Abstract
Purpose
The aim of this study was to evaluate the association between changes in the type of Modic change (MC) and newly developed MCs and low back symptoms.
Methods
This retrospective study includes all the patients suffering from low back pain who has at least two magnetic resonance studies between 2013 and 2016. Patients with MC in at least one vertebra in magnetic resonance imaging (MRI) images were included in the study. The patients who have periods of two MRIs less than six months were excluded.
Results
A total of 129 patients were included in the study and 774 vertebrae were evaluated. At the time of the first admission, MC was observed in 283 out of the 774 vertebrae (37%), whereas in the second admission, MC was observed in 343 of 774 (43%) vertebrae. New MCs were observed in 59 vertebrae. Two patients showed complete resolution of MC in the second admission. It was observed that patients with type 1 change were more associated with pain than other types (p=0.001).
Conclusion
In our retrospective case-control study, we have found that MCs can transform into different types or disappear completely over time. A significant positive correlation was found between the presence of MC type 1 changes in the visual analog scale(VAS).
Keywords: low back pain, magnetic resonance imaging, modic changes, spine
Introduction
It has been suggested that Modic changes (MCs) are a specific reason for low back pain (LBP) [1-3]. In recent years, it has started to be a subject that attracts attention. MCs have been determined by magnetic resonance imaging (MRI) since 1988 (Modic et al).; based on histological studies, they are divided into three types [4]. A type I MC shows a signal reduction in T1-weighted (T1w) MRI and a signal increase in T2-weighted (T2w) MRI, and, histologically, reflects inflammatory changes in the vertebral endplates [4]. A type II MC T1w and T2w show both signal increase and represent a more stable phase of degenerative disc disease but has the potential to transform into another type. A type III MC shows decreased signal intensity in both T1w and T2w and is associated with large subchondral bone sclerosis in plain radiography scans [4-5]. However, when an MC type is transformed into another, mixed MC types can develop [1,4,6-7].
The relationship between MC and LBP has been studied many times, and the presence of MC has been reported to increase pain levels [8-10]. MC type II may depict a more stable phase of degenerative disc disease but has the potential to transform into another type [11-14]. However, type 1 MC has been shown to be more correlated with LBP symptoms than other varieties in both the general population and the clinical patient group [3,15-18]. MCs are quite common in patients with LBP, but the long-term clinical effects have not yielded sufficient results. The aim of this study was to evaluate the association between changes in the type of MC, newly developed MCs, and low back symptoms.
Materials and methods
This retrospective study includes all the patients suffering from low back pain who have had at least two magnetic resonance studies between 2013 and 2016 in Ağrı state hospital. Patients with MC in at least one vertebra in MRI images were included in the study. The patients who have had at least two MRIs at less than six months were excluded. Patients who had vertebral fractures, spondylolisthesis (≥4 mm), spinal stenosis, disc extrusion, neoplasia, inflammatory vertebrae, lumbar disc herniation or lumbar stabilization were not included in the study. Annular tears, disc bulging, and facet joint degeneration were excluded. Because they are often associated with pain and creates biases about the source of low back pain.
The VAS pain score of the 129 patients in the hospital data system was examined. The VAS scores were defined as 0 indicating no pain and 10 indicating the worst pain. This study was approved by the local ethics committee and informed consent was obtained from each participant.
MR imaging method and image analysis
All MR images were obtained using a 1.5T scanner (Siemens, Munich, Germany, or Philips, Best, The Netherlands). For the present study, L1-S1, T1- and T2-weighted sagittal, and T1-weighted axial MRI images were acquired using the following protocol: slice thickness, 5 mm; slice gap, 1 mm; field of view, 280 × 240mm2; and matrix,448 × 336.
All MR images were analyzed by a radiologist who was not informed about the clinical characteristics of patients. The initial and second admission MR images of the patients were evaluated from the L1 corpus to the S1 corpus according to the criteria determined in previous studies [13]. T1 and T2 weighted sagittal images were evaluated, and the modular changes were reported as previously described in the literature (MC type I, MC type II, MC type III, MC type I / II, MC type II / III MC type I/II/III) [5].
