Introduction
Langerhans cell histiocytosis (LCH) is the most common histiocytic neoplasm involving the calvarial bone in children. LCH characteristically shows almost homogeneous signal intensity on gadolinium-enhanced MR imaging.1 However, LCH manifesting as an osteolytic cystic mass with multiple fluid–fluid levels (FFLs) is rare. This unique imaging appearance has rarely been reported.2 Herein, we report a case of solitary LCH in the skull with FFLs.
Case Report
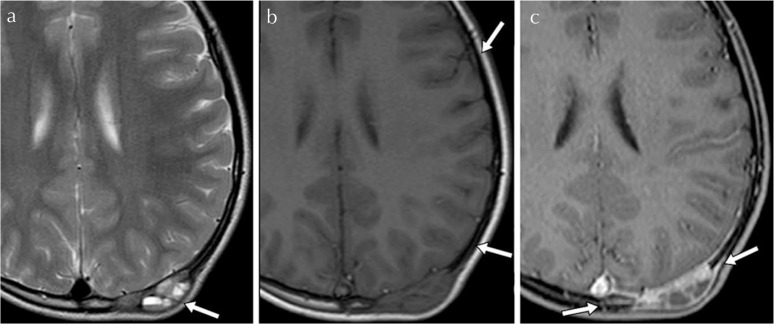
A 10-year-old girl presented with a 3-week history of an occipital mass with persistent swelling and swelling and tenderness for 2 weeks after bruising her head. No other abnormalities were found on clinical examination. Skull radiographs demonstrated a single osteolytic lesion without sclerosis in the left parietal bone. Computed tomography demonstrated a mass that extended beyond the cortex of the inner and outer tables (Fig. 1). A beveled edge appearance was demonstrated due to asymmetrical involvement of the inner and outer tables. T2-weighted images showed multiple FFLs (Fig. 2a), whereas T1-weighted images showed a broad signal intensity change in the adjacent bone marrow (Fig. 2b). Post-contrast T1-weighted images showed enhancement of the solid part of the lesion and adjacent pericranial soft tissue, dura mater, and bone marrow (Fig. 2c).
Fig. 1.
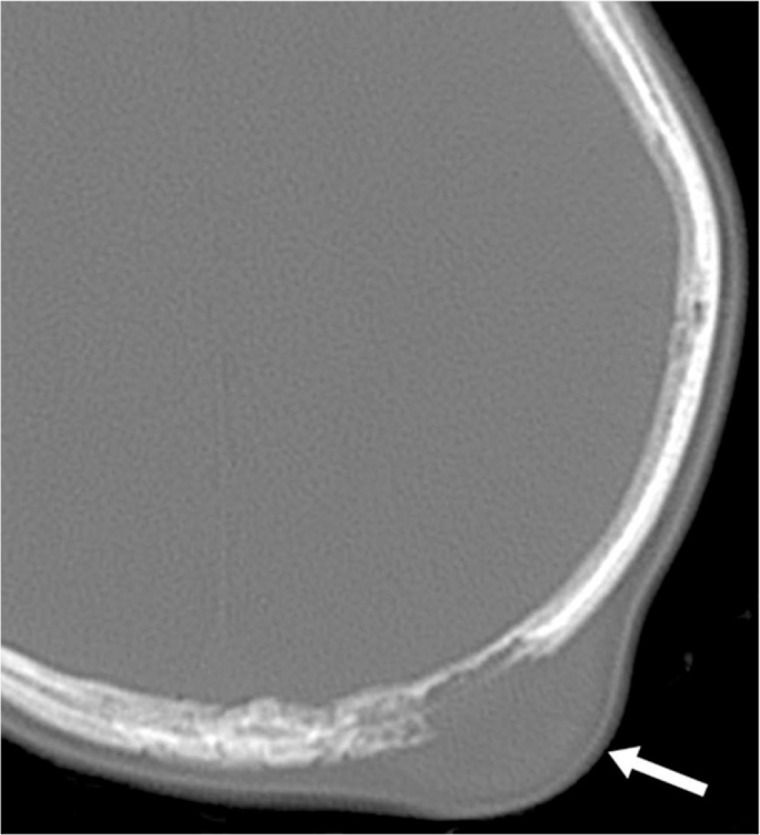
Computed tomography image showing a mass (arrow) extending through and beyond the cortex of the inner and outer tables in the left parietal bone. A beveled edge appearance was demonstrated due to asymmetrical involvement of the inner and outer tables.
