Abstract
Background:
Childhood maltreatment has been related to adverse outcomes on social, cognitive, and biological development with sequelae present throughout the lifespan. As such, caregivers maltreated in childhood may face a different set of challenges and interpersonal stressors in rearing their children. Parental history of maltreatment has the potential to increase the risk of parental depression and exposure to maltreatment in the next generation, both of which can have a negative effect on children’s development.
Objective:
The purpose of this study is to investigate maternal depression and child experiences of maltreatment as mediators of the relationship between mothers’ own maltreatment experiences and child emotion dysregulation in children aged 10–12.
Participants and Setting:
378 low-income mothers and their children were recruited to participate in a research summer camp from 2004–2007.
Methods:
Mothers self-reported on their experiences of maltreatment in childhood and current depressive symptoms. Current generation child maltreatment information was coded from Child Protective Services records. Child emotion dysregulation (rated by camp counselors) was the outcome measure in this study. Structural equation modeling was employed to test associations between maternal maltreatment and child emotion dysregulation.
Results:
Maternal history of maltreatment related to both child maltreatment (β=.24, SE=.052, p<.001) and greater maternal depressive symptoms (β=.28, SE=.049, p<.001). Only child maltreatment mediated the effect of mothers’ maltreatment on child emotion dysregulation (95%CI: .005 - .023).
Conclusions:
In this low-income sample, the rate of intergenerational maltreatment is high and represents a pathway of influence that increases risk for maladaptive socioemotional child development.
Keywords: childhood maltreatment, intergenerational maltreatment, emotion dysregulation, maternal depression
Introduction
Childhood maltreatment represents a severe violation of safety and wellbeing experienced by children in a relational context. Early parenting experiences have an organizational effect on children’s emotions and behavior, and heterogeneous maltreatment experiences can disrupt normative development in a variety of ways (Cicchetti, 1989). Research on the effects of maltreatment in childhood and adulthood indicates that extreme and negative caregiving experiences can initiate processes (Cicchetti & Tucker, 1994; Masten & Cicchetti, 2010) often characterized by compromised adaptations in psychological, biological, and interpersonal domains (Cicchetti, Rogosch, Gunnar, & Toth, 2010; Cicchetti, Rogosch, Howe, & Toth, 2010; Cicchetti & Toth, 2016; Keyes et al., 2012; Kim & Cicchetti, 2010; Sheppes, Suri, & Gross, 2015). To understand the etiology and lifespan consequences of childhood maltreatment, the contribution of multiple ecological levels of the environment must be considered (Cicchetti & Lynch, 1993; Cicchetti & Rizley, 1981). Based on these theoretical perspectives and guided by a developmental psychopathology framework, this study takes an intergenerational approach to study the contributions of maternal history of maltreatment, child maltreatment, and maternal depression on childhood socio-emotional development.
Parental influences on child socio-emotional development
Parents or caregivers, their histories, and their emotional and behavioral functioning contribute to the complex environment in which children develop. As such, early parent-child dyadic interactions serve as the context for the attachment relationship. Parents who are warm, sensitive, and readily available form secure attachments with their infants, while frightening, unavailable, or systematically insensitive parents tend to form insecure attachments (Bowlby, 1969). Through these interactions, children learn to regulate biological, behavioral, and emotional domains in the context of their early caregiving environment. Caregiving relationships organize behavior and emotions in a formative way by providing an important framework for future expectations about relationships and social interactions (Sroufe & Waters, 1977).
Throughout early childhood and into later development, child capacities for social functions and emotional and behavioral expression become more complex. A child’s ability to regulate their internal state becomes closely tied to social competence (Thompson, Lewis, & Calkins, 2008). Emotion regulation abilities help organize and initiate behavior and allow for successful engagement with the social environment (Cicchetti, Ackerman, & Izard, 1995; Cole & Deater-Deckard, 2009), providing an important foundation from which children can go on to succeed at social tasks and interactions. In contrast, children who display greater emotion dysregulation tend to have more behavioral and conduct problems in childhood and are at increased risk for violence and criminology in adolescence and adulthood (Cole, Teti, & Zahn-Waxler, 2003). Furthermore, emotion dysregulation across the lifespan is a hallmark symptom of psychiatric illnesses and psychopathology (Cole & Deater-Deckard, 2009; Sheppes et al., 2015). Importantly, maltreatment experiences are related to higher rates of insecure attachment (Cyr, Euser, Bakermans-Kranenburg, & Van Ijzendoorn, 2010; Stronach et al., 2011), child externalizing behaviors, and emotion dysregulation (Shields & Cicchetti, 1998; Shields & Cicchetti, 2001), indicating that the disruption in safety and security experienced by maltreated children adversely affects socio-emotional development and emotional regulation capacities.
Although proximal parenting behaviors have a clear direct impact on child development, it is vital to investigate historical factors influencing parental behavior and functioning that can subsequently affect child developmental processes (Belsky, 1984). Parental history of maltreatment is one such factor that has received increasing attention in the literature as one determinant of parenting behaviors. For example, mothers who have a history of sexual or physical abuse are observed to be less emotionally available when interacting with their infants than non-maltreated mothers (Fuchs, Möhler, Resch, & Kaess, 2015; Moehler, Biringen, & Poustka, 2007). Additionally, maltreated mothers tend to have less social support and are more likely to have psychiatric diagnoses, risk factors that relate to greater rates of clinically significant emotional problems for children (Bosquet Enlow, Englund, & Egeland, 2016). Maltreated mothers may relate to their children differently than non-maltreated mothers (Gara, Allen, Herzog, & Woolfolk, 2000), suggesting that the process of interacting with and understanding a child might differ depending on a mother’s own childhood experiences with her caregivers. Furthermore, a growing body of literature suggests that maternal emotion dysregulation relates to both child maltreatment risk and child emotion dysregulation (Bridgett, Burt, Edwards, & Deater-Deckard, 2015), indicating that intergenerational patterns of maltreatment and emotion dysregulation may co-occur.
Maternal Depression
One mental health outcome consistently associated with a history of childhood maltreatment is depression (e.g.: Arnow, 2004; Keyes et al., 2012). Depression in post-natal mothers is estimated to be approximately 10% (Parsons, Young, Rochat, Kringelbach, & Stein, 2012), and maltreated parents experience more symptoms of depression than non-maltreated parents (Jaffee et al., 2013; Pears & Capaldi, 2001). Depression in adulthood is often a cyclical, recurrent disorder. Therefore, parental vulnerability to depression can have a chronic effect on children’s emotional development. Research indicates that maternal depression affects the mother-child relationship, child emotional development, attachment security, and children’s biological regulatory systems associated with bonding and emotional regulation (Apter-Levy, Feldman, Vakart, Ebstein, & Feldman, 2013; Cummings & Davies, 1994; Lovejoy, Graczyk, O’Hare, & Neuman, 2000; Morgan et al., 2015; Murray et al., 2011; Teti, Gelfand, Messinger, & Isabella, 1995). Children of depressed mothers show increased vulnerability to psychiatric disorders characterized by emotion dysregulation, such as anxiety, depression, and externalizing disorders (Conroy et al., 2012; Goodman, 2007; Kingston, Tough, & Whitfield, 2012). This research exemplifies the detrimental influence of maternal depression on child development. Maternal depression is a potential intervening variable that could help to explain the relationship between parental history of maltreatment and child emotion dysregulation.
Intergenerational Maltreatment
A history of maltreatment can also increase risk for prospective maltreatment of a parent’s child. The increased rate of continuity, or persistence, of maltreatment across the generations has received considerable attention in research on the etiology of maltreatment (Cicchetti & Rizley, 1981; DeGregorio, 2012; Thornberry & Henry, 2013; Widom, Czaja, & DuMont, 2015). The study of intergenerational maltreatment aims to understand the factors associated with maltreatment that could confer risk for maltreatment continuity (when maltreated parents maltreat their own children) as well as the factors that disrupt or begin a cycle of maltreatment (discontinuity).