Descriptive statistics were used for continuous variables (mean, standard deviation, minimum, maximum, median). The student's t-test was used to compare VAS scores among the Modic group. Significance was set at the 5 % level and all analyses were performed using IBM SPSS Statistics version 22 (IBM Corp., Armonk, NY).
Results
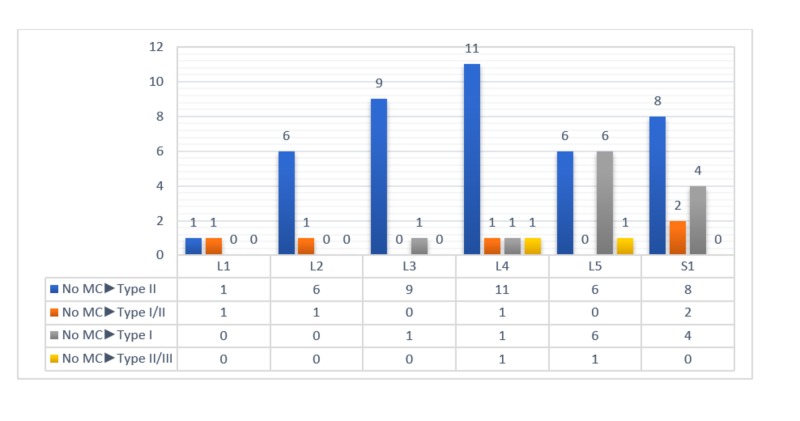
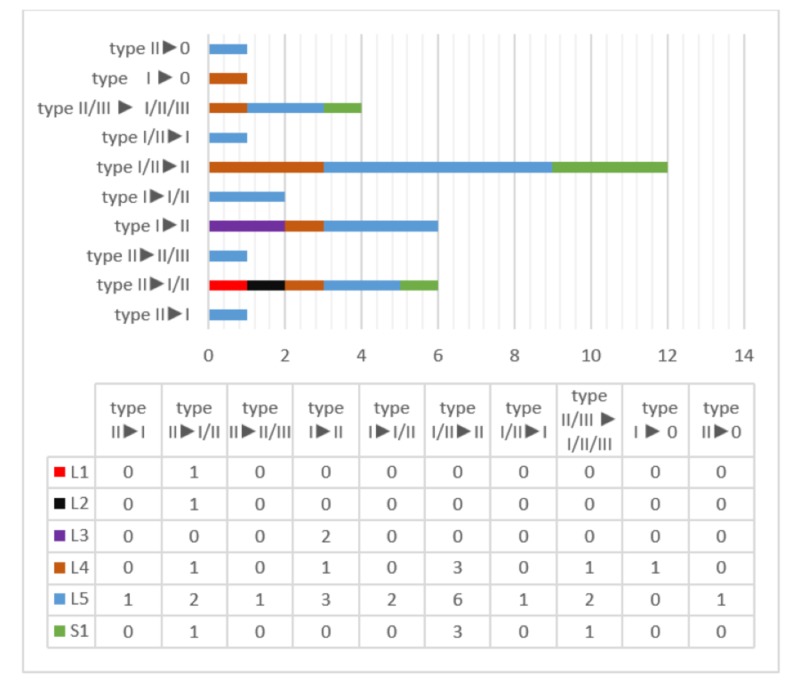
A total of 129 patients (774 vertebrae) (n = 91 (67%) females and n = 38 (33%) males) were included in the study. The mean age of the patients was 42 (min. 18 - max. 77) and the mean time between the first and second admissions was 13.3 months (6-24 months). At the time of the first admission, MC was observed in 283 of the 774 (37%) vertebrae, whereas in the second admission, MC was observed in 341 of 774 (43%) vertebrae. The first and second admissions' scanning results are shown in Table 1. New MCs were observed in 60 vertebrae (Figure 1). Twelve of these cases had type I, 41 had type II, five had type I / II, and two had type II / III. MCs were observed to be transformed in 35 vertebrae (Figure 2). MCs disappeared completely in two patients (Figure 2).
Table 1. Distribution of MCs according to vertebral level in 129 patients (774 vertebrae in total).
