Abstract
Purpose
We examined underlying psychosocial processes of a behavioral treatment for urinary incontinence (UI) of prostate cancer survivors.
Design
Secondary analysis of data collected from a clinical trial.
Sample
244 prostate cancer survivors who participated in a clinical trial of behavioral intervention to UI as intervention or control subjects.
Methods
The participants had a 3-month behavioral intervention or usual care and were followed up for an additional 3 months. They were assessed at baseline, 3, and 6 months. Latent growth curve models were performed to examine trajectories of each study variable and relationships among the variables.
Findings
Increasing self-efficacy and social support were significantly and independently associated with a greater reduction of urinary leakage frequency over time.
Implications for psychosocial oncology
Providing problem-solving skills and social support, including peer support, are essential for empowering patients to reduce UI.
Keywords: prostate cancer, urinary incontinence, self-efficacy, social support, pelvic floor muscle exercises
Urinary incontinence significantly diminishes quality of life of prostate cancer survivors.1–3 It was estimated that 42% of prostate cancer patients experienced urine leakage at one year after surgery and 14% at five years.3 Persistent incontinence can cause functioning decline, restriction of routine activities, compromised sexual and partner relations, and significant distress.4 Pelvic floor muscle exercises (PFME) have been used as a popular behavioral treatment, but its therapeutic effect is under debate partly because its working mechanism has not been well understood.5 Examination of underlying processes in this behavioral treatment can enhance our knowledge and ability to effectively treat urinary incontinence in prostate cancer survivors.
Existing evidence provides some support for behavioral treatments of incontinence. Advocates of PFME believe that regular and repeated muscle contractions strengthen pelvic sphincter muscles,6 resulting in improved urethral sphincter closure during periods of increased intravesical pressure, thus preventing leakage.7 Some studies have shown that PFME contributed to incontinence reduction in prostate cancer patients.8 Other factors such as inadequate fluid intake, caffeine or alcoholic beverage consumption, constipation or obesity, and certain medications or diseases, also worsen incontinence symptoms.9 Management of these lifestyle factors has been used increasingly to reduce incontinence symptoms based on studies of women,10,11 but the use of this management strategy in men has not been studied.6
Conceivably, PFME and symptom self-management should play a role in the recovery of urinary continence. These behaviors are fostered by perceived self-efficacy (i.e., confidence), according to social cognitive theory (SCT).12 Self-efficacy is a product of a self-regulatory process in which individuals evaluate and monitor personal actions to achieve the confidence of performing a task12. Based on the SCT, problem-solving skills (e.g., goal-setting, finding solutions, and feedback of performance) ensure successful self-monitoring and self-evaluation, knowledge of urinary incontinence and treatment promotes acquisition of problem-solving skills, and social support is a motivational factor for behavioral modification. Thus, problem-solving skills, knowledge, and social support are expected to increase self-efficacy of PFME and symptom self-management, resulting in urinary continence improvement.
Despite this theoretical conceptualization, evidence of psychosocial mechanisms of behavioral treatments for urinary incontinence is rather limited. Hohl et al.13 reported significant positive associations among self-efficacy, changes in perceived support, and increased practice of PFME in a study of prostate cancer patients. However, without evidence for the effect of these psychosocial processes on urinary outcome, the working mechanisms of behavioral treatments for urinary incontinence remain uncertain.
In recent years, we conducted a study of prostate cancer patients’ urinary incontinence in which we used problem-solving skills, knowledge, and social support to enhance the perceived self-efficacy of PFME and symptom self-management. The study interventions have been effective in improving continence and the results have been published elsewhere.14 We analyzed this study’s data to gain a better understanding of the underlying processes of the behavioral interventions, particularly the role of self-efficacy. We hypothesized that problem-solving skills, knowledge, and social support provided by the study interventions would contribute to higher levels of self-efficacy of PFME and symptom self-management, and consequently, a significant reduction of urinary incontinence in the study participants of the intervention groups, while in the participants of the control group, this mechanism would remain inactive, and hence, they would have a lack of improvement in urinary leakage.
Methods
Study design and procedures
We performed a secondary analysis of the data from a randomized clinical trial that was conducted from 2010 to 2013 in Cleveland, Ohio. In this trial, subject eligibility included early stage (I, II, or III) prostate cancer, completion of cancer treatment at least 6 months prior, and presenting incontinent symptoms. Exclusion criteria included concurrent hormonal treatment, urinary tract infection or retention, cognitive impairment, and an implant for correcting incontinence. After obtaining institutional review board approval (IRB# CC437), research staff reviewed medical charts to ascertain patient’s disease and treatment status. The International Continence Society ICSmale short form questionnaire (ICSmaleSF),15 the Short Portable Mental Status Questionnaire16 and a symptom checklist were used to screen for incontinence, cognitive impairment, and urinary infection and retention.
Eligible subjects were randomly assigned to three study groups: (a) biofeedback PFME plus a support group (BF+SUPPORT), (b) biofeedback PFME plus telephone (BF+PHONE), and (c) usual care (UC). The study groups were balanced on key variables of treatment type (surgery with and without radiotherapy vs. radiotherapy alone), surgery types (open vs. laparoscopic), radiotherapy types (brachytherapy vs. external beam), and hospital site.
