1. Introduction
Approximately 1 in 40 people aged 50 or over suffer with hallux rigidus, a very common progressive degenerative disease.1 Hallux rigidus is a severe form of arthritis affecting the first metatarsophalangeal joint (1st MTPJ) of the foot. In arthritis joint space is lost, creating increased friction and tension between the opposing metatarsal and proximal phalanx which leads to the formation of dorsal and periarticular osteophytes, loss of articular cartilage and inflammation and destruction of the subchondral bone. In the hallux arthritis first begins as hallux limitus where dorsiflexion is impaired and ultimately as the disease progresses it results in hallux rigidus.2 This causes pain, stiffness and reduced range of motion which, in hallux rigidus, can have a detrimental effect on a person's day to day activities, sporting ability and shoe choice.3 The degenerative and progressive nature of the disease make it a challenge to treat whilst maintaining the functionality and range of motion of the forefoot.
The first metatarsal plays a pivotal role in the mechanics of the foot. During normal gait, as part of the windlass mechanism of the foot, it acts to lift the foot off the ground and tightens the plantar fascia along with the posterior tibialis, maintaining the medial longitudinal arch of the foot.4 Athletes in accelerative, decelerative, twisting and pivoting sports such as football, basketball, American football and athletics rely on the ball of the foot to maintain their agility and speed.5 The metatarsal head can carry upwards of 119% of a person's body weight during the push-off phase.6
Mild symptomatic arthritis of the joint is usually treated by cheilectomy. The current gold standard in treatment of severe arthritis is arthrodesis. Arthrodesis involves fusing the distal metatarsal head and proximal phalanx using screws, plates and/or wires. This procedure boasts excellent patient satisfaction rates as it reduces pain whilst maintaining impressive functional outcomes. On the other hand, it sacrifices the normal biomechanics of the first toe, which can be detrimental to certain athletes and for people who wish to continue wearing high heeled shoes.
Previous hemiarthroplasty procedures utilised silicon-based implants to treat hallux rigidus, however these procedures resulted in poor post-operative outcomes due to material failure and loosening.7 Other implants such as the cobalt surfaced HemiCap,8 and other implants such as ones made of metal8 or ceramic9 also performed worse than arthrodesis. Futhermore, revisions after failure of these implants were difficult to perform due to the amount of bone resected in the primary operation.6
The new Cartiva synthetic cartilage implant (SCI) demonstrated the same biomechanical properties in cadaveric studies as human articular cartilage.10 The Cartiva SCI is a 8 mm or 10 mm polyvinyl alcohol device which can be used to treat hallux rigidus.11 It is able to recreate the joint space between the 1st MTP and the proximal phalanx to reduce pain, increase mobility in dorsiflexion and plantarflexion of the first ray and maintain its functionality. An industry-funded originator series randomised trial “Cartiva Motion Study” compared the patient-recorded outcome measures of Cartiva SCI and arthrodesis surgery for the treatment of advanced hallux rigidus.12 This showed statistically significant pain reduction at 2 years and statistically significant increase in joint mobility in the Cartiva cohort. Follow up of a subsection of the initial Cartiva cohort at 5 years showed similar significant results.13 As of now, there are no independent comparative series for treatment of hallux rigidus utilising polyvinyl alcohol implants and arthrodesis.
The aim of this cohort study is to compare the sporting ability of patients who underwent a Cartiva SCI hemiarthroplasty or an arthrodesis for the treatment of hallux rigidus utilising patient reported outcome measures (PROMs).
2. Methods
Audit approval was obtained from the Wythenshawe Hospital audit department.
Inclusion criteria included adult patients over 18 years of age at a single centre with symptomatic hallux rigidus who underwent primary Cartiva SCI hemiarthroplasty or arthrodesis. Patients with previous surgery to the 1st metatarsal and traumatic osteoarthritis patients were excluded.
