Abstract
Diabetes in pregnancy is associated with risks to the woman and her developing fetus. Management of the condition at the primary care level includes pre-conception care, screening, diagnosis, as well as antenatal and postpartum care. A multidisciplinary approach is essential in ensuring its holistic management.
Keywords: diabetes, pregnancy, screening, diagnosis, antenatal
Introduction
According to the National Health Morbidity Survey 2015, the prevalence of diabetes increases with age. In relation to this, the National Obstetric Report involving 14 tertiary hospitals reported that the incidence of diabetes in pregnancy was 8.66% in 2011 and 8.83% in 2012. There incidence of macrosomia doubled in diabetic patients in both years compared to the incidence in non-diabetics.
There are variations in the management of diabetes in pregnancy at the primary care level. Therefore, clinical practice guidelines (CPG) on this subject is developed below to provide a comprehensive, evidence-based management guide to assist healthcare providers in delivering high-quality care.
Screening and Diagnosis
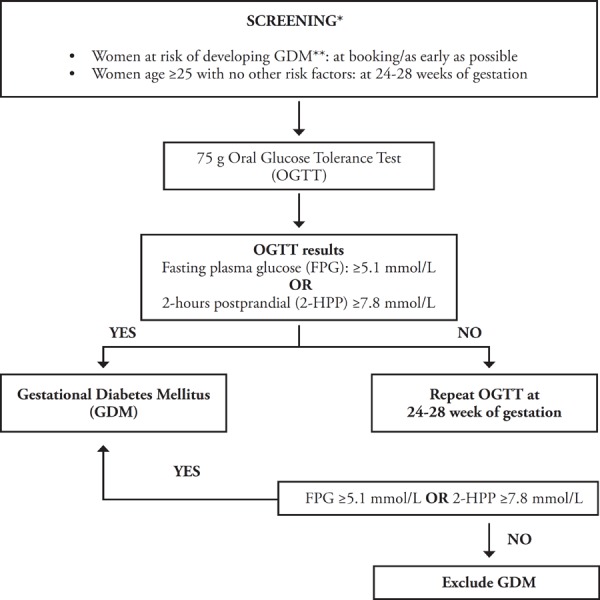
Women at risk for developing gestational diabetes mellitus (GDM) should be screened at booking using the 75-gram oral glucose tolerance test (OGTT). If the test is negative, it should be repeated at 24 – 28 weeks of gestation. Meanwhile, women aged 25 years and above with no other risk factors should be screened at 24 - 28 weeks of gestation.
- Women at risk for developing GDM include:
- Body mass index (BMI) >27 kg/m2
- Previous history of GDM
- First-degree relative with diabetes mellitus (DM)
- History of macrosomia (birth weight >4 kg)
- Poor obstetric history [unexplained intrauterine death, congenital anomalies (i.e., neural tube defects, cardiac defects), shoulder dystocia]
- Glycosuria >2+ on two occasions
- Current obstetric problems (essential hypertension, pregnancy-induced hypertension, polyhydramnios and current use of steroids)
There is no universally accepted definition of overt diabetes in pregnancy. Recognition of the condition should be made early, as its presence may imply the existence of diabetes prior to pregnancy. If the test results indicate overt diabetes, treatment and follow-up should be carried out as in pre-existing diabetes.
The diagnostic criteria for GDM and overt diabetes are as follows:
- GDM is diagnosed in the presence of any one of these results:
- Fasting plasma glucose (FPG) ≥5.1 mmol/L
- 2-hour post-glucose challenge ≥7.8 mmol/L
- Overt diabetes is suspected in the presence of at least one of the following:
- FPG ≥7.0 mmol/L
-
Random plasma glucose (RPG) ≥11.1 mmol/LHowever, the diagnosis of overt diabetes is confirmed with a second test (FPG/RPG/OGTT) on a subsequent day. OGTT is required if the FPG or RPG results do not meet the criteria for overt diabetes.
A summary of the screening and diagnosis of diabetes in pregnancy is illustrated in Algorithm A.
ALGORITHM A. SCREENING AND DIAGNOSIS OF DIABETES IN PREGNANCY.
Pre-Conception Care
Women with pre-existing Type 1 DM (T1DM) and Type 2 DM (T2DM) will benefit from preconception care because such care reduces the incidence of congenital malformation, preterm delivery and perinatal mortality.
