Abstract
Attention-deficit/hyperactivity disorder (ADHD) is one of the most common neurobehavioral disorders of childhood and can profoundly affect children’s academic achievement, well-being, and social interactions. The American Academy of Pediatrics first published clinical recommendations for evaluation and diagnosis of pediatric ADHD in 2000; recommendations for treatment followed in 2001. The guidelines were revised in 2011 and published with an accompanying process of care algorithm (PoCA) providing discrete and manageable steps by which clinicians could fulfill the clinical guideline’s recommendations. Since the release of the 2011 guideline, the Diagnostic and Statistical Manual of Mental Disorders has been revised to the fifth edition, and new ADHD-related research has been published. These publications do not support dramatic changes to the previous recommendations. Therefore, only incremental updates have been made in this guideline revision, including the addition of a key action statement related to diagnosis and treatment of comorbid conditions in children and adolescents with ADHD. The accompanying process of care algorithm has also been updated to assist in implementing the guideline recommendations. Throughout the process of revising the guideline and algorithm, numerous systemic barriers were identified that restrict and/or hamper pediatric clinicians’ ability to adopt their recommendations. Therefore, the subcommittee created a companion article (available in the Supplemental Information) on systemic barriers to the care of children and adolescents with ADHD, which identifies the major systemic-level barriers and presents recommendations to address those barriers; in this article, we support the recommendations of the clinical practice guideline and accompanying process of care algorithm.
INTRODUCTION
This article updates and replaces the 2011 clinical practice guideline revision published by the American Academy of Pediatrics (AAP), “Clinical Practice Guideline: Diagnosis and Evaluation of the Child with Attention-Deficit/Hyperactivity Disorder.”1 This guideline, like the previous document, addresses the evaluation, diagnosis, and treatment of attention-deficit/hyperactivity disorder (ADHD) in children from age 4 years to their 18th birthday, with special guidance provided for ADHD care for preschool-aged children and adolescents. (Note that for the purposes of this document, “preschool-aged” refers to children from age 4 years to the sixth birthday.) Pediatricians and other primary care clinicians (PCCs) may continue to provide care after 18 years of age, but care beyond this age was not studied for this guideline.
Since 2011, much research has occurred, and the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), has been released. The new research and DSM-5 do not, however, support dramatic changes to the previous recommendations. Hence, this new guideline includes only incremental updates to the previous guideline. One such update is the addition of a key action statement (KAS) about the diagnosis and treatment of coexisting or comorbid conditions in children and adolescents with ADHD. The subcommittee uses the term “comorbid,” to be consistent with the DSM-5.
Since 2011, the release of new research reflects an increased understanding and recognition of ADHD’s prevalence and epidemiology; the challenges it raises for children and families; the need for a comprehensive clinical resource for the evaluation, diagnosis, and treatment of pediatric ADHD; and the barriers that impede the implementation of such a resource. In response, this guideline is supported by 2 accompanying documents, available in the Supplemental Information: (1) a process of care algorithm (PoCA) for the diagnosis and treatment of children and adolescents with ADHD and (2) an article on systemic barriers to the care of children and adolescents with ADHD. These supplemental documents are designed to aid PCCs in implementing the formal recommendations for the evaluation, diagnosis, and treatment of children and adolescents with ADHD. Although this document is specific to children and adolescents in the United States in some of its recommendations, international stakeholders can modify specific content (ie, educational laws about accommodations, etc) as needed. (Prevention is addressed in the Mental Health Task Force recommendations.2)
PoCA for the Diagnosis and Treatment of Children and Adolescents With ADHD
In this revised guideline and accompanying PoCA, we recognize that evaluation, diagnosis, and treatment are a continuous process. The PoCA provides recommendations for implementing the guideline steps, although there is less evidence for the PoCA than for the guidelines. The section on evaluating and treating comorbidities has also been expanded in the PoCA document.
Systems Barriers to the Care of Children and Adolescents With ADHD
There are many system-level barriers that hamper the adoption of the best-practice recommendations contained in the clinical practice guideline and the PoCA. The procedures recommended in this guideline necessitate spending more time with patients and their families, developing a care management system of contacts with school and other community stakeholders, and providing continuous, coordinated care to the patient and his or her family. There is some evidence that African American and Latino children are less likely to have ADHD diagnosed and are less likely to be treated for ADHD. Special attention should be given to these populations when assessing comorbidities as they relate to ADHD and when treating for ADHD symptoms.3 Given the nationwide problem of limited access to mental health clinicians,4 pediatricians and other PCCs are increasingly called on to provide services to patients with ADHD and to their families. In addition, the AAP holds that primary care pediatricians should be prepared to diagnose and manage mild-to-moderate ADHD, anxiety, depression, and problematic substance use, as well as co-manage patients who have more severe conditions with mental health professionals. Unfortunately, third-party payers seldom pay appropriately for these time-consuming services.5,6
To assist pediatricians and other PCCs in overcoming such obstacles, the companion article on systemic barriers to the care of children and adolescents with ADHD reviews the barriers and makes recommendations to address them to enhance care for children and adolescents with ADHD.
ADHD EPIDEMIOLOGY AND SCOPE
Prevalence estimates of ADHD vary on the basis of differences in research methodologies, the various age groups being described, and changes in diagnostic criteria over time.7 Authors of a recent meta-analysis calculated a pooled worldwide ADHD prevalence of 7.2% among children8; estimates from some community-based samples are somewhat higher, at 8.7% to 15.5%.9,10 National survey data from 2016 indicate that 9.4% of children in the United States 2 to 17 years of age have ever had an ADHD diagnosis, including 2.4% of children 2 to 5 years of age.11 In that national survey, 8.4% of children 2 to 17 years of age currently had ADHD, representing 5.4 million children.11 Among children and adolescents with current ADHD, almost two-thirds were taking medication, and approximately half had received behavioral treatment of ADHD in the past year. Nearly one quarter had received neither type of treatment of ADHD.11
Symptoms of ADHD occur in childhood, and most children with ADHD will continue to have symptoms and impairment through adolescence and into adulthood. According to a 2014 national survey, the median age of diagnosis was 7 years; approximately one-third of children were diagnosed before 6 years of age.12 More than half of these children were first diagnosed by a PCC, often a pediatrician.12 As individuals with ADHD enter adolescence, their overt hyperactive and impulsive symptoms tend to decline, whereas their inattentive symptoms tend to persist.13,14 Learning and language problems are common comorbid conditions with ADHD.15
Boys are more than twice as likely as girls to receive a diagnosis of ADHD,9,11,16 possibly because hyperactive behaviors, which are easily observable and potentially disruptive, are seen more frequently in boys. The majority of both boys and girls with ADHD also meet diagnostic criteria for another mental disorder.17,18 Boys are more likely to exhibit externalizing conditions like oppositional defiant disorder or conduct disorder.17,19,20 Recent research has established that girls with ADHD are more likely than boys to have a comorbid internalizing condition like anxiety or depression.21
Although there is a greater risk of receiving a diagnosis of ADHD for children who are the youngest in their class (who are therefore less developmentally capable of compensating for their weaknesses), for most children, retention is not beneficial.22
METHODOLOGY
As with the original 2000 clinical practice guideline and the 2011 revision, the AAP collaborated with several organizations to form a subcommittee on ADHD (the subcommittee) under the oversight of the AAP Council on Quality Improvement and Patient Safety.
The subcommittee’s membership included representation of a wide range of primary care and subspecialty groups, including primary care pediatricians, developmental-behavioral pediatricians, an epidemiologist from the Centers for Disease Control and Prevention; and representatives from the American Academy of Child and Adolescent Psychiatry, the Society for Pediatric Psychology, the National Association of School Psychologists, the Society for Developmental and Behavioral Pediatrics (SDBP), the American Academy of Family Physicians, and Children and Adults with Attention-Deficit/Hyperactivity Disorder (CHADD) to provide feedback on the patient/parent perspective.
This subcommittee met over a 3.5-year period from 2015 to 2018 to review practice changes and newly identified issues that have arisen since the publication of the 2011 guidelines. The subcommittee members’ potential conflicts were identified and taken into consideration in the group’s deliberations. No conflicts prevented subcommittee member participation on the guidelines.
Research Questions
The subcommittee developed a series of research questions to direct an evidence-based review sponsored by 1 of the Evidence-based Practice Centers of the US Agency for Healthcare Research and Quality (AHRQ).23 These questions assessed 4 diagnostic areas and 3 treatment areas on the basis of research published in 2011 through 2016.
The AHRQ’s framework was guided by key clinical questions addressing diagnosis as well as treatment interventions for children and adolescents 4 to 18 years of age.
The first clinical questions pertaining to ADHD diagnosis were as follows:
What is the comparative diagnostic accuracy of approaches that can be used in the primary care practice setting or by specialists to diagnose ADHD among children younger than 7 years of age?
What is the comparative diagnostic accuracy of EEC, imaging, or executive function approaches that can be used in the primary care practice setting or by specialists to diagnose ADHD among individuals aged 7 to their 18th birthday?
What are the adverse effects associated with being labeled correctly or incorrectly as having ADHD?
Are there more formal neuropsychological, imaging, or genetic tests that improve the diagnostic process?
The treatment questions were as follows:
What are the comparative safety and effectiveness of pharmacologic and/or nonpharmacologic treatments of ADHD in improving outcomes associated with ADHD?
What is the risk of diversion of pharmacologic treatment?
What are the comparative safety and effectiveness of different monitoring strategies to evaluate the effectiveness of treatment or changes in ADHD status (eg, worsening or resolving symptoms)?
In addition to this review of the research questions, the subcommittee considered information from a review of evidence-based psychosocial treatments for children and adolescents with ADHD24 (which, in some cases, affected the evidence grade) as well as updated information on prevalence from the Centers for Disease Control and Prevention.
Evidence Review
This article followed the latest version of the evidence base update format used to develop the previous 3 clinical practice guidelines.24–26 Under this format, studies were only included in the review when they met a variety of criteria designed to ensure the research was based on a strong methodology that yielded confidence in its conclusions.
The level of efficacy for each treatment was defined on the basis of child-focused outcomes related to both symptoms and impairment. Hence, improvements in behaviors on the part of parents or teachers, such as the use of communication or praise, were not considered in the review. Although these outcomes are important, they address how treatment reaches the child or adolescent with ADHD and are, therefore, secondary to changes in the child’s behavior. Focusing on improvements in the child or adolescent’s symptoms and impairment emphasizes the disorder’s characteristics and manifestations that affect children and their families.
The treatment-related evidence relied on a recent review of literature from 2011 through 2016 by the AHRQ of citations from Medline, Embase, PsycINFO, and the Cochrane Database of Systematic Reviews.
The original methodology and report, including the evidence search and review, are available in their entirety and as an executive summary at https://effectivehealthcare.ahrq.gov/sites/default/files/pdf/cer-203-adhd-final_0.pdf.
The evidence is discussed in more detail in published reports and articles.25
Guideline Recommendations and Key Action Statements
The AAP policy statement, “Classifying Recommendations for Clinical Practice Guidelines,” was followed in designating aggregate evidence quality levels for the available evidence (see Fig 1).27 The AAP policy statement is consistent with the grading recommendations advanced by the University of Oxford Centre for Evidence Based Medicine.
FIGURE 1.
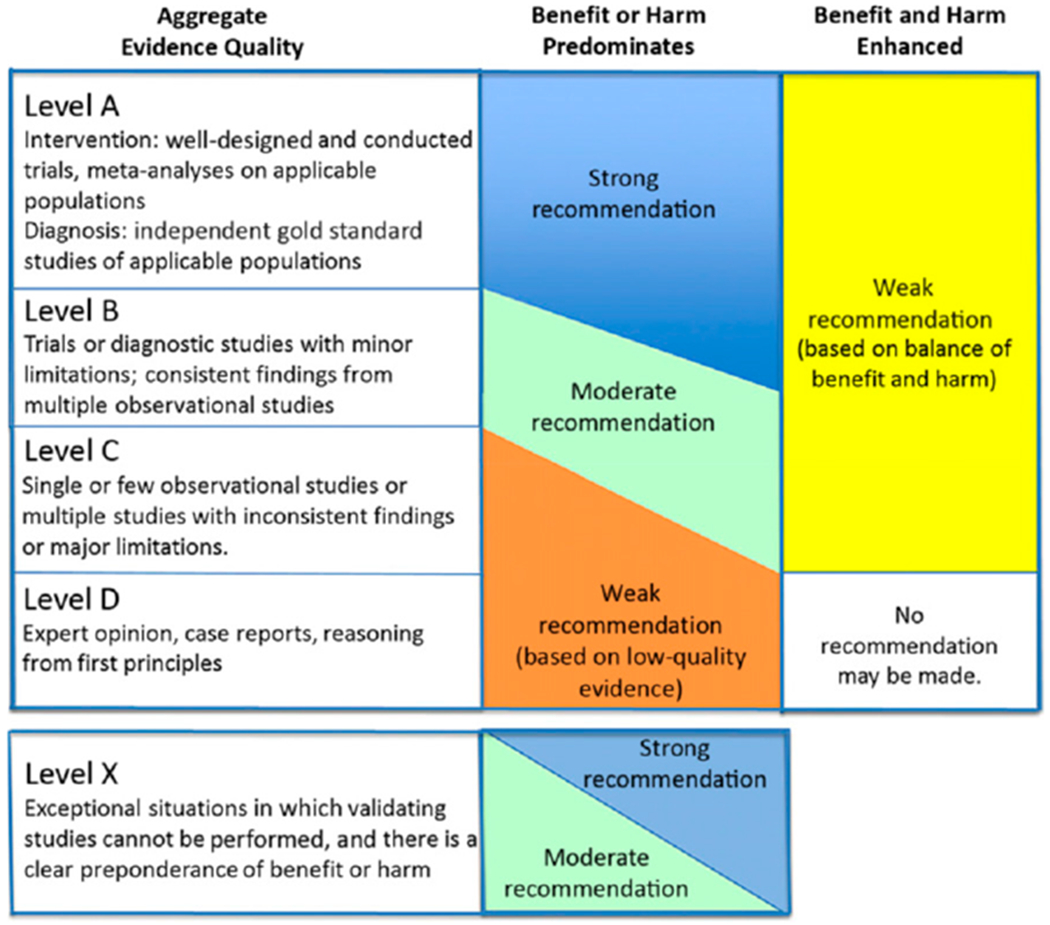
AAP rating of evidence and recommendations.
The subcommittee reached consensus on the evidence, which was then used to develop the clinical practice guideline’s KASs.
