Abstract
Thrombocytopenia is a common laboratory finding in dengue infection. However, it usually resolves as the patient recovers from the infection. Persistent thrombocytopenia following dengue infection requires further investigation. Here, we present a case of immune thrombocytopenic purpura (ITP) following dengue infection complicated by intracranial bleeding.
Keywords: dengue fever, immune thrombocytopenic purpura, bleeding
Introduction
Immune thrombocytopenic purpura (ITP) is a common hematological disorder characterized by mucocutaneous bleeding and a low platelet count.1 It is an autoimmune condition in which pathogenic antibodies bind platelets, leading to accelerated platelet destruction and clearance.2 Generally, ITP can be classified based on its etiology (primary and secondary) or based on time elapsed since diagnosis (newly diagnosed, persistent, and chronic ITP). In children, it commonly occurs following a viral infection and tends to be self-limiting in nature in up to 80% of cases.2 Viral infections, such as human immunodeficiency virus, hepatitis C virus, varicella-zoster virus, rubella, influenza, Epstein-Barr virus, and parvovirus B19, have been reported to precede ITP occurrence.1 Here, we report on a case of ITP following dengue infection complicated by intracranial bleeding.
Case Description
A 13-year-old boy presented with a recent onset of petechiae and multiple bruises over the extremities for 2 weeks duration. Otherwise, he had no other bleeding tendencies. Three weeks prior, he had been admitted for dengue fever with positive dengue non-structural protein-1 (NS-1) and dengue serology (IgM and IgG). He was treated accordingly. His platelet count reached a nadir of 3×109/L and was in recovery trend with a count of 12×109/L at the time of discharge. Further history revealed no previous history of bleeding events and no significant family history of bleeding disorders.
Upon arrival, his vital signs were stable. Mild pallor was present without jaundice. Neither lymphadenopathy nor hepatosplenomegaly were present. Petechiae rashes and multiple bruises were noted over bilateral upper and lower limbs. Other systemic examinations were unremarkable.
His initial laboratory investigations showed anemia (hemoglobin level: 8.2g/dL), mild reticulocytosis, normal white cell count, and severe thrombocytopenia (1×109/L). His serum lactate dehydrogenase (LDH) was not elevated, and there was no evidence of indirect hyperbilirubinemia, which excluded hemolysis. His renal function and coagulation profile were normal. Peripheral blood films showed normocytic, normochromic anemia and thrombocytopenia, with no blasts or abnormal cells seen. Coomb's test and viral screenings for HIV, hepatitis B, hepatitis C were negative. His antinuclear antibody (ANA) was positive with a speckled pattern, but the anti-double stranded DNA test was negative.
He was diagnosed with ITP following recent dengue infection and started on intravenous methylprednisolone for 3 days, followed by high dose oral prednisolone (1mg/kg). Despite this regime, his platelet count did not recover and remained persistently less than 10×109/L. A bone marrow examination was suggested to his parents, but they refused. Subsequently, they insisted on discharging him against medical advice following 1 week of hospitalization with a tapering dose of steroid therapy.
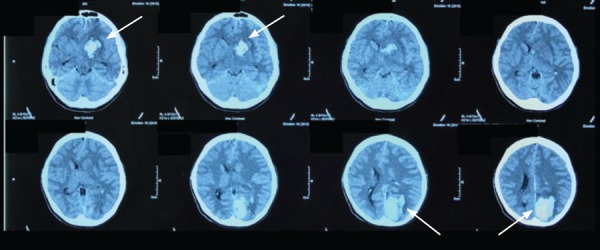
He defaulted his subsequent follow-up and presented 3 months later with sudden onset of headache and persistent vomiting. He was brought immediately to the hospital. Upon reaching the hospital, the patient was intubated and ventilated in view of his poor Glasgow coma scale (GCS). His laboratory investigations showed anemia, thrombocytopenia, and leukocytosis. His renal profile was deranged, and urgent computed tomography (CT) of the brain revealed acute intraparenchymal bleeding of the left basal ganglia and left occipital lobe with intraventricular extension and midline shift (Figure 1). A bone marrow examination revealed normocellular marrow with adequate representation of granulocytic and erythroid series but an increased megakaryocytic series (megakaryocytic thrombocytopenia) consistent with peripheral destruction of platelets. He was started on intravenous immunoglobulin (IVIG) and methylprednisolone and supported with blood products. Unfortunately, his condition deteriorated, and he passed away 6 days after admission to the intensive care unit (ICU).