Experiences of maltreatment are invariably difficult to accurately determine, creating a challenge in quantifying true rates of transmission of maltreatment across generations. There are still very few studies published that use rigorous prospective methods to measure maltreatment across two generations. However, research indicates that parental maltreatment can increase risk for prospective maltreatment experienced by offspring (Madigan et al., 2019; Widom et al., 2015), and therefore further study of intergenerational maltreatment is merited. Current research suggests that there are contextual risk and protective factors that break the cycle of abuse, or contribute to instances where parents with a history of maltreatment have children who do not experience maltreatment (Cicchetti & Aber, 1980). Conversely, there are non-maltreated parents whose children experience maltreatment. The initiation of maltreatment in one generation could be precipitated by contextual, biological, or social risk that occurs in patterns. Maltreatment occurs in the context of a family system and broader ecology surrounding a child (Cicchetti & Rizley, 1981); therefore, continuity and discontinuity of maltreatment across generations are similarly multiply determined.
Risk and protective factors influencing intergenerational transmission of maltreatment have been identified at different ecological levels proximal to the mother, child, and family unit. Parental social support and positive relationships are related to lower rates of maltreatment continuity across generations (Egeland, Jacobvitz, & Sroufe, 1988; Jaffee et al., 2013). In contrast, greater maternal negative emotionality and maternal emotion dysregulation have been shown to mediate the relationship between maternal history of maltreatment and increased risk for maltreatment perpetration (Smith, Cross, Winkler, Jovanovic, & Bradley, 2014). Maternal social information processing deficits associated with a history of physical abuse are related to severity of perpetration of physical abuse (Azar et al., 2016). These studies provide information about maltreatment risk across generations, and work is needed to link the patterns of intergenerational maltreatment to child functioning.
The present study
The purpose of this study is to test maternal depressive symptoms and child maltreatment as two pathways that are posited to link maternal maltreatment experiences and child emotion dysregulation outcomes in middle childhood. Although the association between childhood maltreatment and emotion dysregulation has been demonstrated (Shields & Cicchetti, 1997; Shields, Ryan, & Cicchetti, 2001), it is unclear which processes affected by maternal historical experiences of maltreatment confer risk for child emotion dysregulation during school-aged years. Prior studies have established that family instability, maternal emotionality, and child maltreatment are mechanisms by which parental maltreatment may affect child functioning in early childhood (Bosquet Enlow et al., 2016; Collishaw, Dunn, O’Connor, & Golding, 2007). However, there is a paucity of research, particularly in high-risk mother-child dyads, tracking effects of intergenerational maltreatment on child outcomes in which independent ratings of child maltreatment and emotional and behavioral outcomes for children are used. To advance prior research, this study includes independent (non-parental) ratings of child functioning and prospectively ascertained childhood maltreatment records of offspring. The following hypotheses were tested herein: 1) Maternal maltreatment will predict both higher levels of maternal depression and greater number of subtypes of maltreatment for their children, and 2) Maternal depression and child maltreatment experiences will mediate the relationship between maternal history of maltreatment and child emotion dysregulation.
Methods
Participants
A diverse sample (49% male; 70.5% Black, 14.6% White, 10.5% Hispanic, 4.4% other race) of low-income, school-aged children (Mean=11.24 years, SD=.98, range: 10–12yo) and their biological mothers (N=378) participated in this study. Children attended a week-long summer camp conducted by Mt. Hope Family Center during 2004–2007. The sample included 214 (56.6%) maltreated children and 164 (43.4%) non-maltreated children, with maltreatment status determined by Child Protective Service (CPS) record data.
Families were contacted via mail by the Department of Human Services (DHS) recruitment liaison. Recruitment of mothers and children with and without maltreatment was necessary to ascertain groups comparable in size and socio-economic status. Children in the maltreated group had investigations that substantiated child maltreatment according to Child Protective Services records. To recruit a socio-economically equivalent sample of non-maltreating families, families receiving Temporary Assistance for Needy Families (TANF) were offered the opportunity for participation by the Department of Human Services recruitment liaison. Child Protective Services record checks were performed for these families to ensure they did not have Child Protective Services involvement. Additionally, the Maternal Maltreatment Classification Interview (MICM; Cicchetti, Toth & Manly, 2003) was conducted with mothers to confirm the non-maltreated children did not experience maltreatment.
Eligible families could choose whether they wished to participate. Research procedures were reviewed and approved by the University of Rochester Research Subjects Review Board. For interested families, mothers provided informed consent for the study procedures that their children completed and for their own participation and consented to a review of their family’s Department of Human Services records. Children also provided signed assent agreeing to participate in study activities.
Children enrolled in the study completed the research camp over the course of 5 days. Trained camp counselors worked with the same group of 8–10 children for the duration of each weekly session of summer camp (35 hours of contact). Based on their observations and interactions with each child, counselors completed measures relating to child behavioral functioning. Mothers enrolled in this study also completed self-report measures and interviews.
Measures
Maternal Maltreatment.
Maternal maltreatment experiences were assessed with the Child Trauma Questionnaire (CTQ; Bernstein et al., 2003). This is a widely-used 28-item retrospective self-report measure that yields dimensional and categorical values of maltreatment for 5 subtypes of maltreatment: sexual abuse, physical abuse, emotional abuse, physical neglect, and emotional neglect. Responders rated the frequency with which they encountered experiences during their childhood (until age 18) on a 1–5 scale, with 1 being “never true” and 5 being “very often true.” This measure was developed carefully so that items evoked broad memories about early experiences, allowing participants to report the most accurate characterization of their own childhood (Bernstein et al., 2003). Items were also designed with language sensitive to those who have experienced maltreatment so that under-reporting of difficult memories might be avoided (Bernstein & Fink, 1998). Sample items include: “When I was growing up, people in my family hit me so hard it left me with bruises or marks,” “When I was growing up, people in my family said hurtful or insulting things to me,” and “When I was growing up, someone molested me.”
Cutoff scores for categorical (yes/no) presence of subtypes have been established by the developer of this measure and validated through the use of adult client and therapist-reported maltreatment (Bernstein & Fink, 1998; Bernstein et al., 2003). The maternal maltreatment variable used in these analyses is defined by the number of subtypes (0–5) that met cutoff scores for presence of maltreatment at the moderate/severe range. For each maltreatment subtype, scores could range from 5 to 25. Cutoff scores for moderate to severe maltreatment by subtype are as follows: for emotional maltreatment, raw scores greater than or equal to 13 indicated presence of this subtype of maltreatment, for physical abuse, scores greater than or equal to 10, for sexual abuse, scores greater or equal to 8, for emotional neglect, scores greater or equal to 15, and for physical neglect, scores greater or equal to 10.
In this sample, 60.6% of mothers (n=229) reported at least one subtype of maltreatment at the moderate/severe range on the Childhood Trauma Questionnaire. Specifically, 34.7% (n=131) reported experiencing emotional maltreatment, 33.9% (n=128) reported physical abuse, 38.1% (n=144) reported sexual abuse, 26.5% (n=100) reported emotional neglect, and 23.0% (n=87) reported physical neglect. Of the mothers meeting criteria for maltreatment in childhood, the mean number of subtypes was 2.58 (SD=1.42). In this sample, 30.13% (n=69) of maltreated mothers reported one subtype of maltreatment, 24.90% (n=57) reported 2 subtypes of maltreatment, 17.47% (n=40) reported 3 subtypes of maltreatment, 12.22% (n=28) reported 4 subtypes of maltreatment, and 15.28% (n=35) reported all 5 subtypes of maltreatment.