The interventions consisted of two components: (a) a 60-minute biofeedback session in which the BF+SUPPORT and BF+PHONE subjects learned PFME using a computerized biofeedback machine, and (b) adapted Problem-Solving Therapy (PST)17 delivered through 6 biweekly sessions to teach problem-solving and self-management skills. The intervention subjects were asked to practice PFME 3 times daily (a primary goal) and select one of the following targets (a secondary goal): (1) consuming 2000 cc of noncaffeinated fluid with 2 or fewer caffeine drinks daily, (2) setting bladder voiding schedules, (3) maintaining a diet balanced with fiber and fluid to avoid constipation, and (4) daily exercise such as walking.
The BF+SUPPORT group consisted of 3–5 subjects each and lasted 60–75 minutes per session. The BF+PHONE group subjects had an individual telephone contact with a therapist for approximately 45 minutes in each session. Both groups discussed adherence to daily PFME and self-management skills using the manualized intervention logs. The UC subjects continued receiving usual care without receiving any intervention training sessions. All subjects were assessed at baseline, 3 months (postintervention), and 6 months (follow-up). The details of study methodology are published elsewhere.14
Measurement
The primary outcome of urinary continence was the frequency of daily leakage recorded in a diary for 3 days. The average daily frequency was calculated. The 3-day diaries have shown to be as effective and accurate as 7-day diaries, with good validity and reliability.18–21
Self-efficacy was measured based on Bandura’s guidelines for constructing self-efficacy scales22 on a 0- to 100-point scale with “0” indicating “not confident” and “100” as “certainly confident.” Eight items were measured: (1) correctly contract pelvic floor muscles, (2) maintain repetition of pelvic floor muscle contraction as much and as long as the therapist recommends at each time, (3) practice PFME every day, (4) maintain adequate fluid intake every day, (5) void at regular intervals as needed to avoid leakage, (6) avoid or manage constipation on a daily basis, (7) do regular physical exercise every day, and (8) reduce urinary leakage at will. The average score of the eight questions was used.
Problem-solving skills were measured on the 52-item Social Problem-Solving Inventory-Revised (SPSI-R) on a 5-point Likert scale. The scale has a high internal consistency, test-retest reliability, and validity. The total score of the items was calculated with a higher score indicating more competency.23
Social support was measured on the 20-item Medical Outcomes Study Social Support Survey (MOS-SSS) on a 5-point Likert scale. The item total was rescaled to a 0–100 range, with a higher score indicating more support.24 Further, the 12-item exercise habits subscale of the Social Support for Exercise Behavior Questionnaire (SSQ) was applied to assess specific support for exercise from peers and friends. The scale has good reliability and validity, producing a total score of 12 to 60.25
The 14-item Incontinence Quiz (IQZ) assesses knowledge of incontinence on a 3-point scale.26 We used a modified version of IQZ that included seven additional items to assess knowledge of self-management of PFME, fluid intake, voiding, constipation, exercise, stress, and medication that are relevant to study interventions.
Demographic, socioeconomic, and medical variables (e.g., cancer stage, treatment type, BMI, and comorbidity) were collected at the baseline and verified against the medical chart.
Statistical analysis
As the primary focus of this paper is to understand how the trajectories of self-efficacy are associated with the trajectories for frequency of leakages, latent growth curve (LGC) models were used to test this relationship. An LGC model creates separate latent constructs for the intercept and slope of a variable measured at multiple time points, which are used to define the trajectories of each participant. The intercept represents the average starting point of the slope where it crosses the y-axis at zero and the slope is the average trajectory of a variable over time. For all slopes, the intercept is the starting point of the slope or the trajectory. The intercept and slope can then be used as variables in a model. Trajectories were modeled for linear, quadratic, and freely estimated slopes by weighting the factor loadings of the measure at three time points. The best-fitting model had freely estimated slopes for self-efficacy and frequency of leakages. Freely estimated slopes can be of any shape.27 After this model was developed, the predictors (e.g., social support and problem-solving skills) were added to the latent growth model to identify their impact on the trajectories of self-efficacy and frequency of leakages. The post-intervention values of these predictors at 3 months were used in the model, because they represented the intervention outcome and could indicate how the study interventions had influenced the trajectories of self-efficacy and frequency of leakages. Additionally, the model tested how social support and peer support contributed to problem-solving skills. All models were tested for goodness of fit using the following criteria: Tucker Lewis Index (TLI) >.90, Comparative Fit Index (CFI) >.90, and the Root Mean Square Error of Approximation (RMSEA) <.08.28,29 For the control group, there was insufficient variability of urinary incontinence identified in the LGCs. Therefore, all analyses were conducted initially on the interventions groups, which were combined to suffice the power of the analyses. We then added the control group to the nested models to assess the group difference.
Results
A total of 244 participants, including 162 Intervention Group subjects and 82 Control Group (usual care) subjects, were examined in this study. The groups were of similar age (mean=65 years), race (63% Whites and 35% Blacks in both groups), marital status (65% to 63% married, respectively), education (38% to 34% college or higher degree, respectively), and employment status (44% employed in both groups). The majority of participants in both groups had stage I or II cancer (94% to 95%, respectively), surgery (53% to 57%, respectively), radiation (54% to 48%), elevated comorbidity (Charlson index score range of 0.7 to 0.95), and were overweight (mean BMI=29 kg/m2). They had similar median Gleason scores (6.6 to 7), current PSA (mean: 0.72 to 0.49), and use of medications. Their mean incontinence history was 33.2 and 26.9 months, respectively, and mean frequency of leakage was 2.8 times daily. There was no significant difference in sociodemographic and medical attributes between the study groups (see Table 1).
