Abstract
Aims. –
In Mexico City, the mortality rate among patients with diabetes appears to be four times that of people without diabetes. Our study aimed to refine analyses of the impact of diabetes on mortality in a large cohort of women from different areas in Mexico with healthcare insurance.
Methods. –
Our study followed 111,299 women with comprehensive healthcare coverage from the Mexican Teachers’ Cohort. After a median follow-up of 7.8 years, 5514 (5%) prevalent self-reported diabetes cases and 4023 incident cases were identified, while deaths were identified through employers’ databases and next-of-kin reports, with dates and causes of death for 1121 women obtained from mortality databases. Hazard ratios (HRs) for total and cause-specific mortality were estimated by Cox regression models, using follow-up time as the time scale and allowing for time-variable diabetes status after adjusting for age, socioeconomic status, use of health services, and anthropometric and lifestyle variables.
Results. –
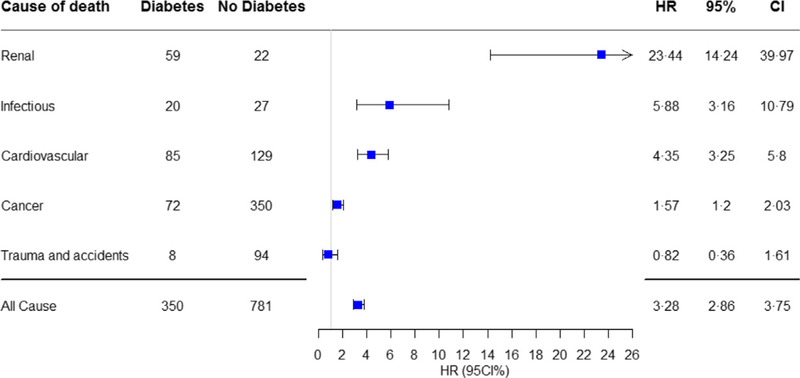
In multivariable-adjusted models, the HR for all-cause mortality was 3.28 (95% CI: 2.86–3.75) in women with vs without diabetes. The impact of diabetes on mortality was higher in rural vs urban areas (HR: 4.72 vs 2.98, respectively). HRs were 1.57 and 23.44 for cancer and renal disease mortality, respectively.
Conclusion. –
In women with healthcare coverage in Mexico, the magnitude of the association between diabetes and all-cause mortality was higher than that observed in high-income countries, but less than what has previously been reported for Mexico. Such elevated mortality suggests a lack of adequate access to quality diabetes care in the population despite comprehensive healthcare coverage.
Keywords: Diabetes, Mexico, Mortality, Public health
INTRODUCTION
Elevated blood glucose is the third most important risk factor for premature death in the world behind hypertension and smoking [1]. Global prevalence of diabetes has more than doubled in the last three decades, and this increment has been more pronounced in low- and middle-income countries (LMICs) [1, 2]. In high-income countries (HICs), patients with diabetes have twice the risk of dying compared with those without diabetes [3]. However, there is little information on the association between diabetes and mortality in LMICs. Emerging evidence from Mexico City has revealed a fourfold higher mortality rate in people with diabetes than in those with normal glucose tolerance [4] whereas, in China, a rural–urban disparity on the impact of diabetes on mortality has been observed, suggesting variable access to healthcare [5].
In Mexico, previously conducted analyses have been important contributors to our knowledge of the causes of mortality in people with diabetes. However, these analyses may have been limited, as some common determinants of diabetes and mortality were not considered, the study location was limited to only two districts in Mexico City and the nationwide universal healthcare programme for those with no social security had not yet been implemented [6]. All of these elements could explain in part the unexpectedly high mortality rate observed among patients with diabetes.
Thus, to further refine our understanding of the impact of diabetes on mortality in Mexico, a large cohort study was initiated and included women with comprehensive healthcare insurance from geographically diverse regions in Mexico comprising both rural and urban areas. In this cohort, diabetes status was updated after taking consideration of baseline status and several risk factors for mortality, including lifestyle factors and use of preventative services, and use of a validated method for identifying diabetes-related deaths.
RESEARCH DESIGN AND METHODS
Study population
The Mexican Teachers’ Cohort (MTC) study was established between 2006 and 2008 when 115,314 female teachers in 12 culturally, geographically and economically diverse states in Mexico responded to a baseline questionnaire on lifestyle and health [7]. During the feasibility phase in 2006, 27,979 women were recruited from two states; in 2008, information on 19,130 women was updated and the study expanded to include 87,335 women from 10 other states. Participants were recruited through a voluntary economically incentivized government programme in which 79% of Mexican public-education teachers were participating at the time of study enrolment. The overall participation rate was 64% (range: 42% to 89% across states). All cohort participants had healthcare coverage at the time of recruitment [79% by the Mexican Institute for Social Security and Services for State Employees (ISSSTE), 11% by the Mexican Institute for Social Security (IMSS) and 10% by other state-level public institutions] that included access to prescription medication for diabetes and treatment for all of its complications at no cost to the patient. This information was updated through a follow-up questionnaire distributed between 2011 and 2013 with an 83% response.
