ABSTRACT
Background: There is a dearth of therapeutic solutions for traumatized young patients. Trauma reactivation conducted under the influence of the reconsolidation blocker propranolol (Reconsolidation Therapy) is a simple, cost-effective treatment option that has some promising initial results in adults suffering from posttraumatic stress disorder (PTSD).
Objective: To explore the usefulness of this novel treatment in children. The primary outcome was the reduction of PTSD symptoms at the end of treatment, while secondary outcomes included reduction in anxiety and in depressive symptoms.
Method: An open-label clinical trial was conducted in a refugee camp in Syria, investigating the safety and efficacy of this therapeutic strategy in 117 children suffering from enduring PTSD symptoms. Participants received propranolol 90 minutes before briefly recalling (i.e. reactivating) a single personal traumatic memory, for 5 consecutive days. Self-reported anxiety, depressive, and PTSD symptoms were assessed at baseline, as well as 4 and 13 weeks after treatment.
Results: A significant, clinically meaningful symptom reduction was observed at all post-treatment measurement times vs. baseline. More specifically, between baseline and the 13-week follow-up we observed a 64% PTSD symptoms reduction (d = 2.71). In a similar vein, we obtained a 39% symptoms reduction for depressive symptoms (d = 1.01). The general anxiety symptoms improved, but eventually returned to prior level, probably because of the deteriorating living conditions in the camp.
Conclusions: This therapy appeared as a potentially safe and useful treatment strategy for children suffering from PTSD symptoms, warranting replication studies using stronger study designs. The social acceptability and ease of implementation of the treatment should also be noted.
KEYWORDS: Traumatic stress, propranolol, treatment, refugees, reconsolidation, war, children
Introducción: Existe una escasez de soluciones terapéuticas para pacientes jóvenes traumatizados. La reactivación del trauma conducida bajo los efectos del propanolol bloqueador de reconsolidación (Terapia de Reconsolidación) es una opción de tratamiento simple, costo-efectiva, que tiene algunos resultados iniciales prometedores en adultos que sufren del trastorno de estrés postraumático (TEPT).
Objetivos: Explorar la utilidad de este novedoso tratamiento en niños. El resultado primario fue la reducción de los síntomas de TEPT al final del tratamiento, mientras que los resultados secundarios incluyeron la reducción de los síntomas ansiosos y depresivos.
Métodos: Se condujo un estudio clínico abierto en un campo de refugiados en Siria, investigando la seguridad y eficacia de esta estrategia terapéutica en 117 niños que permanecían con síntomas de TEPT. Los participantes recibieron propranolol 90 minutos antes de recordar brevemente (es decir, reactivación) un único recuerdo personal traumático, por 5 días consecutivos. Se evaluó los síntomas de ansiedad, depresión y TEPT auto-reportados, tanto al inicio, como a las 4 y 13 semanas después del tratamiento.
Resultados: Se observó una reducción sintomática significativa, clínicamente importante en todas las mediciones post tratamiento versus el nivel basal. Más específicamente, observamos un 64% de reducción de síntomas de TEPT entre el nivel basal y el seguimiento en la semana 13 (d = 2.71). De forma similar, obtuvimos un 39% de reducción de los síntomas depresivos (d =1.01). Los síntomas generales de ansiedad mejoraron, pero retornaron a sus niveles previos al final, probablemtente por las condiciones de vida deteriorantes en el campo de refugiados.
Conclusiones: Esta terapia pareciera ser una estrategia de tratamiento potencialmente segura y útil en niños que sufren síntomas de TEPT, justificando estudios de replicación que usen diseños más estrictos. Se debería hacer notar también la aceptabilidad social y la fácil implementación del tratamiento.
PALABRAS CLAVES: Estrés traumático, niños, guerra, combinación psicoterapia-drogas, trastorno de estrés postraumático, propranolol, psicoterapia
引言: 针对遭受创伤的年轻患者的治疗方案有所欠缺。在再巩固阻滞剂普萘洛尔 (再巩固疗法) 影响下进行的创伤再激活是一种简单划算的治疗选择, 在创伤后应激障碍 (PTSD) 成年患者中取得了一些有希望的初步结果。
目标: 探究此新颖治疗方法在儿童中的有效性。主要结果是治疗结束时PTSD症状的减轻, 次要结果包括焦虑和抑郁症状的减轻。
方法: 在叙利亚一个难民营中进行了一项开放性临床试验, 考查此治疗策略对于117名有持久性PTSD症状的儿童的安全性和有效性。参与者连续5天在简要回忆 (即再激活) 个人创伤记忆的90分钟前摄入普萘洛尔。在基线及治疗后4周和13周时, 对焦虑, 抑郁和PTSD症状进行自评式评估。
结果: 与基线相比, 在治疗后所有测量时间上均观察到显著且有临床意义的症状减轻。更具体地说, 在基线和13周的随访之间, 我们观察到PTSD症状减轻了64% (d = 2.71) 。同样, 我们发现抑郁症状减轻了39% (d = 1.01) 。总体焦虑症状有所改善, 但最终恢复到之前的水平, 这可能是营地生活条件恶化所致。
结论: 对于有PTSD症状的儿童, 这种疗法似乎是一种潜在安全有效的治疗策略, 保证了更强研究设计的重复性研究。也应注意该治疗方法的社会可接受性和易于实施性。
关键词: 创伤应激, 儿童, 战争, 药物-心理治疗结合, 创伤后应激障碍, 普萘洛尔, 心理治疗
HIGHLIGHTS: • One of the few studies that investigated the effects of trauma reactivation under the influence of the reconsolidation blocker propranolol on PTSD symptoms in children.• Findings show that reconsolidation therapy led to significant symptoms improvements of PTSD, anxiety and depressive dimensions, at the end of treatment. • This study document the feasibility and the usefulness of implementing this treatment modality in a war context among refugees.