Maternal Depressive Symptoms.
Maternal depressive symptoms were measured by administration of the Beck Depression Inventory-II (BDI-II; Beck, Steer, & Brown, 1996), a well-validated and widely used self-report measure, yielding a total score of symptoms of depression. Mothers rated their feelings in the past two weeks by choosing one of four statements describing specific symptoms of depression, such as sadness, pessimism, and self-criticism. Answers are scored 0–3, with a higher point value indicating more severe depressive symptoms; scores were summed to yield a total score of depression severity. The 21 items on the Beck Depression Inventory-II displayed high internal consistency (Cronbach’s α=.92) in this sample. The mean total score reported was 15.92 (SD=11.31, range 0–50). Scores in this range indicate mild mood disturbance. Scores greater or equal to 20 indicate clinical-level symptoms of depression.
Child maltreatment.
Child maltreatment was coded by applying the Maltreatment Classification System (MCS; Barnett, Manly, & Cicchetti, 1993) to Child Protective Services records. The Maltreatment Classification System is a comprehensive coding system that reliably quantifies maltreatment subtype, severity, frequency, perpetrator, and developmental timing from written records or by interview. Reliable coders scored lifetime Child Protective Services records and determined the presence or absence of each subtype of maltreatment for each child. The Maltreatment Classification System identifies 4 different types of maltreatment: sexual abuse, physical abuse, emotional maltreatment, and neglect. In the Maltreatment Classification System, sexual abuse is defined as any sexual contact or attempted sexual contact that occurs between a child and a caregiver. Physical abuse is defined by instances where a child experiences a non-accidental injury inflicted by a caregiver. Four types of neglect are also scored: lack of supervision, failure to provide, educational neglect, and moral/legal neglect. Emotional maltreatment is defined by instances where the child’s psychological safety and security, acceptance/self-esteem, and/or age appropriate autonomy is compromised by a caregiver. Examples of emotional maltreatment include but are not limited to exposure to intimate partner violence, threats of (or enacted) abandonment or suicide by a caregiver, and physical restriction of movement for an extended period of time. In this study, the four main subtypes of maltreatment were included (sexual abuse, physical abuse, emotional maltreatment, and neglect), with presence of neglect indicated by presence of any of the categories of neglect described above. The number of subtypes (0–4) was used as a measure of maltreatment in the structural equation model tested in this study.
This study included 214 children who experienced one or more subtypes of maltreatment; 34.1% (n=129) experienced emotional maltreatment, 46.3% (n=175) experienced neglect, 19.0% (n=72) experienced physical abuse, and 5.3% (n=20) experienced sexual abuse. The mean number of subtypes of maltreatment experienced by maltreated children was 1.85(SD=.054); 37% (n=79) of the maltreated children experienced 1 subtype of maltreatment, 44.4% (n=95) experienced 2 subtypes of maltreatment, 15.4% (n=33) experienced 3 subtypes of maltreatment, and 3.3% (n=7) experienced 4 subtypes of maltreatment.
Child Emotion Dysregulation.
The Emotion Regulation Checklist (ERC; Shields & Cicchetti, 1997) was used to measure child emotion dysregulation. The Emotion Regulation Checklist yields two subscales: a negativity/lability subscale and an emotion regulation subscale. The negativity/lability subscale was used in this study. Higher scores on this scale indicate more emotion dysregulation difficulties. The Emotion Regulation Checklist was completed at the end of each week by camp counselors rating children they interacted with during the week on a Likert scale (0–3), from “never” to “almost always.” Sample items include: “Is easily frustrated” and “Is prone to disruptive outburst of energy and exuberance.” This is a validated and reliable measure of these constructs developed in a similar age-range of maltreated and non-maltreated children as the present study (Shields & Cicchetti, 1997). Each child was rated on items by two counselors, and the average intraclass correlation between raters for the negativity/lability subscale was .85. The mean score on the negativity/lability subscale was 1.67 (SD=.53).
Data Analytic Plan
Data were analyzed with SPSS v25 and Mplus7 Version 1.4 (Muthen & Muthén, 2012). A structural equation model (SEM) tested relationships between maternal maltreatment, maternal depression, childhood maltreatment, and child emotion dysregulation (Table 2, bivariate correlations). SEM fit was determined by fit indices including Chi-Squared (χ2) value, the comparative fit index (CFI), standardized root mean square residual (SRMR), and root mean square error of approximation (RMSEA). Good fit was determined by nonsignificant values of the χ2 statistic, values of the CFI greater than .95, SRMR values less than .08, and RMSEA values smaller than .05 (Hu & Bentler, 1999). Full information maximum likelihood (FIML) estimation was used to model missing data on endogenous variables (in this sample, n=1 missing value on a single endogenous variable). No cases were identified as outliers on univariate or multivariate dimensions (univariate skew and kurtosis values range from −.65 to .95); maximum likelihood estimation was used in this analysis. The SEM model tested mediation of the relationship between maternal maltreatment and child dysregulation by maternal depression and child maltreatment experiences using bias-corrected bootstrapping (2000 samples). ANOVA methods were used to test differences between 4 intergenerational maltreatment groups on mean levels of child emotion dysregulation. An a-priori linear contrast was specified to test a hypothesized gradient of emotion dysregulation across groups, with the maltreatment continuity group exhibiting the most dysregulation, followed by the child maltreatment only group, the maternal maltreatment only group, and then the non-maltreatment continuity group. Finally, post-hoc tests using a Bonferroni correction explored six pairwise comparisons of emotion dysregulation across intergenerational groups.
Table 2. Bivariate correlations.
presented for: maternal maltreatment, child maltreatment, maternal depression, child gender (0=male, 1=female), and child emotion dysregulation. N=378.
| Bivariate Correlations | ||||
|---|---|---|---|---|
| # Subtypes Maltreatment (Child) | # Subtypes Maltreatment (Mother) | Maternal Depression (BDI-II) | Child Gender (0=male) | |
| # Subtypes Maltreatment – (Mother) | .24** | |||
| Maternal Depression (BDI-II) | .13* | .28** | ||
| Child Gender (0=male) | −.025 | −.066 | −.007 | |
| Child Emotion Dysregulation (ERC) | .17** | .096† | .079 | −.095† |
p =.05-.10;
p<.05;
p<.01;
(all tests of significance are 2-tailed)
Results
Preliminary Analyses
Intergenerational continuity and discontinuity of maltreatment:
In this study, 229 (60.6%) of the 378 mothers in this study reported at least one subtype of maltreatment. There were significant differences in the observed patterns of maltreatment occurring across generations (χ2(1)=26.75, p<.001) with rates of maltreatment and non-maltreatment continuity exceeding those of discontinuity. Of the mothers who reported a history of maltreatment, 67.25% (154) had children who experienced maltreatment by age 10–12 (maltreatment continuity group), whereas 32.75% (75) had children who did not experience maltreatment and had not had any prior Child Protective Services involvement (mother maltreatment only group). Of the remaining 149 mothers who did not report experiencing any maltreatment in their childhood, 40.27% (60) had children who experienced maltreatment and were involved with Child Protective Services (child maltreatment only group), and 59.73% (89) of non-maltreated mothers had children who had never been involved with Child Protective Services and did not experience maltreatment at the time of the study (non-maltreatment continuity group). Conversely, among the maltreated children, 72% (154) had mothers who had been maltreated in childhood, whereas among non-maltreated children, 45.7% (75) had mothers who reported a history of being maltreated. These rates of continuity and discontinuity of intergenerational maltreatment in each intergenerational group are summarized in Table 1.