For the present analysis, all participants who reported having a chronic disease at the time of recruitment that could affect the frequency with which they used health services [cancer, stroke, myocardial infarction, cirrhosis (n = 4015)] were excluded. Thus, the present analysis included 111,299 women, and was approved by the research, ethics and biosecurity commissions of the Mexican National Institute of Public Health.
Assessment of diabetes
Prevalent diabetes was determined at baseline based on the following question: ‘Has a physician ever diagnosed you with one of the following diseases?’ This was followed by a list of chronic conditions including ‘diabetes or elevated blood sugar (excluding gestational diabetes)’ as well as year of diagnosis, and whether or not the participant was currently undergoing treatment. Women were considered to have diabetes if they provided a positive answer to at least one of the three diabetes-related questions (its diagnosis, treatment and year of diagnosis). The validity of our definition of diabetes had previously been assessed in a subsample of 3265 participants who responded to a supplementary diabetes questionnaire that included detailed information on its diagnosis, treatment and complications. The positive predictive value of the definition of diabetes used in our analysis was high (89%) [8], similar to an observation made in a well-established US cohort [9].
For all participants not classified as diabetic at baseline, information on incident diabetes was obtained through two sources: follow-up questionnaires and death certificates. Follow-up questionnaires included the same questions pertaining to diabetes diagnosis as the baseline questionnaire, and all participants who answered affirmatively to at least one of the three diabetes-related questions in this questionnaire, but not in the baseline one, were classified as incident cases. Participants not previously identified as diabetes cases, but who had a diagnosis of diabetes on their death certificates, were also considered incident cases.
Mortality follow-up and causes
Deaths were identified through yearly updated employer information, pension-fund management databases [ISSSTE, IMSS, El Seguro del Maestro (teachers’ insurance)] and next-of-kin reports. All deaths were cross-linked with two national death registries [Ministry of Health Epidemiological and Death Statistics System (SEED); National Institute of Statistics, Geography and Informatics (INEGI)] from 1 January 2006 through to 31 December 2016 [10, 11]. In addition, all participants for whom no information was available after baseline or who had retired according to their employer were also cross-linked, as yearly death reports for this group were not as readily available. These cross-linkages were performed using a probabilistic record linkage programme accommodating Hispanic names (Registry Plus Link Plus version 2.0 software, CDC, Atlanta, GA, USA). Variables used for linkage were first and last names, gender and national identification number (the latter available for 70% of participants). Previous assessment of the validity of these death registries for identifying deaths found a sensitivity of 87.9% [95% confidence interval (CI): 85.3–90.6] and specificity of 99.1% (95% CI: 97.9–99.7) [12].
For all deaths in our cohort, the data obtained from both registries, when available, included date of death, and underlying and contributory causes of death. The latter was based on the International Classification of Diseases, 10th Revision (ICD-10), coding system: underlying causes of death are classified as infectious (A00–B99, J00–J22), neoplastic (C00–D49), cardiovascular (I00–I99), renal (N00–N39), and trauma and accidents (S00–T88, V00–Y99). However, the two Mexican national registries differ in their data entry and death coding procedures: in SEED, adjudication of the underlying cause of death is by standardized coders, while INEGI uses an automated algorithm. In fact, the underlying cause of death differed between these registries for only 93 (8%) of all deaths, and the cause of death was adjudicated by consensus between two clinicians who reviewed the contributing causes of death information on death certificates. To ensure that diabetes as a cause of death included only acute diabetes complications, all cases in which the underlying cause of death was diabetes (n = 155, 13% of all deaths) were also reviewed by a clinician. In the absence of acute diabetes complications, deaths were reclassified (n = 122, 78% of diabetes deaths) based on information provided by death certificates.
