Abstract
Background
Depression is common in patients with inflammatory bowel disease (IBD) and contributes to poor quality of life (QoL). The use of information technology for the remote management of patients with IBD is growing, but little is known about its impact on depressive symptoms (DS) and QoL. We aimed to evaluate the impact of telemedicine on DS and generic QoL in IBD patients.
Methods
We analyzed data from the Telemedicine for Patients with IBD (TELE-IBD) study. During this 12-month clinical trial, patients were randomized to receive text message-based telemedicine weekly (TELE-IBD W), every other week (TELE-IBD EOW), or to standard care. Depressive symptoms and QoL were assessed over time with the Mental Health Inventory 5 (MHI-5) and the Short Form 12 (SF-12), respectively. We compared the change in MHI-5 and SF-12 (with separate physical (PCS) and mental component summary (MCS) scores) between the study arms.
Results
A total of 217 participants were included in this analysis. After 1 year, there was no significant difference in the change in MHI-5 (TELE-IBD W +3.0 vs TELE-IBD EOW +0.7 vs standard care +3.4; P = 0.70), MCS (TELE-IBD W +1.4 vs TELE-IBD EOW +1.0 vs standard care +2.5; P = 0.89), and PCS scores (TELE-IBD W +0.4 vs TELE-IBD EOW +0.6 vs standard care +3.7; P = 0.06) between the groups.
Conclusions
Text message-based telemedicine does not improve DS or QoL when compared with standard care in IBD patients treated at tertiary referral centers. Further studies are needed to determine whether telemedicine improves DS or QoL in settings with few resources.
Keywords: quality of life, depression, telemedicine, text message, inflammatory bowel disease
INTRODUCTION
Patients with inflammatory bowel disease (IBD) suffer from a chronic gastrointestinal condition that is marked by periods of exacerbation, with symptoms ranging from abdominal pain, diarrhea, and extra-intestinal manifestations. Comprised of ulcerative colitis (UC) and Crohn disease (CD), IBD affects about 3 million people in the United States and exerts a negative impact on the overall well-being of affected persons.1, 2 A significant proportion of patients are diagnosed in their youth and will have to contend with a lifetime of complex medical and surgical therapies for their disease and its complications.3 IBD patients have a higher-than-average rate of emergency room visits and hospitalizations and have considerable lost earnings from loss of productivity related to their disease.4–6 The experience of IBD exerts a particularly heavy toll on the mental health and quality of life of affected individuals.7–9 In a recent population-based study in the US, IBD was found to be independently associated with depressive symptoms (DS).10 About 49% of the IBD patient population was shown to have DS compared with 23% of the non-IBD population, with almost a quarter of them having an increase in suicidal ideation. Because of the sometimes severe mental, physical, and psychosocial consequences of IBD, patients’ perception of their illness and overall life satisfaction is deeply impacted in a negative manner. The quality of life (QoL) of patients with IBD has consistently been shown to be poor when compared to the general population.11–13
The interplay of depression with IBD is complex, with a bi-directional pathway ascribed to this relationship.14 On the one hand, the experience of the physical and physiologic processes of the disease increases the perceived stress of affected persons and, in turn, increases their risk of depression.15 On the other hand, co-existing depression has been shown to predict worse IBD outcomes, with an increase in the likelihood of exacerbations, a decrease in response to treatment, an increase in the risk of surgery, and a greater likelihood of hospital readmission.16–19 As a matter of practicality, the financial burden of depression in IBD patients is also of a major concern. In a US-based study of a national administrative claims database, depression was associated with an increase in mean annual IBD-related cost of $17,706 per patient.20 For these reasons, interventions and practices that can reduce the burden of depression in IBD patients and improve QoL are of urgent public health interest.
In the last two decades, there has been a gradual shift in the mechanism of IBD care delivery due to the introduction of telemedicine in lieu of the in-person encounters of traditional clinical practice. Defined as the use of information technology for remote healthcare delivery, telemedicine has been shown to have high acceptance amongst IBD patients and has important benefits for health systems.21, 22 It has served as a bridge to increase access to subspecialty care and has been shown to lead to a reduction in healthcare utilization and costs, to improve adherence to therapies, and to decrease disease activity.23–25 As the use of telemedicine gains wider acceptance in these times of rapid advancement in communication technology, it is crucial to understand its effect on the key patient-reported measures of depression and QoL. This knowledge can guide the appropriate use of telemedicine and inform future related investments in the IBD population. Published studies in this area have been focused on web-based telemedicine interventions and have had mixed results.23–27 Investigators from our group had previously reported that there was no significant change in disease-specific QoL amongst patients managed via text-message telemedicine, but we wondered whether this was the same for generic QoL.28 In contrast to disease-specific QoL, generic QoL reflects a more holistic assessment of the psychosocial/emotional well-being and the physical functioning of patients.29 Generic QoL measures also enable comparisons of interventions across multiple diseases and conditions, and is beneficial in healthcare service planning.30 Using valid instruments, we compared the change in DS and generic QoL scores over 12 months in IBD patients who received text message-based telemedicine vs standard care in the TELEmedicine for Patients with Inflammatory Bowel Disease (TELE-IBD) trial. We hypothesized that there will be an improvement in DS and generic QoL scores in IBD patients managed with telemedicine compared with the standard care.