MC: Modic change
| First Admission | Second Admission | ||||||||||
| type I | type II | type I/II | type II/III | type I/II/III | type I | type II | type I/II | type II/III | type I/II/III | ||
| L1 | 0 | 8 | 0 | 0 | 0 | 0 | 9 | 1 | 0 | 0 | |
| L2 | 0 | 22 | 0 | 0 | 0 | 2 | 27 | 2 | 0 | 0 | |
| L3 | 5 | 39 | 2 | 0 | 0 | 2 | 49 | 3 | 0 | 0 | |
| L4 | 2 | 56 | 7 | 2 | 0 | 1 | 70 | 6 | 1 | 1 | |
| L5 | 5 | 66 | 14 | 2 | 0 | 8 | 76 | 11 | 3 | 2 | |
| S1 | 0 | 45 | 7 | 1 | 0 | 4 | 55 | 7 | 0 | 1 | |
| total | 12 | 236 | 30 | 5 | 0 | 17 | 286 | 30 | 4 | 4 | |
Figure 1. The distribution of the newly developed MCs at the time of second admission and their distribution according to MC types.
MC: Modic change
Figure 2. Transformation of MCs in the second admission according to vertebra levels and MC types.
MC: Modic change
The mean VAS score was 5.44 (SD 1.26, range 3-9) at the time of the first admission and the mean VAS score was 5.56 (SD 1.2, range 3-9) at the second admission. In the second admission, the mean VAS score of 12 patients with the new MC type 1 was 6.71 (SD 1.32, range 4-9) while the mean VAS score was 5.14 (SD 1.09, range 4-9) at the first admission (p = 0.003). The mean VAS score of patients with MC type I and M type I / II changes at the time of the first and second admission was 6.62 (SD 1.24, range 4-9) and 6.65 (SD 1.12, range 4-9) and the mean VAS score of patients without MC type I changes at the time of the first and second admissions was 5.12 (SD 1.07, range 3-7) and 5.29 (SD 1.06, range 3-8, respectively; (p = 0.001, p = 0.001, respectively).
Discussion
In the present study, we found that the transformation rate in the 13 months' mean period MCs was 12.3%. A significant positive relation was found between the development of new MC type I and transformation to MC type I from other types and the severity of pain. The transformation from MC type I to MC type II was related to a decrease in pain, but it is not statistically significant.
The present study shows that all evaluated MCs can be converted into almost any type and that they can completely disappear and not persist in follow-up (Figure 2). In our study, it was seen that 33% of vertebrae from type I / II to type II and 17% from type I to type II. However, 17% of the vertebrae were seen from MC type I / II to MC type I and 3% from MC type II to MC type I. In one patient, MC type I at L4 level in one patient, and MC type II changes at L5 level at one patient disappeared during the follow-up period. This situation does not comply with the assertion that MCs can be transformed from type I to type I / II or type II [1,4,6-7]. However, in the 14-month follow-up study conducted by Jensen et al. in 2012, they have found conflicting results with the developmental path hypothesis, as in our results [17].
The present study shows a statistically significant relationship between MC type I and the level of LBP. The VAS score of patients with MC type I at the time of first admission and second admission was significantly higher than the other types. In the recent two cohort follow-up studies, patients with MC type I at both first admission and follow-up were found to have a worse prognosis as compared to other types, which was consistent with that in our study [17,19]. The control VAS score was found to be statistically significantly higher than the first admission VAS score of patients with new MC type I (20%) and type I / II (8%) in the second control. Therefore, our findings highlight that MC type I has a stronger relationship with LBP than other MC types [4,10-11,13,20-22]. It is not clearly known how MCs cause pain. However, in human and animal studies, vertebral endplates are known to have immune reactive nerves [23-24]. When the endplate histology of patients with discogenic LBP was evaluated, more inflammation and axon growth were detected in the endplate with MC than the normal endplate cases [25]. In addition, in a one-year follow-up study of chronic LBP patients, the development of MC type I and the increase in the vertebral involvement of the current MC type I showed that adjacent disc degeneration accelerated and disc degeneration was slowed down in patients without MC type I, which suggests that MC type I may be more related to LBP symptoms [26].
There are some limitations to this study. This study did not evaluate other degenerative imaging findings (i.e., disc degeneration, disc bulging, and Schmorl’s nodes). It is based on the assumption that the only source of pain in LBP patients may be MCs. The potential effect of other degenerative MRI scan analyses of LBP symptoms, pain medication, somatic and psychological comorbidities, educational level, and other psychosocial factors have not been evaluated.