Other variables
Women who at baseline worked at a school located in a community with a population of < 2500 people were considered rural [13], and those who reported speaking an indigenous language, or having a parent who did so, were considered indigenous [14]. Various proxy variables for socioeconomic status were also implemented: overcrowding index (persons per room in a dwelling); household assets (telephone, car, computer, vacuum cleaner, microwave oven, mobile and Internet access); indigenous language (parental or self); occupation of household head in childhood; and frequency of meat consumption during childhood. Using factor analysis, it was decided to use a simple socioeconomic status score, given its practicality and because the percentage of variance could be explained by the above-listed seven household assets. Scores were created by adding a point for ownership of each asset, and dividing the population into tertiles (low, medium, high) based on these scores. In addition, given the current healthcare panoply whereby Mexicans can be the beneficiaries of multiple healthcare institutions or pay out of pocket through private insurance, it was decided to consider self-reported healthcare provider use as usual medical care at the time of recruitment (ISSSTE, IMSS, private, other public provider). As a marker of healthcare use, all participants were asked to specify the use of two preventative healthcare services: cervical cytology within the last 5 years; and mammography within the last 2 years. Hypertension was defined as self-reported physician-diagnosed elevated blood pressure under medical treatment. Previously, self-reported treated hypertension in this cohort had been shown to adequately identify 89% of women with hypertension [15]. In addition, participants were classified as never, current or past smokers according to self-reports at baseline, while self-reported height and weight were used to calculate body mass index (BMI), defined as weight (kg) divided by square of height (m2). In this cohort, self-reported height and weight were highly correlated with measured values (r = 0.84 for height, r = 0.93 for weight) [16]. Also assessed were participants’ habitual weekly hours spent doing mild, moderate and vigorous recreational physical activity, using eight response categories for each type of activity (ranging from 0 to > 10 h/week), with estimated total recreational physical activity metabolic equivalents of task (METs) per week calculated by multiplying the usual time (in h) spent doing each activity type by the standardized METs for mild (2.2), moderate (4.7) and vigorous (6.0) physical activity [17]. A supplementary diabetes questionnaire was given to a subgroup of participants who reported diabetes at baseline: respondents confirmed their diagnosis and provided additional information, including age at diagnosis, diagnostic procedures, complications (ketoacidosis, retinopathy, diabetic foot, amputation, myocardial infarction, proteinuria, kidney disease, dialysis, kidney transplantation) and treatment (diet, exercise, use of oral hypoglycaemic agents or insulin).
Statistical analysis
Baseline questionnaires (from either 2006 or 2008) were used to identify prevalent cases of diabetes and follow-up questionnaires (2008 and 2011) for incident cases, plus information from death certificates. Time of diagnosis for incident diabetes cases was defined as the reported date on questionnaires (or date of death for diabetes cases identified through death certificates). When the date of diagnosis was not available, the midpoint between date of completion of the last questionnaire free of disease and date of completion of the questionnaire where diabetes was reported was used. Person-time was calculated from date of completion of baseline questionnaire to date of death or 31 December 2016, whichever happened first.
Potential differences in participants’ characteristics were explored through chi-squared tests and one-way analysis of variance (ANOVA) of age at diagnosis, complications and treatments across medical care providers, using information from 3265 patients with diabetes who confirmed the diagnosis and who completed the diabetes supplementary questionnaire. Hazard ratios (HRs) and 95% CIs for total and cause-specific mortality rates were estimated by Cox regression models, using time in the study as the time scale and allowing for time-variable diabetes status, and SAS version 9.3 software (SAS Institute, Cary, NC, USA). Multivariable models were adjusted for age (continuous), rural residence, indigenous ethnicity, socioeconomic status (low, medium, high), usual medical care provider (ISSSTE, IMSS, private, other), use of preventative healthcare services (none, mammography, cervical cytology, mammography and cervical cytology), hypertension, BMI (< 25, 25–27.5, > 27.5–30, > 30–35, > 35 kg/m2, no data), hours of recreational physical activity (tertiles, no data) and smoker status (current, past, never).
To evaluate the impact of duration of disease, an analysis was conducted wherein diabetes cases were restricted to women who reported being diagnosed ≥ 10 years ago, 6–9 years ago or < 6 years ago. Using stratified analyses, it was possible to explore whether associations differed according to age (< 45 years, ≥ 45 years), rural residence, indigenous ethnicity and usual healthcare provider. Heterogeneity of estimates was also evaluated by including a cross-product term for diabetes, two categories for age, rural residence and indigenous ethnicity, and four categories for usual medical care provider. To evaluate HRs in Cox models, models with and without the interaction term were compared using a log-likelihood test. Sensitivity of results was evaluated by using a stricter definition of self-reported diabetes that required positive answers to all three diabetes-related questions (diagnosis, treatment, date of diagnosis). Analyses were repeated including only prevalent diabetes cases at baseline with no updating of diabetes status and including women who reported cancer, stroke, myocardial infarction or cirrhosis at baseline. Finally, an analysis excluding incident cases found through death certificates was performed, as these participants may not have been aware of their disease and, thus, had never sought medical care for it.
RESULTS
In our present cohort, mean baseline age was 42.9 years and mean age at diabetes diagnosis was 46.4 years; the prevalence of self-reported diabetes at baseline was 5% (n = 5514) and increased with age. In women aged > 65 years, diabetes prevalence was 17.5% (Fig. S1; see supplementary material associated with this article online). A total of 4082 incident cases of diabetes (incidence rate: 4.8 per 1000 person-years) was identified: 4023 (99%) by follow-up questionnaires; and 59 (1%) by death certificates. Age-adjusted characteristics of participants according to diabetes diagnosis are shown in Table I. On average, women with diabetes were older, of lower socioeconomic status and used private health services less frequently, and more frequently had hypertension, obesity and were smokers, than women without diabetes. Less time (in h) also appeared to be spent on recreational physical activity in women with than without diabetes.