1. Introduction
Post-traumatic stress disorder (PTSD) is commonly observed in children exposed to armed conflicts, such as in Lebanon (Saigh, 1989) (current prevalence of 32.5%), Rwanda (Dyregrov, Gupta, Gjestad, & Mukanoheli, 2000) (79%), Kuwait (Nader, Pynoos, Fairbanks, al-Ajeel, & al-Asfour, 1993) (70%), Palestine (Thabet, Abu Tawahina, El Sarraj, & Vostanis, 2008) (41%), Afghanistan (Mghir, Freed, Raskin, & Katon, 1995) (34%), or Bosnia (Papageorgiou et al., 2000) (29%). Perkins, Ajeeb, Fadel, and Saleh (2018) found a high current prevalence of PTSD in children in Syria (35.1%), which has been affected by war for several years. Although reliable data concerning the Syrian conflict are missing, Soykoek, Mall, Nehring, Henningsen, and Aberl (2017) observed that a large proportion of Syrian children living in a refugee camp suffer from PTSD: 26% among 0–6 years old, and 33% among 7–14 years old. These figures are consistent with the World Health Organization’s data, which reports that 1 in 30 Syrians could develop a serious psychiatric disorder (Organisation Mondiale de la Santé, 2016). Among those, the most vulnerable populations are the young refugees, of which more than 40% may develop a psychiatric disorder, such as PTSD, depression and anxiety, according to Fazel, Wheeler, and Danesh (2005).
Besides the lack of epidemiological data, there is also a lack of empirically validated therapeutic solutions for young patients, as noted by several authors. A study by Thabet et al. established a relation between the development of PTSD in children and the parental response in armed conflict zones, as they studied it in Gaza conflict. Although the authors suggest that targeted interventions should preferably involve families, this may be hard to achieve during times of armed conflicts (Forbes et al., 2007). Salloum and Overstreet (2012) compared the efficacy of a Grief and Trauma Intervention with coping skills vs. trauma narrative processing and coping skills only, in a manualized 11-session intervention that included a meeting with the parents. Children in both treatment groups demonstrated significant long-lasting improvements in distress-related symptoms and in social support.
Today, most international guidelines for the treatment of PTSD recommend the implementation of early, evidence-based trauma-focused interventions (Diab, Isosävi, Qouta, Kuittinen, & Punamäki, 2018; Ehlers & Clark, 2003; McNally, Bryant, & Ehlers, 2003; National Collaborating Centre for Mental Health, 2005; National Institute of Mental Health, 2002; Watson & Shalev, 2005). However, there is a need for therapeutic strategies that can be effectively applied to children living in a war zone, an undeniable global public health issue according to the UNICEF (United Nations International Children’s Emergency Fund) estimating that most victims of violence in war zones are women and children (80%), and that 19.2 million refugees are displaced around the world annually, almost half of whom are children (United Nations High Commissioner for Refugees [UNHCR], 2004).
The need for new, easy to implement therapeutic methods targeting children is crucial as we currently have very few psychotherapeutic options, and psychoactive drugs are not recommended as a first line treatment (Bisson et al., 2019). Some interventions such as Eye Movement Desensitization and Reprocessing (EMDR) although recommended (Silver, Rogers, Knipe, & Colelli, 2005) are time-consuming and require extended clinical training (Sar, 2017), which is not easily implemented in a war context. Thus, alternatives with demonstrated efficacy in a context of humanitarian crisis are lacking. Exposure therapy appears to meet these broad enough feasibility criteria. Expected results are involved in the medium and long term (Foa, Rothbaum, Riggs, & Murdock, 1991; Vaughan & Tarrier, 1992). Narrative exposure therapies have already shown interesting results, as described in the study by Ruf et al. (2010), with clinically significant improvements in symptoms.
