level of parathyroid hormone. The definitive therapy for primary hyperparathyroidism is surgery. In the era of minimally invasive surgery, parathyroid imaging has been used as preoperative tool to identify abnormal parathyroid tissue and allow the surgeon to help plan an appropriate operative approach. Ultrasound and technetium-99m methoxyisobutylisonitrile (Tc-99m MIBI) with single-photon emission computed tomography and computed tomography fusion (SPECT/CT) is the most commonly used protocol in major hospitals for the detection of parathyroid lesions. The technological advances and rapidly increasing availability of imaging modalities have led to the discovery of asymptomatic incidentalomas. We report a patient with primary hyperparathyroidism who underwent parathyroid imaging and incidentally found to have breast carcinoma detected by the Tc-99m MIBI SPECT/CT.
CASE REPORT
A 55-year-old female with primary hyperparathyroidism was referred for parathyroid scintigraphy to identify and locate the parathyroid adenoma preoperatively. The 2-hour delayed Tc-99m MIBI SPECT/CT of the neck and chest detected a small area of mild activity adjacent to the posteromedial aspect of the right upper thyroid lobe which subsequently proved to be parathyroid tissue along with multinodular goiter after right upper pole parathyroidectomy and total thyroidectomy. In addition, there was an incidental finding of a mild MIBI-avid 1.3-cm right breast nodule [Figure 1]. Further investigations including mammography and ultrasonography of the breast were performed that reported a spiculated mass about 1.5 cm × 0.7 cm in the right breast categorized as Breast Imaging-Reporting and Data System (BI-RADS) 5, highly suggestive of malignancy [Figure 2]. After confirmation of breast carcinoma by core-needle biopsy, breast-conserving surgery and sentinel lymph node biopsy followed by axillary node dissection were performed in the same setting with parathyroidectomy. Pathology of the breast mass reported invasive ductal carcinoma (grade 1) without lymphovascular invasion. One of the sentinel lymph nodes was positive. Immunohistochemistry studies of estrogen receptor, progesterone receptor, HER2/neu, and Ki-67 were positive 90%, positive 90%, negative 30%, and positive 30% of tumor nuclei, respectively. The patient received standard adjuvant therapy. No recurrence was found after 5 years of follow-up.
Figure 1.
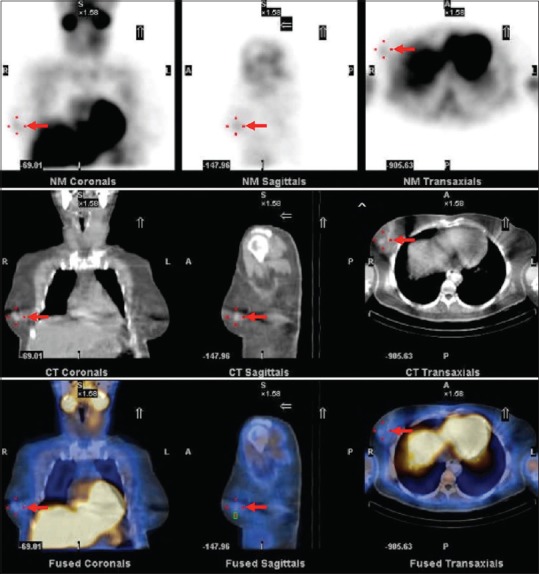
The planar images of technetium-99m methoxyisobutylisonitrile of the neck and chest (upper row) showed an incidental finding of focal uptake at right breast (arrow). Noncontrast computed tomography of the chest (middle row) demonstrated a 1.3-cm breast nodule at right breast corresponding with the technetium-99m methoxyisobutylisonitrile lesion. Further inspection of the corresponding fusion images of single-photon emission computed tomography and computed tomography (lower row) showed nonfunctioning breast nodule
Figure 2.