When the scientific evidence was at least “good” in quality and demonstrated a preponderance of benefits over harms, the KAS provides a “strong recommendation” or “recommendation.”27 Clinicians should follow a “strong recommendation” unless a clear and compelling rationale for an alternative approach is present; clinicians are prudent to follow a “recommendation” but are advised to remain alert to new information and be sensitive to patient preferences27 (see Fig 1).
When the scientific evidence comprised lower-quality or limited data and expert consensus or high-quality evidence with a balance between benefits and harms, the KAS provides an “option” level of recommendation. Options are clinical interventions that a reasonable health care provider might or might not wish to implement in the practice.27 Where the evidence was lacking, a combination of evidence and expert consensus would be used, although this did not occur in these guidelines, and all KASs achieved a “strong recommendation” level except for KAS 7, on comorbidities, which received a recommendation level (see Fig 1).
As shown in Fig 1, integrating evidence quality appraisal with an assessment of the anticipated balance between benefits and harms leads to a designation of a strong recommendation, recommendation, option, or no recommendation.
Once the evidence level was determined, an evidence grade was assigned. AAP policy stipulates that the evidence supporting each KAS be prospectively identified, appraised, and summarized, and an explicit link between quality levels and the grade of recommendation must be defined. Possible grades of recommendations range from “A” to “D,” with “A” being the highest:
grade A: consistent level A studies;
grade B: consistent level B or extrapolations from level A studies;
grade C: level C studies or extrapolations from level B or level C studies;
grade D: level D evidence or troublingly inconsistent or inconclusive studies of any level; and
level X: not an explicit level of evidence as outlined by the Centre for Evidence-Based Medicine. This level is reserved for interventions that are unethical or impossible to test in a controlled or scientific fashion and for which the preponderance of benefit or harm is overwhelming, precluding rigorous investigation.
Guided by the evidence quality and grade, the subcommittee developed 7 KASs for the evaluation, diagnosis, and treatment of ADHD in children and adolescents (see Table 1).
TABLE 1.
Summary of KASs for Diagnosing, Evaluating, and Treating ADHD in Children and Adolescents
| KASs | Evidence Quality, Strength of Recommendation |
|---|---|
| KAS 1: The pediatrician or other PCC should initiate an evaluation for ADHD for any child or adolescent age 4 years to the 18th birthday who presents with academic or behavioral problems and symptoms of inattention, hyperactivity, or impulsivity. | Grade B, strong recommendation |
| KAS 2: To make a diagnosis of ADHD, the PCC should determine that DSM-5 criteria have been met, including documentation of symptoms and impairment in more than 1 major setting (ie, social, academic, or occupational), with information obtained primarily from reports from parents or guardians, teachers, other school personnel, and mental health clinicians who are involved in the child or adolescent’s care. The PCC should also rule out any alternative cause. | Grade B, strong recommendation |
| KAS 3: In the evaluation of a child or adolescent for ADHD, the PCC should include a process to at least screen for comorbid conditions, including emotional or behavioral conditions (eg, anxiety depression, oppositional defiant disorder, conduct disorders, substance use), developmental conditions (eg, learning and language disorders, autism spectrum disorders), and physical conditions (eg, tics, sleep apnea). | Grade B, strong recommendation |
| KAS 4: ADHD is a chronic condition; therefore, the PCC should manage children and adolescents with ADHD in the same manner that they would children and youth with special health care needs, following the principles of the chronic care model and the medical home. | Grade B, strong recommendation |
| KAS 5a: For preschool-aged children (age 4 years to the sixth birthday) with ADHD, the PCC should prescribe evidence-based PTBM and/or behavioral classroom interventions as the first line of treatment, if available. | Grade A, strong recommendation for PTBM |
| Methylphenidate may be considered if these behavioral interventions do not provide significant improvement and there is moderate-to-severe continued disturbance in the 4-through 5-year-old child’s functioning. In areas in which evidence-based behavioral treatments are not available, the clinician needs to weigh the risks of starting medication before the age of 6 years against the harm of delaying treatment. | Grade B, strong recommendation for methylphenidate |
| KAS 5b. For elementary and middle school-aged children (age 6 years to the 12th birthday) with ADHD, the PCC should prescribe FDA-approved medications for ADHD, along with PTBM and/or behavioral classroom intervention (preferably both PTBM and behavioral classroom interventions). Educational interventions and individualized instructional supports, including school environment, class placement, instructional placement, and behavioral supports, are a necessary part of any treatment plan and often include an IEP or a rehabilitation plan (504 plan). | Grade A, strong recommendation for medications Grade A, strong recommendation for training and behavioral treatments for ADHD with family and school |
| KAS 5c. For adolescents (age 12 years to the 18th birthday) with ADHD, the PCC should prescribe FDA-approved medications for ADHD with the adolescent’s assent. The PCC is encouraged to prescribe evidence-based training interventions and/or behavioral interventions as treatment of ADHD, if available. Educational interventions and individualized instructional supports, including school environment, class placement, instructional placement, and behavioral supports, are a necessary part of any treatment plan and often include an IEP or a rehabilitation plan (504 plan). | Grade A, strong recommendation for medications Grade A, strong recommendation for training and behavioral treatments for ADHD with the family and school |
| KAS 6. The PCC should titrate doses of medication for ADHD to achieve maximum benefit with tolerable side effects. | Grade B, strong recommendation |
| KAS 7. The PCC, if trained or experienced in diagnosing comorbid conditions, may initiate treatment of such conditions or make a referral to an appropriate subspecialist for treatment. After detecting possible comorbid conditions, if the PCC is not trained or experienced in making the diagnosis or initiating treatment, the patient should be referred to an appropriate subspecialist to make the diagnosis and initiate treatment. | Grade C, recommendation |
These KASs provide for consistent and high-quality care for children and adolescents who may have symptoms suggesting attention disorders or problems as well as for their families. In developing the 7 KASs, the subcommittee considered the requirements for establishing the diagnosis; the prevalence of ADHD; the effect of untreated ADHD; the efficacy and adverse effects of treatment; various long-term outcomes; the importance of coordination between pediatric and mental health service providers; the value of the medical home; and the common occurrence of comorbid conditions, the importance of addressing them, and the effects of not treating them.
The subcommittee members with the most epidemiological experience assessed the strength of each recommendation and the quality of evidence supporting each draft KAS.
Peer Review
The guidelines and PoCA underwent extensive peer review by more than 30 internal stakeholders (eg, AAP committees, sections, councils, and task forces) and external stakeholder groups identified by the subcommittee. The resulting comments were compiled and reviewed by the chair and vice chair; relevant changes were incorporated into the draft, which was then reviewed by the full subcommittee.
KASS FOR THE EVALUATION, DIAGNOSIS, TREATMENT, AND MONITORING OF CHILDREN AND ADOLESCENTS WITH ADHD
KAS 1
The pediatrician or other PCC should initiate an evaluation for ADHD for any child or adolescent age 4 years to the 18th birthday who presents with academic or behavioral problems and symptoms of inattention, hyperactivity, or impulsivity (Table 2). (Grade B: strong recommendation.)
TABLE 2.
KAS 1: The pediatrician or other PCC should initiate an evaluation for ADHD for any child or adolescent age 4 years to the 18th birthday who presents with academic or behavioral problems and symptoms of inattention, hyperactivity, or impulsivity. (Grade B: strong recommendation.)
| Aggregate evidence quality | Grade B |
|---|---|
| Benefits | ADHD goes undiagnosed in a considerable number of children and adolescents. Primary care clinicians’ more-rigorous identification of children with these problems is likely to decrease the rate of undiagnosed and untreated ADHD in children and adolescents. |
| Risks, harm, cost | Children and adolescents in whom ADHD is inappropriately diagnosed may be labeled inappropriately, or another condition may be missed, and they may receive treatments that will not benefit them. |
| Benefit-harm | The high prevalence of ADHD and limited mental health resources require primary care pediatricians and other PCCs to play |
| assessment | a significant role in the care of patients with ADHD and assist them to receive appropriate diagnosis and treatment. Treatments available have good evidence of efficacy and a lack of treatment has the risk of impaired outcomes. |
| Intentional vagueness | There are limits between what a PCC can address and what should be referred to a subspecialist because of varying degrees of skills and comfort levels present among the former. |
| Role of patient preferences | Success with treatment is dependent on patient and family preference, which need to be taken into account. |
| Exclusions | None. |
| Strength | Strong recommendation. |
| Key references | Wolraich et al31; Visser et al28; Thomas et al8; Egger et al30 |
The basis for this recommendation is essentially unchanged from the previous guideline. As noted, ADHD is the most common neurobehavioral disorder of childhood, occurring in approximately 7% to 8% of children and youth.8,18,28,29 Hence, the number of children with this condition is far greater than can be managed by the mental health system.4 There is evidence that appropriate diagnosis can be accomplished in the primary care setting for children and adolescents.30,31 Note that there is insufficient evidence to recommend diagnosis or treatment for children younger than 4 years (other than parent training in behavior management [PTBM], which does not require a diagnosis to be applied); in instances in which ADHD-like symptoms in children younger than 4 years bring substantial impairment, PCCs can consider making a referral for PTBM.
KAS 2
To make a diagnosis of ADHD, the PCC should determine that DSM-5 criteria have been met, including documentation of symptoms and impairment in more than 1 major setting (ie, social, academic, or occupational), with information obtained primarily from reports from parents or guardians, teachers, other school personnel, and mental health clinicians who are involved in the child or adolescent’s care. The PCC should also rule out any alternative cause (Table 3). (Grade B: strong recommendation.)
TABLE 3.
KAS 2: To make a diagnosis of ADHD, the PCC should determine that DSM-5 criteria have been met, including documentation of symptoms and impairment in more than 1 major setting (ie, social, academic, or occupational), with information obtained primarily from reports from parents or guardians, teachers, other school personnel, and mental health clinicians who are involved in the child or adolescent’s care. The PCC should also rule out any alternative cause. (Grade B: strong recommendation.)
| Aggregate evidence quality | Grade B |
|---|---|
| Benefits | Use of the DSM-5 criteria has led to more uniform categorization of the condition across professional disciplines. The criteria are essentially unchanged from the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV), for children up to their 18th birthday except that DSM-IV required onset prior to age 7 for a diagnosis, while DSM-5 requires onset prior to age 12. |
| Risks, harm, cost | The DSM-5 does not specifically state that symptoms must be beyond expected levels for developmental (rather than chronologic) age to qualify for an ADHD diagnosis, which may lead to some misdiagnoses in children with developmental disorders. |
| Benefit-harm assessment | The benefits far outweigh the harm. |
| Intentional vagueness | None. |
| Role of patient preferences | Although there is some stigma associated with mental disorder diagnoses, resulting in some families preferring other diagnoses, the need for better clarity in diagnoses outweighs this preference. |
| Exclusions | None. |
| Strength | Strong recommendation. |
| Key references | Evans et al25; McGoey et al42; Young43; Sibley et al46 |
The American Psychiatric Association developed the DSM-5 using expert consensus and an expanding research foundation.32 The DSM-5 system is used by professionals in psychiatry, psychology, health care systems, and primary care; it is also well established with third-party payers.
The DSM-5 criteria define 4 dimensions of ADHD:
attention-deficit/hyperactivity disorder primarily of the inattentive presentation (ADHD/I) (314.00 [F90.0]);
attention-deficit/hyperactivity disorder primarily of the hyperactive-impulsive presentation (ADHD/HI) (314.01 [F90.1]);
attention-deficit/hyperactivity disorder combined presentation (ADHD/C) (314.01 [F90.2]); and
ADHD other specified and unspecified ADHD (314.01 [F90.8]).
As with the previous guideline recommendations, the DSM-5 classification criteria are based on the best available evidence for ADHD diagnosis and are the standard most frequently used by clinicians and researchers to render the diagnosis and document its appropriateness for a given child. The use of neuropsychological testing has not been found to improve diagnostic accuracy in most cases, although it may have benefit in clarifying the child or adolescent’s learning strengths and weaknesses. (See the PoCA for more information on implementing this KAS.)
Special Circumstances: Preschool-Aged Children (Age 4 Years to the Sixth Birthday)
There is evidence that the diagnostic criteria for ADHD can be applied to preschool-aged children.33–39 A review of the literature, including the multisite study of the efficacy of methylphenidate in preschool-aged children, found that the DSM-5 criteria could appropriately identify children with ADHD.25
To make a diagnosis of ADHD in preschool-aged children, clinicians should conduct a clinical interview with parents, examine and observe the child, and obtain information from parents and teachers through DSM-based ADHD rating scales.40 Normative data are available for the DSM-5–based rating scales for ages 5 years to the 18th birthday.41 There are, however, minimal changes in the specific behaviors from the DSM-IV, on which all the other DSM-based ADHD rating scales obtained normative data. Both the ADHD Rating Scale-IV and the Conners Rating Scale have preschool-age normative data based on the DSM-IV. The specific behaviors in the DSM-5 criteria for ADHD are the same for all children younger than 18 years (ie, preschool-aged children, elementary and middle school-aged children, and adolescents) and are only minimally different from the DSM-IV. Hence, if clinicians do not have the ADHD Rating Scale-5 or the ADHD Rating Scale-IV Preschool Version,42 any other DSM-based scale can be used to provide a systematic method for collecting information from parents and teachers, even in the absence of normative data.
Pediatricians and other PCCs should be aware that determining the presence of key symptoms in this age group has its challenges, such as observing symptoms across multiple settings as required by the DSM-5, particularly among children who do not attend a preschool or child care program. Here, too, focused checklists can be used to aid in the diagnostic evaluation.
PTBM is the recommended primary intervention for preschool-aged children with ADHD as well as children with ADHD-like behaviors whose diagnosis is not yet verified. This type of training helps parents learn age-appropriate developmental expectations, behaviors that strengthen the parent-child relationship, and specific management skills for problem behaviors. Clinicians do not need to have made an ADHD diagnosis before recommending PTBM because PTBM has documented effectiveness with a wide variety of problem behaviors, regardless of etiology. In addition, the intervention’s results may inform the subsequent diagnostic evaluation. Clinicians are encouraged to recommend that parents complete PTBM, if available, before assigning an ADHD diagnosis.
After behavioral parent training is implemented, the clinician can obtain information from parents and teachers through DSM-5–based ADHD rating scales. The clinician may obtain reports about the parents’ ability to manage their children and about the child’s core symptoms and impairments. Referral to an early intervention program or enrolling in a PTBM program can help provide information about the child’s behavior in other settings or with other observers. The evaluators for these programs and/or early childhood special education teachers may be useful observers, as well.