Table 1.
Descriptive Statistics
| Variables | Intervention Group | Control Group | ||
|---|---|---|---|---|
| N=162 | S.D. / % | N=82 | S.D. / % | |
| Age | 65 | 7.4 | 65 | 8.2 |
| Race | ||||
| White | 102 | 63% | 51 | 63.8% |
| Black | 57 | 35.2% | 28 | 35% |
| Others | 1 | 1% | 1 | 1.3% |
| Marital status (married) | 106 | 65.4% | 52 | 63.4% |
| Education | ||||
| ≥College | 62 | 38.3% | 28 | 34.2% |
| High school, associate degree | 85 | 52.5% | 47 | 57.3% |
| < High school | 15 | 9.2% | 7 | 8.5% |
| Employment (employed) | 71 | 43.8% | 36 | 43.9% |
| Cancer stage (I & II) | 152 | 94% | 78 | 95.1% |
| Surgery (yes) | 86 | 53% | 47 | 57.3% |
| Radiation (yes) | 88 | 54% | 39 | 47.6% |
| BMI | 29 | 5.1 | 29.2 | 5.4 |
| Charlson comorbidity index score | 0.7 | 1.1 | 0.95 | 1.8 |
| Gleason score (median) | 6.6 | 1.1 | 7 | 1.6 |
| Current PSA score | 0.72 | 1.8 | 0.49 | 1.3 |
| Medication use | ||||
| Anticholinergic medicine (yes) | 11 | 6.8% | 1 | 1.2% |
| α-blocker (yes) | 29 | 17.9% | 17 | 20.7% |
| Diuretic medicine (yes) | 28 | 17.3% | 20 | 24.4% |
| Frequency of daily leakage at baseline | 2.8 | 3.2 | 2.8 | 3.1 |
| Months of incontinence | 33.2 | 44.4 | 26.9 | 28.5 |
Latent Growth Curve Models
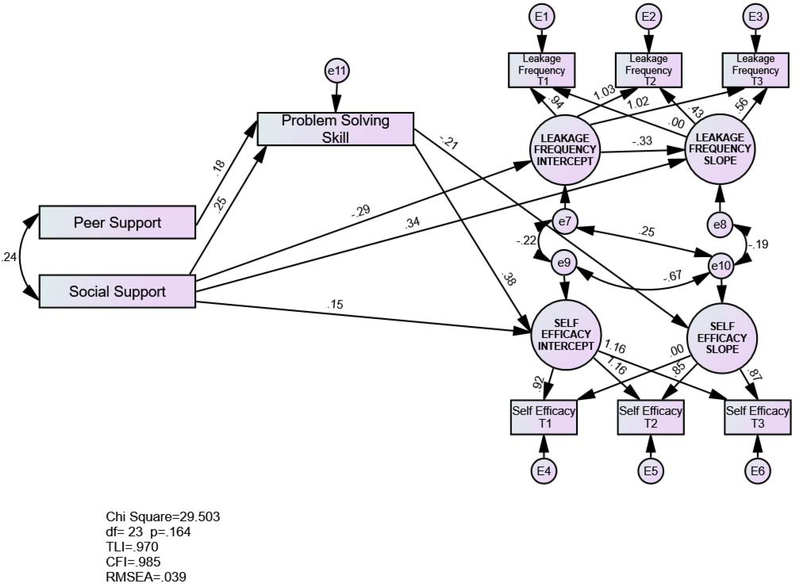
Initially, a bivariate LGC model without predictors was tested to assess the goodness of fit for the association between the trajectories of self-efficacy and frequency of leakage. The bivariate LGC model of self-efficacy and frequency of leakages fit the data well (chi square=14.96, df=9, TLI=.96, CFI=.98, RMSEA=.06). In the next step, peer support, social support, and problem-solving skills were added to the bivariate LGC model. While knowledge was part of the original conceptual model, it was not included on the LGC model because its relationships with self-efficacy and leakage frequency were not significant (see Figure 1). The initial model included all regression paths from peer support, social support, and problem-solving skills to the intercepts and slopes of self-efficacy and frequency of leakage. The regression paths from peer support and social support to problem-solving skills were also added to this model. The model was developed by removing nonsignificant paths one path at a time from the initial model (see Table 2). In order to test if the intercept of leakage frequency and social support were confounded in predicting the slope of the leakage frequency, the intercept of leakage frequency was added as a covariate in the model. Both the intercept of leakage frequency (standardized beta= −.33, unstandardized beta= −.05, p<.001) and social support (standardized beta= .34, unstandardized beta= .01, p<.01) remained significant predictors to the slope of leakage frequency. The final model fit the data well (chi square=29.44, df=23, TLI=.97, CFI=.99, RMSEA=.04). After the model was developed on the treatment group, a nested model comparing the treatment group to the control group was used to test model stability. The nested model fit was acceptable (chi square=81.45, df=48, TLI=.89, CFI=.94, RMSEA=.05). Significant differences between the treatment group and the control group in the model were identified among the structural regression weights.
Figure 1:
Latent Growth Curve Models.
Table 2.