METHODS
Study Design and Eligibility
We analyzed data of participants in the TELE-IBD trial – a randomized controlled trial comparing telemedicine to standard care for IBD patients over 12 months. The design and findings of the TELE-IBD trial have previously been reported (Clinicaltrials.gov identifier: NCT01692743).28, 31 The aim of the present analysis was to evaluate the effect of telemedicine on DS and generic QoL in patients with IBD. Participants in the TELE-IBD trial were recruited from 3 university medical centers in the United States: University of Maryland (UMB), University of Pittsburgh Medical Center (UPMC), and Vanderbilt University (VU). They were randomized in a 1:1:1 fashion to standard care, or to receive text-message-based telemedicine weekly (TELE-IBD W) or every other week (TELE-IBD EOW). To be eligible for inclusion in the TELE-IBD trial, patients had to have documented IBD on the basis of usual diagnostic criteria, be 18 years or older, and have had at least one flare of active IBD within the preceding 2 years.32 Exclusion criteria included the following: inability to speak and/or read English; inability to comply with study protocol; presence of any ostomy, ileo-anal pouch anastomosis, or ileo-rectal anastomosis; imminent surgery; history of short bowel syndrome; uncontrolled medical or psychiatric disease; and/or pregnancy. For the present analysis, only participants that completed the study and had complete DS and generic QoL scores at baseline and at the 12-month study visit were included.
The TELE-IBD system was designed for bidirectional communication between patients and healthcare providers via text messaging only. Participants who were randomized to one of the telemedicine arms received text-message prompts on a weekly basis or every other week to respond to a set of questions designed to evaluate their clinical well-being. They were asked about the presence and characteristics of specific IBD-associated symptoms such as abdominal pain, stool frequency, and the presence of blood in stool. They were also provided with electronic scales at the start of the study and were prompted during self-testing sessions to report on their body weight. Additionally, they were queried on the occurrence of medication-related adverse effects. The provider-initiated prompts were presented in a multiple choice or scale format for ease of administration via text messaging.
On the other end of the TELE-IBD system, healthcare providers had access to a secure decision support server and a website that was continuously populated with patient clinical data after the weekly or biweekly patient testing sessions. Depending on participant responses, they were classified after each session by disease severity and appropriate care was provided. Customized management plans were conveyed to individual participants and this was received via text message. For those in the standard care arm, which served as the control group, they continued to follow with their regular IBD provider at in-person office visits. While the telemedicine patients were monitored via text message, they continued to follow up regularly with their provider and could contact office staff via telephone or electronic messaging. Over the 1-year study period, all participants were expected to have study visits at baseline and then at 6 and 12 months. At these study visits, participants completed health surveys to assess multiple clinical, psychosocial, and behavioral indices. Informed consent was obtained from all study participants before the start of the study. The protocol for this study was approved by the Human Subjects Research Protection Office at all three participating sites.
Outcomes and Covariates
The study outcomes were DS and generic QoL. These were evaluated using the Mental Health Index 5 (MHI-5) scale and the Short Form-12 Questionnaire (SF-12), respectively, at baseline, 6 and 12 months. The MHI-5 is a self-reported and validated measure of DS that is comprised of a 5-question subscale of the Short Form 36 (SF-36).33 While having the advantage of brevity, the MHI-5 can reliably detect and screen for mood and anxiety disorders.34 Answers to questions are graded on a Likert scale, and a responder’s final score ranges between 0 and 100. A lower score correlates with more severe depressive symptoms.35, 36
The SF-12 is a subscale of the SF-36 that is validated for use in measuring generic QoL.37 Questions are drawn from eight health concepts of the SF-36 for a total of 12 survey items. The SF-12 is easy to administer and the concepts assessed are physical functioning, role-physical, role-emotional, mental health, bodily pain, general health, vitality, and social functioning. It provides both a Physical Component Summary score (PCS) and Mental Component Summary score (MCS) for each subject.38, 39 The PCS and MCS scores each range from 0 to 100, with higher scores signifying a feeling of better general health.40
Data on multiple sociodemographic, clinical, and laboratory co-variates were also collected at the study visits. Disease activity was measured using the Harvey Bradshaw Index (HBI) and the Simple Clinical Colitis Activity Index (SCCAI) in patients with CD and UC, respectively.41, 42 Laboratory data collected at study visits included C-reactive protein, a complete blood count, and a comprehensive metabolic profile. Disease-specific QoL was measured using the IBD Questionnaire (IBDQ).43
Statistical Analysis
Categorical variables were expressed as proportions, and means and standard deviations were calculated for continuous variables. The three exposure groups were compared with regards to their baseline socio-demographic and clinical characteristics, using the one-way analysis of variance and the Pearson’s chi-square tests for continuous and categorical variables, respectively. A paired t-test was used to compare the change in MCS, PCS, and MHI-5 scores within exposure groups over time. The primary study outcome was a comparison of the change in MCS, PCS, and MHI-5 scores between the three study arms over 12 months. Stratified analyses were performed to evaluate for effect measure modification. Assessment for confounding was done by separately adjusting for co-variates in a linear regression model, with study arm and change in scores as the independent and dependent variables, respectively. A variable was considered to be a confounder if there was at least a 10% change in the beta coefficient estimate between the crude and variable-adjusted model. A P-value of <0.05 was considered statistically significant.