Special Circumstances: Adolescents (Age 12 Years to the 18th Birthday)
Obtaining teacher reports for adolescents is often more challenging than for younger children because many adolescents have multiple teachers. Likewise, an adolescent’s parents may have less opportunity to observe their child’s behaviors than they did when the child was younger. Furthermore, some problems experienced by children with ADHD are less obvious in adolescents than in younger children because adolescents are less likely to exhibit overt hyperactive behavior Of note, adolescents’ reports of their own behaviors often differ from other observers because they tend to minimize their own problematic behaviors43–45
Despite these difficulties, clinicians need to try to obtain information from at least 2 teachers or other sources, such as coaches, school guidance counselors, or leaders of community activities in which the adolescent participates.46 For the evaluation to be successful, it is essential that adolescents agree with and participate in the evaluation. Variability in ratings is to be expected because adolescents’ behavior often varies between different classrooms and with different teachers. Identifying reasons for any variability can provide valuable clinical insight into the adolescent’s problems.
Note that, unless they previously received a diagnosis, to meet DSM-5 criteria for ADHD, adolescents must have some reported or documented manifestations of inattention or hyperactivity/impulsivity before age 12. Therefore, clinicians must establish that an adolescent had manifestations of ADHD before age 12 and strongly consider whether a mimicking or comorbid condition, such as substance use, depression, and/or anxiety, is present.46
In addition, the risks of mood and anxiety disorders and risky sexual behaviors increase during adolescence, as do the risks of intentional self-harm and suicidal behaviors.31 Clinicians should also be aware that adolescents are at greater risk for substance use than are younger children44,45,47 Certain substances, such as marijuana, can have effects that mimic ADHD; adolescent patients may also attempt to obtain stimulant medication to enhance performance (ie, academic, athletic, etc) by feigning symptoms.48
Trauma experiences, posttraumatic stress disorder, and toxic stress are additional comorbidities and risk factors of concern.
Special Circumstances: Inattention or Hyperactivity/impulsivity (Problem Level)
Teachers, parents, and child health professionals typically encounter children who demonstrate behaviors relating to activity level, impulsivity, and inattention but who do not fully meet DSM-5 criteria. When assessing these children, diagnostic criteria should be closely reviewed, which may require obtaining more information from other settings and sources. Also consider that these symptoms may suggest other problems that mimic ADHD.
Behavioral interventions, such as PTBM, are often beneficial for children with hyperactive/impulsive behaviors who do not meet full diagnostic criteria for ADHD. As noted previously, these programs do not require a specific diagnosis to be beneficial to the family. The previous guideline discussed the diagnosis of problem-level concerns on the basis of the Diagnostic and Statistical Manual for Primary Care (DSM-PC), Child and Adolescent Version,49 and made suggestions for treatment and care. The DSM-PC was published in 1995, however, and it has not been revised to be compatible with the DSM-5. Therefore, the DSM-PC cannot be used as a definitive source for diagnostic codes related to ADHD and comorbid conditions, although it can be used conceptually as a resource for enriching the understanding of problem-level manifestations.
KAS 3
In the evaluation of a child or adolescent for ADHD, the PCC should include a process to at least screen for comorbid conditions, including emotional or behavioral conditions (eg, anxiety, depression, oppositional defiant disorder, conduct disorders, substance use), developmental conditions (eg, learning and language disorders, autism spectrum disorders), and physical conditions (eg, tics, sleep apnea) (Table 4). (Grade B: strong recommendation.)
TABLE 4.
KAS 3: In the evaluation of a child or adolescent for ADHD, the PCC should include a process to at least screen for comorbid conditions, including emotional or behavioral conditions (eg, anxiety, depression, oppositional defiant disorder, conduct disorders, substance use), developmental conditions (eg, learning and language disorders, autism spectrum disorders), and physical conditions (eg, tics, sleep apnea). (Grade B: strong recommendation.)
| Aggregate evidence quality | Grade B |
|---|---|
| Benefits | Identifying comorbid conditions is important in developing the most appropriate treatment plan for the child or adolescent with ADHD. |
| Risks, harm, cost | The major risk is misdiagnosing the comorbid condition(s) and providing inappropriate care. |
| Benefit-harm assessment | There is a preponderance of benefits over harm. |
| Intentional vagueness | None. |
| Role of patient preferences | None. |
| Exclusions | None. |
| Strength | Strong recommendation. |
| Key references | Cuffe et al51; Pastor and Reuben52; Bieiderman et al53; Bieiderman et al54; Bieiderman et al72; Crabtree et al57; LeBourgeois et al58; Chan115; Newcorn et al60; Sung et al61; Larson et al66; Mahajan et al65; Antshel et al64; Rothenberger and Roessner63; Froehlich et al62 |
The majority of both boys and girls with ADHD also meet diagnostic criteria for another mental disorder.17,18 A variety of other behavioral, developmental, and physical conditions can be comorbid in children and adolescents who are evaluated for ADHD, including emotional or behavioral conditions or a history of these problems. These include but are not limited to learning disabilities, language disorder, disruptive behavior, anxiety, mood disorders, tic disorders, seizures, autism spectrum disorder, developmental coordination disorder, and sleep disorders.50–66 In some cases, the presence of a comorbid condition will alter the treatment of ADHD.
The SDBP is developing a clinical practice guideline to support clinicians in the diagnosis of treatment of “complex ADHD,” which includes ADHD with comorbid developmental and/or mental health conditions.67
Special Circumstances: Adolescents (Age 12 Years to the 18th Birthday)
At a minimum, clinicians should assess adolescent patients with newly diagnosed ADHD for symptoms and signs of substance use, anxiety, depression, and learning disabilities. As noted, all 4 are common comorbid conditions that affect the treatment approach. These comorbidities make it important for the clinician to consider sequencing psychosocial and medication treatments to maximize the impact on areas of greatest risk and impairment while monitoring for possible risks such as stimulant abuse or suicidal ideation.
KAS 4
ADHD is a chronic condition; therefore, the PCC should manage children and adolescents with ADHD in the same manner that they would children and youth with special health care needs, following the principles of the chronic care model and the medical home (Table 5). (Grade B: strong recommendation.)
TABLE 5.
KAS 4: ADHD is a chronic condition; therefore, the PCC should manage children and adolescents with ADHD in the same manner that they would children and youth with special health care needs, following the principles of the chronic care model and the medical home. (Grade B: strong recommendation.)
| Aggregate evidence quality | Grade B |
|---|---|
| Benefits | The recommendation describes the coordinated services that are most appropriate to manage the condition. |
| Risks, harm, cost | Providing these services may be more costly. |
| Benefit-harm assessment | There is a preponderance of benefits over harm. |
| Intentional vagueness | None. |
| Role of patient preferences | Family preference in how these services are provided is an important consideration, because it can increase adherence. |
| Exclusions | None |
| Strength | Strong recommendation. |
| Key references | Brito et al69; Biederman et al72; Scheffler et al74; Barbaresi et al75; Chang et al71; Chang et al78; Lichtenstein et al77; Harstad and Levy80 |
As in the 2 previous guidelines, this recommendation is based on the evidence that for many individuals, ADHD causes symptoms and dysfunction over long periods of time, even into adulthood. Available treatments address symptoms and function but are usually not curative. Although the chronic illness model has not been specifically studied in children and adolescents with ADHD, it has been effective for other chronic conditions, such as asthma.68 In addition, the medical home model has been accepted as the preferred standard of care for children with chronic conditions.69
The medical home and chronic illness approach may be particularly beneficial for parents who also have ADHD themselves. These parents can benefit from extra support to help them follow a consistent schedule for medication and behavioral programs.
Authors of longitudinal studies have found that ADHD treatments are frequently not maintained over time13 and impairments persist into adulthood.70 It is indicated in prospective studies that patients with ADHD, whether treated or not, are at increased risk for early death, suicide, and increased psychiatric comorbidity, particularly substance use disorders.71,72 They also have lower educational achievement than those without ADHD73,74 and increased rates of incarceration.75–77 Treatment discontinuation also places individuals with ADHD at higher risk for catastrophic outcomes, such as motor vehicle crashes78,79; criminality, including drug-related crimes77 and violent reoffending76; depression71; interpersonal issues80; and other injuries.81,82
To continue providing the best care, it is important for a treating pediatrician or other PCC to engage in bidirectional communication with teachers and other school personnel as well as mental health clinicians involved in the child or adolescent’s care. This communication can be difficult to achieve and is discussed in both the PoCA and the section on systemic barriers to the care of children and adolescents with ADHD in the Supplemental Information, as is the medical home model.69
Special Circumstances: Inattention or Hyperactivity/Impulsivity (Problem Level)
Children with inattention or hyperactivity/impulsivity at the problem level, as well as their families, may also benefit from the chronic illness and medical home principles.
Recommendations for the Treatment of Children and Adolescents With ADHD: KAS 5a, 5b, and 5c
Recommendations vary depending on the patient’s age and are presented for the following age ranges:
preschool-aged children: age 4 years to the sixth birthday;
elementary and middle school–aged children: age 6 years to the 12th birthday; and
adolescents: age 12 years to the 18th birthday.
The KASs are presented, followed by information on medication, psychosocial treatments, and special circumstances.
KAS 5a
For preschool-aged children (age 4 years to the sixth birthday) with ADHD, the PCC should prescribe evidence-based behavioral PTBM and/or behavioral classroom interventions as the first line of treatment, if available (grade A: strong recommendation). Methylphenidate may be considered if these behavioral interventions do not provide significant improvement and there is moderate-to-severe continued disturbance in the 4-through 5-year-old child’s functioning. In areas in which evidence-based behavioral treatments are not available, the clinician needs to weigh the risks of starting medication before the age of 6 years against the harm of delaying treatment (Table 6). (Grade B: strong recommendation.)
TABLE 6.
KAS 5a: For preschool-aged children (age 4 years to the sixth birthday) with ADHD, the PCC should prescribe evidence-based behavioral PTBM and/or behavioral classroom interventions as the first line of treatment, if available (grade A: strong recommendation). Methylphenidate may be considered if these behavioral interventions do not provide significant improvement and there is moderate-to-severe continued disturbance in the 4-through 5-year-old child’s functioning. In areas in which evidence-based behavioral treatments are not available, the clinician needs to weigh the risks of starting medication before the age of 6 years against the harm of delaying treatment (grade B: strong recommendation).
| Aggregate evidence quality | Grade A for PTBM; Grade B for methylphenidate |
|---|---|
| Benefits | Given the risks of untreated ADHD, the benefits outweigh the risks. |
| Risks, harm, cost | Both therapies increase the cost of care; PTBM requires a high level of family involvement, whereas methylphenidate has some potential adverse effects. |
| Benefit-harm assessment | Both PTBM and methylphenidate have relatively low risks; initiating treatment at an early age, before children experience repeated failure, has additional benefits. Thus, the benefits outweigh the risks. |
| Intentional vagueness | None. |
| Role of patient preferences | Family preference is essential in determining the treatment plan. |
| Exclusions | None. |
| Strength | Strong recommendation. |
| Key references | Greenhill et al83; Evans et al25 |
A number of special circumstances support the recommendation to initiate PTBM as the first treatment of preschool-aged children (age 4 years to the sixth birthday) with ADHD.25,83 Although it was limited to children who had moderate-to-severe dysfunction, the largest multisite study of methylphenidate use in preschool-aged children revealed symptom improvements after PTBM alone.83 The overall evidence for PTBM among preschoolers is strong.
PTBM programs for preschool-aged children are typically group programs and, although they are not always paid for by health insurance, they may be relatively low cost. One evidence-based PTBM, parent-child interaction therapy, is a dyadic therapy for parent and child. The PoCA contains criteria for the clinician’s use to assess the quality of PTBM programs. If the child attends preschool, behavioral classroom interventions are also recommended. In addition, preschool programs (such as Head Start) and ADHD-focused organizations (such as CHADD84) can also provide behavioral supports. The issues related to referral, payment, and communication are discussed in the section on systemic barriers in the Supplemental Information.
In areas in which evidence-based behavioral treatments are not available, the clinician needs to weigh the risks of starting methylphenidate before the age of 6 years against the harm of delaying diagnosis and treatment. Other stimulant or nonstimulant medications have not been adequately studied in children in this age group with ADHD.
KAS 5b
For elementary and middle school–aged children (age 6 years to the 12th birthday) with ADHD, the PCC should prescribe US Food and Drug Administration (FDA)–approved medications for ADHD, along with PTBM and/or behavioral classroom intervention (preferably both PTBM and behavioral classroom interventions). Educational interventions and individualized instructional supports, including school environment, class placement, instructional placement, and behavioral supports, are a necessary part of any treatment plan and often include an Individualized Education Program (IEP) or a rehabilitation plan (504 plan) (Table 7). (Grade A: strong recommendation for medications; grade A: strong recommendation for PTBM training and behavioral treatments for ADHD implemented with the family and school.)
TABLE 7.
KAS 5b: For elementary and middle school–aged children (age 6 years to the 12th birthday) with ADHD, the PCC should prescribe US Food and Drug Administration (FDA)–approved medications for ADHD, along with PTBM and/or behavioral classroom intervention (preferably both PTBM and behavioral classroom interventions). Educational interventions and individualized instructional supports, including school environment, class placement, instructional placement, and behavioral supports, are a necessary part of any treatment plan and often include an Individualized Education Program (IEP) or a rehabilitation plan (504 plan). (Grade A: strong recommendation for medications; grade A: strong recommendation for PTBM training and behavioral treatments for ADHD implemented with the family and school.)
| Aggregate evidence quality | Grade A for Treatment with FDA-Approved Medications; Grade A for Training and Behavioral Treatments for ADHD With the Family and School. |
|---|---|
| Benefits | Both behavioral therapy and FDA-approved medications have been shown to reduce behaviors associated with ADHD and to improve function. |
| Risks, harm, cost | Both therapies increase the cost of care. Psychosocial therapy requires a high level of family and/or school involvement and may lead to increased family conflict, especially if treatment is not successfully completed. FDA-approved medications may have some adverse effects and discontinuation of medication is common among adolescents. |
| Benefit-harm assessment | Given the risks of untreated ADHD, the benefits outweigh the risks. |
| Intentional vagueness | None. |
| Role of patient preferences | Family preference, including patient preference, is essential in determining the treatment plan and enhancing adherence. |
| Exclusions | None. |
| Strength | Strong recommendation. |
| Key references | Evans et al25; Barbaresi et al73; Jain et al103; Brown and Bishop104; Kambeitz et al105; Bruxel et al106; Kieling et al107; Froehlich et al108; Joensen et al109 |
The evidence is particularly strong for stimulant medications; it is sufficient, but not as strong, for atomoxetine, extended-release guanfacine, and extended-release clonidine, in that order (see the Treatment section, and see the PoCA for more information on implementation).