We were interested by the studies demonstrating the efficacy of brief trauma reactivation under the reconsolidation blocker propranolol in adult patients with PTSD (Brunet et al., 2008, 2018). Reconsolidation therapy, inspired by reconsolidation theory (Nader, Schafe, & Le Doux, 2000; Przybyslawski & Sara, 1997), posits that a recalled memory in certain circumstances (Ecker, 2015) becomes labile again and must be reconsolidated in order to persist. The beta-adrenergic blocker propranolol crosses the blood brain barrier, preventing the protein synthesis required to reconsolidate this emotional memory, thereby yielding a durably degraded memory trace (Besnard, Caboche, & Laroche, 2012). Reconsolidation therapy involves writing and subsequently reading a trauma narrative once a week under the reconsolidation blocker propranolol for six consecutive weeks (Brunet et al., 2011). The alleged mechanism is reconsolidation impairment. In light of this literature, we conducted an open label clinical trial. Because of constraints inherent to the test environment, the treatment included a screening session, a five-session treatment phase, a 1-month post-treatment assessment, and a 3-month follow-up. The primary outcome was the reduction of PTSD symptoms at the end of treatment, while secondary outcomes included reduction in anxiety and in depressive symptoms.
2. Methods
2.1. Study design
This open-label clinical trial was conducted in the Sejjo refugee camp in northern Syria between 09/2017 and 06/2018. The Ethics Committee of the Mother Hospital of Azaz, Syria, approved the study protocol on 08/31/2017. The parents or legal guardians gave written informed consent allowing their child to participate in the trial while the children gave oral assent. We were not able to involve Syrian fellow researchers due to the geographic location and the flight of many inhabitants. Moreover, we have not been able to develop this programme over the long term due to security issues.
2.2. Participants
Study participants were 7–14 years old treatment-seeking children, psychologically traumatized for at least 6 consecutive months by war scenes (bombs, executions, and forced displacement). The sample comprised 42% girls versus 58% boys, with 36% of children between 7–10 years old, and 64% of children between 11–14 years old. The exclusion criteria were a lifetime history of cardiovascular, respiratory or neurological disease; a medical condition contraindicating administration of propranolol such as asthma, diabetes, or arrhythmia; current substance dependence; current use of a psychotropic medication; pregnancy or breast-feeding.
Before each session, parents and patients were asked to report, according to a pre-established grid any element that could have been suggestive of a side-effect. We built the grid on the three most frequent side-effects, after introducing an open-ended question: ‘Did the patient notice anything unusual about their health after the session.’ We asked to specify if the patient had experienced any cardiac, gastroenterological, or pulmonary symptom.
A total of 170 individuals were assessed for eligibility. Nine subjects did not meet the inclusion criteria. Of the 161 eligible children, 12 withdrew their consent before treatment began, 2 refused the treatment, 16 left the refugee camp, and 14 patients did not follow the study procedures. A total of 117 patients completed the study protocol with minor or no protocol deviation, as shown in Figure 1. The mean age of the participants was 11.5 ± 2.1 years old. Children excluded from the protocol were offered art-therapy sessions and individual psychotherapy.
Figure 1.
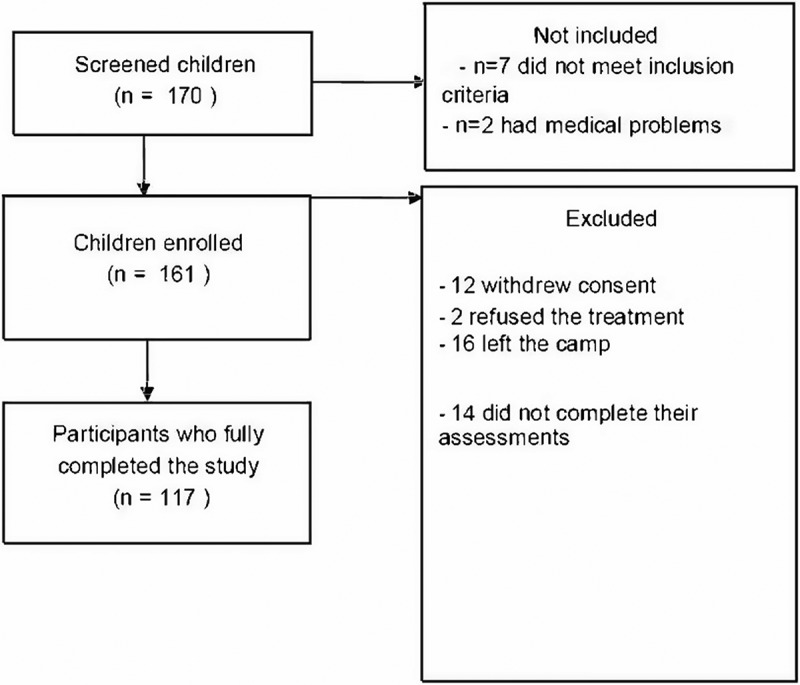
Clinical trial profile of the study.