Ethical Considerations
This study was conducted under a protocol approved by the following: the Human Research Protection Office at UMB, the Office of Research at UPMC, and the Human Research Protection Office at VU.
RESULTS
Characteristics of Study Participants
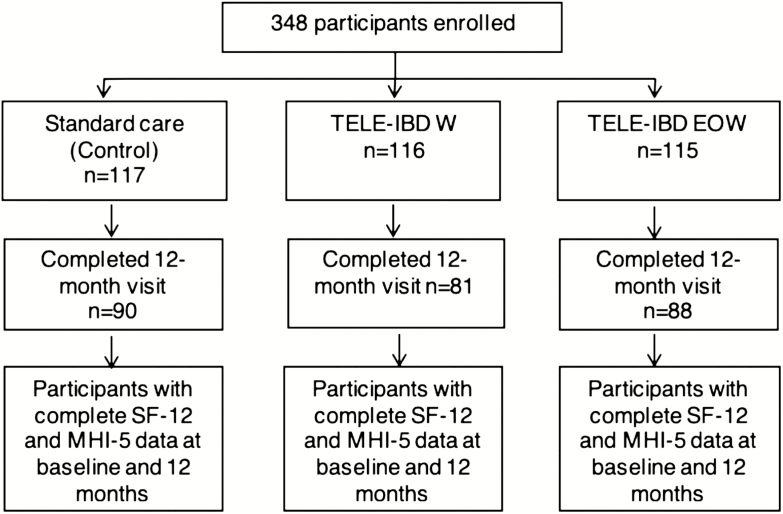
Of the 348 participants enrolled in the TELE-IBD trial, 217 (62%) of them were included in this analysis (Figure 1). There were 72 (62%), 71 (61%), and 74 (64%) participants in the standard care, TELE-IBD W, and TELE-IBD EOW arms, respectively. Mean age was 38.7 ± 12.3 years, 58.9% were women (n = 128), and 94% were Caucasian (n = 204). Sixty-nine percent of participants had CD (n = 150), with nearly a third of these (n = 42) reporting a history of perianal disease. The mean age at onset of IBD was 26.5 ± 11.4 years and the mean disease duration was 11.9 ± 9.2 years. At baseline, the clinical and demographic characteristics of participants in the three groups were comparable (Table 1). The proportion of participants who were compliant with self-monitoring in the two telemedicine groups did not differ significantly (56.3% in the TELE-IBD W vs 63.5% in the TELE-IBD EOW arm, P = 0.38).
FIGURE 1.
Participant flow in the TELEmedicine for Inflammatory Bowel Disease (TELE-IBD) study.
TABLE 1.