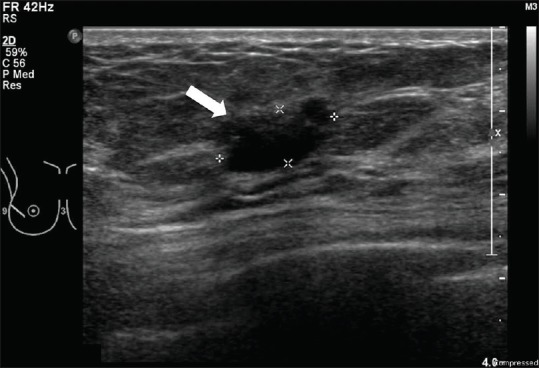
A correlative ultrasonography confirmed the presence of mass with spiculated margins, 1.5 cm × 0.7 cm at the right breast
DISCUSSION
Among the available imaging modalities, mammography is the preferred modality for early screening of breast cancer. However, mammography has limitations due to decreased sensitivity in women with dense breast tissue, limiting its utility in younger women. Ultrasonography has been reported to identify more cancers than mammography alone. Magnetic resonance imaging is recommended as an adjunct to mammography in selected high-risk patients, such as patient with BRCA1 or BRCA2 gene mutation and a history of chest radiation. Functional breast imaging techniques include breast-specific gamma imaging, positron emission tomography, and positron emission mammography. These techniques provide functional assessment of breast lesions at the cellular and metabolic level. Breast-specific gamma imaging is performed after intravenous injection of the radioisotope Tc-99m MIBI. In the past, this technique was found to be unable to detect subcentimeter cancers due to poor resolution of the detector. Currently, the development of high-resolution detector cameras have led to improved results.[1] However, breast-specific gamma imaging has not been validated as an effective screening technique in large-scale multicenter prospective studies. In addition, radiation exposure remains a significant concern. The false-positive results are common and arise from benign cellular proliferative process such as abscess, fibroadenoma, fibrocystic disease, unilateral lactating breast, papilloma, and postsurgical scar. Benign breast conditions, such as active lactation or gynecomastia, can also take up Tc-99m MIBI but appear as bilaterally homogeneous uptake.[2]
Tc-99m MIBI is a lipophilic cation that can accumulate within cytoplasmic mitochondria. Therefore, an area of highly metabolically active cancer cells can be detected. Physiologic distribution of Tc-99m MIBI is commonly seen in several organs, including thyroid, myocardium, breasts during lactation, liver, gallbladder, bowels, kidneys, and urinary bladder. It is eliminated through both urinary and hepatobiliary excretion. Although Tc-99m MIBI is widely used for the evaluation of cardiac perfusion and hyperfunctioning parathyroid gland, it might be used as a tumor-imaging agent in thyroid, parathyroid, breast, and lung cancers. There are previous case reports showing that Tc-99m MIBI could detect noncardiac or nonparathyroid abnormalities such as benign lesions,[3,4] Graves' disease, Hashimoto's thyroiditis, follicular adenoma, multinodular goiter, pneumonia, osteomyelitis, and malignant lesions[5,6,7,8,9] as breast carcinoma, esophageal carcinoma, hepatocellular carcinoma, non-Hodgkin's lymphoma, and osteosarcoma.
CONCLUSION
Although the main purpose for using Tc-99m MIBI is the evaluation of functioning parathyroid lesion or cardiac function, an incidental lesion, especially focal uptake of Tc-99m MIBI together with corresponding CT abnormality in the breast or other nontargeted organs, should not be overlooked. Appropriate precaution with adequate further investigations may lead to an earlier diagnosis and treatment of unexpected significant disease.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Hruska CB, Phillips SW, Whaley DH, Rhodes DJ, O’Connor MK. Molecular breast imaging: Use of a dual-head dedicated gamma camera to detect small breast tumors. AJR Am J Roentgenol. 2008;191:1805–15. doi: 10.2214/AJR.07.3693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gellett LR, Farmer KD, Vivian GC. Tc-99m sestamibi uptake in a patient with gynecomastia: A potential pitfall in the diagnosis of breast cancer. Clin Nucl Med. 1999;24:466. doi: 10.1097/00003072-199906000-00028. [DOI] [PubMed] [Google Scholar]
- 3.Sutter CW, Stadalnik RC. Noncardiac uptake of technetium-99m sestamibi: An updated gamut. Semin Nucl Med. 1996;26:135–40. doi: 10.1016/s0001-2998(96)80035-3. [DOI] [PubMed] [Google Scholar]
- 4.Karacavus S, Ede H, Sarikaya S, Delibas N, Kaya E, Erbay AR, et al. The importance of the incidental thyroid gland uptake during Tc-99m MIBI myocardial perfusion scintigraphy. Eur Rev Med Pharmacol Sci. 2015;19:2781–5. [PubMed] [Google Scholar]
- 5.Homma T, Manabe O, Ichinokawa K, Yamashita H, Oyama-Manabe N, Kato F, et al. Breast cancer detected as an incidental finding on 99mTc-MIBI scintigraphy. Acta Radiol Open. 2017;6:2058460117715665. doi: 10.1177/2058460117715665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kao CH, Wang SJ, Chen CY, Yeh SH. Detection of esophageal carcinoma using Tc-99m MIBI SPECT imaging. Clin Nucl Med. 1994;19:1069–74. doi: 10.1097/00003072-199419120-00007. [DOI] [PubMed] [Google Scholar]
- 7.Caner B, Kitapçl M, Unlü M, Erbengi G, Calikoǧlu T, Göǧüş T, et al. Technetium-99m-MIBI uptake in benign and malignant bone lesions: A comparative study with technetium-99m-MDP. J Nucl Med. 1992;33:319–24. [PubMed] [Google Scholar]
- 8.Sutter CW, Shelton DK. Tc-99m sestamibi uptake and retention in a large hepatoma. Clin Nucl Med. 1995;20:1091. doi: 10.1097/00003072-199512000-00013. [DOI] [PubMed] [Google Scholar]
- 9.Cohen MC, Rastegar JK, DeSilva RA, Hill TC. Demonstration of non-Hodgkin's lymphoma by dual radionuclide myocardial perfusion imaging. J Nucl Cardiol. 1996;3:186–7. doi: 10.1016/s1071-3581(96)90012-4. [DOI] [PubMed] [Google Scholar]