2.3. Procedure
A meeting was organized locally, in the Sejjo refugee camp, with the parents and their children to present the study protocol and obtain informed consent from prospective participants and their parents. Following this first meeting, a group meeting was proposed to discuss any concern with parents and children and to answer different questions. At the end of this meeting, a summary of information about the protocol was provided to the families along with the consent form. A delay of 15 days following the signing of the consent form was observed before the protocol entry.
Upon protocol entry, a medical assessment was performed by an independent general practitioner to exclude participants with contraindications, and to minimize any side effect during treatment. Children who may have difficulties with treatment due to their health condition were excluded from the protocol. Eligible patients had persistent traumatic stress symptoms for at least 6 months. To be included in the study, the child had to be PTSD positive according to the Child PTSD Symptom Scale (Nader et al., 1993) (CPSS). Eligible participants underwent a pre-treatment clinical evaluation, and then 1 and 3 months (±1 week) after the end of treatment.
Assessment and treatment were conducted by two nurses and two therapists recruited as child protection officer who received a one-week training on the study protocol and procedures. During the study period, clinical supervision of the therapists was provided daily (ST).
At each session, children accompanied by their parents came to the psychological support centre to receive treatment with a therapist. Parents’ and patients’ adherence to treatment was requested at the beginning of each session and monitored by the therapists, by asking them the following question: ‘Do you agree to continue the sessions as planned?’
The families all lived in the Sejjo refugee camp. The study was implemented at a time where the camp was safe and secure far away from hostilities. Unfortunately, the area around the camp became increasingly exposed to bombings, which continued during the study period. This context probably influenced the number of patients lost to follow-up in the study, as the perception of insecurity and anxiety increased.
The question of treatment acceptability was raised before and during the study. In order to ensure acceptability, a meeting was convened with the families to present the study protocol and treatment rationale. We took the time to answer all questions. We have also provided our contact details so that families were able to contact us for further questions at all times. Above all, families were mostly concerned by their children suffering and symptoms, and were seeking reassurance about our research protocol.
2.4. Treatment
On the first treatment session, participants wrote with the help of the therapist a one-page trauma narrative in the present tense, first-person singular, focusing on the event’s most disturbing moments, and including five bodily sensations drawn from a checklist, as described elsewhere (Brunet et al., 2018). On the fourth subsequent treatment sessions, the patient read or narrated the trauma narrative once for 10–20 minutes under the influence of 1 mg/kg of long-acting (24hrs) propranolol hydrochloride – a reconsolidation blocker – given 90 minutes earlier per os. We opted to give five once-a-day treatment sessions in order to reduce participant attrition, which can be a major problem in a refugee camp. Some authors of this study (ST, LE, AB) are certified by Alain Brunet from CABA Inc. in conducting Reconsolidation TherapyTM.
2.5. Measures
Past month, DSM-5 (American Psychiatric Association, 2013) PTSD symptom severity was evaluated with the reliable and valid self-report Child PTSD Symptom Scale (Foa, Johnson, Feeny, & Treadwell, 2001) (CPSS-5), that ranges from 0 (no symptom) to 51 (maximum score). For the CPSS, we considered a threshold value of 15 or greater, as defined by the interpretation standards. Depressive symptoms were assessed using the Children’s Depression Inventory (Kovacs, 1992) (CDI), a self-rated 27-item scale applicable to children and adolescents, ranging from 0 (no symptom) to 54. The CDI cut-off is 5 for mild, 20 for moderate, and 25 for severe depression with high sensitivity and specificity. Anxiety was assessed using the validated Revised Children’s Manifest Anxiety Scale (Reynolds & Richmond, 1979) (RCMAS), a self-report instrument measuring anxiety in children and ranging from 0 (no symptom) to 28. The cut-off of RCMAS has been considered at 19 or greater. Every tests and scales were in Arabic, translated by a professional translator from Syria, and completed by the patient with the help of the parents or the legal representatives.
2.6. Statistical analyses
We used a two-sided significance level of.05 with a 95% confidence interval for all analyses. We performed descriptive and parametric statistics using Student’s t-tests. We measured treatment outcomes as the mean difference score between baseline and 1- and 3-months post-treatment assessments. The omnibus test was a repeated measures ANOVA, using Bonferroni corrections.