Baseline Demographic and Clinical Characteristics of Study Participants in the TELEmedicine for Inflammatory Bowel Disease (TELE-IBD) Trial
| Characteristics | Standard of Care (n = 72) | TELE-IBD W (n = 71) | TELE-IBD EOW (n = 74) | P-Value |
|---|---|---|---|---|
| Mean age (± SD) | 39.5 (12.0) | 37.3 (11.6) | 39.3 (13.4) | 0.49 |
| Sex, n (%) | ||||
| Female | 45 (62.5) | 39 (55.0) | 44 (59.5) | 0.65 |
| Race, n (%) | ||||
| White | 66 (91.7) | 67 (94.4) | 71 (96.0) | 0.54 |
| Study site, n (%) | 0.72 | |||
| University of Maryland | 37 (51.4) | 39 (54.9) | 43 (58.1) | |
| University of Pittsburgh | 23 (31.9) | 25 (35.2) | 21 (28.4) | |
| Vanderbilt University | 12 (16.7) | 7 (9.9) | 10 (13.5) | |
| Tobacco use | 0.67 | |||
| Never smoked | 46 (65.7) | 45 (66.2) | 41 (56.2) | |
| Former smoker | 17 (24.3) | 17 (25.0) | 25 (34.2) | |
| Current smoker | 7 (10.0) | 6 (8.8) | 7 (9.6) | |
| Disease type, n (%) | 0.36 | |||
| Crohn’s disease | 50 (69.4) | 45 (63.4) | 55 (74.3) | |
| Ulcerative colitis | 22 (30.6) | 26 (36.6) | 19 (25.7) | |
| UC disease extent, n (%) | 0.99 | |||
| Extensive | 15 (68.2) | 18 (69.2) | 13 (68.4) | |
| CD disease location, n (%) | ||||
| Ileal | 9 (18.0) | 8 (17.8) | 11 (20.0) | 0.95 |
| Colonic | 12 (24.0) | 10 (22.2) | 6 (10.9) | 0.17 |
| Ileocolonic | 22 (44.0) | 25 (55.6) | 26 (47.3) | 0.51 |
| Upper tract involvement | 5 (10.0) | 5 (11.1) | 7 (12.7) | 0.91 |
| CD disease behavior, n (%) | ||||
| Inflammatory | 25 (50.0) | 18 (40.0) | 17 (33.3) | 0.23 |
| Obstructing | 10 (20.0) | 9 (20.0) | 13 (25.5) | 0.75 |
| Perforating | 15 (30.0) | 18 (40.0) | 21 (41.2) | 0.45 |
| Perianal disease, n (%) | 15 (29.4) | 12 (27.9) | 15 (27.8) | 0.97 |
| Age at disease onset in years, mean (± SD) | 26.8 (11.2) | 25.4 (10.9) | 27.5 (12.1) | 0.56 |
| Disease duration in years, mean (± SD) | 12.4 (9.8) | 11.8 (8.6) | 11.7 (9.4) | 0.91 |
| Time since last flare in years, mean (± SD) | 0.6 (0.7) | 0.7 (0.6) | 0.6 (0.6) | 0.72 |
| Disease activity scores mean (± SD) | ||||
| HBI | 4.4 (4.0) | 3.1 (3.1) | 4.3 (3.9) | 0.15 |
| SCCAI | 3.0 (3.1) | 2.7 (2.6) | 2.3 (2.8) | 0.71 |
| IBDQ score, mean (± SD) | 168.1 (32.5) | 173.2 (32.5) | 174.9 (33.5) | 0.43 |
| CRP of 3 or greater | 20 (35.7) | 25 (41.7) | 23 (35.4) | 0.72 |
SD = Standard deviation; HBI = Harvey Bradshaw Index; SCCAI = Simple Clinical Colitis Activity Index; PCS = Physical Component Score; MCS = Mental Component Score; CRP = C-reactive protein; IBDQ = Inflammatory Bowel Disease Questionnaire; W = weekly; EOW = every other week.
Impact of Telemedicine on Depressive Symptoms
Baseline MHI-5 scores were 75.9 ± 15.9, 74.1 ± 17.4, and 74.8 ± 18.3 in the standard care, TELE-IBD W, and TELE-IBD EOW arms, respectively (P = 0.81). At the end of the study, MHI-5 scores increased in all 3 arms to 79.3 ± 12.8, 77.1 ± 17.0, and 75.5 ± 19.9 in the standard care, TELE-IBD W, and TELE-IBD EOW arms, respectively. This increase in MHI-5 over 12 months was not significant within any of the groups (standard care, P = 0.07, TELE-IBD W, P = 0.15, and TELE-IBD EOW, P = 0.72). After adjustment for confounding, there was no significant difference in the change in MHI-5 scores between the three groups (P = 0.70) (Table 2).
TABLE 2.
Comparison of the Change in Mean Mental Component Score, Physical Component Score, and Mental Health Index-5 Over 12 Months in Participants of the TELEmedicine for Inflammatory Bowel Disease (TELE-IBD) Trial
| Standard of Care | Telemedicine Weekly | Telemedicine EOW | Unadjusted P-Value | Adjusted P-Value* | |
|---|---|---|---|---|---|
| Change in PCS, mean | +3.7 | +0.4 | +0.6 | 0.03 | 0.06 |
| Change in MCS, mean | +2.5 | +1.4 | +1.0 | 0.66 | 0.89 |
| Change in MHI-5, mean | +3.4 | +3.0 | +0.7 | 0.57 | 0.70 |
*Adjusted for baseline IBDQ scores.