Table 1.
Age-adjusted baseline characteristics of women with and without prevalent and incident diabetes.
| Diabetes (n = 9596) |
No diabetes (n =101,703) |
|
|---|---|---|
| Mean age (± SD), years | 46.6 (6.7) | 42.6 (7.5) |
| Rural | 25.2 | 24.7 |
| Indigenous | 9.8 | 8.1 |
| High socioeconomic status | 34.4 | 38.7 |
| Usual medical care provider | ||
| ISSSTE | 58.7 | 54.4 |
| IMSS | 11.9 | 9.6 |
| Private | 15.7 | 21.6 |
| Other | 13.7 | 14.4 |
| Use of preventative care servicesa | ||
| No cancer screening | 25.9 | 24.5 |
| Mammography or cervical cytology | 49.1 | 50.8 |
| Mammography and cervical cytology | 25.0 | 24.7 |
| Hypertension | 9.6 | 3.0 |
| Smoker | ||
| Current | 9.8 | 9.0 |
| Past | 17.3 | 13.4 |
| Never | 72.9 | 77.6 |
| Mean body mass index (± SD), kg/m2 | 29.8 (5.1) | 27.0 (4.5) |
| Body mass index, kg/m2 | ||
| < 25 | 15.4 | 33.1 |
| 25–27.5 | 17.7 | 21.6 |
| > 27.5–30 | 18.6 | 16.1 |
| > 30–35 | 25.1 | 14.8 |
| > | 13.6 | 5.1 |
| No data | 9.5 | 9.4 |
| Mean physical activity (± SD), METs/week | 12.6 (16.5) | 14.9 (18.2) |
Data are percentages (%) unless otherwise specified.
ISSSTE: Institute for Social Security and Services for State Employees; IMSS: Mexican Institute for Social Security; METs: metabolic equivalents of task.
Mammography in last 2 years, cervical cytology in last 5 years.
After a median follow-up time of 7.8 years (849,319 person-years), 1121 deaths (340 women with and 781 women without diabetes) were identified. Age at death did not differ among participants [mean ± standard deviation (SD) 52.9 ± 6.5 years with vs 51.1 ± 7.8 years without diabetes]. Age-adjusted mortality in women with diabetes was 4.59 per 1000 person-years whereas the corresponding rate in those without diabetes was 1.09 per 1000 person-years. The age-adjusted HR for diabetes was 3.52 (95% CI: 3.09–4.01). After multivariable adjustments, it was found that mortality rates were three times higher in women with than without diabetes (Table II), and the risk increased with longer diabetes duration: HR for incident cases was 1.12, whereas the estimate for prevalent diabetes cases of > 10 years’ duration was 5.81.
Table 2.
Multivariable hazard ratios (HR) and 95% confidence intervals (95% CI) for mortality in women with vs. without diabetesa.
| Deaths (n) |
Person-years (n) |
HR | 95% CI | P for interaction | |||
|---|---|---|---|---|---|---|---|
| Diabetes | No diabetes | Diabetes | No diabetes | ||||
| All | 340 | 781 | 69,531 | 779,788 | 3.28 | 2.86–3.75 | |
| Prevalent diabetesb | 236 | 885 | 41,973 | 807,371 | 3.21 | 2.76–3.73 | |
| ≥ 10 years’ duration | 72 | 1049 | 5131 | 844,213 | 5.81 | 4.51–7.37 | |
| 6–9 years’ duration | 53 | 1068 | 7100 | 842,244 | 3.49 | 2.60–4.55 | |
| < 6 years’ duration | 85 | 1036 | 25,814 | 823,530 | 1.74 | 1.38–2.16 | |
| Incident diabetes | 104 | 1017 | 31,493 | 817,851 | 1.12 | 1.09–1.15 | |
| Age (years) | |||||||
| < 45 | 68 | 266 | 27,674 | 469,947 | 3.35 | 2.52–4.41 | 0.62 |
| ≥ 45 | 272 | 515 | 41,857 | 309,841 | 3.25 | 2.78–3.78 | |
| Residence | |||||||
| Rural | 79 | 142 | 15,925 | 191,036 | 4.72 | 3.51–6.30 | 0.01 |
| Urban | 261 | 639 | 53,606 | 588,752 | 2.98 | 2.56–3.47 | |
| Ethnicity | |||||||
| Indigenous | 25 | 51 | 6238 | 62,903 | 3.64 | 2.20–5.90 | 0.71 |
| Non-indigenous | 315 | 730 | 63,293 | 716,885 | 3.26 | 2.83–3.74 | |
| Usual medical care | |||||||
| ISSSTE | 218 | 460 | 40,617 | 421,522 | 3.53 | 2.98–4.17 | 0.35 |
| IMSS | 40 | 96 | 8940 | 84,394 | 2.59 | 1.74–3.80 | |
| Private | 39 | 126 | 10,734 | 167,237 | 3.13 | 2.12–4.51 | |
| Other | 43 | 99 | 9233 | 106,644 | 3.11 | 2.11–4.52 | |
Models adjusted for age (continuous), rural residence, indigenous ethnicity, socioeconomic status (low, medium, high), usual medical care provider [Institute for Social Security and Services for State Employees (ISSSTE), Mexican Institute for Social Security (IMSS), private, other], use of preventative care services (none, mammography, cervical cytology, mammography and cervical cytology), hypertension, body mass index (<25, 25–27.5,> 27.5–30,> 30–35, > 35kg/m2, no data), hours of recreational physical activity (tertiles, no data) and smoking status (current, past, never).