Table 1. Intergenerational maltreatment.
continuity and discontinuity presented as number of individuals and percent of column totals (N=378; χ2(1)=26.75, p<.001)
| Child Maltreatment | ||||
|---|---|---|---|---|
| Yes (% column, % row) |
No (% column, % row) |
Total (% total) |
||
| Maternal Maltreatment | Yes | Mal Continuity | MomMal Only | 229 (60.6%) |
| 154 (72.0%, 67.2%) | 75 (45.7%, 32.8%) | |||
| No | ChildMal only | NonMal Continuity | 149 (39.4%) | |
| 60 (28.0%, 40.3%) | 89 (54.3%, 59.7%) | |||
| Total | 214 (56.6%) | 164 (43.4%) | 378 | |
Note: Intergenerational maltreatment group definitions are as follows:
Maltreatment continuity: maltreatment present for mothers and children
ChildMal only: maltreatment present for children, not for mothers
MomMal only: maltreatment present for mothers, not for children
Non-mal continuity: no maltreatment present for mothers or children
Maternal History of Maltreatment and Depression:
The mean score on the Beck Depression Inventory-II for mothers fell in a range consistent with mild mood disturbances (M=15.92, SD=11.31). 129 mothers (34.1%) scored 20 points or more on the Beck Depression Inventory-II, indicating clinical-level symptoms of depression (Beck et al., 1996). The mothers who reported at least one subtype of maltreatment (n=228) had a mean score of 18.12 (SD=11.64), which was significantly higher than the mean score for mothers who did not report a history of maltreatment (M=12.54, SD=9.89; t(376)= 4.83, p<.001). Of the mothers who reported a history of maltreatment, 42.8% (n=98) scored 20 or higher, as compared to 20.8% (n=31) of mothers who reported no history of maltreatment (χ2(1)=19.42, p<.001).
Structural Equation Modeling (SEM)
SEM was used to test maternal depression and child maltreatment as mediators of the relationship between maternal history of maltreatment and child emotion dysregulation. Child emotion dysregulation, as measured by the lability/negativity subscale on the Emotion Regulation Checklist, was predicted by child maltreatment (# subtypes), maternal depression, child gender, and maternal history of maltreatment (# subtypes). Maternal history of maltreatment predicted both maternal depression and child maltreatment. Bivariate correlations among variables entered in the SEM are summarized in Table 2.
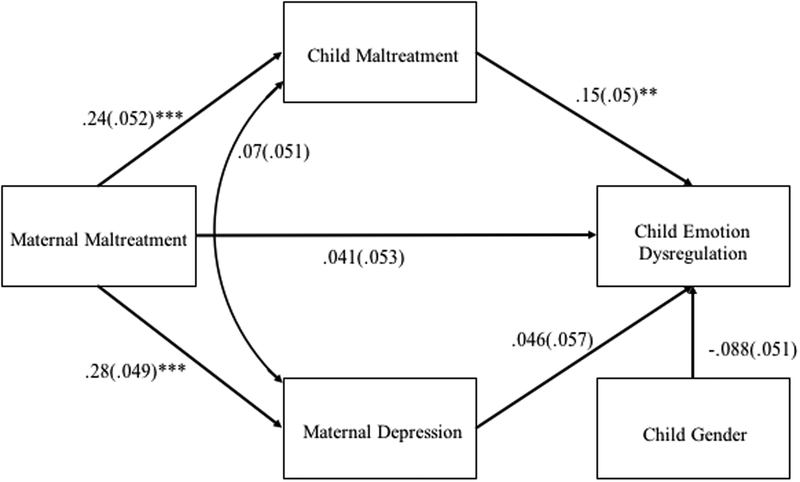
This model was an excellent fit to the data (χ2(2)= .098, p=.95, CFI = 1.0, RMSEA=0.0, SRMR = .003). Individual regression pathways were interpreted. The direct effect of maternal maltreatment on child dysregulation was not significant (β=.041, SE=.053, p=.44, ns). A greater number of subtypes of maltreatment experienced by mothers in childhood reported related to higher levels of maternal depression (β=.28, SE=.049, p<.001) and a greater number of maltreatment subtypes experienced by children (β=.24, SE=.052, p<.001). Maternal depression was not related to greater child emotion dysregulation (β=.046, SE=.057, p=.42, ns). However, a greater number of subtypes of child maltreatment was related to higher ratings of child emotion dysregulation (β=.15, SE=.050, p=.003). There was a trending effect of child gender on emotion dysregulation (β= −.088, SE=.051, p=.082), such that boys were scored higher on emotion dysregulation than girls. There was no significant relationship between correlated residuals of maternal depression and child maltreatment (β=.07, SE=.051, p=.17, ns), indicating that the unpredicted variance of maternal depression and child maltreatment are unrelated. Figure 1 presents the tested SEM with standardized parameter estimates and standard errors.
Figure 1. Structural Equation Model Results.
Standardized parameter estimates and standard errors are presented for SEM testing maternal negative emotion and child maltreatment experiences as mediators between maternal maltreatment and child dysregulation. Maternal Maltreatment is measured by the Childhood Trauma Questionnaire (number of subtypes; maternal report), maternal depressive symptoms is measured by the Beck Depression Inventory-II (maternal report). Child maltreatment was coded from Child Protective Services records, using the Maltreatment Classification System (MCS; number of subtypes). Child Emotion Dysregulation was reported by camp counselor report on the Emotion Regulation Checklist (Negativity/Lability subscale).
Note: Child gender is coded: 1=female, 0=male.
**p<.01
***p<.001
Indirect Effects of Maternal Maltreatment on Child Emotion Dysregulation:
The indirect effects between maternal maltreatment and child dysregulation were tested using bias-corrected bootstrapping (2000 samples). The 95% confidence interval for the effect of maternal maltreatment on emotion dysregulation mediated by maternal depression included 0 (Lower Limit: −.006, Upper Limit: .016) which indicates a non-significant indirect effect. The 95% confidence interval for the mediated effect of child maltreatment did not include 0 (Lower Limit: .005, Upper Limit: .023), indicating a significant indirect effect. Therefore, childhood maltreatment experienced was found to mediate the relationship between maternal maltreatment and child dysregulation, whereas maternal depression did not act as a mediator.
ANOVA Results
The relationship between maltreatment and child emotion dysregulation was further investigated using ANOVA techniques to test group differences between intergenerational groups, which were constructed based on presence or absence of maltreatment for mothers and for children. Intergenerational maltreatment groups are defined as follows: 1) maltreatment present in both generations (maltreatment continuity group; n=154; 40.74%) 2) no maternal maltreatment present, child maltreatment present (child maltreatment only group; n=60, 15.87%), 3) maternal maltreatment present, child maltreatment not present (mother maltreatment only group; n=75, 19.84%), and 4) no maltreatment present in either generation (non-maltreatment continuity group; n=89, 23.54%). A one-way ANOVA was specified with a linear contrast across intergenerational groups. Post-hoc pairwise comparisons between groups (using a Bonferroni correction) were also evaluated.