PCS = Physical Component Score; MCS = Mental Component Score; MHI = Mental Health Index-5; EOW = every other week.
Impact of Telemedicine on Generic QoL
In the standard care, TELE-IBD W, and TELE-IBD EOW groups, baseline MCS scores were 48.6 ± 9.8, 48.5 ± 8.8, and 48.6 ± 9.8, respectively (P = 0.99). This increased to 51.1 ± 7.2, 49.9 ± 8.9, and 49.6 ± 10.6 in the control, TELE-IBD W, and TELE-IBD EOW groups, respectively, at the end of the study. The change in MCS scores from baseline was significant within the standard care group (P = 0.04) but was nonsignificant within the TELE-IBD W (P = 0.20) and TELE-IBD EOW groups (P = 0.37). There was no difference in the change in MCS scores between the three groups (P = 0.89) after adjustment for confounding.
Baseline PCS scores were 46.2 ± 10.1, 48.1 ± 8.7, and 46.4 ± 10.1 in the standard care, TELE-IBD W, and TELE-IBD EOW groups, respectively (P = 0.45). This increased over 12 months to 49.9 ± 8.0, 48.5 ± 9.6, and 47.1 ± 10.7 in the standard care, TELE-IBD W, and TELE-IBD EOW groups, respectively. The improvement in PCS scores was only significant within the standard care group (standard care, P = 0.0003, TELE-IBD W, P = 0.71, and TELE-IBD EOW, P = 0.54). After adjustment for confounding, there was no significant difference in the change in PCS scores between the three groups (P = 0.06). However, comparisons of the standard care with the separate telemedicine arms revealed that the standard care group had a significant increase in PCS scores when compared with the TELE-IBD W group (P = 0.03 for TELE-IBD W vs standard care and P = 0.07 for TELE-IBD EOW vs standard care).
DISCUSSION
In the present study using data from the TELE-IBD trial, we found that text message-based telemedicine did not improve DS or generic QoL in IBD patients when compared to those managed with standard care. Over the 12-month study period, the MHI-5, MCS, and PCS scores improved from baseline in all the study arms, but the within-group score increases were not significant for participants in the two telemedicine arms. On the other hand, those in the standard care group experienced significant increases in MCS and PCS scores over time. We also found that, on separate adjusted analyses, those in the standard care group had a significant improvement in physical functioning over time when compared with the TELE-IBD W group.
To the best of our knowledge, this is the first prospective, randomized, clinical trial to examine the effect of telemedicine with text messaging on DS and general QoL in patients with IBD. The main findings from this study have important implications. The lack of a positive effect of text message-based telemedicine on DS and generic QoL challenges us to re-evaluate the overall value of this modality for IBD patients despite the current paradigm shift toward the increased use of communication technology in patient care. Given the tremendous impact of DS and poor QoL in IBD patients, it is important that healthcare providers and administrators balance the health system-related benefits of telemedicine, such as reduced utilization and cost, with its likely inability to improve key patient-centered outcomes.24, 25
There are no published text message-based telemedicine trials that have evaluated DS in IBD patients, but web-based telemedicine has similarly had little to no effect in improving depression. In a trial where 333 UC patients on 5-aminosalicylate therapy were randomized to a control group or to receive web-based disease education and self-management, Elkjaer et al. found that web-based telemedicine did not significantly improve depressive symptoms in IBD patients in Ireland and Denmark over 12 months.27 On the contrary, they noted improvement in depression scores, as measured with the Hospital Anxiety and Depression Scale (HADS), in Danish control patients (P = 0.01). Like the aforementioned study, the interventions offered in the TELE-IBD trial did not include a specific psychological component. Although it is conceivable that the absence of tailored psychological intervention in the design of telemedicine systems may explain the lack of improvement in DS, psychotherapy-based telemedicine studies have also not been promising. In a randomized study comparing computer-based cognitive behavioral therapy (CCBT) with standard care, researchers found that there was no improvement in depression or anxiety after 6 months.26
We also found that telemedicine did not improve generic QoL. While a few published studies have reported improvement in the generic QoL of IBD patients managed with web-based interventions, others have shown no improvement.24, 27 Pedersen et al. employed a web-treatment program to individualize infliximab maintenance treatment in a study of CD patients. Using the SF-36 instrument, they found that there was no significant difference in the generic QoL of participants at the end of 1 year.23 Psychological telemedicine interventions have also not been found to have a sustained impact on generic QoL. Patients who received self-administered CCBT were found to have significantly improved SF-12 MCS scores at 12 weeks when compared with controls (P = 0.03).26 However, this improvement was not maintained at 6 months (P = 0.31). There were no improvements in PCS scores at 12 weeks or 6 months. Interestingly, the authors found that the limited improvement in MCS scores was only seen among those who had completed at least 50% of the CCBT on per-protocol analyses. This suggests that adherence may be an important substrate for the improvement of QoL in telemedicine. In the present study, only 59% of participants in the two telemedicine groups completed at least 80% of self-testing sessions over the 1-year period. This low level of adherence may have contributed to the absence of a benefit of telemedicine on generic QoL and depression. To improve on this, future telemedicine research should incorporate specific measures in their design phase to optimize participant engagement, adherence, and retention through the course of a study.