Including only those responding since diagnosis.
The prevalence and incidence of diabetes were slightly higher in urban vs rural areas (5.1% vs 4.4% and 4.8 vs 4.5 per 1000 person-years, respectively). However, the mortality rate associated with diabetes was significantly higher in women living in rural vs urban areas. The relationship between diabetes and mortality did not differ according to age, indigenous ethnicity or usual medical care providers, although diabetes appeared to have less of an impact on mortality in women who received their usual medical care from the IMSS compared with other healthcare providers. Yet, in the subgroup of 3265 diabetic women with supplementary information, age at diagnosis and treatment did not differ across healthcare providers (Table SI; see supplementary material associated with this article online), whereas the proportion of women with diabetes complications did (P = 0.002). Women receiving care from private providers had lower rates of complications, whereas those using healthcare provided by ISSSTE had the highest percentages.
In our present cohort, the primary cause of death was cancer (n = 422; 37.6% of all deaths), with the most common sites being the breast (n = 73), ovary (n = 37), colorectum (n = 29), stomach (n = 27) and liver (n = 26); 72 cancer deaths were in women with diabetes, whereas 350 were in women without diabetes. The cancer mortality rate in diabetic women was 57% higher compared with women without diabetes (HR: 1.57, 95% CI: 1.20–2.03), and death due to renal disease was 23 times higher in women with than without diabetes (HR: 23.44, 95% CI: 14.24–39.97; Fig. 1). There were also associations observed with deaths due to cardiovascular disease and infections.
Fig. 1.
Hazard ratios (HRs) and 95% confidence intervals (95CI%) for cause-specific mortality in women with and without diabetes. All models were adjusted for age (continuous), rural residence, indigenous ethnicity, socioeconomic status (low, medium, high), usual medical care provider [Institute for Social Security and Services for State Employees (ISSSTE), Mexican Institute for Social Security (IMSS), private, other], use of preventative care services (none, mammography, cervical cytology, mammography and cervical cytology), hypertension, body mass index (< 25, 25–27.5, > 27.5–30, > 30–35, > 35 kg/m2, no data), hours of recreational physical activity (tertiles, no data) and smoking status (current, past, never).
On sensitivity analyses, HRs did not change appreciably (Table SII; see supplementary material associated with this article online) when the definition of diabetes required positive responses to all three diabetes-related questions (diagnosis, treatment, year of diagnosis) and the analyses were restricted to only prevalent cases or included participants excluded at baseline due to cancer, stroke, myocardial infarction or cirrhosis. In fact, it was found that the HR was somewhat lower when incident cases of diabetes identified through death certificates were excluded.
DISCUSSION
In this large prospective study of women in Mexico with comprehensive healthcare insurance whose diabetes status was updated after baseline, diabetes was associated with a threefold higher all-cause mortality than in those without the disorder. In addition, the impact of diabetes on mortality was higher in women living in rural vs urban areas and also increased with duration of the disease. Adjusted HRs showed that diabetes increased the risk of death due to cancer, cardiovascular disease and infections, although by far the greatest increase was associated with renal disease.
In Sweden, mortality is only 15% higher in patients with diabetes and, on average in HICs, two times higher than in those without the disorder [3, 18]. However, only two prospective studies have evaluated the impact of diabetes on mortality in a middle-income country. The threefold increase observed in the present study is similar to what was reported in a previous study in Mexico City of subjects diagnosed with diabetes and HbA1c levels < 9% (75 mmol/mol; HR: 3.0, 95% CI: 2.8–3.3) [19]. As with that report from Mexico City, longer duration of diabetes was also associated with greater mortality. On the other hand, unlike previous analyses, the present study was able to evaluate whether the association between diabetes and mortality differed in rural vs urban areas, with results consistent with a previous analysis from China [20]. Indeed, in both Mexico and China, although diabetes was more frequently observed in urban areas, the association with mortality was stronger in rural settings, and such an urban–rural disparity was present even in a population with comprehensive healthcare coverage. Also, the strongest association was with renal disease mortality (increased 23 times by diabetes).