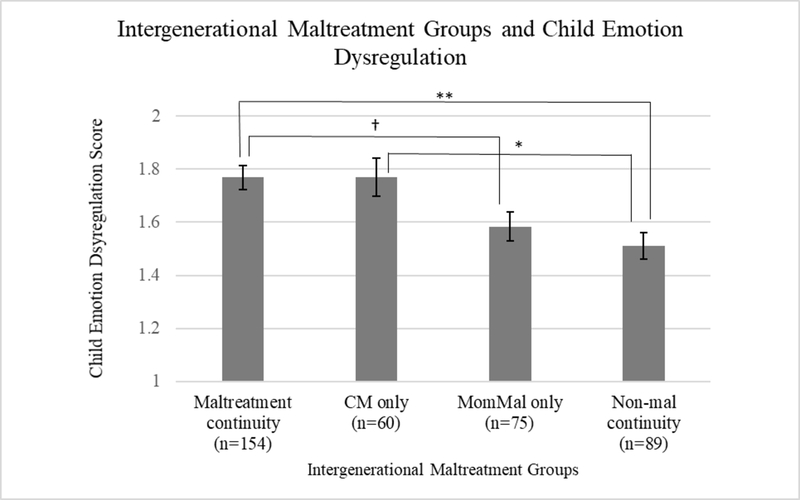
Results from the 1-way ANOVA were significant, indicating differences in child emotion regulation across intergenerational maltreatment groups (F(3, 373)=6.20, p<.001). Levene’s test of homogeneity of variances was not significant at α=.05 (F(3, 373)=1.85, p=.14), therefore homogeneity of variances was assumed. A plot of marginal means is presented in Figure 2. The linear contrast was significant (t(373)=4.30, p<.001), indicating that emotion dysregulation followed a linear trend, with highest emotion dysregulation scores present in the maltreatment continuity group, followed by the child maltreatment only group, the mother only maltreatment group, with children in the non-maltreatment continuity group scoring lowest on emotion dysregulation. Pairwise comparisons indicated that the maltreatment continuity group (M=1.77) scored higher on emotion dysregulation than the non-maltreatment continuity group (Mdiff=.26, p=.001) and marginally higher than the mother maltreatment only group (Mdiff=.18, p=.067). Additionally, the child maltreatment only group (M=1.77) scored higher than the non-maltreatment continuity group (Mdiff=.26, p=.016). No other pairwise comparisons were significant.
Figure 2.
ANOVA results. Child mean scores on emotion dysregulation are shown in each of the intergenerational maltreatment groups. Overall there are differences in emotion regulation across groups (F(3,373)=6.20, p<.001). The linear contrast across groups (left to right) is also significant (t(373)=4.30, p<.001). Pairwise comparisons (Bonferroni correction): †p =.05-.10; *p<.05; **p<.01***p<.001
Note: Intergenerational maltreatment group definitions are as follows:
Maltreatment continuity: maltreatment present for mothers and children
CM only: maltreatment present for children, not for mothers
MomMal only: maltreatment present for mothers, not for children
Non-mal continuity: no maltreatment present for mothers or children
Discussion
This study tests two mediators of the effect of maternal history of maltreatment on child emotion dysregulation. The results suggest that maternal maltreatment is related to both child maltreatment and maternal depression. However, only child maltreatment, measured as number of subtypes experienced, mediated the relationship between maternal history of maltreatment and emotion dysregulation in middle childhood. The finding that the number of subtypes of maltreatment increases relative to the number of subtypes of maltreatment experienced by mothers highlights the importance of considering maltreatment as a dimensional measure rather than a binary status. Children who experience multiple forms of maltreatment also tend to experience chronic maltreatment that occurs in patterns across development and this dimensional view explains greater variation in outcomes associated with maltreatment experiences (Villodas et al., 2012; Warmingham, Handley, Rogosch, Manly, & Cicchetti, 2019).
This mediational pathway builds upon past work documenting substantial continuity of maltreatment across generations (Madigan et al., 2019; Widom et al., 2015), and suggests that generational continuity of maltreatment can confer significant risk for maladaptive socio-emotional development in the second generation. Results are consistent with prior findings that relate intergenerational maltreatment to adverse outcomes for children (Bosquet Enlow et al., 2016) and build upon prior literature by including prospective measures of maltreatment for children and linking parental history of maltreatment to an independent rating of child functioning.
Age-typical emotion regulation capacities at this developmental stage promote adaptation to social contexts, such as school and peer groups (Rydell, Berlin, & Bohlin, 2003; Shields & Cicchetti, 2001). In contrast, emotion dysregulation has the potential to lead to greater behavior problems and increased symptoms of psychopathology (Kim & Cicchetti, 2010). Parenting dysfunction across multiple generations, indicated by a greater number of subtypes of maltreatment experienced by parents and children, is a risk factor for disruption of these adaptive emotion regulatory processes during middle childhood. This finding, although correlational, provides evidence that present day socio-emotional functioning for children is influenced by both a child’s direct experiences of maltreatment and a mother’s history of maltreatment experiences in her childhood. Interventions aimed at treating children with emotion dysregulation problems, often expressed by externalizing and/or internalizing behaviors, should consider the current family context (e.g., a child’s exposure to maltreatment and current parenting practices) as well as the historical family context is taking place (e.g., generational parenting practices, including maltreatment) in order to conceptualize the child and family’s clinical needs.
The linear trend across intergenerational groups and pairwise comparisons elucidate the potentiation of risk for child emotion dysregulation based on patterns of family experiences. As documented in the literature (Kim & Cicchetti, 2010; Warmingham et al., 2019), current generation child maltreatment has a strong impact on child emotion dysregulation, consistent with the perspective that children’s direct parenting experiences have a strong impact on the organization of their behavior and emotional development. This study does not test moderators or mediators of maltreatment transmission across generations, and thus is not able to identify additional factors that could be contribute to the initiation of maltreatment occurring in the second generation or help to explain what contributes to higher emotion dysregulation difficulties in children in the child maltreatment only group. There is research that suggests that intergenerational patterns of emotion dysregulation could potentially explain parental risk for perpetration of child maltreatment and child potential for developing less regulated responses in social settings (Bridgett et al., 2015); however, further research is needed to integrate intergenerational maltreatment and emotion regulation findings.
Prior literature suggests that maltreated mothers are more likely to experience difficulties that could affect their relationship with their child and the child’s socio-emotional development (Fuchs et al., 2015; Gara et al., 2000). Results supporting a linear trend across intergenerational groups display the importance of taking into account parental history when studying variability in child development and functioning; however, no significant differences were found between the mother maltreatment only group and the other intergenerational groups in this study, thereby limiting conclusions about the impact of maternal maltreatment in the absence of current generation child maltreatment. Consistent with extant literature, maternal history of maltreatment was related to maternal depressive symptom and increased rates of clinical-level depression (e.g.: Banyard, Williams, & Siegel, 2003). In this sample, greater depressive symptomatology for mothers did not relate to child emotion dysregulation, an expected association present in other samples across developmental stages (Goodman, 2007; Goodman & Garber, 2017; Gravener et al., 2012). Our evaluation of maternal depression does not take into account cycles of depressive episodes that often occur and have been linked to greater child symptoms (Laurent, 2014). Therefore, this evaluation of maternal depression as a possible contributor to child dysregulation could be limited by the narrow window of evaluation. Additionally, this study does not take into consideration important mechanisms involved in child risk associated with maternal depression (Goodman & Gotlib, 1999). For example, this study does not evaluate the role of multiple caregivers or fathers, who have the potential to buffer or exasperate maternal depression and/or the effect it can have on children (Dietz, Jennings, Kelley, & Marshal, 2009). It is possible that other child outcomes, such as child depressive or anxiety symptoms, would have related to variability in maternal depression (Goodman, 2007). Parental depression does influence many facets of parenting and related child functioning; in this sample, however, child maltreatment experiences exhibited a stronger influence on child emotion dysregulation ratings.
Strengths and Limitations
There are notable strengths and limitations of this study. Strengths include the multi-informant nature of the data. Child maltreatment was coded from Child Protective Services records using the reliable and well-known Maltreatment Classification System (Barnett et al., 1993), providing a thorough and systematic coding of instances of maltreatment documented from the time of a child’s birth to late childhood. Maternal report of child symptoms can be biased by maternal mood (Ordway, 2011), and maltreating parents may provide similarly biased accounts of their child’s experiences and behaviors. Therefore, inclusion of independent determinations of child maltreatment and ratings of child dysregulation is an important feature of this study’s design.