The inability of telemedicine to improve DS or QoL may partly be related to the absence of a real sham group as a comparator in the TELE-IBD trial. The standard care group had significant within-group improvement in generic QoL and a significant increase in PCS scores when compared with the TELE-IBD W group. These improvements are likely reflective of the multidisciplinary and high level of care received by the standard care group. All three study sites are tertiary referral centers with expertise in the care of patients with IBD, and participants were supported by trainees, nurse educators, dieticians, behavioral health specialists, and advanced practice providers. It is possible that any incremental benefit of telemedicine on DS or QoL may have been blunted by the high quality of care received by the standard care group. Additionally, the exclusion of participants with certain markers of severe diseases – such as those with a stoma, ileorectal anastomosis, j pouch or imminent surgery – may have led to the selection of a cohort that was healthier than the typical IBD population and less likely to benefit from any intervention. However, because we used patient report outcomes measures that utilize diarrhea to calculate a disease activity score, we had to exclude these patients since bowel movements could not be calculated or were increased due to altered surgical anatomy. In addition, we excluded patients where surgery was imminent as symptoms would be difficult to interpret immediately after surgery and surgery would likely induce remission with little variability in symptoms during the 1-year follow-up time.
This study has a number of limitations and strengths. Only 62% of participants enrolled in the TELE-IBD trial were eligible for inclusion in our final analysis. While this is concerning for selection bias, we found that the rate of attrition and/or incomplete data collection was comparable between the study arms. Furthermore, the arms were not demonstrably different with respect to baseline socio-demographic and clinical characteristics. Another limitation of this study is that providers were not blinded to participant assignments. This may have led to some bias as the standard care group may have, knowingly or unknowingly, been provided with more thorough care and resources than would have been the case in a non-study context. Finally, our findings are likely not generalizable as all three study sites are tertiary referral centers for IBD care. A major strength of this work is that it utilized a randomized, controlled, trial design. Additionally, we conducted adjusted analyses to account for confounding variables despite the randomization implemented in the trial. We also used valid instruments known to have good measurement properties in IBD to assess DS and QoL in the study cohort.
In conclusion, text message-based telemedicine did not improve DS and QoL in participants in the TELE-IBD trial. In fact, participants in the standard care group had greater improvement in the physical component of QoL when compared with those in the TELE-IBD W arm. Further research is needed to determine if revised telemedicine systems with a multidisciplinary component can better engage patients in remote monitoring to improve DS and generic QoL. Studies on the use of remote monitoring in less-specialized settings are also needed to determine whether telemedicine improves DS and generic QoL in practices where there are fewer resources to care for patients with IBD. Finally, the use of remote monitoring to decrease components of standard care such as routine office visits should be explored to decrease healthcare utilization and to improve access to specialty IBD care.
Funding: The research reported here was supported by the Agency for Healthcare Research and Quality (1R01HS018975-01A1) and the University of Maryland General Clinical Research Centers Program. M.S. was supported by the Program for Research Initiated by Students and Mentors (PRISM) at the University of Maryland School of Medicine. K.C.-O. and A.A. were supported by a T32 Research grant (DK067872-11) from the National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases.
Conflicts of interest: The authors declare that there is no potential conflict of interest with respect to the research, authorship, and/or publication of this article.