KAS 5c
For adolescents (age 12 years to the 18th birthday) with ADHD, the PCC should prescribe FDA-approved medications for ADHD with the adolescent’s assent (grade A: strong recommendation). The PCC is encouraged to prescribe evidence-based training interventions and/or behavioral interventions as treatment of ADHD, if available. Educational interventions and individualized instructional supports, including school environment, class placement, instructional placement, and behavioral supports, are a necessary part of any treatment plan and often include an IEP or a rehabilitation plan (504 plan) (Table 8). (Grade A: strong recommendation.)
TABLE 8.
KAS 5c: For adolescents (age 12 years to the 18th birthday) with ADHD, the PCC should prescribe FDA-approved medications for ADHD with the adolescent’s assent (grade A: strong recommendation). The PCC is encouraged to prescribe evidence-based training interventions and/or behavioral interventions as treatment of ADHD, if available. Educational interventions and individualized instructional supports, including school environment, class placement, instructional placement, and behavioral supports, are a necessary part of any treatment plan and often include an IEP or a rehabilitation plan (504 plan). (Grade A: strong recommendation.)
| Aggregate evidence quality | Grade A for Medications; Grade A for Training and Behavioral Therapy |
|---|---|
| Benefits | Training interventions, behavioral therapy, and FDA-approved medications have been demonstrated to reduce behaviors associated with ADHD and to improve function. |
| Risks, harm, cost | Both therapies increase the cost of care. Psychosocial therapy requires a high level of family and/or school involvement and may lead to unintended increased family conflict, especially if treatment is not successfully completed. FDA-approved medications may have some adverse effects, and discontinuation of medication is common among adolescents. |
| Benefit-harm assessment | Given the risks of untreated ADHD, the benefits outweigh the risks. |
| Intentional vagueness | None. |
| Role of patient preferences | Family preference, including patient preference, is likely to predict engagement and persistence with a treatment. |
| Exclusions | None. |
| Strength | Strong recommendation. |
| Key references | Evans et al25; Webster-Stratton et al87; Evans et al95; Fabiano et al93; Sibley and Graziano et al94; Langberg et al96; Schultz et al97; Brown and Bishop104; Kambeitz et al105; Bruxel et al106; Froehlich et al108; Joensen et al109 |
Transition to adult care is an important component of the chronic care model for ADHD. Planning for the transition to adult care is an ongoing process that may culminate after high school or, perhaps, after college. To foster a smooth transition, it is best to introduce components at the start of high school, at about 14 years of age, and specifically focus during the 2 years preceding high school completion.
Psychosocial Treatments
Some psychosocial treatments for children and adolescents with ADHD have been demonstrated to be effective for the treatment of ADHD, including behavioral therapy and training interventions.24–26,85 The diversity of interventions and outcome measures makes it challenging to assess a meta-analysis of psychosocial treatment’s effects alone or in association with medication treatment. As with medication treatment, the long-term positive effects of psychosocial treatments have yet to be determined. Nonetheless, ongoing adherence to psychosocial treatment is a key contributor to its beneficial effects, making implementation of a chronic care model for child health important to ensure sustained adherence.86
Behavioral therapy involves training adults to influence the contingencies in an environment to improve the behavior of a child or adolescent in that setting. It can help parents and school personnel learn how to effectively prevent and respond to adolescent behaviors such as interrupting, aggression, not completing tasks, and not complying with requests. Behavioral parent and classroom training are well-established treatments with preadolescent children.25,87,88 Most studies comparing behavior therapy to stimulants indicate that stimulants have a stronger immediate effect on the 18 core symptoms of ADHD. Parents, however, were more satisfied with the effect of behavioral therapy, which addresses symptoms and functions in addition to ADHD’s core symptoms. The positive effects of behavioral therapies tend to persist, but the positive effects of medication cease when medication stops. Optimal care is likely to occur when both therapies are used, but the decision about therapies is heavily dependent on acceptability by, and feasibility for, the family.
Training interventions target skill development and involve repeated practice with performance feedback over time, rather than modifying behavioral contingencies in a specific setting. Less research has been conducted on training interventions compared to behavioral treatments; nonetheless, training interventions are well-established treatments to target disorganization of materials and time that are exhibited by most youth with ADHD; it is likely that they will benefit younger children, as well.25,89 Some training interventions, including social skills training, have not been shown to be effective for children with ADHD.25
Some nonmedication treatments for ADHD-related problems have either too little evidence to recommend them or have been found to have little or no benefit. These include mindfulness, cognitive training, diet modification, EEG biofeedback, and supportive counseling. The suggestion that cannabidiol oil has any effect on ADHD is anecdotal and has not been subjected to rigorous study. Although it is FDA approved, the efficacy for external trigeminal nerve stimulation (eTNS) is documented by one 5-week randomized controlled trial with just 30 participants receiving eTNS.90 To date, there is no long-term safety and efficacy evidence for eTNS. Overall, the current evidence supporting treatment of ADHD with eTNS is sparse and in no way approaches the robust strength of evidence documented for established medication and behavioral treatments for ADHD; therefore, it cannot be recommended as a treatment of ADHD without considerably more extensive study on its efficacy and safety.
Special Circumstances: Adolescents
Much less research has been published on psychosocial treatments with adolescents than with younger children. PTBM has been modified to include the parents and adolescents in sessions together to develop a behavioral contract and improve parent-adolescent communication and problem-solving (see above).91 Some training programs also include motivational interviewing approaches. The evidence for this behavioral family approach is mixed and less strong than PTBM with preadolescent children92–94 Adolescents’ responses to behavioral contingencies are more varied than those of younger children because they can often effectively obstruct behavioral contracts, increasing parent-adolescent conflict.
Training approaches that are focused on school functioning skills have consistently revealed benefits for adolescents.95–97 The greatest benefits from training interventions occur when treatment is continued over an extended period of time, performance feedback is constructive and frequent, and the target behaviors are directly applicable to the adolescent’s daily functioning.
Overall, behavioral family approaches may be helpful to some adolescents and their families, and school-based training interventions are well established.25,94 Meaningful improvements in functioning have not been reported from cognitive behavioral approaches.
Medication for ADHD
Preschool-aged children may experience increased mood lability and dysphoria with stimulant medications.83 None of the nonstimulants have FDA approval for use in preschool-aged children. For elementary school–aged students, the evidence is particularly strong for stimulant medications and is sufficient, but less strong, for atomoxetine, extended-release guanfacine, and extended-release clonidine (in that order). The effect size for stimulants is 1.0 and for nonstimulants is 0.7. An individual’s response to methylphenidate verses amphetamine is idiosyncratic, with approximately 40% responding to both and about 40% responding to only 1. The subtype of ADHD does not appear to be a predictor of response to a specific agent. For most adolescents, stimulant medications are highly effective in reducing ADHD’s core symptoms.73
Stimulant medications have an effect size of around 1.0 (effect size = [treatment M − control M)/control SD]) for the treatment of ADHD.98 Among nonstimulant medications, 1 selective norepinephrine reuptake inhibitor, atomoxetine,99,100 and 2 selective α-2 adrenergic agonists, extended-release guanfacine101,102 and extended-release clonidine,103 have also demonstrated efficacy in reducing core symptoms among school-aged children and adolescents, although their effect sizes, —around 0.7 for ah 3, are less robust than that of stimulant medications. Norepinephrine reuptake inhibitors and α-2 adrenergic agonists are newer medications, so, in general, the evidence base supporting them is considerably less than that for stimulants, although it was adequate for FDA approval.
A free list of the currently available, FDA-approved medications for ADHD is available online at www.ADHDMedicationGuide.com. Each medication’s characteristics are provided to help guide the clinician’s prescription choice. With the expanded list of medications, it is less likely that PCCs need to consider the off-label use of other medications. The section on systemic barriers in the Supplemental Information provides suggestions for fostering more realistic and effective payment and communication systems.
Because of the large variability in patients’ response to ADHD medication, there is great interest in pharmacogenetic tools that can help clinicians predict the best medication and dose for each child or adolescent. At this time, however, the available scientific literature does not provide sufficient evidence to support their clinical utility given that the genetic variants assayed by these tools have generally not been fully studied with respect to medication effects on ADHD-related symptoms and/or impairment, study findings are inconsistent, or effect sizes are not of sufficient size to ensure clinical utility.104–109 For that reason, these pharmacogenetics tools are not recommended. In addition, these tests may cost thousands of dollars and are typically not covered by insurance. For a pharmacogenetics tool to be recommended for clinical use, studies would need to reveal (1) the genetic variants assayed have consistent, replicated associations with medication response; (2) knowledge about a patient’s genetic profile would change clinical decision-making, improve outcomes and/or reduce costs or burden; and (3) the acceptability of the test’s operating characteristics has been demonstrated (eg, sensitivity, specificity, and reliability).
Side Effects
Stimulants’ most common short-term adverse effects are appetite loss, abdominal pain, headaches, and sleep disturbance. The Multimodal Treatment of Attention Deficit Hyperactivity Disorder (MTA) study results identified stimulants as having a more persistent effect on decreasing growth velocity compared to most previous studies.110 Diminished growth was in the range of 1 to 2 cm from predicted adult height. The results of the MTA study were particularly noted among children who were on higher and more consistently administered doses of stimulants.110 The effects diminished by the third year of treatment, but no compensatory rebound growth was observed.110 An uncommon significant adverse effect of stimulants is the occurrence of hallucinations and other psychotic symptoms.111
Stimulant medications, on average, increase patient heart rate (HR) and blood pressure (BP) to a mild and clinically insignificant degree (average increases: 1–2 beats per minute for HR and 1–4 mm Hg for systolic and diastolic BP).112 However, because stimulants have been linked to more substantial increases in HR and BP in a subset of individuals (5%–15%), clinicians are encouraged to monitor these vital signs in patients receiving stimulant treatment.112 Although concerns have been raised about sudden cardiac death among children and adolescents using stimulant and medications,113 it is an extremely rare occurrence. In fact, stimulant medications have not been shown to increase the risk of sudden death beyond that observed in children who are not receiving stimulants.114–118 Nevertheless, before initiating therapy with stimulant medications, it is important to obtain the child or adolescent’s history of specific cardiac symptoms in addition to the family history of sudden death, cardiovascular symptoms, Wolff-Parkinson-White syndrome, hypertrophic cardiomyopathy, and long QT syndrome. If any of these risk factors are present, clinicians should obtain additional evaluation to ascertain and address potential safety concerns of stimulant medication use by the child or adolescent.112,114
Among nonstimulants, the risk of serious cardiovascular events is extremely low, as it is for stimulants. The 3 nonstimulant medications that are FDA approved to treat ADHD (ie, atomoxetine, guanfacine, and clonidine) may be associated with changes in cardiovascular parameters or other serious cardiovascular events. These events could include increased HR and BP for atomoxetine and decreased HR and BP for guanfacine and clonidine. Clinicians are recommended to not only obtain the personal and family cardiac history, as detailed above, but also to perform additional evaluation if risk factors are present before starting nonstimulant medications (ie, perform an electrocardiogram [ECG] and possibly refer to a pediatric cardiologist if the ECG is not normal).112
Additional adverse effects of atomoxetine include initial somnolence and gastrointestinal tract symptoms, particularly if the dosage is increased too rapidly, and decreased appetite.119–122 Less commonly, an increase in suicidal thoughts has been found; this is noted by an FDA black box warning. Extremely rarely, hepatitis has been associated with atomoxetine. Atomoxetine has also been linked to growth delays compared to expected trajectories in the first 1 to 2 years of treatment, with a return to expected measurements after 2 to 3 years of treatment, on average. Decreases were observed among those who were taller or heavier than average before treatment.123
For extended-release guanfacine and extended-release clonidine, adverse effects include somnolence, dry mouth, dizziness, irritability, headache, bradycardia, hypotension, and abdominal pain.30,124,125 Because rebound hypertension after abrupt guanfacine and clonidine discontinuation has been observed,126 these medications should be tapered off rather than suddenly discontinued.
Adjunctive Therapy
Adjunctive therapies may be considered if stimulant therapy is not fully effective or limited by side effects. Only extended-release guanfacine and extended-release clonidine have evidence supporting their use as adjunctive therapy with stimulant medications sufficient to have achieved FDA approval.127 Other medications have been used in combination on an off-label basis, with some limited evidence available to support the efficacy and safety of using atomoxetine in combination with stimulant medications to augment treatment of ADHD.128
Special Circumstances: Preschool-Aged Children (Age 4 Years to the Sixth Birthday)
If children do not experience adequate symptom improvement with PTBM, medication can be prescribed for those with moderate-to-severe ADHD. Many young children with ADHD may require medication to achieve maximum improvement; methylphenidate is the recommended first-line pharmacologic treatment of preschool children because of the lack of sufficient rigorous study in the preschool-aged population for nonstimulant ADHD medications and dextroamphetamine. Although amphetamine is the only medication with FDA approval for use in children younger than 6 years, this authorization was issued at a time when approval criteria were less stringent than current requirements. Hence, the available evidence regarding dextroamphetamine’s use in preschool-aged children with ADHD is not adequate to recommend it as an initial ADHD medication treatment at this time.80
No nonstimulant medication has received sufficient rigorous study in the preschool-aged population to be recommended for treatment of ADHD of children 4 through 5 years of age.
Although methylphenidate is the ADHD medication with the strongest evidence for safety and efficacy in preschool-aged children, it should be noted that the evidence has not yet met the level needed for FDA approval. Evidence for the use of methylphenidate consists of 1 multisite study of 165 children83 and 10 other smaller, single-site studies ranging from 11 to 59 children, for a total of 269 children.129 Seven of the 10 single-site studies revealed efficacy for methylphenidate in preschoolers. Therefore, although there is moderate evidence that methylphenidate is safe and effective in preschool-aged children, its use in this age group remains on an “off-label” basis.
With these caveats in mind, before initiating treatment with medication, the clinician should assess the severity of the child’s ADHD. Given current data, only preschool-aged children with ADHD and moderate-to-severe dysfunction should be considered for medication. Severity criteria are symptoms that have persisted for at least 9 months; dysfunction that is manifested in both home and other settings, such as preschool or child care; and dysfunction that has not responded adequately to PTBM.83
The decision to consider initiating medication at this age depends, in part, on the clinician’s assessment of the estimated developmental impairment, safety risks, and potential consequences if medications are not initiated. Other considerations affecting the treatment of preschool-aged children with stimulant medications include the lack of information and experience about their longer-term effects on growth and brain development, as well as the potential for other adverse effects in this population. It may be helpful to obtain consultation from a mental health specialist with specific experience with preschool-aged children, if possible.