Pre-conception care should be provided by a multidisciplinary team. Ideally, all pregnancies should be planned. The use of oral contraceptive pills (OCP) is allowed only for uncomplicated diabetes. Studies have shown that an intrauterine contraceptive device is the preferred contraceptive method. Caution should be exercised when using Depo-Provera, as it may weaken glycemic control.
Before conceiving, women with pre-existing diabetes are advised to:
reduce their weight if they are overweight or obese
exercise for at least 150 minutes per week
maintain a blood pressure below <130/80 mmHg
keep HbA1c at the optimal level (<6.5% or 48 mmol/mol)
review medications (discontinue potentially teratogenic medications)
undergo screening for diabetic complications (i.e., retinopathy and nephropathy)
undergo a cardiovascular (CV) risk assessment before withdrawal of contraception
start on a folic acid supplement (5 mg daily) three months before withdrawal of contraception
In addition, women with pre-existing diabetes should be informed of glycemic control targets and empowered to achieve control before conception. They should also be counseled on risks and expected management strategies during pregnancy.
Antenatal Care
a. Glycemic control
The self-monitoring of blood glucose (SMBG) is recommended for all pregnant women with pre-existing diabetes or GDM in order to achieve glycemic control and improve pregnancy outcomes. SMBG guides women in adjusting their medications, particularly multiple daily insulin (MDI), to achieve desired glycemic targets. Furthermore, it helps to prevent hypoglycemia and hyperglycemia episodes.
Monitoring of blood glucose is preferably done at home. The timing for SMBG is shown below:
| Timing of SMBG | Breakfast | Lunch | Dinner | |||
|---|---|---|---|---|---|---|
| Mode of treatment | Pre | Post | Pre | Post | Pre | Post/Pre-bed |
| Diet only | ✓ | ✓ | ✓ | ✓ | ||
| Oral antidiabetic agent or single- dose insulin | ✓ | ✓ | ✓ | ✓ | ||
| MDI | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
In a local setting when SMBG is not feasible, a clinic-based blood sugar profile (BSP) may be done to assess glycemic control. The frequency of BSP should be once every two weeks until delivery or more often, if indicated. However, the traditional BSP performed in the clinic/hospital may not reflect the actual day-to-day blood sugar levels The blood glucose targets should be the following:
fasting or preprandial: ≤5.3 mmol/L
1-hour postprandial: ≤7.8 mmol/L
2-hour postprandial: ≤6.7 mmol/L
Pregnant women who are on insulin or OAD should maintain a capillary blood glucose level >4.0 mmol/L.
b. Medical Nutrition Therapy
Medical nutrition therapy (MNT) consists of a nutritional diagnosis and therapy, which includes dietary intervention and counseling. MNT should be individualized according to nutritional needs and cultural preferences to ensure positive maternal and fetal outcomes. MNT for pregnant women with diabetes focuses on a carbohydrate (CHO)-controlled meal plan. The aim is to achieve and maintain optimum glycemic levels and appropriate gestational weight gain (GWG) while providing essential nutrients to promote positive maternal and fetal outcomes.
Pregnant women with the following conditions should be referred to a dietitian for early initiation of MNT:
at risk for GDM
pre-existing diabetes
at diagnosis of GDM
at initiation of insulin therapy
postpartum care
The recommended GWG is determined based on each woman's pre-pregnancy BMI as follows:
| Pre-pregnancy body weight status (BMI in kg/m2) | Total weight gain (ranges in kg) | Rate of weight gain in second and third trimester [mean (range) in kg/wk] |
|---|---|---|
| Underweight (<18.5 kg/m2) | 12.5–18.0 | 0.51 (0.44–0.58) |
| Normal weight (18.5–24.9 kg/m2) | 11.5–16.0 | 0.42 (0.35–0.50) |
| Overweight (25.0–29.9 kg/m2) | 7.0–11.5 | 0.28 (0.23–0.33) |
| Obese (≥30 kg/m2) | 5.0–9.0 | 0.22 (0.17–0.27) |
In the local setting, the BMI criteria for overweight women is 23.0 – 27.4 kg/ m2, and it is ≥27.5 kg/m2 for obesity. There is no evidence on weight gain totals and rates for local populations. However, targeting a GWG in the lower range may be recommended to improve pregnancy outcomes.