REFERENCES
- 1. Dahlhamer JM, Zammitti EP, Ward BW, et al. Prevalence of inflammatory bowel disease among adults aged ≥18 years - United States, 2015. MMWR Morb Mortal Wkly Rep. 2016;65:1166–1169. [DOI] [PubMed] [Google Scholar]
- 2. Kemp K, Griffiths J, Lovell K. Understanding the health and social care needs of people living with IBD: a meta-synthesis of the evidence. World J Gastroenterol. 2012;18:6240–6249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Loftus EV Jr, Sandborn WJ. Epidemiology of inflammatory bowel disease. Gastroenterol Clin North Am. 2002;31:1–20. [DOI] [PubMed] [Google Scholar]
- 4. Cohen R, Skup M, Ozbay AB, et al. Direct and indirect healthcare resource utilization and costs associated with ulcerative colitis in a privately-insured employed population in the US. J Med Econ. 2015;18:447–456. [DOI] [PubMed] [Google Scholar]
- 5. Gibson TB, Ng E, Ozminkowski RJ, et al. The direct and indirect cost burden of Crohn’s disease and ulcerative colitis. J Occup Environ Med. 2008;50:1261–1272. [DOI] [PubMed] [Google Scholar]
- 6. Ganz ML, Sugarman R, Wang R, et al. The economic and health-related impact of Crohn’s disease in the United States: evidence from a nationally representative survey. Inflamm Bowel Dis. 2016;22:1032–1041. [DOI] [PubMed] [Google Scholar]
- 7. Ananthakrishnan AN, Khalili H, Pan A, et al. Association between depressive symptoms and incidence of Crohn’s disease and ulcerative colitis: results from the Nurses’ Health Study. Clin Gastroenterol Hepatol. 2013;11:57–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mittermaier C, Dejaco C, Waldhoer T, et al. Impact of depressive mood on relapse in patients with inflammatory bowel disease: a prospective 18-month follow-up study. Psychosom Med. 2004;66:79–84. [DOI] [PubMed] [Google Scholar]
- 9. Loftus EV Jr, Guérin A, Yu AP, et al. Increased risks of developing anxiety and depression in young patients with Crohn’s disease. Am J Gastroenterol. 2011;106:1670–1677. [DOI] [PubMed] [Google Scholar]
- 10. Bhandari S, Larson ME, Kumar N, Stein D. Association of inflammatory bowel disease (IBD) with depressive symptoms in the United States population and independent predictors of depressive symptoms in an IBD population: a NHANES study. Gut Liver. 2017;11:512–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bernklev T, Jahnsen J, Lygren I, et al. Health-related quality of life in patients with inflammatory bowel disease measured with the short form-36: psychometric assessments and a comparison with general population norms. Inflamm Bowel Dis. 2005;11:909–918. [DOI] [PubMed] [Google Scholar]
- 12. Janke KH, Klump B, Gregor M, et al. Determinants of life satisfaction in inflammatory bowel disease. Inflamm Bowel Dis. 2005;11:272–286. [DOI] [PubMed] [Google Scholar]
- 13. Janke KH, Raible A, Bauer M, et al. Questions on life satisfaction (FLZM) in inflammatory bowel disease. Int J Colorectal Dis. 2004;19:343–353. [DOI] [PubMed] [Google Scholar]
- 14. Keefer L, Kane SV. Considering the bidirectional pathways between depression and IBD: recommendations for comprehensive IBD Care. Gastroenterol Hepatol (N Y). 2017;13:164–169. [PMC free article] [PubMed] [Google Scholar]
- 15. Sajadinejad MS, Asgari K, Molavi H, et al. Psychological issues in inflammatory bowel disease: an overview. Gastroenterol Res Pract. 2012;2012:106502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gaines LS, Slaughter JC, Horst SN, et al. Association between affective-cognitive symptoms of depression and exacerbation of Crohn’s disease. Am J Gastroenterol. 2016;111:864–870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mawdsley JE, Macey MG, Feakins RM, et al. The effect of acute psychologic stress on systemic and rectal mucosal measures of inflammation in ulcerative colitis. Gastroenterology. 2006;131:410–419. [DOI] [PubMed] [Google Scholar]
- 18. Allegretti JR, Borges L, Lucci M, et al. Risk factors for rehospitalization within 90 days in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2015;21:2583–2589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ananthakrishnan AN, Gainer VS, Perez RG, et al. Psychiatric co-morbidity is associated with increased risk of surgery in Crohn’s disease. Aliment Pharmacol Ther. 2013;37:445–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wong JJ, Sceats L, Dehghan M, et al. Depression and health care use in patients with inflammatory bowel disease. J Crohns Colitis. 2019;13:19–26. [DOI] [PubMed] [Google Scholar]
- 21. Cross RK, Arora M, Finkelstein J. Acceptance of telemanagement is high in patients with inflammatory bowel disease. J Clin Gastroenterol. 2006;40:200–208. [DOI] [PubMed] [Google Scholar]