Fig. 2.
(a) T2-weighted image showing an expansive osteolytic cystic mass with multiple fluid–fluid levels (arrow). (b) T1-weighted image revealing low signal intensity changes in the adjacent bone marrow (arrows). (c) Post-contrast T1-weighted image showing enhancement of the adjacent pericranial soft tissue, dura mater, and bone marrow as well as of the mass (arrows).
During surgery, an extradural encapsulated cystic mass containing hematoma was found beneath the periosteum. Pathologic examination of hematoxylin–eosin stained sections revealed proliferation of plasma cells, lymphocytes, and histiocytic cells. The histiocytic cells were confirmed to be Langerhans cells by their positive immunohistochemical staining for CD1a, langerin, and S100 protein. Thus, the diagnosis was LCH.
Discussion
Langerhans cell histiocytosis characteristically shows almost homogeneous enhancement on MR imaging,1 whereas in our patient it was manifested as a bony mass lesion containing small cystic portions with FFLs. Nabavizadeh et al. reported 11 pediatric patients with skull masses containing FFLs. The underlying pathology was LCH in four children, aneurysmal bone cysts (ABCs) in three, cephalohematoma in three, and metastatic neuroblastoma in one.2 Though FFLs are famous characteristics of ABCs, the beveled edge appearance in this case cannot be seen in ABCs. These FFLs in LCH represented hemorrhage, which were caused by trauma or developed spontaneously.2 Therefore, the top differential diagnosis for cystic skull lesions with FFLs in children is LCH.
Our patient also showed T1-weighted low-intensity changes in adjacent bone marrow that resolved after resection of the lesion. Stull et al.3 have reported that signal-intensity alterations within surrounding marrow suggest either reactive edema or inflammation. Okamoto et al.4 reported similar changes of calvarial LCH. Thus, these reactive changes on MR imaging may be characteristic of LCH, and unlikely imaging findings for malignant tumors accompanied with FFLs.
We consider awareness of these unique presentations of LCH on MR imaging is important to know.
Acknowledgments
We thank Hiroyuki Tatekawa for reviewing the manuscript and providing useful suggestions and Dr Trish Reynolds, MBBS, FRACP, from Edanz Group (www.edanzediting.com/ac) for editing a draft of this manuscript.
Footnotes
Conflicts of Interest
The authors declare that they have no conflicts of interest.
References
- 1.D’Ambrosio N, Soohoo S, Warshall C, Johnson A, Karimi S. Craniofacial and intracranial manifestations of langerhans cell histiocytosis: report of findings in 100 patients. AJR Am J Roentgenol 2008; 191:589–597. [DOI] [PubMed] [Google Scholar]
- 2.Nabavizadeh SA, Bilaniuk LT, Feygin T, Shekdar KV, Zimmerman RA, Vossough A. CT and MRI of pediatric skull lesions with fluid–fluid levels. AJNR Am J Neuroradiol 2014; 35:604–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stull MA, Kransdorf MJ, Devaney KO. Langerhans cell histiocytosis of bone. Radiographics 1992; 12:801–823. [DOI] [PubMed] [Google Scholar]
- 4.Okamoto K, Ito J, Furusawa T, Sakai K, Tokiguchi S. Imaging of calvarial eosinophil granuloma. Neuroradiology 1999; 41:723–728. [DOI] [PubMed] [Google Scholar]