Conclusions
In our retrospective study, we have found that MCs can transform into different types or disappear completely over time. MC type I has a stronger relationship with LBP than other MC types.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained by all participants in this study
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.Vertebral end-plate (Modic) changes on lumbar spine MRI: correlation with pain reproduction at lumbar discography. Braithwaite I, White J, Saifuddin A, Renton P, Taylor BA. Eur Spine J. 1998;7:363–368. doi: 10.1007/s005860050091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Painful lumbar disk derangement: relevance of endplate abnormalities at MR imaging. Weishaupt D, Zanetti M, Hodler J, Min K, Fuchs B, Pfirrmann CW, Boos N. Radiology. 2001;218:420–427. doi: 10.1148/radiology.218.2.r01fe15420. [DOI] [PubMed] [Google Scholar]
- 3.Modic changes in endplates of lumbar vertebral bodies. Prevalence and association with low back and sciatic pain among middle-aged male workers. Kuisma M, Karppinen J, Niinimaki J, et al. Spine (Phila Pa 1976) 2007;32:1116–1122. doi: 10.1097/01.brs.0000261561.12944.ff. [DOI] [PubMed] [Google Scholar]
- 4.Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Modic MT, Steinberg PM, Ross JS, Masaryk TJ, Carter JR. Radiology. 1988;166:193–199. doi: 10.1148/radiology.166.1.3336678. [DOI] [PubMed] [Google Scholar]
- 5.Imaging of degenerative disk disease. Modic MT, Masaryk TJ, Ross JS, Carter JR. Radiology. 1988;168:177–186. doi: 10.1148/radiology.168.1.3289089. [DOI] [PubMed] [Google Scholar]
- 6.Lumbar degenerative disk disease. Modic MT, Ross JS. Radiology. 2007;245:43–61. doi: 10.1148/radiol.2451051706. [DOI] [PubMed] [Google Scholar]
- 7.Longitudinal study of vertebral type-1 end-plate changes on MR of the lumbar spine. Mitra D, Cassar-Pullicino VN, McCall IW. Eur Radiol. 2004;14:1574–1581. doi: 10.1007/s00330-004-2314-4. [DOI] [PubMed] [Google Scholar]
- 8.Painful disc lesion: can modern biplanar magnetic resonance imaging replace discography? Lei D, Rege A, Koti M, Smith FW, Wardlaw D. J Spinal Disord Tech. 2008;21:430–435. doi: 10.1097/BSD.0b013e318153f7e4. [DOI] [PubMed] [Google Scholar]
- 9.Accuracy of MRI for diagnosis of discogenic pain. O’Neill C, Kurgansky M, Kaiser J, Lau W. https://www.painphysicianjournal.com/current/pdf?article=OTkz&journal=43. Pain Physician. 2008;11:311–326. [PubMed] [Google Scholar]
- 10.Modic changes on MR images as studied with provocative diskography: clinical relevance—a retrospective study of 2457 disks. Thompson KJ, Dagher AP, Eckel TS, Clark M, Reinig JW. Radiology. 2009;250:849–855. doi: 10.1148/radiol.2503080474. [DOI] [PubMed] [Google Scholar]
- 11.MRI follow-up of subchondral signal abnormalities in a selected group of chronic low back pain patients. Luoma K, Vehmas T, Grönblad M, Kerttula L, Kääpä E. Eur Spine J. 2008;17:1300–1308. doi: 10.1007/s00586-008-0716-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Relationship of Modic type 1 change with disc degeneration: a prospective MRI study. Luoma K, Vehmas T, Grönblad M, Kerttula L, Kääpä E. Skeletal Radiol. 2009;38:237–244. doi: 10.1007/s00256-008-0611-8. [DOI] [PubMed] [Google Scholar]
- 13.A three-year follow-up of lumbar spine endplate (Modic) changes. Kuisma M, Karppinen J, Niinimäki J, Kurunlahti M, Haapea M, Vanharanta H, Tervonen O. Spine (Phila Pa 1976) 2006;31:1714–1718. doi: 10.1097/01.brs.0000224167.18483.14. [DOI] [PubMed] [Google Scholar]