Evidence suggests that the rate of metabolizing methylphenidate is slower in children 4 through 5 years of age, so they should be given a low dose to start; the dose can be increased in smaller increments. Maximum doses have not been adequately studied in preschool-aged children.83
Special Circumstances: Adolescents (Age 12 Years to the 18th Birthday)
As noted, before beginning medication treatment of adolescents with newly diagnosed ADHD, clinicians should assess the patient for symptoms of substance use. If active substance use is identified, the clinician should refer the patient to a subspecialist for consultative support and guidance.2,130–134
In addition, diversion of ADHD medication (ie, its use for something other than its intended medical purposes) is a special concern among adolescents.135 Clinicians should monitor the adolescent’s symptoms and prescription refill requests for signs of misuse or diversion of ADHD medication, including by parents, classmates, or other acquaintances of the adolescent. The majority of states now require prescriber participation in prescription drug monitoring programs, which can be helpful in identifying and preventing diversion activities. They may consider prescribing nonstimulant medications that minimize abuse potential, such as atomoxetine and extended-release guanfacine or extended-release clonidine.
Given the risks of driving for adolescents with ADHD, including crashes and motor vehicle violations, special concern should be taken to provide medication coverage for symptom control while driving.79,136,137 Longer-acting or late-afternoon, short-acting medications may be helpful in this regard.138
Special Circumstances: Inattention or Hyperactivity/Impulsivity (Problem Level)
Medication is not appropriate for children whose symptoms do not meet DSM-5 criteria for ADHD. Psychosocial treatments may be appropriate for these children and adolescents. As noted, psychosocial treatments do not require a specific diagnosis of ADHD, and many of the studies on the efficacy of PTBM included children who did not have a specific psychiatric or ADHD diagnosis.
Combination Treatments
Studies indicate that behavioral therapy has positive effects when it is combined with medication for preadolescent children.139 (The combined effects of training interventions and medication have not been studied.)
In the MTA study, researchers found that although the combination of behavioral therapy and stimulant medication was not significantly more effective than treatment with medication alone for ADHD’s core symptoms, after correcting for multiple tests in the primary analysis,139 a secondary analysis of a combined measure of parent and teacher ratings of ADHD symptoms did find a significant advantage for the combination, with a small effect of d = 0.28.140 The combined treatment also offered greater improvements on academic and conduct measures, compared to medication alone, when the ADHD was comorbid with anxiety and the child or adolescent lived in a lower socioeconomic environment.
In addition, parents and teachers of children who received combined therapy reported that they were significantly more satisfied with the treatment plan. Finally the combination of medication management and behavioral therapy allowed for the use of lower stimulant dosages, possibly reducing the risk of adverse effects.141
School Programming and Supports
Encouraging strong family-school partnerships helps the ADHD management process.142 Psychosocial treatments that include coordinating efforts at school and home may enhance the effects.
Children and adolescents with ADHD may be eligible for services as part of a 504 Rehabilitation Act Plan (504 plan) or special education IEP under the “other health impairment” designation in the Individuals with Disability Education Act (IDEA).143 (ADHD qualifies as a disability under a 504 plan. It does not qualify under an IEP unless its severity impairs the child’s ability to learn. See the PoCA for more details.) It is helpful for clinicians to be aware of the eligibility criteria in their states and school districts to advise families of their options. Eligibility decisions can vary considerably between school districts, and school professionals’ independent determinations might not agree with the recommendations of outside clinicians.
There are essentially 2 categories of school-based services for students with ADHD. The first category includes interventions that are intended to help the student independently meet age-appropriate academic and behavioral expectations. Examples of these interventions include daily report cards, training interventions, point systems, and academic remediation of skills. If successful, the student’s impairment will resolve, and the student will no longer need services.
The second category is intended to provide changes in the student’s program so his or her ADHD-related problems no longer result in failure and cause distress to parents, teachers, and the student.144 These services are referred to as “accommodations” and include extended time to complete tests and assignments, reduced homework demands, the ability to keep study materials in class, and provision of the teacher’s notes to the student. These services are intended to allow the student to accomplish his work successfully and communicate that the student’s impairment is acceptable. Accommodations make the student’s impairment acceptable and are separate from interventions aimed at improving the students’ skills or behaviors. In the absence of such interventions, long-term accommodations may lead to reduced expectations and can lead to the need for accommodations to be maintained throughout the student’s education.
Encouraging strong family-school partnerships helps the ADHD management process, and addressing social determinants of health is essential to these partnerships.145,146 Psychosocial treatments that include coordinating efforts at school and home may enhance the effects.
KAS 6
The PCC should titrate doses of medication for ADHD to achieve maximum benefit with tolerable side effects (Table 9). (Grade B: strong recommendation.)
TABLE 9.
KAS 6: The PCC should titrate doses of medication for ADHD to achieve maximum benefit with tolerable side effects. (Grade B: strong recommendation.)
| Aggregate evidence quality | Grade B |
|---|---|
| Benefits | The optimal dose of medication is required to reduce core symptoms to, or close to, the levels of children without ADHD. |
| Risks, harm, cost | Higher levels of medication increase the chances of side effects. |
| Benefit-harm assessment | The importance of adequately treating ADHD outweighs the risk of adverse effects. |
| Intentional vagueness | None. |
| Role of patient preferences | The families’ preferences and comfort need to be taken into consideration in developing a titration plan, as they are likely to predict engagement and persistence with a treatment. |
| Exclusions | None |
| Strength | Strong recommendation |
| Key references | Jensen et al140; Solanto147; Brinkman et al149 |
The MTA study is the landmark study comparing effects of methylphenidate and behavioral treatments in children with ADHD. Investigators compared treatment effects in 4 groups of children who received optimal medication management, optimal behavioral management, combined medication and behavioral management, or community treatment. Children in the optimal medication management and combined medication and behavioral management groups underwent a systematic trial with 4 different doses of methylphenidate, with results suggesting that when this full range of doses is administered, more than 70% of children and adolescents with ADHD are methylphenidate responders.140
Authors of other reports suggest that more than 90% of patients will have a beneficial response to 1 of the psychostimulants if a range of medications from both the methylphenidate and amphetamine and/or dextroamphetamine classes are tried.147 Of note, children in the MTA study who received care in the community as usual, either from a clinician they chose or to whom their family had access, showed less beneficial results compared with children who received optimal medication management. The explanation offered by the study investigators was that the community treatment group received lower medication doses and less frequent monitoring than the optimal medication management group.
A child’s response to stimulants is variable and unpredictable. For this reason, it is recommended to titrate from a low dose to one that achieves a maximum, optimal effect in controlling symptoms without adverse effects. Calculating the dose on the basis of milligrams per kilogram has not usually been helpful because variations in dose have not been found to be related to height or weight In addition, because stimulant medication effects are seen rapidly, titration can be accomplished in a relatively short time period. Stimulant medications can be effectively titrated on a 7-day basis, but in urgent situations, they may be effectively titrated in as few as 3 days.140
Parent and child and adolescent education is an important component in the chronic illness model to ensure cooperation in efforts to achieve appropriate titration, remembering that the parents themselves may be significantly challenged by ADHD.148,149 The PCC should alert parents and children that changing medication dose and occasionally changing a medication may be necessary for optimal medication management, may require a few months to achieve optimal success, and that medication efficacy should be monitored at regular intervals.
By the 3-year (ie, 36-month) follow-up to the MTA interventions, there were no differences among the 4 groups (ie, optimal medications management, optimal behavioral management, a combination of medication and behavioral management, and community treatment). This equivalence in poststudy outcomes may, however, have been attributable to convergence in ongoing treatments received for the 4 groups. After the initial 14-month intervention, the children no longer received the careful monthly monitoring provided by the study and went back to receiving care from their community providers; therefore, they all effectively received a level of ongoing care consistent with the “community treatment” study arm of the study. After leaving the MTA trial, medications and doses varied for the children who had been in the optimal medication management or combined medication and behavioral management groups, and a number stopped taking ADHD medication. On the other hand, some children who had been in the optimal behavioral management group started taking medication after leaving the trial. The results further emphasize the need to treat ADHD as a chronic illness and provide continuity of care and, where possible, provide a medical home.140
See the PoCA for more on implementation of this KAS.
KAS 7
The PCC, if trained or experienced in diagnosing comorbid conditions, may initiate treatment of such conditions or make a referral to an appropriate subspecialist for treatment. After detecting possible comorbid conditions, if the PCC is not trained or experienced in making the diagnosis or initiating treatment, the patient should be referred to an appropriate subspecialist to make the diagnosis and initiate treatment (Table 10). (Grade C: recommendation.)
TABLE 10.
KAS 7: The PCC, if trained or experienced in diagnosing comorbid conditions, may initiate treatment of such conditions or make a referral to an appropriate subspecialist for treatment After detecting possible comorbid conditions, if the PCC is not trained or experienced in making the diagnosis or initiating treatment, the patient should be referred to an appropriate subspecialist to make the diagnosis and initiate treatment. (Grade C: recommendation.)
| Aggregate evidence | Grade C |
|---|---|
| quality | |
| Benefits | Clinicians are most effective when they know the limits of their practice to diagnose comorbid conditions and are aware of resources in their community. |
| Risks, harm, cost | Under-identification or inappropriate identification of comorbidities can lead to inadequate or inappropriate treatments. |
| Benefit-harm assessment | The importance of adequately identifying and addressing comorbidities outweighs the risk of inappropriate referrals or treatments. |
| Intentional vagueness | None. |
| Role of patient preferences | The families’ preferences and comfort need to be taken into consideration in identifying and treating or referring their patients with comorbidities, as they are likely to predict engagement and persistence with a treatment. |
| Exclusions | None. |
| Strength | Recommendation. |
| Key references | Pliszka et al150; Pringsheim et al151 |
The effect of comorbid conditions on ADHD treatment is variable. In some cases, treatment of the ADHD may resolve the comorbid condition. For example, treatment of ADHD may lead to improvement in coexisting aggression and/or oppositional defiant, depressive, or anxiety symptoms.150,151
Sometimes, however, the comorbid condition may require treatment in addition to the ADHD treatment. If the PCC is confident of his or her ability to diagnose and treat certain comorbid conditions, the PCC may do so. The PCC may benefit from additional consultative support and guidance from a mental health subspecialist or may need to refer a child with ADHD and comorbid conditions, such as severe mood or anxiety disorders, to subspecialists for assessment and management. The subspecialists could include child and adolescent psychiatrists, clinical child psychologists, developmental-behavioral pediatricians, neurodevelopmental disability physicians, child neurologists, or child- or school-based evaluation teams.
IMPLEMENTATION: PREPARING THE PRACTICE
It is generally the role of the primary care pediatrician to manage mild-to-moderate ADHD, anxiety, depression, and substance use. The AAP statement “The Future of Pediatrics: Mental Health Competencies for Pediatric Primary Care” describes the competencies needed in both pediatric primary and specialty care to address the social-emotional and mental health needs of children and families.152 Broadly, these include incorporating mental health content and tools into health promotion, prevention, and primary care intervention, becoming knowledgeable about use of evidence-based treatments, and participating as a team member and comanaging with pediatric and mental health specialists.
The recommendations made in this guideline are intended to be integrated with the broader mental health algorithm developed as part of the AAP Mental Health Initiatives.2,133,153 Pediatricians have unique opportunities to identify conditions, including ADHD, intervene early, and partner with both families and specialists for the benefit of children’s health. A wealth of useful information is available at the AAP Mental Health Initiatives Web site (https://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/Mental-Health/Pages/Tips-For-Pediatricians.aspx).
It is also important for PCCs to be aware of health disparities and social determinants that may impact patient outcomes and strive to provide culturally appropriate care to all children and adolescents in their practice.145,146,154,155
The accompanying PoCA provides supplemental information to support PCCs as they implement this guideline’s recommendations. In particular, the PoCA describes steps for preparing the practice that provide useful recommendations to clinicians. For example, the PoCA includes information about using standardized rating scales to diagnose ADHD, assessing for comorbid conditions, documenting all aspects of the diagnostic and treatment procedures in the patient’s records, monitoring the patient’s treatment and outcomes, and providing families with written management plans.
The AAP acknowledges that some PCCs may not have the training, experience, or resources to diagnose and treat children and adolescents with ADHD, especially if severity or comorbid conditions make these patients complex to manage. In these situations, comanagement with specialty clinicians is recommended. The SDBP is developing a guideline to address such complex cases and aid pediatricians and other PCCs to manage these cases; the SDBP currently expects to publish this document in 2019.67
AREAS FOR FUTURE RESEARCH
There is a need to conduct research on topics pertinent to the diagnosis and treatment of ADHD, developmental variations, and problems in children and adolescents in primary care. These research opportunities include the following:
assessment of ADHD and its common comorbidities: anxiety, depression, learning disabilities, and autism spectrum disorder;
identification and/or development of reliable instruments suitable for use in primary care to assess the nature or degree of functional impairment in children and adolescents with ADHD and to monitor improvement over time;
refinement of developmentally informed assessment procedures for evaluating ADHD in preschoolers;
study of medications and other therapies used clinically but not FDA approved for ADHD;
determination of the optimal schedule for monitoring children and adolescents with ADHD, including factors for adjusting that schedule according to age, symptom severity, and progress reports;
evaluation of the effectiveness and adverse effects of medications used in combination, such as a stimulant with an α-adrenergic agent, selective serotonin reuptake inhibitor, or atomoxetine;
evaluation of processes of care to assist PCCs to identify and treat comorbid conditions;
evaluation of the effectiveness of various school-based interventions;
comparisons of medication use and effectiveness in different ages, including both harms and benefits;
development of methods to involve parents, children, and adolescents in their own care and improve adherence to both psychosocial and medication treatments;
conducting research into psychosocial treatments, such as cognitive behavioral therapy and cognitive training, among others;
development of standardized and documented tools to help primary care providers identify comorbid conditions;
development of effective electronic and Web-based systems to help gather information to diagnose and monitor children and adolescents with ADHD;
improvements to systems for communicating with schools, mental health professionals, and other community agencies to provide effective collaborative care;
development of more objective measures of performance to more objectively monitor aspects of severity, disability, or impairment;
assessment of long-term outcomes for children in whom ADHD was first diagnosed at preschool ages; and
identification and implementation of ideas to address the barriers that hamper the implementation of these guidelines and the PoCA.
CONCLUSIONS
Evidence is clear with regard to the legitimacy of the diagnosis of ADHD and the appropriate diagnostic criteria and procedures required to establish a diagnosis, identify comorbid conditions, and effectively treat with both psychosocial and pharmacologic interventions. The steps required to sustain appropriate treatments and achieve successful long-term outcomes remain challenging, however.