Figure 1. Plain computed tomography (CT) of the brain revealed acute intraparenchymal bleeding of the left basal ganglia and left occipital lobe (arrows) with an intraventricular extension and midline shift.
Discussion
Thrombocytopenia is a common laboratory finding in dengue infection. It usually reaches its nadir during the critical phase and resolves subsequently. The pathophysiology of thrombocytopenia in dengue infection is not clearly understood. It is believed that it rests mainly on two events: decreased in bone marrow production and/or increased peripheral destruction and clearance of platelets.3,4 Immune-mediated clearance of antibody-coated platelets has been proposed as one of the mechanisms leading to thrombocytopenia. The cross-reactivity of antibodies directed against NS-1 antigen and platelets suggests the role of antiplatelet antibody in the pathogenesis of thrombocytopenia.5 In addition, complement-mediated platelets destruction plays an important role during dengue infection.6
In Europe, the annual incidence of ITP is approximately 3 to 4 per 100,000 adults/year7–8. The risk of severe hemorrhage at disease onset was less than 1% in a population-based study.9 Intracranial hemorrhage (ICH) is one of the most devastating complications in patients with ITP. Despite its rarity, it is associated with significant morbidity and mortality. Overall, the proportion of adults with ICH was reported at 1.4% compared to 9.6% for non-ICH severe hemorrhages.10
Our patient presented initially with easy bruising 3 weeks after the initial infection accompanied by severe thrombocytopenia. Post infectious ITP is relatively more common in children and adolescents compared to adults.11 In the approach to patients presenting with persistent thrombocytopenia post viral infection, the initial work-up should include taking a complete history and conducting a physical examination to assess for the presence of lymphadenopathy, hepatosplenomegaly, and other features supportive of secondary causes. Investigations should aim to exclude secondary causes of thrombocytopenia, as ITP is a diagnosis of exclusion.
Corticosteroids remain the first-line therapy in patients with ITP that developed post- dengue infections, as the majority of reported cases responded well to corticosteroid therapy.12–14 Conversely, IVIG is most useful in patients who require rapid, temporary increases in platelet counts, such as in the case of severe hemorrhages, prior to invasive procedures or in patients who are unable to tolerate corticosteroids and are awaiting second-line treatment. As the effect of IVIG only lasts for 2 to 6 weeks, second-line treatment must be instituted concurrently.15 In patients initially diagnosed with ITP, who do not respond to first-line treatment, a bone marrow examination should be carried out to exclude marrow disorders such as leukemia, lymphoma, or infiltration.16 Unfortunately, our patient did not respond well to the initial corticosteroid therapy. Thus, he was offered a bone marrow examination prior to the initiation of second-line treatment, which could include ciclosporin, danazol, splenectomy, monoclonal antibody, and thrombopoietin (TPO) receptor agonist. Unfortunately, his parents refused the examination and decided to discharge him against medical advice.
Conclusion
ITP may occur in patients diagnosed recently with dengue infection. In the presence of persistent thrombocytopenia post infection, ITP should be considered as one of the differential diagnoses after excluding other conditions with thrombocytopenia. It is important to rule out secondary causes of ITP, such as systemic lupus erythematosus, and lymphoproliferative disorders, before attributing the ITP to dengue infection. Early diagnosis and treatment is crucial in order to prevent life-threatening complications such as intracranial bleeding.
A take-home message for physicians
Better care of the patient can be achieved with shared care between the primary health care center and tertiary hospital.
Adequate monitoring of platelet trend recovery is important after an episode of dengue fever.
Persistent thrombocytopenia in dengue infection warrants urgent referral to secondary and tertiary hospitals for further investigation.
Acknowledgments
The authors would like to thank the Director General of Health Malaysia for permission to publish this article.
Funding and conflicts of interest
None.