In addition, in contrast to those two previous analyses, our study found a relatively strong association with cancer mortality, which was nearly 60% higher in women with than without diabetes. In fact, diabetes has previously been associated with an increased risk of breast, bladder, liver, pancreatic and colorectal cancers [21]. Yet, even though diabetes and cancer may share risk factors, our adjusted analysis also appears to support a direct impact of hyperinsulinaemia, hyperglycaemia and inflammation on cancer mortality [22]. Moreover, some but not all studies have suggested that Hispanics may be at higher risk for diabetes complications [23–25]. Nevertheless, inadequate diabetes management and limited access to quality care for diabetes complications may be driving the marked increased in mortality in women with diabetes in Mexico. A nationwide survey conducted in 2012 revealed that 75% of Mexicans with diabetes had inadequately controlled levels of HbA1c and, of the 25% of diagnosed cases without access to care, most were living in rural areas [26]. Also, despite the fact that 63% of patients with diabetes reported keeping regular medical appointments, very few reported undergoing screening for early detection of complications (such as microalbumin tests) during those visits. Age at the time of death did not differ between women with and without diabetes, most likely because a large proportion of deaths in those without diabetes were due to accidents and aggressive forms of cancer, causing a large proportion to die at a younger age compared with diabetic women. Finally, despite some limitations in evaluating the impact of diabetes on mortality according to healthcare provider, this hypothesis was nonetheless explored and revealed that there may be some heterogeneity across providers in impact of diabetes on mortality and prevalence of complications.
The capacity to update diabetes status from baseline and to assess several mortality risk factors as well as healthcare providers, a sample population of women from different regions in Mexico and a validated method of identifying deaths in Mexico are all important strengths of the present study. However, the following limitations should also be considered.
First, some participants may have been unaware of their disease and therefore wrongly classified as disease-free and, conversely, some women may have reported having diabetes without a formal physician’s diagnosis. However, such misclassification would most likely have no effect on mortality or, if any, would bias results towards no association. Also, our previously validated definition of diabetes using a detailed supplementary questionnaire plus several sensitivity analyses using different definitions of diabetes did not appreciably change our results.
Second, our cause-specific mortality relied on information from death certificates and, although mortality records in Mexico are considered high in quality [27], the possibility that the designation of an underlying cause of death may have been influenced by a previous diagnosis of diabetes cannot be ruled out.
Third, as with any observational study, some residual confounding by measured and unmeasured factors remains a possibility, although our models were adjusted for several socioeconomic and behavioural risk factors for mortality associated with diabetes and led to only modest changes in the magnitude of the association. Also, even though dietary behaviours may be an important determinant of diabetes and death, no adjustment was made for diet because women with a diabetes diagnosis may well have changed their dietary habits.
Fourth, our present results may only be generalizable to educated and employed women who have comprehensive healthcare insurance. Nevertheless, even though our analysis may only represent the diabetes burden in a fraction of the general population, our results underscore the importance of boosting diabetes care both locally and globally. Indeed, in a middle-income country and despite a population with healthcare insurance and higher socioeconomic status, diabetes still exerts a marked influence on mortality.
Fifth, while it was not possible to stratify our results by diabetes type (1 or 2), it is likely that the proportion of patients with type 1 diabetes was small in our cohort [28, 29].
Finally, the causal effect of diabetes on mortality can be difficult to define, as diabetes may result from various risk factors (such as diet and amount of physical activity) and differences in the distribution of these risk factors may affect its impact on mortality. For this reason, calculation of a population excess fraction was considered inappropriate for our study.
In conclusion, diabetes has an impact on mortality in Mexico that far exceeds what has been observed in HICs and even among people who enjoy comprehensive healthcare. Thus, in such settings and in the face of increasing diabetes prevalence, population-wide diabetes prevention policies (such as taxes on sweetened soft drinks) as well as guarantees of adequate access to quality diabetes care are urgent public-health priorities. Moreover, healthcare providers need to boost and constantly monitor their diabetes programmes to ensure their efficacy and positive impact on health outcomes.
Supplementary Material
Fig. S1. Prevalence of diabetes by age in women in the Mexican Teachers’ Cohort (MTC) study.
ACKNOWLEDGEMENTS
The authors would like to thank all participants for their time and involvement in the study, and the ISSSTE for its continuing support.
FUNDING/FINANCIAL SUPPORT
This research received no specific grant from any funding agency in the public, commercial or non-profit sectors.