As noted, this clinical practice guideline is supported by 2 accompanying documents available in the Supplemental Information: the PoCA and the article on systemic barriers to the car of children and adolescents with ADHD. Full implementation of the guideline’s KASs, the PoCA, and the recommendations to address barriers to care may require changes in office procedures and the identification of community resources. Fully addressing systemic barriers requires identifying local, state, and national entities with which to partner to advance solutions and manifest change.156
Supplementary Material
ABBREVIATIONS
- AAP
American Academy of Pediatrics
- ADHD
attention-deficit/hyperactivity disorder
- ADHD/C
attention-deficit/hyperactivity disorder combined presentation
- ADHD/HI
attention-deficit/hyperactivity disorder primarily of the hyperactive-impulsive presentation
- ADHD/I
attention-deficit/hyperactivity disorder primarily of the inattentive presentation
- AHRQ
Agency for Healthcare Research and Quality
- BP
blood pressure
- CHADD
Children and Adults with Attention-Deficit/Hyperactivity Disorder
- DSM-5
Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition
- DSM-IV
Diagnostic and Statistical Manual of Mental Disorders Fourth Edition
- DSM-PC
Diagnostic and Statistical Manual for Primary Care
- ECG
electrocardiogram
- eTNS
external trigeminal nerve stimulation
- FDA
US Food and Drug Administration
- HR
heart rate
- IDEA
Individuals with Disability Education Act
- IEP
Individualized Education Program
- KAS
key action statement
- MTA
The Multimodal Treatment of Attention Deficit Hyperactivity Disorder
- PCC
primary care clinician
- PoCA
process of care algorithm
- PTBM
parent training in behavior management
- SDBP
Society for Developmental and Behavioral Pediatrics
Footnotes
SUBCOMMITTEE ON CHILDREN AND ADOLESCENTS WITH ADHD (OVERSIGHT BY THE COUNCIL ON QUALITY IMPROVEMENT AND PATIENT SAFETY)
Mark L. Wolraich, MD, FAAP, Chairperson, Section on Developmental Behavioral Pediatrics
Joseph F. Hagan Jr, MD, FAAP, Vice Chairperson, Section on Developmental Behavioral Pediatrics
Carla Allan, PhD, Society of Pediatric Psychology
Eugenia Chan, MD, MPH, FAAP, Implementation Scientist
Dale Davison, MSpEd, PCC, Parent Advocate, Children and Adolescents with Attention-Deficit/Hyperactivity Disorder
Marian Earls, MD, MTS, FAAP, Mental Health Leadership Work Group
Steven W. Evans, PhD, Clinical Psychologist
Tanya Froehlich, MD, FAAP, Section on Developmental Behavioral Pediatrics/Society for Developmental and Behavioral Pediatrics
Jennifer Frost, MD, FAAFP, American Academy of Family Physicians
Joseph R. Holbrook, PhD, MPH, Epidemiologist, Centers for Disease Control and Prevention
Herschel Robert Lessin, MD, FAAP, Section on Administration and Practice Management
Karen L. Pierce, MD, DFAACAP, American Academy of Child and Adolescent Psychiatry
Christoph Ulrich Lehmann, MD, FAAP, Partnership for Policy Implementation
Jonathan D. Winner, MD, FAAP, Committee on Practice and Ambulatory Medicine
William Zurhellen, MD, FAAP, Section on Administration and Practice Management
STAFF
Kymika Okechukwu, MPA, Senior Manager, Evidence-Based Medicine Initiatives
Jeremiah Salmon, MPH, Program Manager, Policy Dissemination and Implementation
CONSULTANT
Susan K. Flinn, MA, Medical Editor
The guidance in this report does not indicate an exclusive course of treatment or serve as a standard of medical care. Variations, taking into account individual circumstances, may be appropriate.
All clinical practice guidelines from the American Academy of Pediatrics automatically expire 5 years after publication unless reaffirmed, revised, or retired at or before that time.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. Dr Holbrook was not an author of the accompanying supplemental section on barriers to care.
This document is copyrighted and is property of the American Academy of Pediatrics and its Board of Directors. All authors have filed conflict of interest statements with the American Academy of Pediatrics. Any conflicts have been resolved through a process approved by the Board of Directors. The American Academy of Pediatrics has neither solicited nor accepted any commercial involvement in the development of the content of this publication.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
POTENTIAL CONFLICT OF INTEREST: All authors have filed conflict of interest statements with the American Academy of Pediatrics. Any conflicts have been resolved through a process approved by the American Academy of Pediatrics board of directors. Dr Allan reports a relationship with ADDitude Magazine; Dr Chan reports relationships with TriVox Health and Wolters Kluwer; Dr Lehmann reports relationships with International Medical Informatics Association, Springer Publishing, and Thieme Publishing Group; Dr Wolraich reports a Continuing Medical Education trainings relationship with the Resource for Advancing Children’s Health Institute; the other authors have indicated they have no potential conflicts of interest to disclose.
REFERENCES
- 1.American Academy of Pediatrics. Subcommittee on Attention-Deficit/Hyperactivity Disorder, Steering Committee on Quality Improvement and Management. ADHD: Clinical guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. 2011;128(5):1007–1022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Academy of Pediatrics Task Force on Mental Health. Addressing Mental Health Concerns in Primary Care: A Clinician’s Toolkit [CD-ROM]. Elk Grove Village, IL: American Academy of Pediatrics; 2010 [Google Scholar]
- 3.Pastor PN, Reuben CA. Racial and ethnic differences in ADHD and LD in young school-age children: parental reports in the National Health Interview Survey. Public Health Rep. 2005;120(4):383–392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.US Department of Health and Human Services; Health Resources and Services Administration. Designated health professional shortage areas statistics: designated HPSA quarterly summary. Rockville, MD: Health Resources and Services Administration; 2018 [Google Scholar]
- 5.Pelech D, Hayford T. Medicare advantage and commercial prices for mental health services. Health Aff (Millwood). 2019;38(2):262–267 [DOI] [PubMed] [Google Scholar]
- 6.Melek SP, Perlman D, Davenport S. Differential Reimbursement of Psychiatric Services by Psychiatrists and Other Medical Providers. Seattle, WA: Milliman;2017 [DOI] [PubMed] [Google Scholar]
- 7.Holbrook JR, Bitsko RH, Danielson ML, Visser SN. Interpreting the prevalence of mental disorders in children: tribulation and triangulation. Health Promot Pract. 2017;18(1):5–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thomas R, Sanders S, Doust J, Beller E, Glasziou P. Prevalence of attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. Pediatrics. 2015;135(4). Available at: www.pediatrics.org/cgi/content/full/135/4/e994 [DOI] [PubMed] [Google Scholar]
- 9.Wolraich ML, McKeown RE, Visser SN, et al. The prevalence of ADHD: its diagnosis and treatment in four school districts across two states. J Atten Disord. 2014;18(7):563–575 [DOI] [PubMed] [Google Scholar]
- 10.Rowland AS, Skipper BJ, Umbach DM, et al. The prevalence of ADHD in a population-based sample. J Atten Disord. 2015;19(9):741–754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Danielson ML, Bitsko RH, Ghandour RM, Holbrook JR, Kogan MD, Blumberg SJ. Prevalence of parent-reported ADHD diagnosis and associated treatment among U.S. children and adolescents, 2016. J Clin Child Adolesc Psychol. 2018; 47(2):199–212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Visser SN, Zablotsky B, Holbrook JR, et al. National Health Statistics Reports, No 81: Diagnostic Experiences of Children with Attention-Deficit/Hyperactivity Disorder. Hyattsville, MD: National Center for Health Statistics; 2015 [PubMed] [Google Scholar]
- 13.Molina BS, Hinshaw SP, Swanson JM, et al. ; MTA Cooperative Group. The MTA at 8 years: prospective follow-up of children treated for combined-type ADHD in a multisite study. J Am Acad Child Adolesc Psychiatry. 2009;48(5):484–500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Holbrook JR, Cuffe SP, Cai B, et al. Persistence of parent-reported ADHD symptoms from childhood through adolescence in a community sample. J Atten Disord. 2016;20(1):11–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mueller KL, Tomblin JB. Examining the comorbidity of language disorders and ADHD. Top Lang Disord. 2012;32(3): 228–246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pastor PN, Reuben CA, Duran CR, Hawkins LD. Association Between Diagnosed ADHD and Selected Characteristics Among Children Aged 4–17 Years: United States, 2011–2013 NCHS Data Brief, No. 201. Hyattsville, MD: National Center for Health Statistics; 2015 [PubMed] [Google Scholar]
- 17.Elia J, Ambrosini P, Berrettini W. ADHD characteristics: I. Concurrent co-morbidity patterns in children & adolescents. Child Adolesc Psychiatry Ment Health. 2008;2(1):15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention (CDC). Mental health in the United States. Prevalence of diagnosis and medication treatment for attention-deficit/hyperactivity disorder--United States, 2003. MMWR Morb Mortal Wkly Rep. 2005;54(34):842–847 [PubMed] [Google Scholar]
- 19.Cuffe SP, Visser SN, Holbrook JR, et al. ADHD and psychiatric comorbidity: functional outcomes in a school-based sample of children [published online ahead of print November 25, 2015]. J Atten Disord. doi: 10.1177/1087054715613437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gaub M, Carlson CL. Gender differences in ADHD: a meta-analysis and critical review. J Am Acad Child Adolesc Psychiatry. 1997;36(8):1036–1045 [DOI] [PubMed] [Google Scholar]
- 21.Tung I, Li JJ, Meza JI, et al. Patterns of comorbidity among girls with ADHD: a meta-analysis. Pediatrics. 2016;138(4): e20160430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Layton TJ, Barnett ML, Hicks TR, Jena AB. Attention deficit-hyperactivity disorder and month of school enrollment. N Engl J Med. 2018;379(22): 2122–2130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kemper AR, Maslow GR, Hill S, et al. Attention Deficit Hyperactivity Disorder: Diagnosis and Treatment in Children and Adolescents Comparative Effectiveness Reviews, No. 203. Rockville, MD: Agency for Healthcare Research and Quality; 2018 [PubMed] [Google Scholar]
- 24.Pelham WE Jr, Wheeler T, Chronis A. Empirically supported psychosocial treatments for attention deficit hyperactivity disorder. J Clin Child Psychol. 1998;27(2):190–205 [DOI] [PubMed] [Google Scholar]
- 25.Evans SW, Owens JS, Wymbs BT, Ray AR. Evidence-based psychosocial treatments for children and adolescents with attention deficit/hyperactivity disorder. J Clin Child Adolesc Psychol. 2018;47(2):157–198 [DOI] [PubMed] [Google Scholar]
- 26.Pelham WE Jr, Fabiano GA. Evidence-based psychosocial treatments for attention-deficit/hyperactivity disorder. J Clin Child Adolesc Psychol. 2008;37(1):184–214 [DOI] [PubMed] [Google Scholar]
- 27.American Academy of Pediatrics Steering Committee on Quality Improvement and Management. Classifying recommendations for clinical practice guidelines. Pediatrics. 2004;114(3):874–877 [DOI] [PubMed] [Google Scholar]
- 28.Visser SN, Lesesne CA, Perou R. National estimates and factors associated with medication treatment for childhood attention-deficit/hyperactivity disorder. Pediatrics. 2007;119(suppl 1):S99–S106 [DOI] [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention (CDC). Increasing prevalence of parent-reported attention-deficit/hyperactivity disorder among children–United States, 2003 and 2007. MMWR Morb Mortal Wkly Rep. 2010;59(44):1439–1443 [PubMed] [Google Scholar]
- 30.Egger HL, Kondo D, Angold A. The epidemiology and diagnostic issues in preschool attention-deficit/hyperactivity disorder: a review. Infants Young Child. 2006;19(2):109–122 [Google Scholar]
- 31.Wolraich ML, Wibbelsman CJ, Brown TE, et al. Attention-deficit/hyperactivity disorder among adolescents: a review of the diagnosis, treatment, and clinical implications. Pediatrics. 2005;115(6): 1734–1746 [DOI] [PubMed] [Google Scholar]
- 32.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5). 5th ed. Arlington, VA: American Psychiatric Association; 2013 [Google Scholar]
- 33.Lahey BB, Pelham WE, Stein MA, et al. Validity of DSM-IV attention-deficit/hyperactivity disorder for younger children. J Am Acad Child Adolesc Psychiatry. 1998;37(7):695–702 [DOI] [PubMed] [Google Scholar]
- 34.Pavuluri MN, Luk SL, McGee R. Parent reported preschool attention deficit hyperactivity: measurement and validity. Eur Child Adolesc Psychiatry. 1999;8(2):126–133 [DOI] [PubMed] [Google Scholar]
- 35.Harvey EA, Youngwirth SD, Thakar DA, Errazuriz PA. Predicting attention-deficit/hyperactivity disorder and oppositional defiant disorder from preschool diagnostic assessments. J Consult Clin Psychol. 2009;77(2): 349–354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Keenan K, Wakschlag LS. More than the terrible twos: the nature and severity of behavior problems in clinic-referred preschool children. J Abnorm Child Psychol. 2000;28(1):33–46 [DOI] [PubMed] [Google Scholar]
- 37.Gadow KD, Nolan EE, Litcher L, et al. Comparison of attention-deficit/hyperactivity disorder symptom subtypes in Ukrainian schoolchildren. J Am Acad Child Adolesc Psychiatry. 2000;39(12):1520–1527 [DOI] [PubMed] [Google Scholar]
- 38.Sprafkin J, Volpe RJ, Gadow KD, Nolan EE, Kelly K. A DSM-IV-referenced screening instrument for preschool children: the Early Childhood Inventory-4. J Am Acad Child Adolesc Psychiatry. 2002;41(5):604–612 [DOI] [PubMed] [Google Scholar]
- 39.Poblano A, Romero E. ECI-4 screening of attention deficit-hyperactivity disorder and co-morbidity in Mexican preschool children: preliminary results. Arq Neuropsiquiatr. 2006;64(4):932–936 [DOI] [PubMed] [Google Scholar]