References
- 1.Cines DB, Blanchette VS. Immune thrombocytopenic purpura. N Engl J Med. 2002;346:995–1008. doi: 10.1056/NEJMra010501. [DOI] [PubMed] [Google Scholar]
- 2.Recht M. Thrombocytopenia and anemia in infants and children. Emerg Med Clin North Am. 2009;27:505–23. doi: 10.1016/j.emc.2009.04.009. [DOI] [PubMed] [Google Scholar]
- 3.Rudnick A, Tan EE, Lucas JK, Omar MB. Mosquito-borne hemorrhagic fever in Malaya. Br Med J. 1965;1:1269–1272. doi: 10.1136/bmj.1.5445.1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.La Russa VF, Innis BL. Mechanisms of dengue virus-induced bone marrow suppression. Baillières Clin Haematol. 1995;8:249–70. doi: 10.1016/s0950-3536(05)80240-9. [DOI] [PubMed] [Google Scholar]
- 5.Falconar AKI. The dengue virus nonstructural 1 protein (NS1) generates antibodies to common epitopes on human blood clotting, integrin/adhesin proteins and binds to human endothelial cells: Potential implications in haemorrhagic fever pathogenesis. Arch Virol. 1997;142:897–916. doi: 10.1007/s007050050127. [DOI] [PubMed] [Google Scholar]
- 6.Lin CF, Lei HY, Liu CC, Liu HS, Yeh TM, Wang ST, et al. Generation of IgM anti-platelet autoantibody in dengue patients. J Med Virol. 2001;63:143–9. [PubMed] [Google Scholar]
- 7.Abrahamson PE, Hall SA, Feudjo-Tepie M, Mitrani-Gold FS, Logie J. The incidence of idiopathic thrombocytopenic purpura among adults: a population-based study and literature review. European Journal of Haematology. 2009 Aug;83(2):83–9. doi: 10.1111/j.1600-0609.2009.01247.x. [DOI] [PubMed] [Google Scholar]
- 8.Terrell DR, Beebe LA, Vesely SK, Neas BR, Segal JB, George JN. The incidence of immune thrombocytopenic purpura in children and adults: a critical review of published reports. American Journal of Hematology. 2010 Mar;85(3):174–80. doi: 10.1002/ajh.21616. [DOI] [PubMed] [Google Scholar]
- 9.Moulis G, Palmaro A, Montastruc JL, Godeau B, Lapeyre-Mestre M, Sailler L. Epidemiology of incident immune thrombocytopenia: a nationwide population-based study in France. Blood. 2014 Nov 20;124(22):3308–15. doi: 10.1182/blood-2014-05-578336. [DOI] [PubMed] [Google Scholar]
- 10.Neunert C, Noroozi N, Norman G, Buchanan GR, Goy J, Nazi I, Kelton JG, Arnold DM. Severe bleeding events in adults and children with primary immune thrombocytopenia: a systematic review. Journal of Thrombosis and Haemostasis. 2015 Mar;13(3):457–64. doi: 10.1111/jth.12813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kühne T, Buchanan GR, Zimmerman S, Michaels LA, Kohan R, Berchtold W, Imbach P. A prospective comparative study of 2540 infants and children with newly diagnosed idiopathic thrombocytopenic purpura (ITP) from the Intercontinental Childhood ITP Study Group. The Journal of Pediatrics. 2003 Nov 1;143(5):605–8. doi: 10.1067/s0022-3476(03)00535-3. [DOI] [PubMed] [Google Scholar]
- 12.Leong KW, Srinivas P. Corticosteroid-responsive prolonged thrombocytopenia following dengue hemorrhagic fever. Med J Malaysia. 1993;48:369–72. [PubMed] [Google Scholar]
- 13.De Souza LJ, Neto CG, Bastos DA, et al. Dengue and immune thrombocytopenic purpura. WHO Dengue Bull. 2005;29:136–49. [Google Scholar]
- 14.Verma SP, Hamide A, Wadhwa J, Sivamani K. Case report: corticosteroid responsive prolonged thrombocytopenia in a case of dengue fever. BMJ Case Reports. 2013;2013:bcr2013200249. doi: 10.1136/bcr-2013-200249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.George JN, Arnold DM, Leung LL, Tirnauer JS. Immune thrombocytopenia (ITP) in adults: initial treatment and prognosis. Waltham, MA: UpToDate; 2016. pp. 1–1. [Google Scholar]
- 16.Provan D, Newland AC. Primary immune thrombocytopenia. 7th. Postgraduate haematology; 2016. pp. 776–777. Chapter 42. edition. Pages. [Google Scholar]