Patients with missing data, who refused the treatment, or who dropped-out during the protocol without having completed the questionnaires at the 1-month measurement time were excluded from the analyses (27.3%). Seven patients did not reach the threshold score at CPSS. Patients were excluded for the following reasons: epilepsy diagnosed by the paediatrician, heart problems, parents refused to give the pills to their child (n = 9), patients refused to take the pills (n = 3), families who left the camp without giving information about their departure (n = 16), and children who did not agree to complete the questionnaires (n = 14). The latter displayed weariness or nervousness, preferring activities with the other children instead of study participation. We assumed that missing data due to dropouts occurred mainly for noninformative reasons (essentially random, e.g. a study subject moves to another city with his or her family). (Hamer & Simpson, 2009) For patients who discontinued their participation, missing values were estimated using the last observation carried forward (LOCF) method. The LOCF approach is conservative and recommended when the proportion of missing data is important (> 20% dropouts).
3. Results
3.1. Group comparisons on treatment related variables
3.1.1. PTSD symptoms
As shown in Table 1, we found a significant decrease in the PTSD symptoms total score between baseline and 1-month post-treatment (−37.4%), and between 1- and 3-months follow-up (−42.4%). The total decrease between baseline and 3-months follow-up is −63.8%. This could indicate a long-lasting positive effect of the treatment on the PTSD symptoms. We also calculated effect sizes (Cohen’s d) showing a very large symptom decrease over time (d = 2.71).
Table 1.
Clinical data of the sample (n = 117).
| Baseline (B) | T1 | Cohen’s d B vs T1 |
T2 | Cohen’s d B vs T2 |
F | p | |
|---|---|---|---|---|---|---|---|
| PTSD symptomsa | |||||||
| Total score | 42.0 ± 12.7 | 26.3 ± 8.3 | 1.46 | 15.1 ± 5.9 | 2.71 | 267.62 | ** |
| Intrusion score | 12.1 ± 3.8 | 7.1 ± 2.4 | 1.57 | 4.1 ± 1.5 | 2.67 | 269.70 | ** |
| Avoidance score | 4.8 ± 2.1 | 3.1 ± 1.8 | 0.87 | 1.8 ± 1.4 | 1.69 | 93.87 | ** |
| Changes in cognition and mood score | 14.5 ± 6.1 | 9.9 ± 3.6 | 0.92 | 6.1 ± 6.1 | 1.38 | 112.46 | ** |
| Arousal and hyperreactivity score | 10.2 ± 4.7 | 6.0 ± 3.2 | 1.04 | 3.2 ± 1.7 | 2.00 | 123.04 | ** |
| Depressive symptomsb | |||||||
| Total score | 19.6 ± 9.2 | 12.3 ± 9.3 | 0.79 | 11.9 ± 5.5 | 1.01 | 36.52 | ** |
| Anxiety symptomsc | |||||||
| Total score | 15.4 ± 5.5 | 9.5 ± 6.4 | 0.99 | 13.1 ± 4.9 | 0.44 | 32.21 | ** |
| Physiological score | 5.6 ± 2.3 | 3.6 ± 2.2 | 0.89 | 4.5 ± 1.8 | 0.53 | 28.87 | ** |
| Anxiety score | 6.2 ± 2.6 | 3.7 ± 2.8 | 0.92 | 5.0 ± 2.0 | 0.52 | 29.68 | ** |
* < .05; ** < .001; SD: Standard deviation; T1: 1 month after treatment; T2: 3 months after treatment; aChild PTSD Symptom Scale (CPSS-5); bChild Depression Inventory (CDI); cRevised Children’s Manifest Anxiety Scale (RCMAS).
3.1.2. Depression symptoms
As shown in Table 1, the change in CDI scores were significant between baseline and at 1-month follow-up, with an important decrease in symptom severity (−37.2%). A significant improvement was also observed between 1- and 3-months follow-up (−3,1%), and between baseline and 3-months follow-up (−39.3%).
3.1.3. Anxiety symptoms
As shown in Table 1, the general anxiety symptoms showed a significant decrease between baseline and 1-month follow-up (−38.4%). However, we observed an increase in anxiety scores between 1- and 3-months follow-up (+37.8%). This may be explained by the fact that this is not a measure specific to PTSD symptoms, and by the poor living conditions in the camp under permanent threats of bombardments during the study period.
3.1.4. Patients lost to follow-up
We wanted to take into account the patients lost to follow-up. Thus, we conducted an analysis that simulates two possible scenarios, i.e. no change and increase in symptoms. In Scenario 1, we considered that the subjects lost to follow-up kept their symptom scores unchanged from baseline. We observed in the entire sample a significant decrease in post-traumatic stress symptoms of 27.3% between baseline and T1, and of 46.4% between baseline and T2. Depressive symptoms also decreased significantly of 26.5% between baseline and T1, and of 28.1% between baseline and T2 (Supplemental Table 1). In Scenario 2, we considered that the subjects lost to follow-up worsened their symptoms and all their scores by 10%. We reported in the entire sample a significant decrease in post-traumatic stress symptoms of 20.6% between baseline and T1, and of 40.8% between baseline and T2. Depressive symptoms declined but not significantly as we observed a decrease of 23.5% between baseline and T1, and of 14.7% between baseline and T2 (Supplemental Table 2). We observed the same pattern with anxiety symptoms.