MODEL development
| Model Step | Chi Square | df | p | TLI | CFI | RMSEA |
|---|---|---|---|---|---|---|
| 1. Initial Model | 24.29 | 15 | .06 | .94 | .98 | .06 |
| 2. Remove path Peer Support → Slope of Self Efficacy | 24.32 | 16 | .08 | .95 | .98 | .05 |
| 3. Remove path Social Support → Slope of Self Efficacy | 24.52 | 17 | .11 | .95 | .98 | .05 |
| 4. Remove path Peer Support → Intercept of Self Efficacy | 25.07 | 18 | .12 | .96 | .98 | .05 |
| 5. Remove path Problem Solving → Intercept of Leakage Frequency | 26.01 | 19 | .13 | .96 | .98 | .05 |
| 6. Remove path Problem Solving → Slope of Leakage Frequency | 26.65 | 20 | .15 | .97 | .99 | .04 |
| 7. Remove path Peer Support → Intercept of Leakage Frequency | 28.10 | 21 | .14 | .97 | .98 | .04 |
| 8. Remove path Peer Support → Slope of Leakage Frequency | 29.40 | 22 | .13 | .97 | .98 | .04 |
| 9. Remove covariance between error terms for Slope of Leakage Frequency ← → Intercept of Self Efficacy | 29.44 | 23 | .17 | .97 | .99 | .04 |
Correlations in the Bivariate Latent Growth Curve Model
There were four significant correlations among the constructs for the intercept of leakage frequency, the freely estimated slope of leakage frequency, the intercept of self-efficacy, and the freely estimated slope of self-efficacy (see Figure 1). The intercept of self-efficacy was negatively related with the freely estimated slope of self-efficacy (r= −.67). Individuals starting with lower levels of self-efficacy had more of an increase in self-efficacy over time (slope) as compared to individuals who started out with high levels of self-efficacy.
The intercept of leakage frequency was negatively related with the intercept of self-efficacy (r= −.22). Participants with a high level of self-efficacy had less leakage frequency. The freely estimated slope of leakage frequency was negatively related with the freely estimated slope of self-efficacy (r= −.19). The larger the increase in self-efficacy over time (slope) was associated with a lower leakage frequency over time (slope). The intercept of leakage frequency was positively related with the freely estimated slope of self-efficacy (r= .25). Individuals who started out with more leakage frequency had more of an increase in self-efficacy over time (slope), as these individuals needed to work more on their self-efficacy, compared to individuals who had few problems initially and therefore had less of an increase in self-efficacy over time (slope).
Predictors of the Latent Growth Curve Model for Leakage Frequency
The intercept of leakage frequency and social support were treated as covariates predicting the freely estimated slope of leakage frequency. The intercept of leakage frequency negatively predicted the freely estimated slope of leakage frequency (standardized beta= −.33, unstandardized beta=−.05, p<.01). While this may seem counterintuitive, it reflects that individuals who had more leakage frequency initially had a larger decline in leakage frequency over time (slope) as they needed to improve more, compared to individuals who had few problems initially and therefore had less decline in leakage frequency over time (slope).
Social support predicted both the intercept and the freely estimated slope of leakage frequency. Individuals with less social support had more leakage frequency initially (standardized beta= −.29, unstandardized beta=−.04, <.001). Over time, individuals receiving less social support had more decrease in leakage frequency (slope) than those receiving more social support (standardized beta=.34, unstandardized beta=.01, p<.01). This may seem counterintuitive; however, individuals with less social support and greater leakage frequency to begin with had rooms to improve more, compared to individuals who had more social support and few problems initially and thus had less room to make an improvement. This ceiling effect appears small. The unstandardized beta (.01) suggests that there is a very small decrease (.01 slope units) of leakage frequency for every 1-unit decrease in social support.
Predictors of the Latent Growth Curve Model for Self-Efficacy
Problem-solving skills predicted both the intercept and the freely estimated slope of self-efficacy, while social support only predicted the intercept of self-efficacy. Individuals with more problem-solving skills started with higher initial levels of self-efficacy (standardized beta=.38, unstandardized beta=.66, p<.001). Over time, individuals obtaining more problem-solving skills had less of a slope in self-efficacy (standardized beta =−.21, unstandardized beta=−.09, p=.05); as these individuals gained higher levels of problem-solving, their self-efficacy scores could not increase as much. Participants with more social support had higher initial levels of self-efficacy (standardized beta=15, unstandardized beta=.16, p=.02).
Predictors of Problem-Solving Skills
Peer support and social support predicted problem-solving skills. Individuals with more peer support had more problem-solving skills (standardized beta=.18, unstandardized beta=.29, p=.03). Participants with more social support had more problem-solving skills (standardized beta=.25, unstandardized beta=.16, p=.003).
Nested Models
Nested models testing for model stability compare the model between groups, by constraining the parameters estimates (e.g., regression weights) to be equal across groups. For the current model, to determine differences, regression weights were constrained to be equal. Constrained models are compared to the baseline unconstrained model, and if significant chi square differences and a drop in CFI <.01 occur, differences exist. Follow-up tests on significant differences in critical ratio comparing differences in regression paths between groups were identified. In testing for model stability, a nested model comparing treatment and groups identified significant differences in the structural regressions weight for the following four paths: Social support negatively predicted the intercept of leakage frequency in the treatment group (unstandardized beta=−.04, p=.001) and positively in the control group (unstandardized beta=.04, p<.01). Social support positively predicted the slope of leakage frequency in the treatment group (unstandardized beta=.01, p=.001) and negatively in the control group (unstandardized beta=−.01, p=.10). Problem-solving skills negatively predicted the slope of self-efficacy of leakage frequency in the treatment group (unstandardized beta=−.09, p<.05) and positively in the control group (unstandardized beta=.09, p<.09). Problem-solving skills positively predicted the intercept of self-efficacy of leakage frequency in the treatment group (unstandardized beta=.66, p<.001) and negatively in the control group (unstandardized beta=−.05, p=.83).