First MTPJ arthritis was radiographically graded preoperatively, utilising PACS, according to the Hattrup and Johnson (HJ) classification. First MTPJ arthritis is graded between 1 and 3, where Grade 1 is mild changes to the MTPJ with minimal osteophytosis, Grade 2 are moderate changes to the MTPJ including narrowing of the joint with osteophytosis of the metatarsal head and/or phalanx and subchondral sclerosis and/or cysts, and Grade 3 are severely arthritis MTPJ with loss of joint space, marked osteophytosis and subchondral bone changes.
Post-operative sporting ability was evaluated utilising the patient-reported outcomes were evaluated using the Foot and Ankle Ability Measure Sports14 (FAAM Sports) subscale. Data was collected at minimum 1 year post-surgery. In addition, patients were asked which sports they actively participate in to allow comparison between the sporting demand of both groups.
FAAM Sports consists of 8 questions relating to sporting ability. Each is scored by the patient between “No difficulty” and “Extremely difficult” or “Unable to do”, where “No difficulty” is given a score of 4, “Unable to do” a score of 0 and the remaining answers a score in between. The total score is divided by 32, however, for every question the patient marks as “Unable to do” are not scored in the final tally, and this score is then multiplied by 100 to express as a percentage.
GraphPad Prism15 was utilised to perform a Mann-Whitney U test to identify statistically significant results between the two groups as determined by a p value of <0.05.
3. Results
In total, 42 Arthrodesis and 30 Cartiva patients were included in this study. The Cartiva group consisted of 7 male and 23 female patients with a mean age of 57 (39–80). In this group there were 9 HJ2 and 21 HJ3 patients with no HJ1 patients. The Arthrodesis group consisted of 15 male and 27 female patients with a mean age of 64 (41–77). In this group there were 3 HJ1, 17 HJ2 and 22 HJ3 patients (Table 1).
Table 1.
Patient demographics.
| Surgery | Number of patients | Gender | Average age/years | Average follow up/months | Hattrup and Johnson Grade |
|---|---|---|---|---|---|
| Cartiva | 30 | 7 Male 23 Female |
57 (min 39, max 80) | 18 (min 12, max 30) | HJ 1 = 0 HJ 2 = 9 HJ 3 = 21 |
| Arthrodesis | 42 | 15 Male 27 Female |
64 (min 41, max 77) | 19 (min 14, max 36) | HJ 1 = 3 HJ 2 = 17 HJ 3 = 22 |
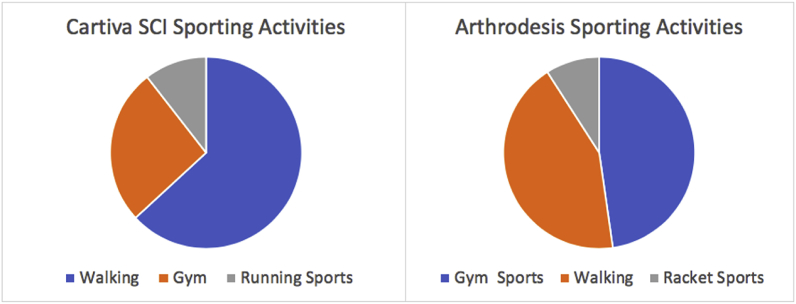
There were four main activity profiles both cohorts participated in, Walking, Gym sports (gym, swimming, yoga, zumba, aerobics, bowling and cycling), Racket sports (tennis, badminton and golf) and Running sports (running and football). In the Cartiva group the majority of patients participates in Walking (63%) followed by Gym sports (26%) and Running Sports (11%). In the Arthrodesis group Gym sports (48%) and Walking (43%) were the most popular sporting activities followed by Running sports (9%) (Fig. 1).
Fig. 1.
Cartiva SCI and Arthrodesis sporting activities.
Mean post-operative FAAM Sports scores were 76.4% for Cartiva SCI and 80.9% for Arthrodesis. Mann-Whitney U testing revealed no statistically significant difference between Cartiva SCI and Arthrodesis (p > 0.3) (Table 2). Kruskal-Walli one-way Anova testing was utilised to match patients comparing age (<55 and >55), gender and severity of arthritis based on the HJ classification. No statistically significant results (p < 0.05) were found.