Despite these strengths, there are limitations. Due to temporal considerations, this study could not investigate mechanisms by which maternal maltreatment might increase risk for prospective child maltreatment. The transmission of maltreatment is complex, and factors that have been shown to influence the transmission were not measured in this study. Additionally, maltreatment in mothers was measured by a different method than maltreatment in children, which could influence rates of intergenerational maltreatment. Although the Childhood Trauma Questionnaire is a widely used and validated measure, maternal retrospective self-report of maltreatment experiences may be biased (Brewin, Andrews, & Gotlib, 1993). The single two-week window of assessment for maternal depression is also a limitation.
Conclusions and Future Directions
Present findings provide evidence that maternal history of maltreatment affects child dysregulation through a child’s experiences of maltreatment. Building from these results, future studies should investigate more specific patterning of intergenerational maltreatment and its effect on child functioning. Person-centered approaches, such as latent class analysis or latent transition analysis (Collins & Lanza, 2010; Lanza, Bray, & Collins, 2013) have been used to identify subgroups of maltreated children (Pears, Kim, & Fisher, 2008; Villodas et al., 2012; Warmingham et al., 2019). These approaches could be used to identify patterns of intergenerational maltreatment that are not captured by mean effects of continuity or discontinuity. Employing person-centered approaches in the study of intergenerational maltreatment could help explain differences in socioemotional and behavioral outcomes in children who experience maltreatment. Additionally, given evidence of intergenerational transmission of emotion regulation abilities (Bridgett et al., 2015), models of parental and child emotion regulation capabilities could be combined with models of intergenerational maltreatment to advance understanding of the pathways of influence between maltreatment experiences and socio-emotional functioning for parents and children.
Importantly, the study of intergenerational maltreatment has clear implications for clinical work and intervention research (Guild, Alto, & Toth, 2017). Parents with histories of trauma and maltreatment have the potential to break the cycle of violence and promote positive developmental adaptations in their children, as demonstrated herein by the group of dyads with maltreatment only present in mothers and more fully described in recent work investigating moderators and mechanisms of maltreatment transmission (Alink, Cyr, & Madigan, 2019). Importantly, parents with significant maltreatment histories are at heightened risk for displaying depressive symptoms as well as a range of other symptomatology (Cicchetti & Toth, 2016) and could benefit greatly from added supports aimed at treating mental health symptoms, decreasing parenting stress, and promoting secure attachments and positive parenting practices (Guild et al., 2017). Evidence-based interventions that target the mother-child relationship early in development and are informed by attachment theory, such as Child-Parent Psychotherapy (CPP; Lieberman, 2004) and Attachment and Bio-behavioral Catchup (ABC; Dozier et al., 2006), help parents form secure attachment relationships with their infants early in development and address basic needs and parental historical or environmental adversity that may make it challenging for parents to show sensitivity when caring for their children (Fraiberg, Adelson, & Shapiro, 1975). There is evidence that maltreatment that occurs early in a child’s life puts a child at risk for maltreatment in subsequent periods of development (Villodas et al., 2012), further emphasizing the need for early intervention to prevent maltreatment.
The present study characterizes risk for maladaptive socio-emotional development in the context of intergenerational maltreatment. The results advance understanding of the etiology of emotion dysregulation in late childhood and highlight the developmental risk associated with maternal maltreatment through experiences of maltreatment in the next generation. These findings contribute to a literature that aims to elucidate the complex etiology and effects of maltreatment throughout the lifespan. Understanding the effects of maltreatment on parents and their children is an important step in further promoting health, safety, and well-being for generations of children and parents.
Acknowledgments
This research was supported by grants received from the National Institute on Drug Abuse (R01DA17741) and the Spunk Fund, Inc.
References
- Alink LRA, Cyr C, & Madigan S (2019). The effect of maltreatment experiences on maltreating and dysfunctional parenting: A search for mechanisms. Development and Psychopathology, 31(1), 1–7. 10.1017/S0954579418001517 [DOI] [Google Scholar]
- Apter-Levy Y, Feldman M, Vakart A, Ebstein RP, & Feldman R (2013). Impact of maternal depression across the first 6 years of life on the child’s mental health, social engagement, and empathy: The moderating role of oxytocin. American Journal of Psychiatry, 170(10), 1161–1168. 10.1176/appi.ajp.2013.12121597 [DOI] [PubMed] [Google Scholar]
- Arnow BA (2004). Relationships between childhood maltreatment, adult health and psychiatric outcomes, and medical utilization. Journal of Clinical Psychiatry, 65(SUPPL. 12), 10–15. 10.4088/JCP.v65n0103 [DOI] [PubMed] [Google Scholar]
- Azar ST, Miller EA, McGuier DJ, Stevenson MT, ODonnell E, Olsen N, & Spence N (2016). Maternal Social Information Processing and the Frequency and Severity of Mother-Perpetrated Physical Abuse. Child Maltreatment, 21(4), 308–316. 10.1177/1077559516668047 [DOI] [PubMed] [Google Scholar]
- Banyard VL, Williams LM, & Siegel JA (2003). The Impact of Complex Trauma and Depression on Parenting: An Exploration of Mediating Risk and Protective Factors. Child Maltreatment, 8(4), 334–349. 10.1177/1077559503257106 [DOI] [PubMed] [Google Scholar]
- Barnett D, Manly JT, & Cicchetti D (1993). Defining Child Maltreatment: The interface between policy and research. In Advances in Applied Developmental Psychology: Child Abuse, Child Development and Social Policy. (pp. 7–73.). [Google Scholar]
- Beck AT, Steer R, & Brown G (1996). BDI-II, Beck depression inventory: manual. … for Beck Depression Inventory-II [Google Scholar]
- Belsky J (1984). The Determinants of Parenting : A Process Model. Child Development, 55(1), 83–96. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, & Fink L (1998). Childhood trauma questionnaire: A retrospective self-report: Manual. The Psychological Corporation. Harcourt Brace & Company. [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, … Zule W (2003). Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse and Neglect, 27(2), 169–190. 10.1016/S0145-2134(02)00541-0 [DOI] [PubMed] [Google Scholar]
- Bosquet Enlow M, Englund MM, & Egeland B (2016). Maternal Childhood Maltreatment History and Child Mental Health: Mechanisms in Intergenerational Effects. Journal of Clinical Child and Adolescent Psychology, 00(00), 1–16. 10.1080/15374416.2016.1144189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowlby J (1969). Attachment and loss. Attachment (Vol. 1). [Google Scholar]
- Brewin CR, Andrews B, & Gotlib IH (1993). Psychopathology and Early Experience: A Reappraisal of Retrospective Reports. Psychological Bulletin, 113(1), 82–98. 10.1037/0033-2909.113.1.82 [DOI] [PubMed] [Google Scholar]