Discussion
The latent growth curve model analysis revealed several patterns of changes over time. Piecing the patterns together, the study findings suggest that self-efficacy of PFME and symptom self-management mediate the recovery of urinary continence and is enhanced by problem-solving skills, social support, and peer support. The recovery of urinary continence is also augmented by social support directly.
Two findings demonstrated a significant role of the self-efficacy in the reduction of urinary incontinence. First, study participants that leaked more frequently at the initial level (i.e., the intercept) have gained significantly more self-efficacy than those that leaked less frequently at the initial level. This result was supported by a positive and significant association between the intercept of daily leakage frequency and the slope (i.e., over time trajectory) of the self-efficacy (r=.25, p=.03). Second, there is a clear trend that the more the self-efficacy grew over time, the less frequent the daily leakage became, as the two trajectory slopes of the self-efficacy and daily leakage frequency correlated moderately and negatively (r=−.19, p=.09). With the participants gaining more self-efficacy while reducing incontinence, it appears that increasing self-efficacy mediated a decrease of daily leakage frequency over a 6-month period.
The study findings shed light on individual differences in the growth of self-efficacy and urinary continence. At the initial level of assessment periods (i.e., the intercept), the higher the self-efficacy, the less daily leakage frequency and vice versa (r=−.22, p=.03). However, in the trajectories of the self-efficacy over time, there appeared to be a “ceiling effect” as the self-efficacy at the initial level (i.e., intercept) was significantly and negatively associated with its slope (i.e., trajectory; r=−.67, p< .001). This finding indicates that the participants feeling less confident (i.e., lower self-efficacy) at the initial level have gained significantly more self-efficacy over time than those feeling more confident at the initial level; in other words, those starting with high self-efficacy had limited room to improve. Similarly, there was a “floor effect” in the trajectory of the daily leakage frequency, as daily leakage frequency at the initial level (i.e., the intercept) was significantly and negatively associated with its slope (i.e., trajectory; r=−.33, p=.02). This finding indicates that the participants leaking more frequently at the initial level have reduced daily leakage frequency more significantly than those leaking less frequently at the initial level; in other words, those initially having a minimal leakage problem had less to improve. Hence, those starting with worse leakage episodes gained self-efficacy and improved urinary continence significantly more over the six months.
The study findings also enlightened sources that strengthened the self-efficacy of PFME and symptom self-management. Examining the problem-solving skills as the main component of the study interventions, we found that the acquired problem-solving skills at 3 months postintervention had a positive association with the intercept and a negative association with the slope of the self-efficacy. These findings suggest that individuals possessing more problem-solving skills at 3 months started with greater self-efficacy at the initial level (standardized β=.38, p<.001); yet, those with more problem-solving skills at 3 months gained less self-efficacy over time (standardized β=−.21, p=.04). Apparently, the problem-solving skills and self-efficacy went hand in hand, but enhancement of the self-efficacy waned when the problem-solving skills had been largely acquired. Further, social support and peer support were associated with acquisition of the problem-solving skills, thus indirectly related to the self-efficacy. At 3 months postintervention, a one-unit increase of general social support contributed to an increase of problem-solving skills by 16% (standardized β=.25, p=.003), while a one-unit increase of a peer support contributed to an increase of problem-solving skills by 29% (standardized β=.18, p= .03). Moreover, social support served as an additional enhancer of the self-efficacy. An increase of social support per unit at 3 months is associated with an increase of self-efficacy by 16% (standardized β=.15, p=.02).
In parallel with the mechanism of self-efficacy, the study findings illustrated another mechanism of leakage reduction—the social support, which showed a direct effect on daily leakage frequency. In this study, the social support at 3 months postintervention had a negative association with the intercept (standardized β=−.29, p< .001) and a positive association with the slope (standardized β=.34, p< .01) of the daily leakage frequency. This is not a negative finding, as it appears that individuals with low leakage frequency initially were maintaining a low level of leakage, while individuals who had worse conditions (higher levels of leakage) at starting point were showing signs of improvement regardless of social support. The implication of these findings is that the study participants having a high level of social support started with less daily leakage episodes and thus had less room to improve over time, while those having a low level of social support started with more daily leakage episodes and thus had more room to significantly improve. This result and the initial impact of social support on leakage frequency (at the intercept) show that not only social support has an indirect effect on continence recovery through an association with problem-solving behaviors and self-efficacy, but also has an independent and direct effect on reduction of incontinence episodes. However, we need to keep in mind that the findings merely brought to light an association between social support and urinary incontinence. It is possible that social support not only impacts health behaviors,30 but also has a biological effect on incontinence reduction. Conversely, it is also possible that those who had improved continence became capable of moving around social situations and hence acquired more social support than those who continued leaking over time. The later scenario is an important consideration for patients’ social health and deserves a full consideration in future investigations.