3.2. Treatment safety
Different studies on child population indicate the absence of significant side-effects and safe use of propranolol, used for instance in the case of the nocturnal enuresis (Çaksen, Yazıcıoğlu, & Ataş, 2018), or supraventricular tachycardias (Dworkin, Bell, & Mirowski, 1973). The literature describes few sides effect like lightheadedness, visual disturbances, purpura and paraesthesia among children. We did not observe any serious side-effect of the study medication in our sample. One participant who suffered from increased anxiety was referred to the general practitioner. One child complained of mild transient neurovegetative symptoms at the end of the treatment, which lasted for 2 days. No further adverse cardiac, gastroenterological, or pulmonary experience was reported.
4. Discussion
In this protocol evaluating the usefulness of trauma reactivation under propranolol in refugee children in the context of the Syrian war, participants accepted and were compliant for the most part with the proposed treatment. They showed a very large (see Cohen’s d) mean significant symptom reduction at post-treatment and follow-up, compared to pre-treatment. Reconsolidation therapy led to significant reductions of all evaluated dimensions, namely intrusion, avoidance, mood and cognition, hypervigilance, and distress/impairment. Concerning the anxiety and depressive dimensions, significant symptoms improvements were also obtained. The results observed in this study invite us to consider the interest of this approach as worthy of further investigations in the treatment of PTSD in children. In this study, we were able to teach this treatment protocol to non-western therapists working in a warzone with a child population, a premiere. It is not so much the evaluation as the difference between the professional profiles which is interesting (nurse, therapist, psychologist …), that the personnel not trained in the general psychotherapy proper, while respecting the protocol, can accompany the patient in this therapeutic approach. These elements document the ease of implementing this treatment modality among professionals with a limited background in psychopathology and suggests that it is not culture bound from the patient perspective.
Nonetheless, this study has several limitations. First of all, as would be the case for any type of psychological treatment, implementing this type of protocol in a war context represents a major challenge and longer-term monitoring of such patients is next to impossible. A sizeable number of study participants – fourteen of them – were lost to follow-up, rendering interpretation of our study results more difficult. This question challenges the feasibility of such research protocols in the context of war contributing to increased anxiety among children.
Second, in an attempt to deal with the participants lost to follow-up, we tested two scenarios (no change and worsening of symptoms) and in the second scenario patients kept high anxiety and depression symptoms in the follow-up. However, in both scenarios we observed an improvement in the post-traumatic stress symptoms, which is encouraging.
Third, although this treatment is congruent with reconsolidation theory, it cannot be assumed that the therapeutic ingredient is necessarily or uniquely reconsolidation impairment since the study did not have the required control groups to demonstrate that. This study took place in a refugee camp and it was not ethically acceptable to propose a placebo-controlled study. Despite the numerous difficulties on the ground and the ever-growing anxiety related to bombings, we were able to conduct this study and find evidence of positive and persistent results. Such results should be replicated in future studies under improved methodological conditions. Even in these conditions, we used a personal traumatic script in which the children were able to tell their own story with their own words and beliefs. Other limiting factors are that we relied solely on self-report data, and thus lost 14 patients who did not complete their self-report assessments. A more rigorous replication study should ideally be double-blind, have a control group, and integrate objective as well as clinician-based symptom measures. In sum, this study highlights promising data and warrants replication under more stringent conditions.
Funding Statement
The funder of the study, the NGO No Lost Generation, had no role to play in the study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to the data and holds the responsibility for the decision to submit for publication the manuscript on behalf of all the co-authors.
Disclosure statement
WEH reports personal fees from EISAI, Janssen, Lundbeck, Otsuka, UCB, Roche and Chugai. He received grants from the Fondation de France, and from the French National Hospital Program for Clinical Research (PHRC), unrelated to the submitted work. No potential conflict of interest was reported by the other authors.
Supplemental data
Supplemental data for this article can be accessed here.