ABBREVIATIONS
- LMICs
low-and-middle income countries
- HICs
high-income countries
- MTC
Mexican Teachers’ Cohort
- ISSSTE
Institute for Social Security and Services for State Employees
- IMSS
Mexican Institute for Social Security
- SEED
Epidemiological and Death Statistics System
- INEGI
National Institute of Statistics, Geography and Informatics
- ICD-10
International Classification of Diseases, 10th Revision
Footnotes
DATA AVAILABLE
Datasets generated during and/or analyzed in the present study are available from the corresponding author upon reasonable request.
Statement of assistance: Nothing to disclose
Guarantor’s name: Martin Lajous
Appendix supplementary material
Supplementary materials (Fig. S1, Tables SI and SII) associated with this article can be found at http://www.scincedirect.com at doi . . .
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Publisher's Disclaimer: This is a PDF file of an article that has undergone enhancements after acceptance, such as the addition of a cover page and metadata, and formatting for readability, but it is not yet the definitive version of record. This version will undergo additional copyediting, typesetting and review before it is published in its final form, but we are providing this version to give early visibility of the article. Please note that, during the production process, errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CONFLICTS OF INTEREST
Dr Lajous and Dr Lopez-Ridaura report grants from the National Cancer Institute, National Council for Science and Technology (CONACYT) Mexico and AstraZeneca Mexico during the conduct of the study. All other authors have nothing to disclose.
REFERENCES
- [1].Collaboration NCD Risk Factor Collaboration. Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet 2016; 387:1513–30. 10.1016/S0140-6736(16)00618-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].WHO. Global Report on Diabetes. World Health Organization, 2016. France. Available from: http://apps.who.int/iris/bitstream/10665/204871/1/9789241565257_eng.pdf [Google Scholar]
- [3].Rao Kondapally Seshasai S, Kaptoge S, Thompson A, Di Angelantonio E, Gao P, Sarwar N et al. Diabetes mellitus, fasting glucose, and risk of cause-specific death. N Engl J Med 2011; 364: 829–41. 10.1056/NEJMoa1008862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Alegre-Diaz J, Herrington W, Lopez-Cervantes M, Gnatiuc L, Ramirez R, Hill M et al. Diabetes and Cause-Specific Mortality in Mexico City. N Engl J Med 2016; 375: 1961–71. 10.1056/NEJMoa1605368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Bragg F, Li L, Chen Z. Urban-Rural Differences in Diabetes-Associated Mortality in China-Reply. JAMA 2017; 317: 1689 10.1001/jama.2017.3350 [DOI] [PubMed] [Google Scholar]
- [6].Arredondo A. Diabetes duration, HbA1c, and cause-specific mortality in Mexico. Lancet Diabetes Endocrinol 2018; 6: 429–31. 10.1016/S2213-8587(18)30098-6 [DOI] [PubMed] [Google Scholar]
- [7].Lajous M, Ortiz-Panozo E, Monge A, Santoyo-Vistrain R, Garcia-Anaya A, Yunes-Diaz E et al. Cohort Profile: The Mexican Teachers’ Cohort (MTC). Int J Epidemiol 2017; 46: e10. 10.1093/ije/dyv123 [DOI] [PubMed] [Google Scholar]
- [8].Stern D, Mazariegos M, Ortiz-Panozo E, Campos H, Malik VS, Lajous M et al. Sugar-Sweetened Soda Consumption Increases Diabetes Risk Among Mexican Women. J Nutr 2019; 149: 795–803. 10.1093/jn/nxy298 [DOI] [PubMed] [Google Scholar]
- [9].Schneider AL, Pankow JS, Heiss G, Selvin E. Validity and reliability of self-reported diabetes in the Atherosclerosis Risk in Communities Study. Am J Epidemiol 2012; 176: 738–43. 10.1093/aje/kws156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].INEGI (2016) Estadística de defunciones generales. Marco metodológico. Instituto Nacional de Estadística y Geografía. Mexico. Available from http://www.beta.inegi.org.mx/app/biblioteca/ficha.html?upc=702825086114.