Finally, the results from the nested models showed that although social support and problem-solving skills significantly predicted the slope of leakage frequency or both the intercept and slope of self-efficacy in the intervention group, such effects were insignificant in the control group. Obviously, the two intervention elements—social support and problem-solving skills— were not provided to the control group, and hence, did not affect their self-efficacy and leakage frequency outcome. These findings supported our hypothesis that social support and problem- solving skills are a mechanism for improving urinary continence in the intervention group, but were not operative in the control group. Contrary to the intervention group, there was a significant and positive association between social support and the intercept (initial level) of leakage frequency in the control group. Participants of the control group started with more frequent leakage frequency despite having higher social support. This perhaps suggests that social support directed at continence improvement, such as that provided in our intervention study (e.g., the social support group), is most helpful.
Overall, our study demonstrated two separate and interrelated processes of incontinence reduction: self-efficacy of PFME and symptom self-management mediates a reduction of leakage episodes, and social support reduces leakage episodes, likely through a neurological-physiological pathway. In both cases, people with severe incontinence or limited social resources benefit most from the respective mechanisms. It is noteworthy that peer support for PFME and self-management activities significantly predicted both self-efficacy (standardized β=.18, p= .03) and social support (r=.24, p=.007).
Several considerations are noted for future research and clinical practice. First, teaching problem-solving skills is essential for increasing the self-efficacy of PFME and symptom self-management and reducing urinary incontinence. Second, incorporating the social support group into the treatment modality is therapeutic and necessary. The direct effect of social support on incontinence and a potential psychoneuroimmunological mechanism deserve further investigation. The reciprocal impact of improved continence on social support is another area that warrants future research attention. Lastly, peer support from partner, relative, or friend enhances social support and self-efficacy of PFME and symptom self-management, which reduce incontinence. Incorporating peer support into behavioral treatments of urinary incontinence is worthy of exploring in the future. Herein important lessons can be drawn for improving evidence-based clinical practice.
We have reported elsewhere that both the BF+SUPPORT and BF+PHONE intervention groups had less frequent daily leakage than the UC group at 3 months (P=0.019; P≤ .001, respectively).14 In real life, this means a reduction of 1 leakage episode per day out of 3 daily leakage episodes on average. This study provided fresh evidence regarding psychosocial mechanisms of an effective behavioral treatment and contributed to our knowledge of management of urinary incontinence among prostate cancer survivors. However, this evidence must be viewed in perspective. The reported findings were generated from an intervention study in which problem-solving skill training and social support were utilized to spur individual growth. The intervention effect, especially stemming from social support, may not be evident in other types of treatment for urinary incontinence such as pharmaceutical or surgical treatment. However, this is not to say that there are no other psychosocial mechanisms for reducing urinary incontinence that have yet to be discovered and evaluated. In this analysis, knowledge was not found to be a significant predictor, probably because of a moderate internal consistency of the adapted Incontinence Quiz (Cronbach’s α=0.59, 0.60, and 0.62 at T1, T2, and T3). The 8-item self-efficacy scale, however, has a satisfactory internal consistency (Cronbach’s α=0.78 at T1 and 0.76 at T2 and T3), but we did not have data to assess reliability of these two measures. The social support measures captured the level of general social support rather than specific social support for participant’s self-management of incontinence symptoms. Also, we were unable to compare the two intervention groups to detect their difference in a growth curve due to a sample size issue. Therefore, our insight into the intervention impact on growth curve was limited. Finally, we analyzed the problem-solving skills, social support, and peer support at 3 months postintervention as exogenous factors in our model. These factors represent the intervention outcomes and ideal predictors for understanding dynamics of growth patterns. However, the impact of these factors can vary when the entire time span, including pre-intervention and follow-up time points, is taken into consideration.
Table 3.
Structural Equation Model Parameter Estimates
| Measurement Weights | ||||
| PATHS | Standardized Weights | Unstandardized Weights | Standard Error | P-value |
| Latent Growth Curves | ||||
| 1. Intercept of Leakage Frequency → Leakage Frequency Time 1 | .95 | 1.00 | NA | NA |
| 2. Intercept of Leakage Frequency → Leakage Frequency Time 2 | 1.03 | 1.00 | NA | NA |
| 3. Intercept of Leakage Frequency → Leakage Frequency Time 3 | 1.03 | 1.00 | NA | NA |
| 4. Freely Estimated Slope of Leakage Frequency → Leakage Frequency Time 1 | .00 | .00 | NA | NA |
| 5. Freely Estimated Slope of Leakage Frequency → Leakage Frequency Time 2 | .43 | 3.00 | NA | NA |