- 40.American Academy of Pediatrics. Mental Health Screening and Assessment Tools for Primary Care. Elk Grove Village, IL: American Academy of Pediatrics; 2012. Available at: http//www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/Mental-Health/Documents/MH_ScreeningChart.pdf Accessed September 8, 2019 [Google Scholar]
- 41.DuPaul GJ, Power TJ, Anastopoulos AD, Reid R. ADHD Rating Scale – 5 for Children and Adolescents: Checklists, Norms, and Clinical Interpretation. 2nd ed. New York, NY: Guilford Press; 2016 [Google Scholar]
- 42.McGoey KE, DuPaul GJ, Haley E, Shelton TL. Parent and teacher ratings of attention-deficit/hyperactivity disorder in preschool: the ADHD rating scale-IV preschool version. J Psychopathol Behav Assess. 2007;29(4):269–276 [Google Scholar]
- 43.Young J Common comorbidities seen in adolescents with attention-deficit/hyperactivity disorder. Adolesc Med State Art Rev. 2008;19(2):216–228, vii [PubMed] [Google Scholar]
- 44.Freeman RD; Tourette Syndrome International Database Consortium. Tic disorders and ADHD: answers from a world-wide clinical dataset on Tourette syndrome. Eur Child Adolesc Psychiatry. 2007;16(suppl 1):15–23 [DOI] [PubMed] [Google Scholar]
- 45.Riggs PD. Clinical approach to treatment of ADHD in adolescents with substance use disorders and conduct disorder. J Am Acad Child Adolesc Psychiatry. 1998;37(3):331–332 [DOI] [PubMed] [Google Scholar]
- 46.Sibley MH, Pelham WE, Molina BSG, et al. Diagnosing ADHD in adolescence. J Consult Clin Psychol. 2012;80(1): 139–150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kratochvil CJ, Vaughan BS, Stoner JA, et al. A double-blind, placebo-controlled study of atomoxetine in young children with ADHD. Pediatrics. 2011;127(4). Available at: www.pediatrics.org/cgi/content/full/127/4/e862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Harrison AG, Edwards MJ, Parker KC. Identifying students faking ADHD: preliminary findings and strategies for detection. Arch Clin Neuropsychol. 2007; 22(5):577–588 [DOI] [PubMed] [Google Scholar]
- 49.Wolraich ML, Felice ME, Drotar DD. The Classification of Child and Adolescent Mental Conditions in Primary Care: Diagnostic and Statistical Manual for Primary Care (DSM-PC), Child and Adolescent Version. Elk Grove Village, IL: American Academy of Pediatrics; 1996 [Google Scholar]
- 50.Rowland AS, Lesesne CA, Abramowitz AJ. The epidemiology of attention-deficit/hyperactivity disorder (ADHD): a public health view. Ment Retard Dev Disabil Res Rev. 2002;8(3):162–170 [DOI] [PubMed] [Google Scholar]
- 51.Cuffe SP, Moore CG, McKeown RE. Prevalence and correlates of ADHD symptoms in the national health interview survey. J Atten Disord. 2005; 9(2):392–401 [DOI] [PubMed] [Google Scholar]
- 52.Pastor PN, Reuben CA. Diagnosed attention deficit hyperactivity disorder and learning disability: United States, 2004-2006. Vital Health Stat 10. 2008; 10(237):1–14 [PubMed] [Google Scholar]
- 53.Biederman J, Faraone SV, Wozniak J, Mick E, Kwon A, Aleardi M. Further evidence of unique developmental phenotypic correlates of pediatric bipolar disorder: findings from a large sample of clinically referred preadolescent children assessed over the last 7 years. J Affect Disord. 2004; 82(suppl 1):S45–S58 [DOI] [PubMed] [Google Scholar]
- 54.Biederman J, Kwon A, Aleardi M, et al. Absence of gender effects on attention deficit hyperactivity disorder: findings in nonreferred subjects. Am J Psychiatry. 2005;162(6):1083–1089 [DOI] [PubMed] [Google Scholar]
- 55.Biederman J, Ball SW, Monuteaux MC, et al. New insights into the comorbidity between ADHD and major depression in adolescent and young adult females. J Am Acad Child Adolesc Psychiatry. 2008;47(4):426–434 [DOI] [PubMed] [Google Scholar]
- 56.Biederman J, Melmed RD, Patel A, McBurnett K, Donahue J, Lyne A. Long-term, open-label extension study of guanfacine extended release in children and adolescents with ADHD. CNS Spectr. 2008;13(12):1047–1055 [DOI] [PubMed] [Google Scholar]
- 57.Crabtree VM, Ivanenko A, Gozal D. Clinical and parental assessment of sleep in children with attention-deficit/hyperactivity disorder referred to a pediatric sleep medicine center. Clin Pediatr (Phila). 2003;42(9):807–813 [DOI] [PubMed] [Google Scholar]
- 58.LeBourgeois MK, Avis K, Mixon M, Olmi J, Harsh J. Snoring, sleep quality, and sleepiness across attention-deficit/hyperactivity disorder subtypes. Sleep. 2004;27(3):520–525 [PubMed] [Google Scholar]
- 59.Chan E, Zhan C, Homer CJ. Health care use and costs for children with attention-deficit/hyperactivity disorder: national estimates from the Medical Expenditure Panel Survey. Arch Pediatr Adolesc Med. 2002;156(5):504–511 [DOI] [PubMed] [Google Scholar]
- 60.Newcorn JH, Miller SR, Ivanova I, et al. Adolescent outcome of ADHD: impact of childhood conduct and anxiety disorders. CNS Spectr. 2004;9(9): 668–678 [DOI] [PubMed] [Google Scholar]
- 61.Sung V, Hiscock H, Sciberras E, Efron D. Sleep problems in children with attention-deficit/hyperactivity disorder: prevalence and the effect on the child and family. Arch Pediatr Adolesc Med. 2008;162(4):336–342 [DOI] [PubMed] [Google Scholar]
- 62.Froehlich TE, Fogler J, Barbaresi WJ, Elsayed NA, Evans SW, Chan E. Using ADHD medications to treat coexisting ADHD and reading disorders: a systematic review. Clin Pharmacol Ther. 2018;104(4):619–637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rothenberger A, Roessner V. The phenomenology of attention-deficit/hyperactivity disorder in tourette syndrome In: Martino D, Leckman JF, eds. Tourette Syndrome. New York, NY: Oxford University Press; 2013:26–49 [Google Scholar]
- 64.Antshel KM, Zhang-James Y, Faraone SV. The comorbidity of ADHD and autism spectrum disorder. Expert Rev Neurother. 2013;13(10):1117–1128 [DOI] [PubMed] [Google Scholar]
- 65.Mahajan R, Bernal MP, Panzer R, et al. ; Autism Speaks Autism Treatment Network Psychopharmacology Committee. Clinical practice pathways for evaluation and medication choice for attention-deficit/hyperactivity disorder symptoms in autism spectrum disorders. Pediatrics. 2012;130(suppl 2):S125–S138 [DOI] [PubMed] [Google Scholar]
- 66.Larson K, Russ SA, Kahn RS, Halfon N. Patterns of comorbidity, functioning, and service use for US children with ADHD, 2007. Pediatrics. 2011;127(3): 462–470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Society for Developmental and Behavioral Pediatrics. ADHD special interest group. Available at: www.sdbp.org/committees/sig-adhd.cfm Accessed September 8, 2019 [Google Scholar]
- 68.Medical Home Initiatives for Children With Special Needs Project Advisory Committee. American Academy of Pediatrics. The medical home. Pediatrics. 2002;110(1 pt 1):184–186 [PubMed] [Google Scholar]
- 69.Brito A, Grant R, Overholt S, et al. The enhanced medical home: the pediatric standard of care for medically underserved children. Adv Pediatr. 2008;55:9–28 [DOI] [PubMed] [Google Scholar]
- 70.Sibley MH, Swanson JM, Arnold LE, et al. ; MTA Cooperative Group. Defining ADHD symptom persistence in adulthood: optimizing sensitivity and specificity. J Child Psychol Psychiatry. 2017;58(6): 655–662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Chang Z, D’Onofrio BM, Quinn PD, Lichtenstein P, Larsson H. Medication for attention-deficit/hyperactivity disorder and risk for depression: a nationwide longitudinal cohort study. Biol Psychiatry. 2016;80(12):916–922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Biederman J, Monuteaux MC, Spencer T, Wilens TE, Faraone SV. Do stimulants protect against psychiatric disorders in youth with ADHD? A 10-year follow-up study. Pediatrics. 2009;124(1):71–78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Barbaresi WJ, Katusic SK, Colligan RC, Weaver AL, Jacobsen SJ. Modifiers of long-term school outcomes for children with attention-deficit/hyperactivity disorder: does treatment with stimulant medication make a difference? Results from a population-based study. J Dev Behav Pediatr. 2007; 28(4):274–287 [DOI] [PubMed] [Google Scholar]
- 74.Scheffler RM, Brown TT, Fulton BD, Hinshaw SP, Levine P, Stone S. Positive association between attention-deficit/hyperactivity disorder medication use and academic achievement during elementary school. Pediatrics. 2009; 123(5):1273–1279 [DOI] [PubMed] [Google Scholar]
- 75.Barbaresi WJ, Colligan RC, Weaver AL, Voigt RG, Killian JM, Katusic SK. Mortality, ADHD, and psychosocial adversity in adults with childhood ADHD: a prospective study. Pediatrics. 2013;131(4):637–644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Chang Z, Lichtenstein P, Långström N, Larsson H, Fazel S. Association between prescription of major psychotropic medications and violent reoffending after prison release. JAMA. 2016; 316(17):1798–1807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lichtenstein P, Halldner L, Zetterqvist J, et al. Medication for attention deficit-hyperactivity disorder and criminality. N Engl J Med. 2012;367(21):2006–2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Chang Z, Quinn PD, Hur K, et al. Association between medication use for attention-deficit/hyperactivity disorder and risk of motor vehicle crashes. JAMA Psychiatry. 2017;74(6):597–603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Chang Z, Lichtenstein P, D’Onofrio BM, Sjölander A, Larsson H. Serious transport accidents in adults with attention-deficit/hyperactivity disorder and the effect of medication: a population-based study. JAMA Psychiatry. 2014;71(3):319–325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Harstad E, Levy S; Committee on Substance Abuse. Attention-deficit/hyperactivity disorder and substance abuse. Pediatrics. 2014;134(1). Available at: www.pediatrics.org/cgi/content/full/134/1/e293 [DOI] [PubMed] [Google Scholar]
- 81.Dalsgaard S, Leckman JF, Mortensen PB, Nielsen HS, Simonsen M. Effect of drugs on the risk of injuries in children with attention deficit hyperactivity disorder: a prospective cohort study. Lancet Psychiatry. 2015;2(8):702–709 [DOI] [PubMed] [Google Scholar]
- 82.Raman SR, Marshall SW, Haynes K, Gaynes BN, Naftel AJ, Stürmer T. Stimulant treatment and injury among children with attention deficit hyperactivity disorder: an application of the self-controlled case series study design. Inj Prev. 2013;19(3):164–170 [DOI] [PubMed] [Google Scholar]
- 83.Greenhill L, Kollins S, Abikoff H, et al. Efficacy and safety of immediaterelease methylphenidate treatment for preschoolers with ADHD. J Am Acad Child Adolesc Psychiatry. 2006;45(11): 1284–1293 [DOI] [PubMed] [Google Scholar]
- 84.Children and Adults with Attention-Deficit/Hyperactivity Disorder. CHADD; Available at: www.chadd.org Accessed September 8, 2019 [Google Scholar]
- 85.Sonuga-Barke EJ, Daley D, Thompson M, Laver-Bradbury C, Weeks A. Parent-based therapies for preschool attention-deficit/hyperactivity disorder: a randomized, controlled trial with a community sample. J Am Acad Child Adolesc Psychiatry. 2001;40(4):402–408 [DOI] [PubMed] [Google Scholar]
- 86.Van Cleave J, Leslie LK. Approaching ADHD as a chronic condition: implications for long-term adherence. J Psychosoc Nurs Ment Health Serv. 2008;46(8):28–37 [DOI] [PubMed] [Google Scholar]
- 87.Webster-Stratton CH, Reid MJ, Beauchaine T. Combining parent and child training for young children with ADHD. J Clin Child Adolesc Psychol. 2011;40(2):191–203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Shepard SA, Dickstein S. Preventive intervention for early childhood behavioral problems: an ecological perspective. Child Adolesc Psychiatr Clin N Am. 2009;18(3):687–706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Evans SW, Langberg JM, Egan T, Molitor SJ. Middle school-based and high school-based interventions for adolescents with ADHD. Child Adolesc Psychiatr Clin N Am. 2014;23(4):699–715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.McGough JJ, Sturm A, Cowen J, et al. Double-blind, sham-controlled, pilot study of trigeminal nerve stimulation for attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2019;58(4):403–411.e3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Robin AL, Foster SL. The Guilford Family Therapy Series Negotiating Parent–Adolescent Conflict: A Behavioral–Family Systems Approach. New York, NY: Guilford Press; 1989 [Google Scholar]
- 92.Barkley RA, Guevremont DC, Anastopoulos AD, Fletcher KE. A comparison of three family therapy programs for treating family conflicts in adolescents with attention-deficit hyperactivity disorder. J Consult Clin Psychol. 1992;60(3):450–462 [DOI] [PubMed] [Google Scholar]
- 93.Fabiano GA, Schatz NK, Morris KL, et al. Efficacy of a family-focused intervention for young drivers with attention-deficit hyperactivity disorder. J Consult Clin Psychol. 2016;84(12):1078–1093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Sibley MH, Graziano PA, Kuriyan AB, et al. Parent-teen behavior therapy 1 motivational interviewing for adolescents with ADHD. J Consult Clin Psychol. 2016;84(8):699–712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Evans SW, Langberg JM, Schultz BK, et al. Evaluation of a school-based treatment program for young adolescents with ADHD. J Consult Clin Psychol. 2016;84(1):15–30 [DOI] [PubMed] [Google Scholar]
- 96.Langberg JM, Dvorsky MR, Molitor SJ, et al. Overcoming the research-topractice gap: a randomized trial with two brief homework and organization interventions for students with ADHD as implemented by school mental health providers. J Consult Clin Psychol. 2018; 86(1):39–55 [DOI] [PubMed] [Google Scholar]
- 97.Schultz BK, Evans SW, Langberg JM, Schoemann AM. Outcomes for adolescents who comply with long-term psychosocial treatment for ADHD. J Consult Clin Psychol. 2017;85(3): 250–261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Newcorn JH, Kratochvil CJ, Allen AJ, et al. ; Atomoxetine/Methylphenidate Comparative Study Group. Atomoxetine and osmotically released methylphenidate for the treatment of attention deficit hyperactivity disorder: acute comparison and differential response. Am J Psychiatry. 2008;165(6): 721–730 [DOI] [PubMed] [Google Scholar]