Table 2.
Foot and Ankle Ability Measure Sports (FAAM Sports) scores.
| Surgery | FAAM SPORTS | Mann-Whitney U |
|---|---|---|
| Cartiva | 76.4% (SD±16.6) | P > 0.3 |
| Arthrodesis | 80.9% (SD±21.9) |
There was 1 Cartiva to Arthrodesis revision at 17 months post-operative due to pain. No revisions were performed in the Arthrodesis group. Revision surgery to arthrodesis is made possible by the small amount of bone resection required to fit the primary Cartiva implant.
4. Discussion
Hallux rigidus is a common and debilitating condition which causes pain, reduced range of motion and swelling. Athletes and the active patient population who wish to preserve their sporting ability will demand the most efficacious treatment. Arthrodesis has long been the gold standard treatment option as it eliminates pain in the majority but sacrifices joint mobility. For some this can be detrimental. With recent improvements in technology and research it is hoped to create a prosthesis which would allow full range of motion and pain elimination to offer patients the best hopes of a successful return to sports.
One patient in this cohort had a revision to arthrodesis due to persistent pain at seventeen months post-operative, whereas no revision surgeries were performed in the Arthrodesis group.
Comparing the severity of arthritis, the arthrodesis group had a lower proportion of HJ3 compared to HJ2 than the cartiva group, we would have expected the Cartiva group to perform less favourably, however no statistically significant results were found. This may indicate that the Cartiva SCI can be as effective as arthrodesis, in the management of severe hallux rigidus in highly physically demanding patient populations.
Also, adjusting the results for age (<55 and >55) and gender (male/female) revealed no statistically significant results indicating that either management technique is applicable to both genders and across all age groups.
The industry funded “Cartiva Motion Study” compared the sporting ability of the Cartiva SCI and Arthrodesis. Its results at 2 years post-op also demonstrated equivalent results with no statistically significant differences. They quoted a 9% Cartiva to Arthrodesis revision rate due to persistent pain which is higher than our study, however, they had a larger cohort of patients as the study was performed across several centers.
Our study demonstrates that both the Cartiva SCI and Arthrodesis result in similar post-operative sporting ability with no statistically significant differences, although clinically, the Arthrodesis group faired better. Cartiva SCI hemiarthroplasty results in a faster return to activities and does preserve some joint mobility whilst reducing pain and therefore may be a viable alternative to arthrodesis.
These initial results for the Cartiva SCI are very encouraging, however, more independent, non industry funded research is necessary with larger cohorts to identify implant survivalship and long term efficacy.
5. Limitations
This is a level 2 cohort study comparing two surgical management techniques for hallux rigidus. There were no set points for data collection, however, minimum follow up was set at 1 year to allow for full recovery of sporting ability. Unfortunately, we could not return Cartiva SCI patients to clinic for evaluation of dorsiflexion as we had no funding for the conduct of this study.
6. Conclusions
Our results suggest that both Arthrodesis and Cartiva SCI result in similar post-operative sporting ability. Cartiva SCI results in a faster return to activities and preserves joint flexibility with adequate pain reduction. Initial results of Cartiva SCI are favourable and comparable to arthrodesis. More research with larger cohorts and longer follow up by non-industry sponsored researchers is indicated.
Funding received
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
None.
Declarations of interest
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jor.2019.09.023
Contributor Information
Bernardo Brandao, Email: brandaobernardo@hotmail.com.
Ahmed Aljawadi, Email: ahmed.aljawadi@doctors.org.uk.
ZhiSheng Edmund Poh, Email: edmundpoh@hotmail.com.
Anna Fox, Email: anna.fox@mft.nhs.uk.