| 6. Freely Estimated Slope of Leakage Frequency → Leakage Frequency Time 3 | .56 | 4.00 | .41 | <.001 |
| 7. Intercept of Self Efficacy → Self Efficacy Time 1 | .92 | 1.00 | NA | NA |
| 8. Intercept of Self Efficacy → Self Efficacy Time 2 | 1.17 | 1.00 | NA | NA |
| 9. Intercept of Self Efficacy → Self Efficacy Time 3 | 1.16 | 1.00 | NA | NA |
| 10. Freely Estimated Slope of Self Efficacy → Self Efficacy Time 1 | .00 | .00 | NA | NA |
| 11. Freely Estimated Slope of Self Efficacy → Self Efficacy Time 2 | .85 | 3.00 | NA | NA |
| 12. Freely Estimated Slope of Self Efficacy → Self Efficacy Time 1 | .87 | 3.06 | .25 | <.001 |
| Structural Regression Weights | ||||
| Paths | Standardized Weights | Unstandardized Weights | Standard Error | P-value |
| 1. Intercept of Leakage Frequency → Freely Estimated Slope of Leakage Frequency | −.33 | −.05 | .02 | <.01 |
| 1. Social Support → Intercept of Leakage frequency | −.29 | −.04 | .01 | <.001 |
| 2. Social Support → Freely Estimated Slope of Leakage Frequency | .34 | .01 | .002 | <.01 |
| 3. Social Support → Intercept of Self Efficacy | .15 | .16 | .07 | .02 |
| 4. Problem Solving Skills → Intercept of Self Efficacy | .38 | .65 | .15 | <.001 |
| 5. Problem Solving Skills → Freely Estimated Slope of Self Efficacy | −.21 | −.09 | .045 | .05 |
| 6. Social Support → Problem Solving Skills | .25 | .16 | .05 | .003 |
| 7. Peer Support → Problem Solving Skills | .18 | .29 | .13 | .03 |
| Structural Covariances | ||||
| Paths | Correlations | Covariances | Standard Error | P-value |
| 1. Intercept of Self Efficacy ← → Freely Estimated Slope of Self Efficacy | −.67 | −91.23 | 20.39 | <.001 |
| 2. Intercept of Leakage Frequency ← → Intercept of Self Efficacy | −.22 | −14.18 | 6.48 | .03 |
| 3. Freely Estimated Slope of Leakage Frequency ← → Freely Estimated Slope of Self Efficacy | −.19 | −.39 | .24 | .09 |
| 4. Intercept of Leakage Frequency ← → Freely Estimated Slope of Self Efficacy | .25 | 4.35 | 2.01 | .03 |
| Measurement Covariances | ||||
| Paths | Correlations | Covariances | Standard Error | P-value |
| 1. Peer Support ← → Social Support | .24 | 55.45 | 20.4951 | .007 |
| Squared Multiple Correlations | ||||
| Endogenous Variable | R square | |||
| 1. Problem Solving Skills | .12 | |||
| 2. Intercept of Leakage Frequency | .09 | |||
| 3. Freely Estimated Slope of Leakage Frequency | .29 | |||
| 4. Intercept of Self Efficacy | .20 | |||
| 5. Freely Estimated Slope of Self Efficacy | .05 | |||
Acknowledgements
The study was supported by the National Institutes of Health/National Cancer Institute (R01CA127493–01A2; PI: Zhang). Cleveland Clinic, University Hospital Cleveland Medical Center, Louis Stokes Cleveland Veterans Affairs Medical Center, and the MetroHealth System, which are all affiliated with Case Western Reserve University, provided support for patient access.
Dataset Status
The data that support the findings of this study are available on request from the corresponding author, AZ. The data are not publicly available due to inclusion of information that could compromise the privacy of research participants.
Footnotes
Compliance with Ethical Standards
Informed consent was obtained from all individual participants included in the study.
There are no financial disclosures from the authors.
References
- 1.Ko WFY, Sawatzky JAV. Understanding urinary incontinence after radical prostatectomy: a nursing framework. Clinical Journal of Oncology Nursing. 2008;12(4): 647–654. [DOI] [PubMed] [Google Scholar]
- 2.Barry MJ, Gallagher PM, Skinner JS, Fowler FJ. Adverse effects of robotic-assisted laparoscopic versus open retropubic radical prostatectomy among a nationwide random sample of medicare-age men. JCO. 2012;30(6):513–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Penson DF, McLerran D, Feng Z, Li L, Albertsen PC, Gilliland FD, Hamilton A, Hoffman RM, Stephenson RA, Potosky AL, Stanford JL. 5-year urinary and sexual outcomes after radical prostatectomy: results from the prostate cancer outcomes study. J Urol. 2005;173(5):1701–1705. [DOI] [PubMed] [Google Scholar]
- 4.Martin AD, Nakamura LY, Nunez RN, Wolter CE, Humphreys MR, Castle EP. Incontinence after radical prostatectomy: a patient centered analysis and implications for preoperative counseling. The Journal of urology. 2011;186(1):204–208. [DOI] [PubMed] [Google Scholar]
- 5.Anderson CA, Omar MI, Campbell SE, Hunter KF, Cody JD & Glazener CMA. Conservative management for postprostatectomy urinary incontinence (Review). Cochrane Database Syst Rev. 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ocampo-Trujillo Á, Carbonell-González J, Martínez-Blanco A, Díaz-Hung A, Munoz CA, Ramírez-Vélez R. Pre-operative training induces changes in the histomorphometry and muscle function of the pelvic floor in patients with indication of radical prostatectomy. Actas Urológicas Españolas (English Edition). 2014;38(6):378–384. [DOI] [PubMed] [Google Scholar]
- 7.Filocamo MT, Marzi VL, Del Popolo G, Cecconi F, Marzocco M, Tosto A, & Nicita G Effectiveness of early pelvic floor rehabilitation treatment for post-prostatectomy incontinence. European Urology. 2005;48(5):734–738. [DOI] [PubMed] [Google Scholar]
- 8.Fernández RA, García-Hermoso A, Solera-Martínez M, Martín Correa MT, Morales AF, Martínez-Vizcaíno V. Improvement of continence rate with pelvic floor muscle training post-prostatectomy: A meta-analysis of randomized controlled trials. Urologia Internationalis. 2015;94:125–132. [DOI] [PubMed] [Google Scholar]
- 9.Registered Nurses’ Association of Ontario (RNAO) Nursing Best Practice Guideline-Shaping the Future of Nursing: Promoting Continence Using Prompted Voiding (Revised); 2011. http://rnao.ca/bpg/guidelines/promoting-continence-using-prompted-voiding.