- Bridgett DJ, Burt NM, Edwards ES, & Deater-Deckard K (2015). Intergenerational Transmission of Self-Regulation : A Multidisciplinary Review and Integrative Conceptual Framework. Psychological Bulletin, 141(3), 602–654. 10.1037/a0038662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D (1989). How research on child maltreatment has informed the study of child development: Perspectives from developmental psychopathology In Cicchetti D & Carlson V (Eds.), Child maltreatment: Theory and research on the causes and consequences of child abuse and neglect (pp. 377–431). New York: Cambridge University Press. [Google Scholar]
- Cicchetti D, & Aber JL (1980). Abused children - abusive parents: An overstated case? Harvard Educational Review, 50(2), 244–255. [Google Scholar]
- Cicchetti D, Ackerman BP, & Izard CE (1995). Emotions and emotion regulation in developmental psychopathology. Development and Psychopathology, 7(01), 1 10.1017/S0954579400006301 [DOI] [Google Scholar]
- Cicchetti D, & Lynch M (1993). Toward an Ecological Transactional Model of Community Violence and Child Maltreatment - Consequences for Childrens Development. Psychiatry-Interpersonal and Biological Processes, 56(1), 96–118. 10.1521/00332747.1993.11024624 [DOI] [PubMed] [Google Scholar]
- Cicchetti D, & Rizley R (1981). Developmental perspectives on the etiology, intergenerational transmission, and sequelae of child maltreatment. New Directions for Child and Adolescent Development, 1981(11), 31–55. 10.1002/cd.23219811104 [DOI] [Google Scholar]
- Cicchetti D, Rogosch FA, Gunnar MR, & Toth SL (2010). The Differential Impacts of Early Physical and Sexual Abuse and Internalizing Problems on Daytime Cortisol Rhythm in School-Aged Children. Child Development, 81(1), 252–269. 10.1111/j.1467-8624.2009.01393.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA, Howe ML, & Toth SL (2010). The Effects of Maltreatment and Neuroendocrine Regulation on Memory Performance. Child Development, 81(5), 1504–1519. 10.1111/j.1467-8624.2010.01488.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D, & Toth SL (2016). Child Maltreatment and Developmental Psychopathology: A Multilevel Perspective. In Cicchetti D(Ed.), Developmental Psychopathology (3rd ed, Vol. 3, pp. 457–512). Wiley. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D, Toth SL, & Manly JT (2003). Mother Child Maltreatment Interview. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, & Tucker D (1994). Development and self-regulatory structures of the mind. Development and Psychopathology, 6(04), 533–549. 10.1017/S0954579400004673 [DOI] [Google Scholar]
- Cole PM, & Deater-Deckard K (2009). Emotion regulation, risk, and psychopathology. Journal of Child Psychology and Psychiatry and Allied Disciplines, 50(11), 1327–1330. 10.1111/j.1469-7610.2009.02180.x [DOI] [PubMed] [Google Scholar]
- Cole PM, Teti LO, & Zahn-Waxler C (2003). Mutual emotion regulation and the stability of conduct problems between preschool and early school age. Development and Psychopathology, 15(1), 1–18. 10.1017/S0954579403000014 [DOI] [PubMed] [Google Scholar]
- Collins LM, & Lanza S (2010). Latent class and latent transition analysis: with applications in the social, behavioral, and health sciences (1st ed). Wiley. [Google Scholar]
- Collishaw S, Dunn J, O’Connor TG, & Golding J (2007). Maternal childhood abuse and offspring adjustment over time. Development and Psychopathology, 19(2), 367–383. 10.1017/S0954579407070186 [DOI] [PubMed] [Google Scholar]
- Conroy S, Pariante CM, Marks MN, Davies HA, Farrelly S, Schacht R, & Moran P (2012). Maternal psychopathology and infant development at 18 months: The impact of maternal personality disorder and depression. Journal of the American Academy of Child and Adolescent Psychiatry, 51(1), 51–61. 10.1016/j.jaac.2011.10.007 [DOI] [PubMed] [Google Scholar]
- Cummings EM, & Davies PT (1994). Maternal Depression and Child Development. Journal of Child Psychology and Psychiatry, 35(1), 73–122. 10.1111/j.1469-7610.1994.tb01133.x [DOI] [PubMed] [Google Scholar]
- Cyr C, Euser EM, Bakermans-Kranenburg MJ, & Van Ijzendoorn MH (2010). Attachment security and disorganization in maltreating and high-risk families: A series of meta-analyses. Development and Psychopathology, 22(1), 87–108. 10.1017/S0954579409990289 [DOI] [PubMed] [Google Scholar]
- DeGregorio LJ (2012). Intergenerational Transmission of Abuse: Implications for Parenting Interventions From a Neuropsychological Perspective. Traumatology. 10.1177/1534765612457219 [DOI] [Google Scholar]
- Dietz LJ, Jennings KD, Kelley SA, & Marshal M (2009). Maternal depression, paternal psychopathology, and toddlers’ behavior problems. Journal of Clinical Child and Adolescent Psychology, 38(1), 48–61. 10.1080/15374410802575362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dozier M, Peloso E, Lindhiem O, Gordon MK, Manni M, Sepulveda S, … Levine S (2006). Developing evidence-based interventions for foster children: An example of a randomized clinical trial with infants and toddlers. Journal of Social Issues, 62(4), 767–785. 10.1111/j.1540-4560.2006.00486.x [DOI] [Google Scholar]
- Egeland B, Jacobvitz D, & Sroufe LA (1988). Breaking the Cycle of Abuse. Child Development, 59(4), 1080–1088. [DOI] [PubMed] [Google Scholar]
- Fraiberg S, Adelson E, & Shapiro V (1975). Ghosts in the nursery: A psychoanalytic approach to the problems of impaired infant-mother relationships. Journal of the American Academy of Child & Adolescent Psychiatry, 14(3), 387–421. [DOI] [PubMed] [Google Scholar]
- Fuchs A, Möhler E, Resch F, & Kaess M (2015). Impact of a maternal history of childhood abuse on the development of mother-infant interaction during the first year of life. Child Abuse and Neglect, 48, 179–189. 10.1016/j.chiabu.2015.05.023 [DOI] [PubMed] [Google Scholar]
- Gara MA, Allen LA, Herzog EP, & Woolfolk RL (2000). The abused child as parent: The structure and content of physically abused mothers’ perceptions of their babies. Child Abuse and Neglect, 24(5), 627–639. 10.1016/S0145-2134(00)00130-7 [DOI] [PubMed] [Google Scholar]
- Goodman SH (2007). Depression in Mothers. Annual Review of Clinical Psychology, 3(1), 107–135. 10.1146/annurev.clinpsy.3.022806.091401 [DOI] [PubMed] [Google Scholar]
- Goodman SH, & Garber J (2017). Evidence-Based Interventions for Depressed Mothers and Their Young Children. Child Development, 88(2), 368–377. 10.1111/cdev.12732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman SH, & Gotlib IH (1999). Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review, 106(3), 458–490. [DOI] [PubMed] [Google Scholar]
- Gravener JA, Rogosch FA, Oshri A, Narayan AJ, Cicchetti D, & Toth SL (2012). The Relations among Maternal Depressive Disorder, Maternal Expressed Emotion, and Toddler Behavior Problems and Attachment. Journal of Abnormal Child Psychology, 40(5), 803–813. 10.1007/s10802-011-9598-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guild DJ, Alto ME, & Toth SL (2017). Preventing the Intergenerational Transmission of Child Maltreatment Through Relational Interventions (pp. 127–137). Springer International Publishing; 10.1007/978-3-319-40920-7_8 [DOI] [Google Scholar]