References
- American Psychiatric Association . (2013). Diagnostic and statistical manual of mental disorders (5th ed.). doi: 10.1176/appi.books.9780890425596 [DOI] [Google Scholar]
- Besnard, A., Caboche, J., & Laroche, S. (2012). Reconsolidation of memory: A decade of debate. Progress in Neurobiology, 99(1), 61‑80. [DOI] [PubMed] [Google Scholar]
- Bisson, J. I., Berliner, L., Cloitre, M., Forbes, D., Jensen, T. K., Lewis, C., … Shapiro, F. (2019). The international society for traumatic stress studies new guidelines for the prevention and treatment of posttraumatic stress disorder: Methodology and development process. Journal of Traumatic Stress, 32(4), 475–8. [DOI] [PubMed] [Google Scholar]
- Brunet, A., Orr, S. P., Tremblay, J., Robertson, K., Nader, K., & Pitman, R. K. (2008). Effect of post-retrieval propranolol on psychophysiologic responding during subsequent script-driven traumatic imagery in post-traumatic stress disorder. Journal of Psychiatric Research, 42, 503–506. [DOI] [PubMed] [Google Scholar]
- Brunet, A., Poundja, J., Tremblay, J., Bui, E., Thomas, E., Orr, S. P., … Pitman, R. K. (2011). Trauma reactivation under the influence of propranolol decreases posttraumatic stress symptoms and disorder : 3 open-label trials. Journal of Clinical Psychopharmacology, 31(4), 547‑550. [DOI] [PubMed] [Google Scholar]
- Brunet, A., Saumier, D., Liu, A., Streiner, D. L., Tremblay, J., & Pitman, R. K. (2018). Reduction of PTSD symptoms with pre-reactivation propranolol therapy: A randomized controlled trial. American Journal of Psychiatry, 175(5), 427‑433. [DOI] [PubMed] [Google Scholar]
- Çaksen, H., Yazıcıoğlu, P., & Ataş, B. (2018). Use of propranolol in children with primary nocturnal enuresis. Sudan Journal of Paediatrics, 18(2), 33–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diab, S. Y., Isosävi, S., Qouta, S. R., Kuittinen, S., & Punamäki, R. L. (2018). The protective role of maternal posttraumatic growth and cognitive trauma processing among Palestinian mothers and infants. Infant Behavior and Development, 50, 284‑299. [DOI] [PubMed] [Google Scholar]
- Dworkin, P., Bell, B., & Mirowski, B. (1973). Propranolol in supraventricular tachycardias of childhood. Archives of Disease in Childhood, 48(5), 382–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyregrov, A., Gupta, L., Gjestad, R., & Mukanoheli, E. (2000). Trauma exposure and psychological reactions to genocide among Rwandan children. Journal of Traumatic Stress, 13(1), 3‑21. [DOI] [PubMed] [Google Scholar]
- Ecker, B. (2015). Memory reconsolidation understood and misunderstood. International Journal of Neuropsychotherapy, 3, 2–46. [Google Scholar]
- Ehlers, A., & Clark, D. (2003). Early psychological interventions for adult survivors of trauma : A review. Biological Psychiatry, 53(9), 817‑826. [DOI] [PubMed] [Google Scholar]
- Fazel, M., Wheeler, J., & Danesh, J. (2005). Prevalence of serious mental disorder in 7 000 refugees resettled in western countries: A systematic review. Lancet, 365(9467), 1309‑1314. [DOI] [PubMed] [Google Scholar]
- Foa, E. B., Johnson, K. M., Feeny, N. C., & Treadwell, K. R. (2001). The child PTSD symptom scale : A preliminary examination of its psychometric properties. Journal of Clinical Child Psychology, 30(3), 376‑384. [DOI] [PubMed] [Google Scholar]
- Foa, E. B., Rothbaum, B. O., Riggs, D. S., & Murdock, T. B. (1991). Treatment of posttraumatic stress disorder in rape victims : A comparison between cognitive-behavioral procedures and counseling. Journal of Consulting and Clinical Psychology, 59(5), 715‑723. [DOI] [PubMed] [Google Scholar]
- Forbes, D., Creamer, M., Phelps, A., Bryant, R., McFarlane, A., Devilly, G. J., … Newton, S. (2007). Australian guidelines for the treatment of adults with acute stress disorder and post-traumatic stress disorder. Australian and New Zealand Journal of Psychiatry, 41(8), 637‑648. [DOI] [PubMed] [Google Scholar]
- Hamer, R. M., & Simpson, P. M. (2009). Last observation carried forward versus mixed models in the analysis of psychiatric clinical trials. American Journal of Psychiatry, 166(6), 639–641. [DOI] [PubMed] [Google Scholar]
- Kovacs, M. (1992). Children’s depression inventory. North Tonawanda, NY: Multi-Health System. [Google Scholar]
- McNally, R. J., Bryant, R. A., & Ehlers, A. (2003). Does early psychological intervention promote recovery from posttraumatic stress? Psychological Science in the Public Interest, 4(2), 45‑79. [DOI] [PubMed] [Google Scholar]