- 14.Reverse transformation of Modic type 2 changes to Modic type 1 changes during sustained chronic low-back pain severity. Report of two cases and review of the literature. Marshman LA, Trewhella M, Friesem T, Bhatia CK, Krishna M. J Neurosurg Spine. 2007;6:152–155. doi: 10.3171/spi.2007.6.2.152. [DOI] [PubMed] [Google Scholar]
- 15.Modic changes and their associations with clinical findings. Kjaer P, Korsholm L, Bendix T, Sørensen JS, Leboeuf-Yde C. Eur Spine J. 2006;15:1312–1319. doi: 10.1007/s00586-006-0185-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vertebral endplate signal changes (Modic change): a systematic literature review of prevalence and association with non-specific low back pain. Jensen TS, Karppinen J, Sørensen JS, Niinimäki J, Leboeuf-Yde C. Eur Spine J. 2008;17:1407–1422. doi: 10.1007/s00586-008-0770-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Is the development of Modic changes associated with clinical symptoms? A 14-month cohort study with MRI. Jensen RK, Leboeuf-Yde C, Wedderkopp N, Sørensen JS, Jensen TS, Manniche C. Eur Spine J. 2012;21:2271–2279. doi: 10.1007/s00586-012-2309-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Type 1 Modic changes was a significant risk factor for 1-year outcome in sick-listed low back pain patients: a nested cohort study using magnetic resonance imaging of the lumbar spine. Jensen OK, Nielsen CV, Sørensen JS, Stengaard-Pedersen K. Spine J. 2014;14:2568–2581. doi: 10.1016/j.spinee.2014.02.018. [DOI] [PubMed] [Google Scholar]
- 19.Association between changes in lumbar Modic changes and low back symptoms over a two-year period. Järvinen J, Karppinen J, Niinimäki J, Haapea M, Grönblad M, Luoma K, Rinne E. BMC Musculoskelet Disord. 2015;16:98. doi: 10.1186/s12891-015-0540-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Modic changes following lumbar disc herniation. Albert HB, Manniche C. Eur Spine J. 2007;16:977–982. doi: 10.1007/s00586-007-0336-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Modic changes and associated features in Southern European chronic low back pain patients. Arana E, Kovacs FM, Royuela A, et al. Spine J. 2011;11:402–411. doi: 10.1016/j.spinee.2011.03.019. [DOI] [PubMed] [Google Scholar]
- 22.Reactive endplate marrow changes: a systematic morphologic and epidemiologic evaluation. Karchevsky M, Schweitzer ME, Carrino JA, Zoga A, Montgomery D, Parker L. Skeletal Radiol. 2005;34:125–129. doi: 10.1007/s00256-004-0886-3. [DOI] [PubMed] [Google Scholar]
- 23.Sensory and sympathetic innervation of the vertebral endplate in patients with degenerative disc disease. Brown MF, Hukkanen MV, McCarthy ID, et al. J Bone Joint Surg Br. 1997;79:147–153. doi: 10.1302/0301-620x.79b1.6814. [DOI] [PubMed] [Google Scholar]
- 24.ISSLS prize winner: the innervation of the intervertebral disc: a quantitative analysis. Fagan A, Moore R, Vernon RB, Blumbergs P, Fraser R. Spine (Phila Pa 1976) 2003;28:2570–2576. doi: 10.1097/01.BRS.0000096942.29660.B1. [DOI] [PubMed] [Google Scholar]
- 25.Tumor necrosis factor-immunoreactive cells and PGP 9.5-immunoreactive nerve fibers in vertebral endplates of patients with discogenic low back pain and Modic type 1 or type 2 changes on MRI. Ohtori S, Inoue G, Ito T, et al. Spine (Phila Pa 1976) 2006;31:1026–1031. doi: 10.1097/01.brs.0000215027.87102.7c. [DOI] [PubMed] [Google Scholar]
- 26.Modic type I change may predict rapid progressive, deforming disc degeneration: a prospective 1-year follow-up study. Kerttula L, Luoma K, Vehmas T, Gronblad M, Kaapa E. Eur Spine J. 2012;21:1135–1142. doi: 10.1007/s00586-012-2147-9. [DOI] [PMC free article] [PubMed] [Google Scholar]