- 99.Cheng JY, Chen RY, Ko JS, Ng EM. Efficacy and safety of atomoxetine for attention-deficit/hyperactivity disorder in children and adolescents-meta-analysis and meta-regression analysis. Psychopharmacology (Berl). 2007; 194(2):197–209 [DOI] [PubMed] [Google Scholar]
- 100.Michelson D, Allen AJ, Busner J, et al. Once-daily atomoxetine treatment for children and adolescents with attention deficit hyperactivity disorder: a randomized, placebo-controlled study. Am J Psychiatry. 2002;159(11): 1896–1901 [DOI] [PubMed] [Google Scholar]
- 101.Biederman J, Melmed RD, Patel A, et al. ; SPD503 Study Group. A randomized, double-blind, placebo-controlled study of guanfacine extended release in children and adolescents with attention-deficit/hyperactivity disorder. Pediatrics. 2008;121(1). Available at: www.pediatrics.org/cgi/content/full/121/1/e73 [DOI] [PubMed] [Google Scholar]
- 102.Sallee FR, Lyne A, Wigal T, McGough JJ. Long-term safety and efficacy of guanfacine extended release in children and adolescents with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol. 2009; 19(3):215–226 [DOI] [PubMed] [Google Scholar]
- 103.Jain R, Segal S, Kollins SH, Khayrallah M. Clonidine extended-release tablets for pediatric patients with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2011; 50(2):171–179 [DOI] [PubMed] [Google Scholar]
- 104.Brown JT, Bishop JR. Atomoxetine pharmacogenetics: associations with pharmacokinetics, treatment response and tolerability. Pharmacogenomics. 2015;16(13):1513–1520 [DOI] [PubMed] [Google Scholar]
- 105.Kambeitz J, Romanos M, Ettinger U. Meta-analysis of the association between dopamine transporter genotype and response to methylphenidate treatment in ADHD. Pharmacogenomics J. 2014;14(1):77–84 [DOI] [PubMed] [Google Scholar]
- 106.Bruxel EM, Akutagava-Martins GC, Salatino-Oliveira A, et al. ADHD pharmacogenetics across the life cycle: new findings and perspectives. Am J Med Genet B Neuropsychiatr Genet. 2014;165B(4):263–282 [DOI] [PubMed] [Google Scholar]
- 107.Kieling C, Genro JP, Hutz MH, Rohde LA. A current update on ADHD pharmacogenomics. Pharmacogenomics. 2010;11(3): 407–419 [DOI] [PubMed] [Google Scholar]
- 108.Froehlich TE, McGough JJ, Stein MA. Progress and promise of attention-deficit hyperactivity disorder pharmacogenetics. CNS Drugs. 2010; 24(2):99–117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Joensen B, Meyer M, Aagaard L. Specific genes associated with adverse events of methylphenidate use in the pediatric population: a systematic literature review. J Res Pharm Pract. 2017;6(2): 65–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Swanson JM, Elliott GR, Greenhill LL, et al. Effects of stimulant medication on growth rates across 3 years in the MTA follow-up. J Am Acad Child Adolesc Psychiatry. 2007;46(8):1015–1027 [DOI] [PubMed] [Google Scholar]
- 111.Mosholder AD, Gelperin K, Hammad TA, Phelan K, Johann-Liang R. Hallucinations and other psychotic symptoms associated with the use of attention-deficit/hyperactivity disorder drugs in children. Pediatrics. 2009; 123(2):611–616 [DOI] [PubMed] [Google Scholar]
- 112.Cortese S, Holtmann M, Banaschewski T, et al. ; European ADHD Guidelines Group. Practitioner review: current best practice in the management of adverse events during treatment with ADHD medications in children and adolescents. J Child Psychol Psychiatry. 2013;54(3):227–246 [DOI] [PubMed] [Google Scholar]
- 113.Avigan M Review of AERS Data From Marketed Safety Experience During Stimulant Therapy: Death, Sudden Death, Cardiovascular SAEs (Including Stroke) Report No. D030403. Silver Spring, MD: Food and Drug Administration, Center for Drug Evaluation and Research; 2004 [Google Scholar]
- 114.Perrin JM, Friedman RA, Knilans TK; Black Box Working Group; Section on Cardiology and Cardiac Surgery. Cardiovascular monitoring and stimulant drugs for attention-deficit/hyperactivity disorder. Pediatrics. 2008; 122(2):451–453 [DOI] [PubMed] [Google Scholar]
- 115.McCarthy S, Cranswick N, Potts L, Taylor E, Wong IC. Mortality associated with attention-deficit hyperactivity disorder (ADHD) drug treatment: a retrospective cohort study of children, adolescents and young adults using the general practice research database. Drug Saf. 2009;32(11):1089–1096 [DOI] [PubMed] [Google Scholar]
- 116.Gould MS, Walsh BT, Munfakh JL, et al. Sudden death and use of stimulant medications in youths. Am J Psychiatry. 2009;166(9):992–1001 [DOI] [PubMed] [Google Scholar]
- 117.Cooper WO, Habel LA, Sox CM, et al. ADHD drugs and serious cardiovascular events in children and young adults. N Engl J Med. 2011;365(20):1896–1904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Schelleman H, Bilker WB, Strom BL, et al. Cardiovascular events and death in children exposed and unexposed to ADHD agents. Pediatrics. 2011;127(6): 1102–1110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Garnock-Jones KP, Keating GM. Atomoxetine: a review of its use in attention-deficit hyperactivity disorder in children and adolescents. Paediatr Drugs. 2009;11(3):203–226 [DOI] [PubMed] [Google Scholar]
- 120.Reed VA, Buitelaar JK, Anand E, et al. The safety of atomoxetine for the treatment of children and adolescents with attention-deficit/hyperactivity disorder: a comprehensive review of over a decade of research. CNS Drugs. 2016;30(7):603–628 [DOI] [PubMed] [Google Scholar]
- 121.Bangs ME, Tauscher-Wisniewski S, Polzer J, et al. Meta-analysis of suiciderelated behavior events in patients treated with atomoxetine. J Am Acad Child Adolesc Psychiatry. 2008;47(2): 209–218 [DOI] [PubMed] [Google Scholar]
- 122.Bangs ME, Jin L, Zhang S, et al. Hepatic events associated with atomoxetine treatment for attention-deficit hyperactivity disorder. Drug Saf. 2008; 31(4):345–354 [DOI] [PubMed] [Google Scholar]
- 123.Spencer TJ, Kratochvil CJ, Sangal RB, et al. Effects of atomoxetine on growth in children with attention-deficit/hyperactivity disorder following up to five years of treatment. J Child Adolesc Psychopharmacol. 2007;17(5):689–700 [DOI] [PubMed] [Google Scholar]
- 124.Elbe D, Reddy D. Focus on guanfacine extended-release: a review of its use in child and adolescent psychiatry. J Can Acad Child Adolesc Psychiatry. 2014; 23(1):48–60 [PMC free article] [PubMed] [Google Scholar]
- 125.Croxtall JD. Clonidine extended-release: in attention-deficit hyperactivity disorder. Paediatr Drugs. 2011;13(5): 329–336 [DOI] [PubMed] [Google Scholar]
- 126.Vaughan B, Kratochvil CJ. Pharmacotherapy of pediatric attention-deficit/hyperactivity disorder. Child Adolesc Psychiatr Clin N Am. 2012; 21(4):941–955 [DOI] [PubMed] [Google Scholar]
- 127.Hirota T, Schwartz S, Correll CU. Alpha-2 agonists for attention-deficit/hyperactivity disorder in youth: a systematic review and meta-analysis of monotherapy and add-on trials to stimulant therapy. J Am Acad Child Adolesc Psychiatry. 2014;53(2):153–173 [DOI] [PubMed] [Google Scholar]
- 128.Treuer T, Gau SS, Méndez L, et al. A systematic review of combination therapy with stimulants and atomoxetine for attention-deficit/hyperactivity disorder, including patient characteristics, treatment strategies, effectiveness, and tolerability. J Child Adolesc Psychopharmacol. 2013;23(3): 179–193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Greenhill LL, Posner K, Vaughan BS, Kratochvil CJ. Attention deficit hyperactivity disorder in preschool children. Child Adolesc Psychiatr Clin N Am. 2008;17(2):347–366, ix [DOI] [PubMed] [Google Scholar]
- 130.Wilens TE, Spencer TJ. Understanding attention-deficit/hyperactivity disorder from childhood to adulthood. Postgrad Med. 2010;122(5):97–109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Foy JM, ed. Psychotropic medications in primary care. In: Mental Health Care of Children and Adolescents: A Guide for Primary Care Clinicians. Itasca, IL: American Academy of Pediatrics; 2018: 315–374 [Google Scholar]
- 132.Wilens TE, Adler LA, Adams J, et al. Misuse and diversion of stimulants prescribed for ADHD: a systematic review of the literature. J Am Acad Child Adolesc Psychiatry. 2008;47(1): 21–31 [DOI] [PubMed] [Google Scholar]
- 133.American Academy of Pediatrics. Mental health initiatives. Available at: https://www.aap.org/en-us/advocacyand-policy/aap-health-initiatives/Mental-Health/Pages/default.aspx Accessed September 8, 2019 [Google Scholar]
- 134.Levy S, Campbell MD, Shea CL, DuPont R. Trends in abstaining from substance use in adolescents: 1975-2014. Pediatrics. 2018;142(2):e20173498. [DOI] [PubMed] [Google Scholar]
- 135.Graff Low K, Gendaszek AE. Illicit use of psychostimulants among college students: a preliminary study. Psychol Health Med. 2002;7(3):283–287 [Google Scholar]
- 136.Barkley RA, Cox D. A review of driving risks and impairments associated with attention-deficit/hyperactivity disorder and the effects of stimulant medication on driving performance. J Safety Res. 2007;38(1):113–128 [DOI] [PubMed] [Google Scholar]
- 137.Jerome L, Habinski L, Segal A. Attention-deficit/hyperactivity disorder (ADHD) and driving risk: a review of the literature and a methodological critique. Curr Psychiatry Rep. 2006;8(5): 416–426 [DOI] [PubMed] [Google Scholar]
- 138.Cox DJ, Merkel RL, Moore M, Thorndike F, Muller C, Kovatchev B. Relative benefits of stimulant therapy with OROS methylphenidate versus mixed amphetamine salts extended release in improving the driving performance of adolescent drivers with attention-deficit/hyperactivity disorder.Pediatrics. 2006;118(3). Available at: www.pediatrics.org/cgi/content/full/118/3/e704 [DOI] [PubMed] [Google Scholar]
- 139.The MTA Cooperative Group; Multimodal Treatment Study of Children with ADHD. A 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder. Arch Gen Psychiatry. 1999;56(12):1073–1086 [DOI] [PubMed] [Google Scholar]
- 140.Jensen PS, Hinshaw SP, Swanson JM, et al. Findings from the NIMH Multimodal Treatment Study of ADHD (MTA): implications and applications for primary care providers. J Dev Behav Pediatr. 2001;22(1):60–73 [DOI] [PubMed] [Google Scholar]
- 141.Pelham WE Jr, Gnagy EM. Psychosocial and combined treatments for ADHD. Ment Retard Dev Disabil Res Rev. 1999; 5(3):225–236 [Google Scholar]
- 142.Homer CJ, Klatka K, Romm D, et al. A review of the evidence for the medical home for children with special health care needs. Pediatrics. 2008;122(4). Available at: www.pediatrics.org/cgi/content/full/122/4/e922 [DOI] [PubMed] [Google Scholar]
- 143.Davila RR, Williams ML, MacDonald JT. Memorandum on clarification of policy to address the needs of children with attention deficit disorders within general and/or special education In: Parker HC, ed. The ADD Hyperactivity Handbook for Schools. Plantation, FL: Impact Publications Inc; 1991:261–268 [Google Scholar]
- 144.Harrison JR, Bunford N, Evans SW, Owens JS. Educational accommodations for students with behavioral challenges: a systematic review of the literature. Rev Educ Res. 2013;83(4): 551–597 [Google Scholar]
- 145.Committee on Pediatric Workforce. Enhancing pediatric workforce diversity and providing culturally effective pediatric care: implications for practice, education, and policy making. Pediatrics. 2013;132(4). Available at: www.pediatrics.org/cgi/content/full/132/4/e1105 [DOI] [PubMed] [Google Scholar]
- 146.Berman RS, Patel MR, Belamarich PF, Gross RS. Screening for poverty and poverty-related social determinants of health. Pediatr Rev. 2018;39(5):235–246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Solanto MV. Neuropsychopharmacological mechanisms of stimulant drug action in attention-deficit hyperactivity disorder: a review and integration. Behav Brain Res. 1998;94(1):127–152 [DOI] [PubMed] [Google Scholar]
- 148.Wagner E Chronic disease management: what will it take to improve care for chronic illness? Effect Clin Pract. 1998;1(1):2–4 [PubMed] [Google Scholar]
- 149.Brinkman WB, Sucharew H, Majcher JH, Epstein JN. Predictors of medication continuity in children with ADHD. Pediatrics. 2018;141(6):e20172580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Pliszka SR, Crismon ML, Hughes CW, et al. ; Texas Consensus Conference Panel on Pharmacotherapy of Childhood Attention Deficit Hyperactivity Disorder. The Texas Children’s Medication Algorithm Project: revision of the algorithm for pharmacotherapy of attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2006;45(6):642–657 [DOI] [PubMed] [Google Scholar]
- 151.Pringsheim T, Hirsch L, Gardner D, Gorman DA. The pharmacological management of oppositional behaviour, conduct problems, and aggression in children and adolescents with attention-deficit hyperactivity disorder, oppositional defiant disorder, and conduct disorder: a systematic review and meta-analysis. Part 1: psychostimulants, alpha-2 agonists, and atomoxetine. Can J Psychiatry. 2015; 60(2):42–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Committee on Psychosocial Aspects of Child and Family Health and Task Force on Mental Health. Policy statement--The future of pediatrics: mental health competencies for pediatric primary care. Pediatrics. 2009;124(1):410–421 [DOI] [PubMed] [Google Scholar]
- 153.Foy JM, ed. Algorithm: a process for integrating mental health care into pediatric practice In: Mental Health Care of Children and Adolescents: A Guide for Primary Care Clinicians. Itasca, IL: American Academy of Pediatrics; 2018:815 [Google Scholar]
- 154.Cheng TL, Emmanuel MA, Levy DJ, Jenkins RR. Child health disparities: what can a clinician do? Pediatrics. 2015;136(5):961–968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Stein F, Remley K, Laraque-Arena D, Pursley DM. New resources and strategies to advance the AAP’s values of diversity, inclusion, and health equity. Pediatrics. 2018;141(4):e20180177. [DOI] [PubMed] [Google Scholar]
- 156.American Academy of Pediatrics, Committee on Child Health Financing. Scope of health care benefits for children from birth through age 26. Pediatrics. 2012;129(1):185–189 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