- Mghir, R., Freed, W., Raskin, A., & Katon, W. (1995). Depression and posttraumatic stress disorder among a community sample of adolescent and young adult Afghan refugees. Journal of Nervous and Mental Disease, 183(1), 24‑30. [DOI] [PubMed] [Google Scholar]
- Nader, K., Schafe, G. E., & Le Doux, J. E. (2000). Fear memories require protein synthesis in the amygdala for reconsolidation after retrieval. Nature, 406(6797), 722‑726. [DOI] [PubMed] [Google Scholar]
- Nader, K. O., Pynoos, R. S., Fairbanks, L. A., al-Ajeel, M., & al-Asfour, A. (1993). A preliminary study of PTSD and grief among the children of Kuwait following the Gulf crisis. British Journal of Clinical Psychology, 32(4), 407–416. [DOI] [PubMed] [Google Scholar]
- National Collaborating Centre for Mental Health . (2005). Post-traumatic stress disorder: The management of PTSD in adults and children in primary and secondary care. Leicester, UK: Gaskell. [PubMed] [Google Scholar]
- National Institute of Mental Health . (2002). Mental health and mass violence: Evidence-based early psychological intervention for victims/survivors of mass violence: A workshop to reach consensus on best practices. Washington: Government Print Office. [Google Scholar]
- Organisation Mondiale de la Santé . (2016). Guérir les blessures invisibles dues au conflit syrien. Bulletin de l’Organisation Mondiale de la Santé, 94, 6–7. [Google Scholar]
- Papageorgiou, V., Frangou-Garunovic, A., Iordanidou, R., Yule, W., Smith, P., & Vostanis, P. (2000). War trauma and psychopathology in Bosnian refugee children. European Child and Adolescent Psychiatry, 9(2), 84‑90. [DOI] [PubMed] [Google Scholar]
- Perkins, J. D., Ajeeb, M., Fadel, L., & Saleh, G. (2018). Mental health in Syrian children with a focus on post-traumatic stress : A cross-sectional study from Syrian schools. Social Psychiatry and Psychiatric Epidemiology, 53(11), 1231‑1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Przybyslawski, J., & Sara, S. J. (1997). Reconsolidation of memory after its reactivation. Behavioural Brain Research, 84(1–2), 241–246. [DOI] [PubMed] [Google Scholar]
- Reynolds, C. R., & Richmond, B. O. (1979). Factor structure and construct validity of ’What I think and feel’: The revised children’s manifest anxiety scale. Journal of Personality Assessment, 43(3), 281‑283. [DOI] [PubMed] [Google Scholar]
- Ruf, M., Schauer, M., Neuner, F., Catani, C., Schauer, E., & Elbert, T. (2010). Narrative exposure therapy for 7- to 16-year-olds: A randomized controlled trial with traumatized refugee children. Journal of Traumatic Stress, 23(4), 437–445. [DOI] [PubMed] [Google Scholar]
- Saigh, P. A. (1989). The validity of the DSM-III posttraumatic stress disorder classification as applied to children. Journal of Abnormal Psychology, 98(2), 189‑192. [DOI] [PubMed] [Google Scholar]
- Salloum, A., & Overstreet, S. (2012). Grief and trauma intervention for children after disaster : Exploring coping skills versus trauma narration. Behaviour Research and Therapy, 50(3), 169‑179. [DOI] [PubMed] [Google Scholar]
- Sar, V. (2017). Post-traumatic stress in terror and war. Okmeydani Hospital Medical Journal, 33, 114‑120. [Google Scholar]
- Silver, S., Rogers, S., Knipe, J., & Colelli, G. (2005). EMDR therapy following the 9/11 terrorist attacks : A community-based intervention project in New York city. International Journal of Stress Management, 12, 29‑42. [Google Scholar]
- Soykoek, S., Mall, V., Nehring, I., Henningsen, P., & Aberl, S. (2017). Post-traumatic stress disorder in Syrian children of a German refugee camp. Lancet, 389(10072), 903‑904. [DOI] [PubMed] [Google Scholar]
- Thabet, A. A., Abu Tawahina, A., El Sarraj, E., & Vostanis, P. (2008). Exposure to war trauma and PTSD among parents and children in the Gaza strip. European Child and Adolescent Psychiatry, 17(4), 191‑199. [DOI] [PubMed] [Google Scholar]
- United Nations High Commissioner for Refugees (UNHCR) . (2004). Global refugee trends. Overview of refugee populations, new arrivals, durable solutions, stateless and other persons of concern to UNHCR. Geneva: UNHCR. [Google Scholar]
- Vaughan, K., & Tarrier, N. (1992). The use of image habituation training with post-traumatic stress disorders. British Journal of Psychiatry, 161, 658‑664. [DOI] [PubMed] [Google Scholar]
- Watson, P. J., & Shalev, A. Y. (2005). Assessment and treatment of adult acute responses to traumatic stress following mass traumatic events. CNS Spectrum, 10(2), 123‑131. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