- 10.Wallace SA, Roe B, Williams K, Palmer M. Bladder training for urinary incontinence in adults. Cochrane Database Syst Rev. 2004; (1). doi: 10.1002/14651858.CD001308.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Du Moulin MF, Hamers JP, Paulus A, Berendsen C, Halfens R. The role of the nurse in community continence care: a systematic review. Int J Nurs Stud. 2005;42(4):479–92. [DOI] [PubMed] [Google Scholar]
- 12.Bandura A Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, N.J.: Prentice-Hall; 1986. [Google Scholar]
- 13.Hohl DH, Knoll N, Wiedemann A, Keller J, Scholz U, Schrader M, & Burkert S. Enabling or cultivating? The role of prostate cancer patients’ received partner support and self-efficacy in the maintenance of pelvic floor exercise following tumor surgery. Ann. Behav. Med 2016;50:247–258. [DOI] [PubMed] [Google Scholar]
- 14.Zhang AY, Bodner DR, Fu AZ, Ganzler DD, Klein E, Kresevic D, Moore S, Ponsky L, Purdum M, Strauss G, Zhu H. Effects of patient-centered interventions on persistent urinary incontinence after prostate cancer treatment: A randomized controlled trial. The Journal of Urology. 2015;194(6): 1675–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Donovan JL, Peters TJ, Abrams P, Brookes ST, de aa Rosette JJ, Schafer W. Scoring the short form ICSmaleSF questionnaire. International Continence Society. J Urol. 2000;164(6):1948–55. [PubMed] [Google Scholar]
- 16.Pfeiffer E, Johnson TM, Chiofolo RC. Functional assessment of elderly subjects in four service settings. J Am Geriatr Soc. 1981;29(10):433–437. [DOI] [PubMed] [Google Scholar]
- 17.Nezu AM, Nezu CM, Friedman SH, Faddis S, Houts PS. Helping Cancer Patients Cope: A Problem-Solving Approach. Washington, DC: American Psychological Association; 1998. [Google Scholar]
- 18.Dmochowski RR, Sanders SW, Appell RA, Nitti VW, Davila GW. Bladder-health diaries: an assessment of 3-day vs 7-day entries. BJU Int. 2005;96(7):1049–54. [DOI] [PubMed] [Google Scholar]
- 19.Locher JL, Goode PS, Roth DL, Worrell RL, Burgio KL. Reliability assessment of the bladder diary for urinary incontinence in older women. J Gerontol A Biol Sci Med Sci. 2001;56(1):M32–5. [DOI] [PubMed] [Google Scholar]
- 20.Homma Y, Ando T, Yoshida M, Kageyama S, Takei M, Kimoto K, Ishizuka O, Gotoh M, Hashimoto T. Voiding and incontinence frequencies: variability of diary data and required diary length. Neurourol Urodyn. 2002;21(3):204–9. [DOI] [PubMed] [Google Scholar]
- 21.Brown JS, McNaughton KS, Wyman JF, Burgio KL, Harkaway R, Bergner D, Altman DS, Kaufman K, Girman C. Measurement characteristics of a voiding diary for use by men and women with overactive bladder. Urology. 2003;61(4):802–9. [DOI] [PubMed] [Google Scholar]
- 22.Bandura A Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215. [DOI] [PubMed] [Google Scholar]
- 23.D’Zurilla TJ, Nezu AM. Development and preliminary evaluation of the social problem-solving inventory. Psychological Assessment.1990;2(2):156–163. [Google Scholar]
- 24.Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32(6):705–14. [DOI] [PubMed] [Google Scholar]
- 25.Sallis JF, Grossman RM, Pinski RB, Patterson TL, Nader PR. The development of scales to measure social support for diet and exercise behaviors. Prev Med. 1987;16(6):825–36. [DOI] [PubMed] [Google Scholar]
- 26.Keller SL. Urinary incontinence: occurrence, knowledge, and attitudes among women aged 55 and older in a rural Midwestern setting. J Wound Ostomy Continence Nurs. 1999;26(1):30–8. [DOI] [PubMed] [Google Scholar]
- 27.Burant CJ. Latent growth curve models: Tracking changes over time. Int J Aging Hum Dev. 2016;82(4):336–350. [DOI] [PubMed] [Google Scholar]
- 28.Bentler PM, Bonett DG. Significance tests and goodness of fit in the analysis of covariance structures. Psychol Bull. 1980;88(3):588–606. [Google Scholar]
- 29.Browne MW, Cudeck R. Alternative ways of assessing model fit In Bollen KA & Long JS (Eds.), Testing structural equation models. Newbury Park, CA: Sage; 1993. [Google Scholar]
- 30.Reblin M, Uchino BN. Social and emotional support and its implication for health. Curr Opin Psychiatry. 2008; 21(2): 201–2015. [DOI] [PMC free article] [PubMed] [Google Scholar]