Anand Pillai, Email: anandpillai@nhs.net.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Gould N., Schneider W., Ashikaga T. Epidemiological survey of foot problems in the continental United States: 1978-1979. Foot Ankle. 1980;1(1):8–10. doi: 10.1177/107110078000100104. [DOI] [PubMed] [Google Scholar]
- 2.Lam A., Chan J.J., Surace M.F., Vulcano E. Hallux rigidus: how do I approach it? World J Orthop. 2017;8(5):364–371. doi: 10.5312/wjo.v8.i5.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brage M.E., Ball S.T. Surgical options for salvage of end- stage hallux rigidus. Foot Ankle Clin North Am. 2002;7:49–73. doi: 10.1016/s1083-7515(01)00004-3. [DOI] [PubMed] [Google Scholar]
- 4.Hicks J.H. The mechanics of the foot: II. The plantar aponeurosis and the arch. J Anat. 1954;88(Pt1):25–30. 1. [PMC free article] [PubMed] [Google Scholar]
- 5.York P.J., Wydra F.B., Hunt K.J. Injuries to the great toe. Curr. Rev. Musculoskelet. Med. 2017;10(1):104–112. doi: 10.1007/s12178-017-9390-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jacob H.A. Forces acting in the forefoot during normal gait— an estimate. Clin Biomech. 2001;16(9):783–792. doi: 10.1016/s0268-0033(01)00070-5. [DOI] [PubMed] [Google Scholar]
- 7.Gross C.E., Hsu A.R., Lin J., Holmes G.B., Lee S. Revision MTP arthrodesis for failed MTP arthroplasty. Foot Ankle Spec. 2013;6(6):471–478. doi: 10.1177/1938640013502725. [DOI] [PubMed] [Google Scholar]
- 8.Kline A.J., Hasselman C.T. U.S. National Library of Medicine; May 2013. “Metatarsal Head Resurfacing for Advanced Hallux Rigidus.” Current Neurology And Neuroscience Reports.www.ncbi.nlm.nih.gov/pubmed/23407017 [DOI] [PubMed] [Google Scholar]
- 9.Dawson-Bowling S. U.S. National Library of Medicine; July 2012. “MOJE Ceramic Metatarsophalangeal Arthroplasty: Disappointing Clinical Results at Two to Eight Years.” Current Neurology and Neuroscience Reports.www.ncbi.nlm.nih.gov/pubmed/22835393 [DOI] [PubMed] [Google Scholar]
- 10.Baker M.I., Walsh S.P., Schwartz Z., Boyan B.D. A review of polyvinyl alcohol and its uses in cartilage and orthopedic applications. J Biomed Mater Res B Appl Biomater. 2012 Jul;100(5):1451–1457. doi: 10.1002/jbm.b.32694. [DOI] [PubMed] [Google Scholar]
- 11.Baumhauer J.F., Singh D., Glazebrook M. Correlation of hallux rigidus grade with motion, VAS pain, intraoperative cartilage loss, and treatment success for first MTP joint arthrodesis and synthetic cartilage implant. Foot Ankle Int. 2017 Nov;38(11):1175–1182. doi: 10.1177/1071100717735289. 1071100717735289.5. [DOI] [PubMed] [Google Scholar]
- 12.Baumhauer J.F., Singh D., Glazebrook M. Prospective, randomized, multi-centered clinical trial assessing safety and efficacy of a synthetic cartilage implant versus first metatarsophalangeal arthrodesis in advanced hallux rigidus. Foot Ankle Int. 2016;37(5):457–469. doi: 10.1177/1071100716635560. [DOI] [PubMed] [Google Scholar]
- 13.Daniels T.R., Younger S.E., Penner M.J. Midterm outcomes of polyvinyl alcohol hydrogel hemiarthroplasty of the first metatarsophalangeal joint in advanced hallux rigidus. Foot Ankle Int. 2017;38(3):243–247. doi: 10.1177/1071100716679979. [DOI] [PubMed] [Google Scholar]
- 14.Martin R., Irrgang J., Burdett R., Conti S., VanSwearingen J. Evidence of validity for the foot and Ankle ability measure. Foot Ankle Int. 2005;26(11):968–983. doi: 10.1177/107110070502601113. [DOI] [PubMed] [Google Scholar]
- 15.GraphPad Software, La Jolla California USA, www.graphpad.com.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.