c. Oral antidiabetic agents
Metformin should be offered to women with GDM if diet and exercise do not control their blood glucose adequately within 1-2 weeks. It should be continued in women already on the treatment before pregnancy.
d. Insulin
Insulin therapy can be initiated in the outpatient setting in pregnant women with diabetes when:
blood glucose targets are not met after MNT and metformin therapy
metformin is contraindicated or unacceptable
FPG ≥7.0 mmol/L at diagnosis (with or without metformin)
there is an FPG of 6.0–6.9 mmol/L with complications, e.g., macrosomia or polyhydramnios (start insulin immediately, with or without metformin)
Human insulin is the preferred choice in pregnant women who need insulin therapy. Both rapid- and long-acting (basal) insulin analogues are as efficacious as human insulin in pregnant women with pre-existing diabetes and GDM. Women who are already on insulin analogues and have established good blood glucose control before pregnancy should continue using them during pregnancy.
Insulin analogues are associated with fewer incidences of hypoglycemia. Rapid-acting insulin analogues may be considered for women who experience frequent hypoglycemia or postprandial hyperglycemia while using human insulins during pregnancy. Long-acting insulin analogues may benefit women who experience repeated nocturnal hypoglycemia.
The preferred insulin regime for diabetes in pregnancy is MDI.
e. Pre-eclampsia prophylaxis
Low-dose aspirin (75 – 150 mg daily) should be given to prevent pre-eclampsia in women with pre-existing diabetes from 12 weeks of gestation until term.
f. Assessment of diabetes complications
In women with pre-existing diabetes, retinal and renal assessments should be performed at booking and repeated at least once throughout the pregnancy. Women with pre-existing renal disease should be managed in a combined clinic.
g. Fetal surveillance
Fetuses of women with diabetes in pregnancy are at higher risk for developing major congenital malformations, macrosomia and being large/small for their gestational age. Therefore, fetal surveillance via ultrasound scans should be offered to women with pre-existing diabetes as follows:
| Timing | Parameters |
|---|---|
| 11–14 weeks of gestation |
|
| 18–20 weeks of gestation |
|
| 28–36 weeks of gestation |
|
h. Timing and mode of delivery
Delivery timing should be determined based on the following chart:
| Condition | Timing | |
|---|---|---|
| Pre-existing | without complications | between 37+0 and 38+6 weeks |
| diabetes | with maternal or fetal complications | before 37+0 weeks |
| GDM | on diet alone with no complications | before 40+0 weeks |
| on oral antidiabetic agents or insulin | between 37+0 and 38+6 weeks | |
| with maternal or fetal complications | before 37+0 weeks | |
The mode of delivery should be individualized while taking into consideration the estimated fetal weight and obstetric factors.
Postpartum Care
Postpartum lifestyle interventions include MNT, physical activity and behavioral modifications. These interventions have been shown to be effective in reducing weight and insulin resistance as well as the development of T2DM among women with a history of GDM. Contraception counselling should be individualized with an emphasis on planned future pregnancies.
a. Pre-existing diabetes
Women with insulin-treated pre-existing diabetes should reduce their insulin immediately after birth and monitor their blood glucose levels carefully to establish the appropriate dose. Postnatally, women are more likely to experience hypoglycemia, especially during breastfeeding. Therefore, they should be advised to have a meal or snack before or during feeds.
b. Gestational diabetes mellitus
Most women diagnosed with GDM should be able to discontinue their diabetes medications immediately after delivery.
In women with a history of GDM, OGTT should be performed at six weeks after delivery to detect diabetes and pre-diabetes. If the result is normal, annual screenings for diabetes should be performed. However, if the OGTT result is abnormal, metformin and intensive lifestyle interventions should be considered to prevent diabetes. Breastfeeding for at least 3 months should be encouraged to reduce the risk of diabetes.
Acknowledgements
Details of the evidence supporting the above statements can be found in the CPG on the Management of Diabetes in Pregnancy 2017, which is available on the following websites: http://www.moh.gov.my (Ministry of Health Malaysia) and http://www.acadmed.org.my (Academy of Medicine). Corresponding organization: CPG Secretariat, Health Technology Assessment Section, Medical Development Division, Ministry of Health Malaysia; contactable at htamalaysia@moh.gov.my.