- Hu LT, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6(1), 1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- Jaffee SR, Bowes L, Ouellet-Morin I, Fisher HL, Moffitt TE, Merrick MT, & Arseneault L (2013). Safe, stable, nurturing relationships break the intergenerational cycle of abuse: A prospective nationally representative Cohort of children in the United Kingdom. Journal of Adolescent Health, 53(4 SUPPL), 4–10. 10.1016/j.jadohealth.2013.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Eaton NR, Krueger RF, McLaughlin KA, Wall MM, Grant BF, & Hasin DS (2012). Childhood maltreatment and the structure of common psychiatric disorders. British Journal of Psychiatry, 200(2), 107–115. 10.1192/bjp.bp.111.093062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J, & Cicchetti D (2010). Longitudinal pathways linking child maltreatment, emotion regulation, peer relations, and psychopathology. Journal of Child Psychology and Psychiatry and Allied Disciplines, 51(6), 706–716. 10.1111/j.1469-7610.2009.02202.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kingston D, Tough S, & Whitfield H (2012). Prenatal and Postpartum Maternal Psychological Distress and Infant Development: A Systematic Review. Child Psychiatry & Human Development, 43(5), 683–714. 10.1007/s10578-012-0291-4 [DOI] [PubMed] [Google Scholar]
- Lanza ST, Bray BC, & Collins LM (2013). An introduction to latent class and latent transition analysis In Schinka JA, Velicer WF, & Weiner IB (Eds.), Handbook of psychology (2nd ed., pp. 691–716). Hoboken, NJ, USA: WIley. [Google Scholar]
- Laurent HK (2014). Clarifying the contours of emotion regulation: Insights from parent-child stress research. Child Development Perspectives, 8(1), 30–35. 10.1111/cdep.12058 [DOI] [Google Scholar]
- Lieberman A (2004). Child-parent psychotherapy: a relationship-based approach to the treatment of mental health disorders in infancy and early childhood In Sameroff AJ & McDonough SC (Eds.), Treating Parent-Infant Relationship Problems: Strategies for Intervention (pp. 97–122). New York: Guildford Press. [Google Scholar]
- Lovejoy MC, Graczyk PA, O’Hare E, & Neuman G (2000). Maternal depression and parenting behavior. Clinical Psychology Review, 20(5), 561–592. 10.1016/S0272-7358(98)00100-7 [DOI] [PubMed] [Google Scholar]
- Madigan S, Cyr C, Eirich R, Fearon RMP, Ly A, Rash C, … Alink LRA (2019). Testing the cycle of maltreatment hypothesis: Meta-analytic evidence of the intergenerational transmission of child maltreatment. Development and Psychopathology, 31(1), 23–51. 10.1017/s0954579418001700 [DOI] [PubMed] [Google Scholar]
- Masten AS, & Cicchetti D (2010). Developmental cascades. Development and Psychopathology, 22(03), 491–495. 10.1017/S0954579410000222 [DOI] [PubMed] [Google Scholar]
- Moehler E, Biringen Z, & Poustka L (2007). Emotional Availability in a Sample of Mothers With a History of Abuse. American Journal of Orthopsychiatry, 77(4), 624–628. 10.1037/0002-9432.77.4.624 [DOI] [PubMed] [Google Scholar]
- Morgan JK, Ambrosia M, Forbes EE, Cyranowski JM, Amole MC, Silk JS, … Swartz HA (2015). Maternal response to child affect: Role of maternal depression and relationship quality. Journal of Affective Disorders, 187, 106–113. 10.1016/j.jad.2015.07.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray L, Arteche A, Fearon P, Halligan S, Goodyer I, & Cooper P (2011). Maternal postnatal depression and the development of depression in offspring Up to 16 years of age. Journal of the American Academy of Child and Adolescent Psychiatry, 50(5), 460–470. 10.1016/j.jaac.2011.02.001 [DOI] [PubMed] [Google Scholar]
- Muthen LK, & Muthén BO (2012). Mplus User’s Guide. Seventh Edition Los Angeles, CA: Muthen & Muthen. [Google Scholar]
- Ordway M (2011). Depressed Mothers as Informants on Child Behavior: Methodological Issues. Research In Nursing Health, 4(164), 520–532. 10.1002/nur.20463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons CE, Young KS, Rochat TJ, Kringelbach ML, & Stein A (2012). Postnatal depression and its effects on child development: A review of evidence from low- and middle-income countries. British Medical Bulletin, 101(1), 57–79. 10.1093/bmb/ldr047 [DOI] [PubMed] [Google Scholar]
- Pears KC, & Capaldi DM (2001). Intergenerational transmission of abuse: A two-generational prospective study of an at-risk sample. Child Abuse and Neglect, 25(11), 1439–1461. 10.1016/S0145-2134(01)00286-1 [DOI] [PubMed] [Google Scholar]
- Pears KC, Kim HK, & Fisher PA (2008). Psychosocial and cognitive functioning of children with specific profiles of maltreatment. Child Abuse and Neglect, 32(10), 958–971. 10.1016/j.chiabu.2007.12.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rydell AM, Berlin LJ, & Bohlin G (2003). Emotionality, Emotion Regulation, and Adaptation among 5- to 8-Year-Old Children. Emotion, 3(1), 30–47. 10.1037/1528-3542.3.1.30 [DOI] [PubMed] [Google Scholar]
- Sheppes G, Suri G, & Gross JJ (2015). Emotion Regulation and Psychopathology. Annual Review of Clinical Psychology, 11(1), 379–405. 10.1146/annurev-clinpsy-032814-112739 [DOI] [PubMed] [Google Scholar]
- Shields A, & Cicchetti D (1997). Emotion regulation among school-age children: The development and validation of a new criterion Q-sort scale. Developmental Psychology, 33(6), 906–916. 10.1037/0012-1649.33.6.906 [DOI] [PubMed] [Google Scholar]
- Shields A, & Cicchetti D (1998). Reactive aggression among maltreated children: the contributions of attention and emotion dysregulation. Journal of Clinical Child Psychology, 27(4), 381–395. 10.1207/s15374424jccp2704_2 [DOI] [PubMed] [Google Scholar]
- Shields A, & Cicchetti D (2001). Parental maltreatment and emotion dysregulation as risk factors for bullying and victimization in middle childhood. Journal of Clinical Child Psychology, 30(3), 349–363. 10.1097/00004703-200202000-00019 [DOI] [PubMed] [Google Scholar]
- Shields A, Ryan RM, & Cicchetti D (2001). Narrative Representation of Caregivers and Emotion Dysregulation as Predictors of Maltreated Children’s Rejection by Peer. Developmental Psychology, 37(3), 321–337. [DOI] [PubMed] [Google Scholar]
- Smith AL, Cross D, Winkler J, Jovanovic T, & Bradley B (2014). Emotional Dysregulation and Negative Affect Mediate the Relationship Between Maternal History of Child Maltreatment and Maternal Child Abuse Potential. Journal of Family Violence, 29(5), 483–494. 10.1007/s10896-014-9606-5 [DOI] [Google Scholar]
- Sroufe LA, & Waters E (1977). Attachment as an Organizational Construct. Child Development, 48(4), 1184–1199. [Google Scholar]
- Stronach EP, Toth SL, Rogosch FA, Oshri A, Manly JT, & Cicchetti D (2011). Child maltreatment, attachment security, and internal representations of mother and mother-child relationships. Child Maltreatment, 16(2), 137–145. 10.1177/1077559511398294 [DOI] [PubMed] [Google Scholar]
- Teti DM, Gelfand DM, Messinger DS, & Isabella R (1995). Maternal depression and the quality of early attachment: An examination of infants, preschoolers, and their mothers. Developmental Psychology, 31(3), 364–376. 10.1037/0012-1649.31.3.364 [DOI] [Google Scholar]
- Thompson RA, Lewis MD, & Calkins SD (2008). Reassessing emotion regulation. Child Development Perspectives, 2(3), 124–131. 10.1111/j.1750-8606.2008.00054.x [DOI] [Google Scholar]
- Thornberry TP, & Henry KL (2013). Intergenerational Continuity in Maltreatment. Journal of Abnormal Child Psychology, 41(4), 555–569. 10.1007/s10802-012-9697-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villodas MT, Litrownik AJ, Thompson R, Roesch SC, English DJ, Dubowitz H, … Runyan DK (2012). Changes in youth’s experiences of child maltreatment across developmental periods in the LONGSCAN consortium. Psychology of Violence, 2(4), 325–338. 10.1037/a0029829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warmingham JM, Handley ED, Rogosch FA, Manly JT, & Cicchetti D (2019). Identifying maltreatment subgroups with patterns of maltreatment subtype and chronicity: A latent class analysis approach. Child Abuse and Neglect. 10.1016/j.chiabu.2018.08.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widom CS, Czaja SJ, & DuMont KA (2015). Intergenerational transmission of child abuse and neglect: Real or detection bias? Science, 347(6229), 1480–1485. 10.1126/science.1259917 [DOI] [PMC free article] [PubMed] [Google Scholar]