- [11].DGAE (2012) Manual de Procedimientos Estandarizados para el Sistema Estadístico Epidemiológico de las Defunciones (SEED). Mexico. Available from http://www.ssm.gob.mx/portal/page/vig_epid/1/manuales/26%20Manual%20SEED.pdf
- [12].Zazueta OE et al. (2016) Comparing the usefulness of two mortality databases for population health research in Mexico. In: Research Symposium. Global Partnerships to Advance NCD Research within the Agenda of the Sustainable Development Goals. [Google Scholar]
- [13].INEGI (2010) Población rural y urbana. Instituto Nacional de Estadística y Geografía. Mexico.Available from http://cuentame.inegi.org.mx/poblacion/rur_urb.aspx?tema=P2018 [Google Scholar]
- [14].JEVM García López., Herrera Daniel Martínez, Angel Miguel. (2004) Clasificación de localidades de México según grado de presencia indígena, 2000. México. Available from http://www.conapo.gob.mx/es/CONAPO/Clasificacion_de_localidades_de_Mexico_segun_grado_de_presencia_indigena_2000_
- [15].Monge A, Lajous M, Ortiz-Panozo E, Rodriguez BL, Gongora JJ, Lopez-Ridaura R. Western and Modern Mexican dietary patterns are directly associated with incident hypertension in Mexican women: a prospective follow-up study. Nutr J 2018; 17: 21 10.1186/s12937-018-0332-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Ortiz-Panozo E, Yunes-Díaz E, Lajous M, Romieu I, Monge A, López-Ridaura R. Validity of self-reported anthropometry in adult Mexican women. Salud Pública de México 2017; 59: 266–75. [DOI] [PubMed] [Google Scholar]
- [17].Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc 2000; 32(9 Suppl): S498–504. [DOI] [PubMed] [Google Scholar]
- [18].Tancredi M, Rosengren A, Svensson AM, Kosiborod M, Pivodic A, Gudbjörnsdottir S et al. Excess Mortality among Persons with Type 2 Diabetes. N Engl J Med 2015; 373: 1720–32. 10.1056/NEJMoa1504347 [DOI] [PubMed] [Google Scholar]
- [19].Herrington WG, Alegre-Diaz J, Wade R, Gnatiuc L, Ramirez-Reyes R, Hill M et al. Effect of diabetes duration and glycaemic control on 14-year cause-specific mortality in Mexican adults: a blood-based prospective cohort study. Lancet Diabetes Endocrinol 2018; 6: 455–63. 10.1016/S2213-8587(18)30050-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Bragg F, Holmes MV, Iona A, Guo Y, Chen Y, Bian Z et al. Association Between Diabetes and Cause-Specific Mortality in Rural and Urban Areas of China. JAMA 2017; 317: 280–9. 10.1001/jama.2016.19720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Giovannucci E, Harlan DM, Archer MC, Bergenstal RM, Gapsur SM, Habel La et al. Diabetes and cancer: a consensus report. Diabetes Care 2010; 33: 1674–85. 10.2337/dc10-0666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Orgel E, Mittelman SD. The links between insulin resistance, diabetes, and cancer. Curr Diab Rep 2013; 13: 213–22. 10.1007/s11892-012-0356-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Hunt KJ, Gonzalez ME, Lopez R, Haffner SM, Stern MP, Gonzalez-Villalpando C. Diabetes is More Lethal in Mexicans and Mexican-Americans Compared to Non-Hispanic Whites. Ann Epidemiol 2011; 21: 899–906. 10.1016/j.annepidem.2011.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Aguilar-Salinas CA, Reyes-Rodriguez E, Ordonez-Sanchez ML, Torres MA, Ramirez-Jimenez S, Dominguez-Lopez A et al. (2001) Early-onset type 2 diabetes: metabolic and genetic characterization in the Mexican population. J Clin Endocrinol Metab 2001; 86: 220–6. 10.1210/jcem.86.1.7134 [DOI] [PubMed] [Google Scholar]
- [25].Aguilar-Salinas CA, Rojas R, Gomez-Perez FJ, Garcia E, Valles V, Rios-Torres JM et al. Prevalence and characteristics of early-onset type 2 diabetes in Mexico. Am J Med 2002; 113: 569–74. [DOI] [PubMed] [Google Scholar]
- [26].Flores Hernández S. Reyes-Morales H, Villalpando S, Reynoso Noverón N, Hernández Ávila M. Diabetes en adultos: urgente mejorar la atención y el control Enquesta nacional de Salud y nutricion 2012; INSP. [Google Scholar]
- [27].Phillips DE, Lozano R, Naghavi M, Atkinson C, Gonzalez-Medina D, Mikkelsen L et al. A composite metric for assessing data on mortality and causes of death: the vital statistics performance index. Popul Health Metr 2014; 12: 14 10.1186/1478-7954-12-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].American Diabetes Association. (2018) Statistics about Diabetes. Available from http://www.diabetes.org/diabetes-basics/statistics/
- [29].Segovia-Gamboa, Rodriguez-Arellano ME, Munoz-Solis A, Retana-Jimenez JE, Vargas-Ayala G, Granados J et al. High Prevalence of Humoral Autoimmunity in First-Degree Relatives of Mexican Type 1 Diabetes Patients. Acta Diabetol 2018; 55:1275–82. 10.1007/s00592-018-1241-9 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Fig. S1. Prevalence of diabetes by age in women in the Mexican Teachers’ Cohort (MTC) study.