- 22. Cross RK, Finkelstein J. Feasibility and acceptance of a home telemanagement system in patients with inflammatory bowel disease: a 6-month pilot study. Dig Dis Sci. 2007;52:357–364. [DOI] [PubMed] [Google Scholar]
- 23. Pedersen N, Elkjaer M, Duricova D, et al. eHealth: individualisation of infliximab treatment and disease course via a self-managed web-based solution in Crohn’s disease. Aliment Pharmacol Ther. 2012;36:840–849. [DOI] [PubMed] [Google Scholar]
- 24. Pedersen N, Thielsen P, Martinsen L, et al. eHealth: individualization of mesalazine treatment through a self-managed web-based solution in mild-to-moderate ulcerative colitis. Inflamm Bowel Dis. 2014;20:2276–2285. [DOI] [PubMed] [Google Scholar]
- 25. Cross RK, Cheevers N, Rustgi A, et al. Randomized, controlled trial of home telemanagement in patients with ulcerative colitis (UC HAT). Inflamm Bowel Dis. 2012;18:1018–1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. McCombie A, Gearry R, Andrews J, et al. Does computerized cognitive behavioral therapy help people with inflammatory bowel disease? A randomized controlled trial. Inflamm Bowel Dis. 2016;22:171–181. [DOI] [PubMed] [Google Scholar]
- 27. Elkjaer M, Shuhaibar M, Burisch J, et al. E-health empowers patients with ulcerative colitis: a randomised controlled trial of the web-guided ‘Constant-care’ approach. Gut. 2010;59:1652–1661. [DOI] [PubMed] [Google Scholar]
- 28. Cross RK, Langenberg P, Regueiro M, et al. A randomized controlled trial of TELEmedicine for Patients with Inflammatory Bowel Disease (TELE-IBD). Am J Gastroenterol. 2019;114:472–482. [DOI] [PubMed] [Google Scholar]
- 29. Alrubaiy L, Rikaby I, Dodds P, et al. Systematic review of health-related quality of life measures for inflammatory bowel disease. J Crohns Colitis. 2015;9:284–292. [DOI] [PubMed] [Google Scholar]
- 30. Pallis AG, Mouzas IA. Instruments for quality of life assessment in patients with inflammatory bowel disease. Dig Liver Dis. 2000;32:682–688. [DOI] [PubMed] [Google Scholar]
- 31. Cross RK, Jambaulikar G, Langenberg P, et al. TELEmedicine for Patients with Inflammatory Bowel Disease (TELE-IBD): design and implementation of randomized clinical trial. Contemp Clin Trials. 2015;42:132–144. [DOI] [PubMed] [Google Scholar]
- 32. Lennard-Jones JE. Classification of inflammatory bowel disease. Scand J Gastroenterol Suppl. 1989;170:2–6; discussion 16. [DOI] [PubMed] [Google Scholar]
- 33. Cuijpers P, Smits N, Donker T, et al. Screening for mood and anxiety disorders with the five-item, the three-item, and the two-item Mental Health Inventory. Psychiatry Res. 2009;168:250–255. [DOI] [PubMed] [Google Scholar]
- 34. Strand BH, Dalgard OS, Tambs K, Rognerud M. Measuring the mental health status of the Norwegian population: a comparison of the instruments SCL-25, SCL-10, SCL-5 and MHI-5 (SF-36). Nord J Psychiatry. 2003;57:113–118. [DOI] [PubMed] [Google Scholar]
- 35. van den Beukel TO, Siegert CE, van Dijk S, et al. Comparison of the SF-36 five-item Mental Health Inventory and Beck Depression Inventory for the screening of depressive symptoms in chronic dialysis patients. Nephrol Dial Transplant. 2012;27:4453–4457. [DOI] [PubMed] [Google Scholar]
- 36. Friedman B, Heisel M, Delavan R. Validity of the SF-36 five-item mental health index for major depression in functionally impaired, community-dwelling elderly patients. J Am Geriatr Soc. 2005;53:1978–1985. [DOI] [PubMed] [Google Scholar]
- 37. Gandek B, Ware JE, Aaronson NK, et al. Cross-validation of item selection and scoring for the SF-12 health survey in nine countries: results from the IQOLA project. International Quality of Life Assessment. J Clin Epidemiol. 1998;51:1171–1178. [DOI] [PubMed] [Google Scholar]
- 38. Ware J Jr, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. [DOI] [PubMed] [Google Scholar]
- 39. Ware JE, Kosinski M, Keller SD.. SF-12: How to Score the SF-12 Physical and Mental Health Summary Scales. 4th ed. Boston, MA: Quality Metric Inc.; 2002. [Google Scholar]
- 40. Jenkinson C, Coulter A, Wright L. Short form 36 (SF36) health survey questionnaire: normative data for adults of working age. Bmj. 1993;306:1437–1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Walmsley RS, Ayres RC, Pounder RE, Allan RN. A simple clinical colitis activity index. Gut. 1998;43:29–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Harvey RF, Bradshaw JM. A simple index of Crohn’s-disease activity. Lancet. 1980;1:514. [DOI] [PubMed] [Google Scholar]
- 43. Guyatt G, Mitchell A, Irvine EJ, et al. A new measure of health status for clinical trials in inflammatory bowel disease. Gastroenterology. 1989;96:804–810. [PubMed] [Google Scholar]